Introduction
Previous studies have shown that systemic diseases
are known to be associated with periodontitis (1). The prevalence of both diabetes mellitus
and hypertension is increasing worldwide (2). Diabetes and hypertension are widely
studied for possible association with periodontitis (3,4). The
rapid increase in the prevalence of diabetes is also seen in Korea
(5). The prevalence of diabetes
among adults aged ≥30 years in 2001, 2005 and 2007–2009 was 8.9,
9.1 and 9.9%, respectively based on the series of Korea National
Health and Nutrition Examination Surveys (5). The report with more current results
showed that the prevalence of diabetes increased up to 11.0% in
2013 (6). Complication of diabetes
includes diabetic retinopathy, diabetic nephropathy, diabetic
neuropathy and macrovascular diseases (7). Previous report showed that the
prevalence of hypertension was 28.5% in the Korean National Health
and Nutrition Examination Survey in 2011 (8). The report indicated that the awareness,
treatment, and control rates of the generation population were
generally improved. Researchers have shown that a relationship
exists between type 2 diabetes mellitus and periodontal disease
(9). Glycemic control has been shown
to affect periodontal disease and participants having poorly
controlled diabetes were associated with severe periodontitis
(10). Similarly, a positive
association has been reported between hypertension and
periodontitis (4). All periodontal
measures had significant associations with hypertension (11).
However, the association between impaired fasting
glucose or high blood pressure and periodontitis in individuals
without diabetes or hypertension is not yet well understood. Thus,
this study was performed to assess the relationship between fasting
glucose and systolic/diastolic blood pressure on the prevalence of
periodontitis in non-diabetic and non-hypertensive adults using
nationally representative data. Subgroup analysis was performed to
evaluate the combined effects of obesity/abdominal obesity and
impaired fasting glucose.
Materials and methods
Survey and subjects
This survey was reviewed and approved by the
Institutional Review Board of the Korean Centers for Disease
Control and Prevention, and all participants provided written
informed consent. This study is a secondary data analysis of data
collected during the Korean National Health and Nutrition
Examination Survey (KNHANES) from 2013 to 2015. The Institutional
Review Board at the Catholic University of Korea approved of this
study (KC16EISI0713). This study is a human observational study and
the authors have conformed to the STROBE guidelines.
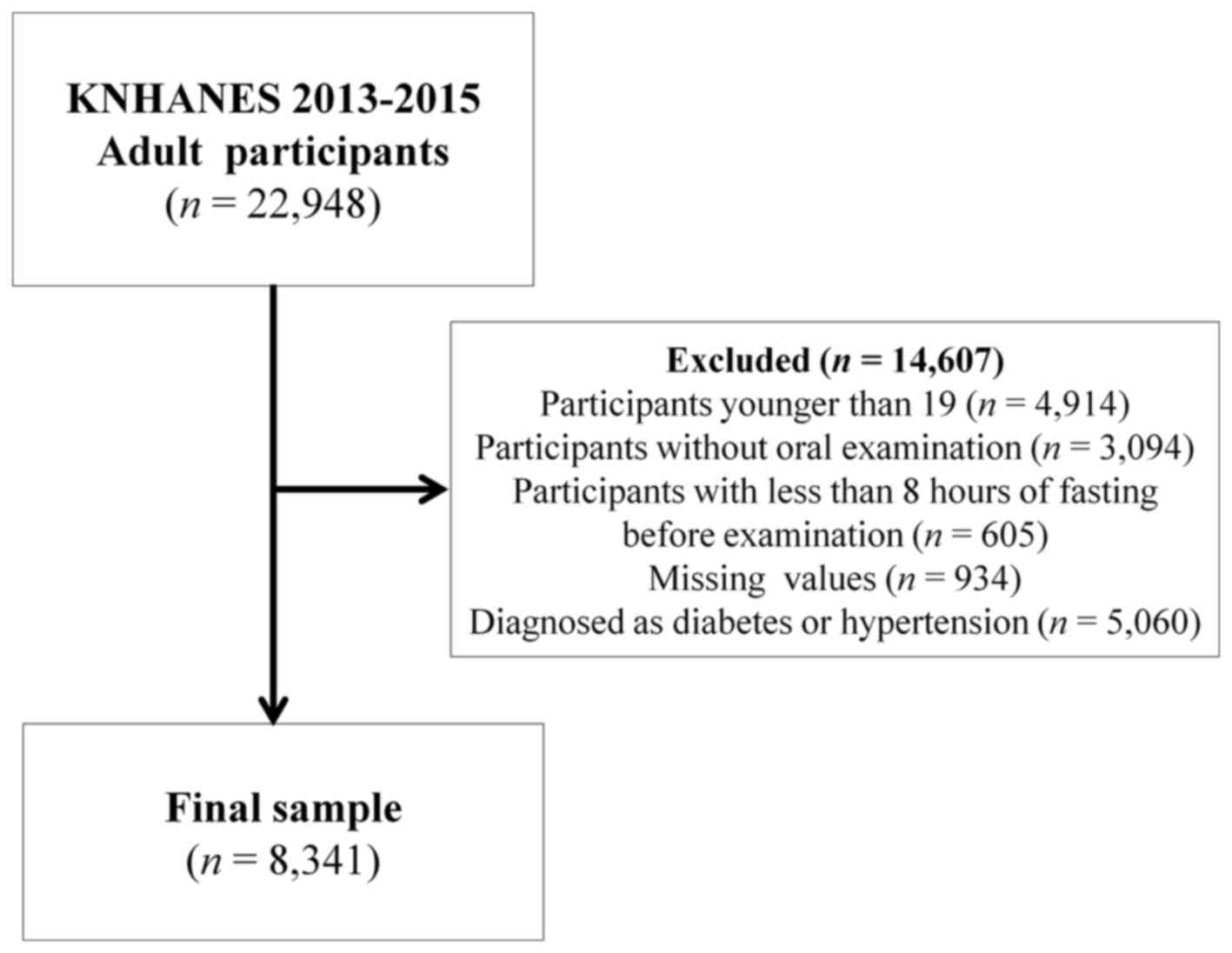
A total of 22,948 individuals participated in the
KNHANES survey. The number of surveys was reduced to 13,401 by
excluding participants without periodontal examination,
participants with less than 8 h of fasting before examination, and
individuals who were younger than 19 years old. The analysis in
this study was confined to a total of 8,341 responses that had no
missing values for the outcome variables (Fig. 1).
Demographic variables
Sociodemographic and lifestyle variables of
participants were evaluated with a self-administered questionnaire
regarding education level, household income, smoking, and alcohol
intake. Smokers were classified as current smokers or non-smokers.
Alcohol consumption was categorized as drinkers [mild to moderate
drinkers (1–30 g/day)], and heavy drinkers (>30 g/day), or
non-drinkers. Education level was categorized as either entered
high school (≥10 years) or not. Number of household members was
evaluated. Household income was divided into quartiles by number of
included family members. The lowest quartile of household income
was less than 1,092.40 USD/month.
Anthropometric measurements
Trained staff members performed the measurements of
the participants. Heath status of each participant was evaluated.
Body weight and height were measured with the participants in light
indoor clothing without shoes (12).
Waist circumference was measured at the narrowest point between the
lower border of the rib cage and the iliac crest. Body mass index
was calculated by the following formula: weight/height2
(kg/m2). Systolic blood pressure and diastolic blood
pressure were measured on the right arm using a standard mercury
sphygmomanometer (Baumanometer; W.A. Baum Co., Inc., Copiague, NY,
USA). Systolic blood pressure and diastolic blood pressure
measurements were performed two times with a 5-min interval, and
the average of the two measurements was used for the analysis.
After fasting for more than 8 h, blood samples were
collected from the antecubital veins. Serum fasting plasma glucose,
glycated hemoglobin, the total concentration of cholesterol,
low-density lipoprotein, and triglycerides were tested with the
Automatic Analyzer 7600 (Hitachi, Tokyo, Japan) using the kits
(Daiichi, Tokyo, Japan) (13).
Description of obesity, diabetes
mellitus, and hypertension
Body mass index was categorized by ≥25
kg/m2 or lower. Waist circumference was categorized as
≥90 cm in men and ≥80 cm in women. A body mass index (BMI) ≥25
kg/m2 was defined as the presence of obesity (14), and the cutoffs of abdominal obesity
were defined as waist circumference (WC) ≥90 cm in men or ≥85 cm in
women (15). Diabetes was diagnosed
if fasting blood sugar was ≥126 mg/dl, glycated hemoglobin was
≥6.5% or the individual was currently using antidiabetic
medications (16). Impaired fasting
glucose was defined as a level of blood glucose between 100 and 125
mg/dl with no diabetic medication. Hypertension was defined as
systolic blood pressure ≥140 mmHg and diastolic blood pressure was
≥90 mmHg or reported use of regular antihypertensive drugs
(17). Metabolic syndrome was
diagnosed if three or more of the following criteria were
fulfilled: waist circumference ≥90 cm in men and ≥80 cm in women;
fasting triglycerides ≥150 mg/dl or use of lipid-lowering
medication; high-density lipoprotein cholesterol <40 mg/dl in
men and <50 mg/dl in women or use of lipid-lowering medication;
blood pressure ≥130/85 mmHg or use of antihypertensive medication;
and fasting blood glucose ≥100 mg/dl or current use of antidiabetic
medication (18).
Oral health behaviors and
periodontitis
Periodontal treatment needs were assessed using the
Community Periodontal Index (CPI), which the World Health
Organization/Federation Dentaire Internationale has defined as an
epidemiological screening procedure for rough depiction of
periodontal status and treatment needs by trained dental
practitioners (19). All teeth of
each subject were divided into sextants. A specially designed
periodontal probe (PWHO, Osung MND, Seoul, Republic of Korea) with
a ball end 0.5 mm in diameter was used. Ten specific index teeth
(17, 16, 11, 26, 27, 36, 37, 31, 46 and 47) were examined to
evaluate each sextant's score. A sextant was only scanned if two or
more teeth were present. If index teeth were absent from a sextant,
then all of the remaining teeth were examined to produce the score,
and the highest score was recorded as the score for the sextant.
Code 3 was used for a shallow pocket with depth of 3.5–5.5 mm and
code 4 for a deep pocket depth ≥5.5 mm. Moderate periodontal
disease was defined if CPI was code 3 and severe periodontitis was
defined if CPI was code 4. Presence of periodontitis was defined if
CPI was 3 or greater.
The frequency of daily tooth brushing and use of
secondary oral products were used for the evaluation of oral health
behavior. Secondary oral products included dental floss, mouthwash,
interdental brushes, electric toothbrushes, irrigation devices,
tongue cleaners, end-tufted brushes, and special devices for
dentures. The survey also recorded the participants' tooth
pain.
Statistical analysis
All analyses were conducted using SAS version 9.3
(SAS Institute Inc., Cary, NC, USA). The SAS survey procedure was
applied to reflect the complex sampling design and the sampling
weights of KNHANES and to provide nationally representative
prevalence estimates. The data are presented as the mean ± standard
error of the mean for continuous variables and as proportions
(standard errors) for categorical variables. A Chi-square test for
categorical variables or an independent t-test for continuous
variables was performed to assess the differences in
characteristics categorized by presence of periodontitis. Logistic
regression analysis was used to evaluate the periodontitis in
association with impaired fasting glucose categorized by the
presence of obesity or abdominal obesity. The model was adjusted
for age, sex, smoking, drinking, education, income, body mass
index, number of natural teeth, frequency of tooth brushing per
day, and use of secondary oral products.
Results
Table I shows the
baseline characteristics of study participants according to the
presence of periodontitis. Among the 8,341 participants, 1,968 were
diagnosed as having periodontitis. The percentage of males was
higher in periodontitis group (P<0.05). The systolic blood
pressure, diastolic blood pressure, glucose level, glycated
hemoglobin, body mass index, total cholesterol, low-density
lipoprotein, and triglycerides were statistically higher in the
periodontitis group (P<0.05). The numbers of current smokers and
individuals with lower income or tooth pain were higher in the
periodontitis group. However, the percentage of individuals with
tooth brushing frequency of three or higher per day and the
percentage of individuals using secondary oral products were
significantly lower in the periodontitis group (P<0.05).
 | Table I.Baseline characteristics of study
participants according to presence of periodontitis. |
Table I.
Baseline characteristics of study
participants according to presence of periodontitis.
|
| Periodontitis |
|
|---|
|
|
|
|
|---|
| Variables | No | Yes | P-valuea |
|---|
| Total | 6,373 | 1,968 |
|
| Age, years |
37.94±0.23 |
49.29±0.37 | <0.0001 |
| Male | 44.65 (0.66) | 56.24 (1.17) | <0.0001 |
| Systolic blood
pressure (mmHg) | 109.73±0.18 | 112.91±0.31 | <0.0001 |
| Diastolic blood
pressure (mmHg) |
72.33±0.15 |
74.01±0.22 | <0.0001 |
| Glucose (mg/dl) |
91.66±0.15 |
94.88±0.24 | <0.0001 |
| Glycated hemoglobin
(%) |
5.46±0.01 |
5.59±0.01 | <0.0001 |
| Body mass index
(kg/m2) |
22.98±0.05 |
23.69±0.08 | <0.0001 |
| Body mass index ≥25
kg/m2 (%) | 23.64 (0.62) | 30.92 (1.20) | <0.0001 |
| Waist circumference
(cm) |
78.33±0.17 |
81.4±0.24 | <0.0001 |
| Waist circumference
≥90 cm in men and ≥80 cm in women (%) | 15.37 (0.56) | 21.6
(1.11) | <0.0001 |
| Metabolic syndrome
(yes) | 9.6
(0.43) | 18.76 (1.08) | <0.0001 |
| Total cholesterol
(mg/dl) | 184.57±0.50 | 193.38±0.88 | <0.0001 |
| Low-density
lipoprotein (mg/dl) | 109.12±0.43 |
116.9±0.81 | <0.0001 |
|
Triglyceridesb | 95.07
(93.48–96.69) | 116.28
(112.80–119.88) | <0.0001 |
| Smoking,
current | 16.39 (0.66) | 27.52 (1.33) | <0.0001 |
| Drinking,
current | 61.74 (0.70) | 58.78 (1.37) | 0.0421 |
|
Education-university graduate or
higher | 45.47 (0.90) | 32.61 (1.51) | <0.0001 |
| Income, lowest
quartile | 9.14
(0.54) | 12.52 (0.96) | 0.0004 |
| Number of natural
teeth | 26.6±0.05 |
24.94±0.13 | <0.0001 |
| Frequency of tooth
brushing per day |
|
| <0.0001 |
| ≤1 | 6.55
(0.37) | 9.98
(0.78) |
|
| 2 | 34.09 (0.66) | 39.94 (1.36) |
|
| ≥3 | 59.36 (0.72) | 50.08 (1.38) |
|
| Use of secondary
oral products | 56.99 (0.77) | 52.18 (1.43) | 0.0021 |
| Tooth pain | 35.99 (0.87) | 44.89 (1.41) | <0.0001 |
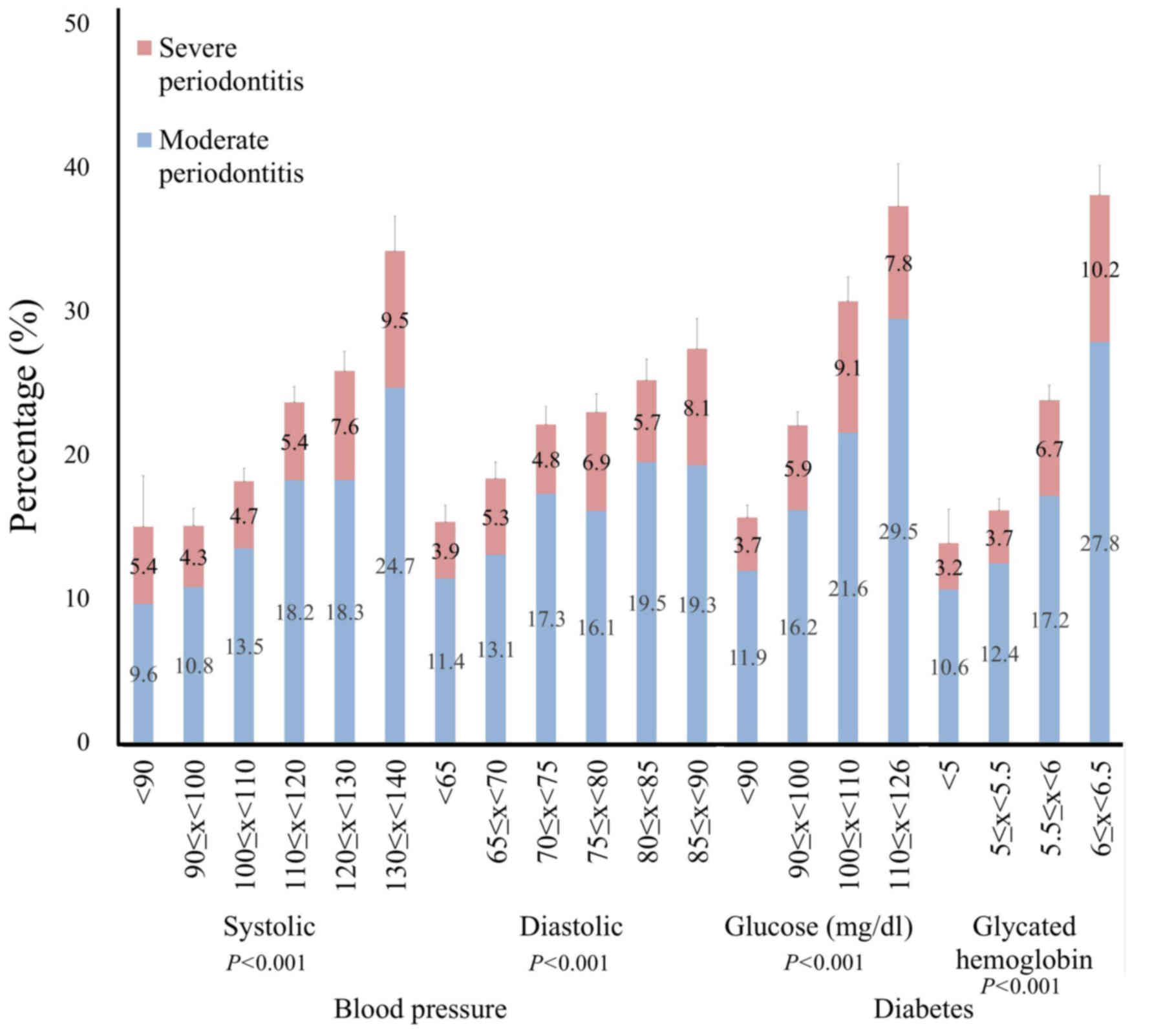
The percentage of moderate and severe periodontitis
categorized by blood pressure and glucose level is shown in
Fig. 2. The percentage of
periodontitis increased with increasing systolic blood pressure.
Similar trends were seen with diastolic blood pressure. The
percentage of periodontitis increased with higher glucose level,
with similar trends in glycated hemoglobin.
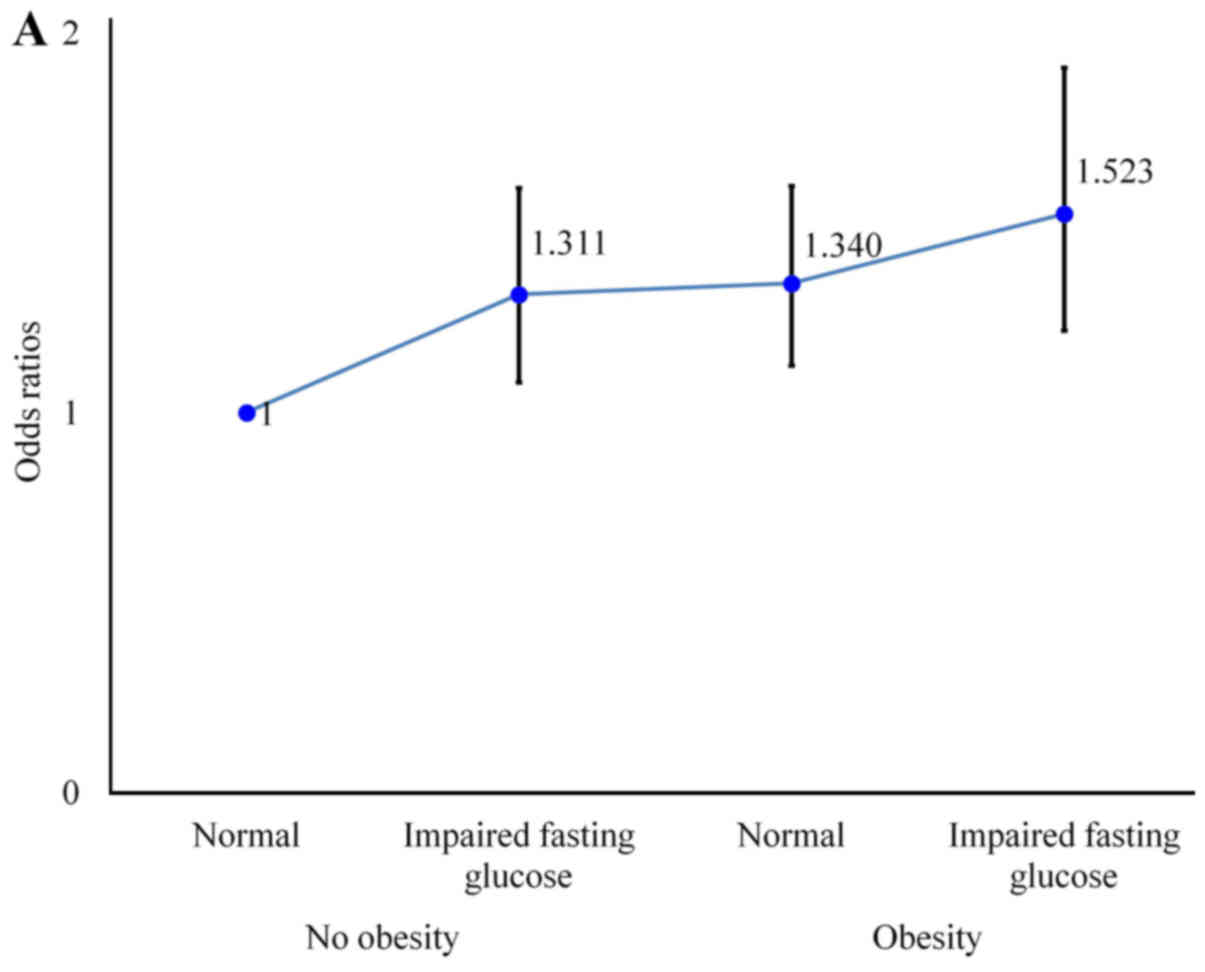
The prevalence of periodontitis in the combination
of obesity/abdominal obesity and impaired fasting glucose level is
shown in Fig. 3. Fig. 3A shows odds ratios (ORs) of
periodontitis categorized by the presence of obesity and impaired
fasting glucose. Even for participants without obesity, the ORs
increased to 1.311. For participants with obesity having impaired
fasting glucose, the ORs of periodontitis increased to 1.523.
Similar trends were seen with participants with abdominal obesity
(Fig. 3B). ORs for participants
without abdominal obesity having impaired glucose, participants
with abdominal obesity with normal glucose level, and individuals
having combination of abdominal obesity and impaired fasting
glucose were 1.320, 1.297 and 1.434, respectively, when a
non-abdominally obese individual with normal fasting glucose was
considered as reference.
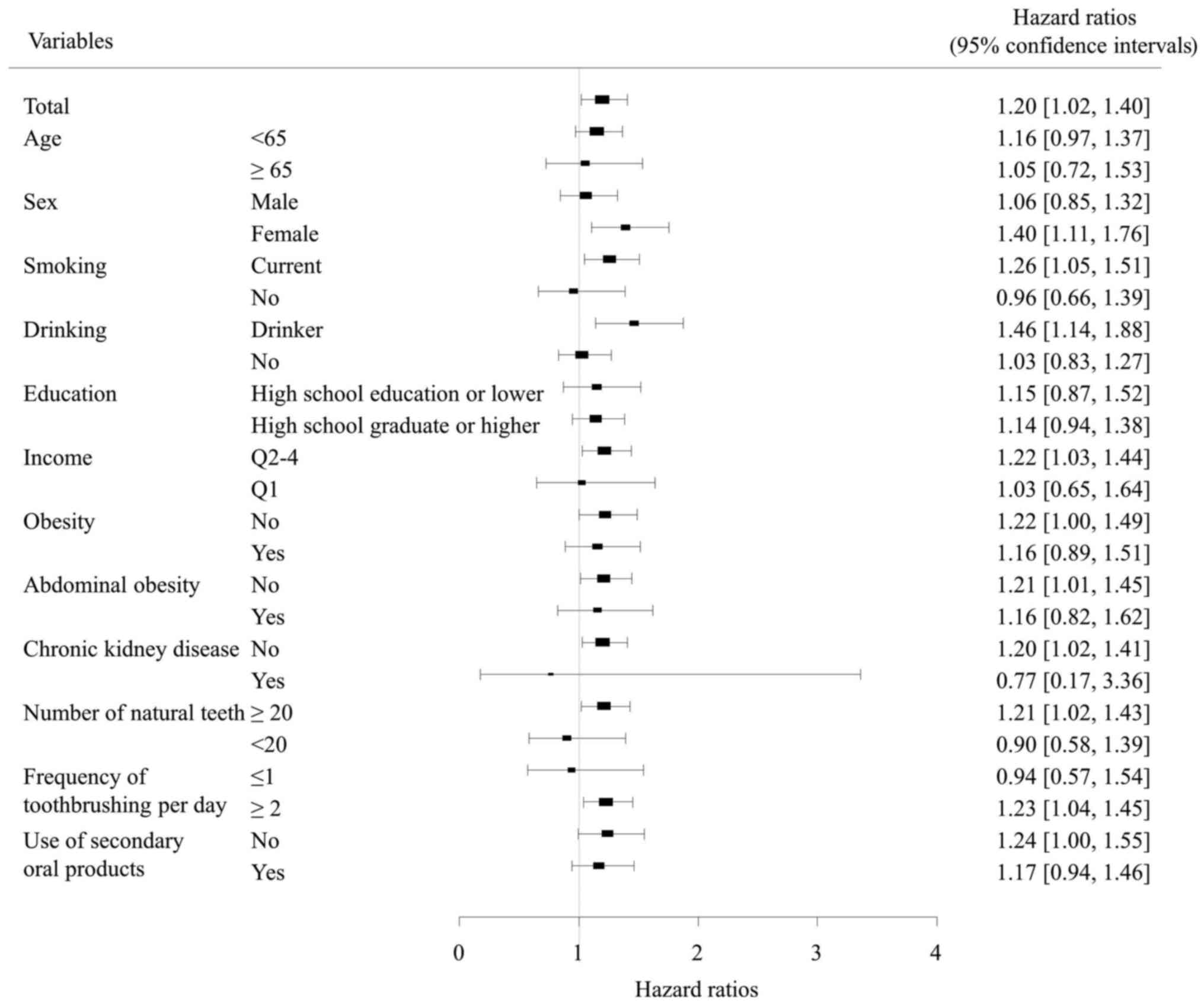
Fig. 4 shows ORs and
95% confidence intervals (CIs) of periodontitis after adjustments
for age, sex, smoking, drinking, education, income, body mass
index, waist circumference, chronic kidney disease, number of
natural teeth, frequency of tooth brushing per day, and use of
secondary oral products.
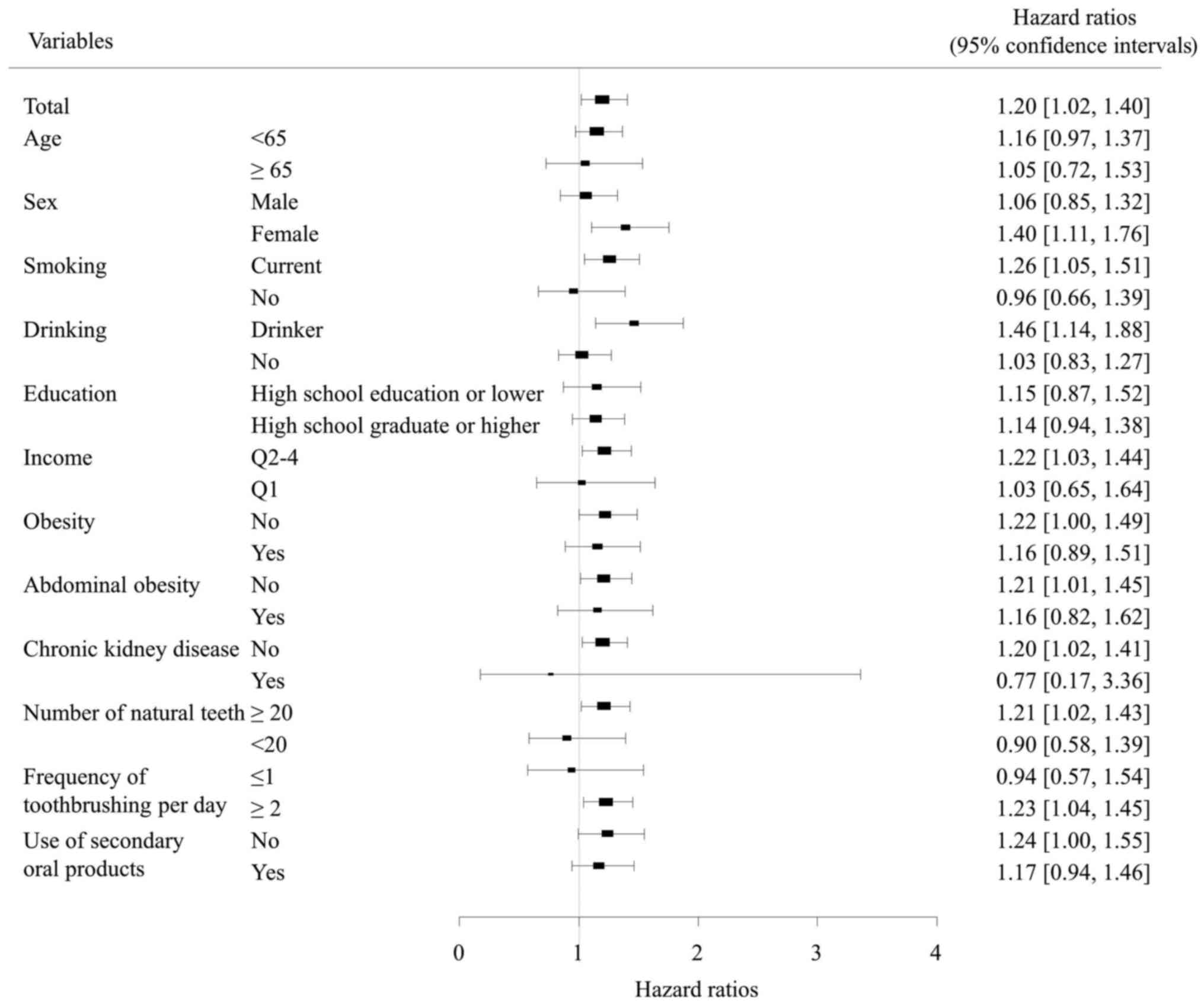 | Figure 4.Hazard ratios and 95% confidence
intervals of periodontitis in individuals with impaired fasting
glucose after adjustments for age, sex, smoking, drinking,
education, income, body mass index, waist circumference, chronic
kidney disease, number of natural teeth, frequency of tooth
brushing per day, use of secondary oral products and duration of
sleep. |
Table II shows the
ORs and 95% CIs of periodontitis categorized by systolic blood
pressure, diastolic blood pressure, glucose, and glycated
hemoglobin. The ORs and 95% CIs for systolic blood pressure of
90≤x<100, 100≤x<110, 110≤x<120, 120≤x<130, and
130≤x<140 were 1.116 (0.591, 2.107), 1.165 (0.624, 2.175), 1.238
(0.673, 2.278), 1.008 (0.538, 1.888), and 1.042 (0.545, 1.993),
respectively, when systolic blood pressure <90 was considered as
reference. The ORs and 95% CIs for diastolic blood pressure of
65≤x<70, 70≤x<75, 75≤x<80, 80≤x<85, and 85≤x<90 were
1.192 (0.94, 1.511), 1.324 (1.049, 1.67), 1.152 (0.905, 1.467),
1.188 (0.931, 1.516), and 1.263 (0.937, 1.702), respectively, when
diastolic blood pressure <65 was considered as reference. The
ORs and 95% CIs for glucose of 90≤x<100, 100≤x<110, and
110≤x<126 were 1.074 (0.92, 1.253), 1.214 (0.986, 1.494), and
1.358 (1.005, 1.834), respectively, when glucose <90 was
considered as reference. The ORs and 95% CIs for glycated
hemoglobin 5≤x<5.5, 5.5≤x<6, and 6≤x<6.5 were 0.887
(0.583, 1.348), 0.853 (0.559, 1.301), and 1.021 (0.652, 1.599),
respectively, when glycated hemoglobin <5 was considered as
reference.
 | Table II.Odds ratios and 95% confidence
interval for periodontitis categorized by systolic blood pressure,
diastolic blood pressure, glucose and glycated hemoglobin. |
Table II.
Odds ratios and 95% confidence
interval for periodontitis categorized by systolic blood pressure,
diastolic blood pressure, glucose and glycated hemoglobin.
|
| Odds ratios (95%
confidence interval) |
|---|
|
|
|
|---|
| Variables | Model 1 | Model 2 | Model 3 |
|---|
| Systolic blood
pressure (mmHg) |
|
<90 | 1 (reference) | 1 (reference) | 1 (reference) |
|
90≤x<100 | 1.191 (0.642,
2.21) | 1.113 (0.589,
2.101) | 1.118 (0.591,
2.114) |
|
100≤x<110 | 1.247 (0.676,
2.301) | 1.156 (0.619,
2.158) | 1.169 (0.625,
2.185) |
|
110≤x<120 | 1.37 (0.754,
2.487) | 1.243 (0.676,
2.284) | 1.245 (0.676,
2.293) |
|
120≤x<130 | 1.183 (0.641,
2.184) | 1.014 (0.542,
1.899) | 1.013 (0.540,
1.900) |
|
130≤x<140 | 1.259 (0.669,
2.369) | 1.072 (0.56,
2.055) | 1.044 (0.545,
2.002) |
| Diastolic blood
pressure (mmHg) |
|
<65 | 1 (reference) | 1 (reference) | 1 (reference) |
|
65≤x<70 | 1.149 (0.912,
1.447) | 1.171 (0.927,
1.481) | 1.193 (0.941,
1.513) |
|
70≤x<75 | 1.391 (1.107,
1.747) | 1.322 (1.05,
1.665) | 1.325 (1.050,
1.672) |
|
75≤x<80 | 1.227 (0.968,
1.556) | 1.156 (0.91,
1.468) | 1.156 (0.908,
1.472) |
|
80≤x<85 | 1.267 (0.995,
1.612) | 1.177 (0.924,
1.498) | 1.190 (0.933,
1.519) |
|
85≤x<90 | 1.443 (1.082,
1.925) | 1.271 (0.945,
1.711) | 1.270 (0.942,
1.711) |
| Glucose
(mg/dl) |
|
<90 | 1 (reference) | 1 (reference) | 1 (reference) |
|
90≤x<100 | 1.113 (0.959,
1.292) | 1.076 (0.923,
1.254) | 1.071 (0.918,
1.250) |
|
100≤x<110 | 1.333 (1.093,
1.627) | 1.214 (0.988,
1.492) | 1.212 (0.984,
1.492) |
|
110≤x<126 | 1.542 (1.163,
2.044) | 1.364 (1.014,
1.835) | 1.355 (1.003,
1.830) |
| Glycated hemoglobin
(%) |
|
<5 | 1 (reference) | 1 (reference) | 1 (reference) |
|
5≤x<5.5 | 0.958 (0.634,
1.447) | 0.893 (0.586,
1.36) | 0.887 (0.584,
1.349) |
|
5.5≤x<6 | 1.027 (0.68,
1.55) | 0.864 (0.565,
1.321) | 0.853 (0.559,
1.302) |
|
6≤x<6.5 | 1.354 (0.881,
2.081) | 1.072 (0.682,
1.684) | 1.018 (0.650,
1.594) |
Discussion
This study showed that both impaired fasting glucose
and prehypertension were associated with periodontitis by multiple
logistic regression analyses after adjusting for confounding
factors among Korean adults. Subgroup analysis revealed that ORs of
periodontitis increased in impaired fasting glucose in both
non-obese and obese participants. Highest ORs were seen with the
combination of impaired fasting glucose and obesity/abdominal
obesity.
Various parameters can be used to determine impaired
fasting glucose and prehypertension (17,20–24).
Impaired fasting glucose was defined as a level of blood glucose
between 100 and 125 mg/dl with no diabetic medication (17). The criteria for the World Health
Organization is 110≤x<125 mg/dl (20). Regarding hypertension, if the
participants were ≥60 years old, then average blood pressure of
150/90 mmHg or lower was considered as controlled, and the criteria
of blood pressure <140/90 mmHg was considered controlled for
individuals younger than 60 (21). A
previous report recommended lower targets for individuals with
diabetes mellitus of 130/80 mmHg (22). In a previous study, prehypertension
was defined as systolic blood pressure between 120 and 139 mmHg or
diastolic blood pressure between 80 to 89 mmHg (23). In another study, participants with
repeated measurements of systolic pressure of 130 to 139 mmHg and
diastolic pressure of 89 mmHg or lower, or systolic pressure of 139
mmHg or lower and diastolic pressure of 85 to 89 mmHg, were
assigned to the treatment of prehypertension (24). In this study, we classified the
glucose level and glycated hemoglobin into four stages according to
the severity. Systolic and diastolic blood pressure was categorized
into six stages according to the severity.
A previous report recommended initiating treatment
in adults aged 60 years or older with systolic blood pressure
persistently at or above 150 mmHg to achieve a target systolic
blood pressure of less than 150 mmHg to reduce the risk for
mortality, stroke, and cardiac events (25). However, it was noted that evidence
was low in quality for achieving a target systolic blood pressure
of less than 140 mmHg to reduce the risk of stroke or cardiac
events. Similarly, another report showed that more intensive blood
pressure-lowering treatment of a group with mean blood pressure
level of 133/76 mmHg resulted in no clear effects on total
mortality, cardiovascular death, heart failure, or end-stage renal
disease (26). Fewer studies have
been performed regarding prehypertension and it was shown that
prehypertension was considered a precursor of stage 1 hypertension
and a predictor of excessive cardiovascular risk (24). Prevalence of periodontitis in the
prehypertension group increased from 25.8% for systolic blood
pressure of 120≤x<130 mmHg and 34.2% for 130≤x<140 mmHg,
respectively. Prevalence of periodontitis in the prehypertension
group increased from 25.2 to 27.4% for diastolic blood pressure of
80≤x<85 and 85≤x<90 mmHg, respectively.
A previous report showed pre-diabetes related to
impaired fasting glucose was positively associated with
periodontitis (27). Research has
also shown that periodontitis showed an association with decreased
β-cell function and increased prevalence of impaired fasting
glucose before onset of diabetes (28). It was also shown that chronic
periodontitis measured by clinical attachment loss and pocket depth
was positively associated in a linear relation with impaired
fasting glucose (28). This study
also showed that the percentage of periodontitis increased from
22.0% for fasting glucose level of 90≤x<100 mg/dl, 30.7% for
fasting glucose level of 100≤x<110 mg/dl, and 37.3% for fasting
glucose level of 110≤x<126 mg/dl. ORs of periodontitis increased
with impaired fasting glucose and combination of obesity and
impaired fasting glucose showed the highest ORs of 1.523. The
relative increase of ORs of impaired fasting glucose for
periodontitis was 1.311 for no obesity but 1.137 for the obesity
group. Similar trends were seen regarding abdominal obesity. The
relative increase of ORs of impaired fasting glucose for
periodontitis was 1.320 for no abdominal obesity but 1.106 for the
abdominal obesity group. It should also be considered that more
care may be given to prehypertensive individuals with impaired
fasting glucose (23).
This study emphasized the importance of evaluation
and treatment of periodontitis in individuals with prediabetes and
prehypertension. This study has great strength because the
conclusion was derived from nationally representative data
(29). The design of this study is
based on a stratified, multistage, probability-cluster survey of
the population of institutionalized civilians (30). Oral health was evaluated using
periodontal index from index teeth using probing depth (31). A multiple regression analysis was
used to evaluate periodontitis in relation to impaired fasting
glucose and blood pressure after adjustment for various confounding
factors including age, sex, smoking, drinking, socioeconomic
factors, oral health behavior, and systemic diseases (32). However, it should be noted that the
causal direction of the associations between
prediabetes/prehypertension and periodontitis cannot be ascertained
due to the design of this study being cross-sectional (33).
The association between fasting glucose/blood
pressure and periodontitis was proven by multiple logistic
regression analyses after adjusting for confounding factors among
non-diabetic and non-hypertensive Korean adults. Subgroup analysis
showed that higher ORs of periodontitis were noted in participants
having both impaired glucose level and obesity when compared with
individuals without impaired glucose level or obesity. Further
prospective studies with a larger sample size of individuals over a
longer period of time are required to evaluate the cause-and-effect
association. The results of the present study suggest that
detection of fasting glucose and blood pressure may serve as a risk
indicator for periodontal disease.
Acknowledgements
The authors thank the Korea Centers for Disease
Control and Prevention for providing the necessary data.
Funding
This study was supported by Research Fund of Seoul
St. Mary's Hospital, The Catholic University of Korea. This work
was partly supported by Basic Science Research Program through the
National Research Foundation of Korea funded by the Ministry of
Science, ICT & Future Planning, Daejeon, Republic of Korea
(grant no. NRF-2017R1A1A1A05001307).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KH and JP collaborated to design the study; KH and
JP were responsible for data access and analysis; KH and JP wrote
the manuscript; both authors reviewed the manuscript.
Ethics approval and consent to
participate
The Institutional Review Board at the Catholic
University of Korea approved this study (approval no.
KC16EISI0713).
Patient consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Kim J and Amar S: Periodontal disease and
systemic conditions: A bidirectional relationship. Odontology.
94:10–21. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tatsumi Y and Ohkubo T: Hypertension with
diabetes mellitus: Significance from an epidemiological perspective
for Japanese. Hypertens Res. 40:795–806. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Paizan Macedo ML and Vilela-Martin JF: Is
there an association between periodontitis and hypertension? Curr
Cardiol Rev. 10:355–361. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Choi HM, Han K, Park YG and Park JB:
Associations among oral hygiene behavior and hypertension
prevalence and control: The 2008 to 2010 Korea national health and
nutrition examination survey. J Periodontol. 86:866–873. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cho NH: Diabetes burden and prevention in
Korea and the Western Pacific Region. Diabetes Res Clin Pract. 106
Suppl 2:S282–S287. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ha KH and Kim DJ: Current status of
managing diabetes mellitus in Korea. Korean J Intern Med.
31:845–850. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cade WT: Diabetes-related microvascular
and macrovascular diseases in the physical therapy setting. Phys
Ther. 88:1322–1335. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee HY and Park JB: The Korean society of
hypertension guidelines for the management of hypertension in 2013:
Its essentials and key points. Pulse (Basel). 3:21–28. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Amiri AA, Maboudi A, Bahar A, Farokhfar A,
Daneshvar F, Khoshgoeian HR, Nasohi M and Khalilian A: Relationship
between Type 2 diabetic retinopathy and periodontal disease in
iranian adults. N Am J Med Sci. 6:139–144. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lakschevitz F, Aboodi G, Tenenbaum H and
Glogauer M: Diabetes and periodontal diseases: Interplay and links.
Curr Diabetes Rev. 7:433–439. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsakos G, Sabbah W, Hingorani AD, Netuveli
G, Donos N, Watt RG and D'Aiuto F: Is periodontal inflammation
associated with raised blood pressure? Evidence from a National US
survey. J Hypertens. 28:2386–2393. 2010.PubMed/NCBI
|
|
12
|
Nam GE, Kim do H, Cho KH, Park YG, Han KD,
Choi YS, Kim SM, Ko BJ, Kim YH and Lee KS: Estimate of a predictive
cut-off value for serum 25-hydroxyvitamin D reflecting abdominal
obesity in Korean adolescents. Nutr Res. 32:395–402. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wallace TM, Levy JC and Matthews DR: Use
and abuse of HOMA modeling. Diabetes Care. 27:1487–1495. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Oh SW, Shin SA, Yun YH, Yoo T and Huh BY:
Cut-off point of BMI and obesity-related comorbidities and
mortality in middle-aged Koreans. Obes Res. 12:2031–2040. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee S, Park HS, Kim SM, Kwon HS, Kim DY,
Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, et al: Cut-off points of
waist circumference for defining abdominal obesity in the Korean
population. Korean J Obes. 15:1–9. 2006. View Article : Google Scholar
|
|
16
|
Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH,
Kim CS, Song KH, Won JC, Lim S, Choi SH, et al: Prevalence of
diabetes and prediabetes according to fasting plasma glucose and
HbA1c. Diabetes Metab J. 37:349–357. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Worede A, Alemu S, Gelaw YA and Abebe M:
The prevalence of impaired fasting glucose and undiagnosed diabetes
mellitus and associated risk factors among adults living in a rural
Koladiba town, northwest Ethiopia. BMC Res Notes. 10:2512017.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim YH, Kim DH, Lim KS, Ko BJ, Han BD, Nam
GE, Park YG, Han KD, Kim JH and Cho KH: Oral health behaviors and
metabolic syndrome: The 2008–2010 Korean National Health And
Nutrition Examination Survey. Clin Oral Investig. 18:1517–1524.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Park JB, Han K, Park YG and Ko Y:
Association between alcohol consumption and periodontal disease:
The 2008 to 2010 Korea national health and nutrition examination
survey. J Periodontol. 85:1521–1528. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Alberti KG and Zimmet PZ: Definition,
diagnosis and classification of diabetes mellitus and its
complications. Part 1: diagnosis and classification of diabetes
mellitus provisional report of a WHO consultation. Diabet Med.
15:539–553. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
James PA, Oparil S, Carter BL, Cushman WC,
Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML,
MacKenzie TD, Ogedegbe O, et al: 2014 evidence-based guideline for
the management of high blood pressure in adults: Report from the
panel members appointed to the Eighth Joint National Committee (JNC
8). JAMA. 311:507–520. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Arguedas JA, Leiva V and Wright JM: Blood
pressure targets for hypertension in people with diabetes mellitus.
Cochrane Database Syst Rev CD008277. 2013. View Article : Google Scholar
|
|
23
|
Zhang Y, Lee ET, Devereux RB, Yeh J, Best
LG, Fabsitz RR and Howard BV: Prehypertension, diabetes, and
cardiovascular disease risk in a population-based sample: The
Strong Heart Study. Hypertension. 47:410–414. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Julius S, Nesbitt SD, Egan BM, Weber MA,
Michelson EL, Kaciroti N, Black HR, Grimm RH Jr, Messerli FH,
Oparil S, et al: Feasibility of treating prehypertension with an
angiotensin-receptor blocker. N Engl J Med. 354:1685–1697. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Qaseem A, Wilt TJ, Rich R, Humphrey LL,
Frost J and Forciea MA: Clinical Guidelines Committee of the
American College of Physicians and the Commission on Health of the
Public and Science of the American Academy of Family Physician:
Pharmacologic treatment of hypertension in adults aged 60 years or
older to higher versus lower blood pressure targets: A clinical
practice guideline from the american college of physicians and the
american academy of family physicians. Ann Intern Med. 166:430–437.
2017. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xie X, Atkins E, Lv J, Bennett A, Neal B,
Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, et al:
Effects of intensive blood pressure lowering on cardiovascular and
renal outcomes: Updated systematic review and meta-analysis.
Lancet. 387:435–443. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Arora N, Papapanou PN, Rosenbaum M, Jacobs
DR Jr, Desvarieux M and Demmer RT: Periodontal infection, impaired
fasting glucose and impaired glucose tolerance: Results from the
continuous national health and nutrition examination survey
2009–2010. J Clin Periodontol. 41:643–652. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Islam SK, Seo M, Lee YS and Moon SS:
Association of periodontitis with insulin resistance, beta-cell
function and impaired fasting glucose before onset of diabetes.
Endocr J. 62:981–989. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Song IS, Han K, Ryu JJ and Park JB:
Association between underweight and tooth loss among Korean adults.
Sci Rep. 7:415242017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hong M, Park JB, Kim YS, Lee DH, Kim H,
Lee JI, Ahn HS, Sohn TS, Lee TK, et al: Association between
Cockroach-specific Immunoglobulin E and periodontitis in Korean
male adults Based on Korean National Health And Nutrition
Examination Survey. Sci Rep. 7:463732017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Han K, Ko Y, Park YG and Park JB:
Associations between the periodontal disease in women before
menopause and menstrual cycle irregularity: The 2010–2012 Korea
national health and nutrition examination survey. Medicine
(Baltimore). 95:e27912016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Choi HM, Han K, Park YG and Park JB:
Associations between the number of natural teeth and renal
dysfunction. Medicine (Baltimore). 95:e46812016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Han K and Park JB: Association between
oral health behavior and periodontal disease among Korean adults:
The Korea national health and nutrition examination survey.
Medicine (Baltimore). 96:e61762017. View Article : Google Scholar : PubMed/NCBI
|