Introduction
Retina originates from neuroectodermal growth in
human embryonic development. Retina has complex tissue structure,
active metabolism and high susceptibility to injury, such as
ischemia and hypoxia (1,2). Nutrition for each layer of retina comes
from the blood circulation in vein, artery and choroid on retina,
which is also the main factor of the formation and maintenance of
vision (3). Once the blood
microcirculation of retina is affected by a sudden disease, human
vision will be affected and a series of ophthalmic diseases, such
as amblyopia, cataract, glaucoma and even blindness will be caused
(4).
Central serous chorioretinopathy (CSC) is relatively
common among retinal diseases (5).
CSC is a choroid retinopathy caused by the detachment of posterior
serous neural epithelium after vasospasm resulted by the
neurovascular disease, and mainly occurs in one eye (6). At present, fundus fluorescein
angiography (FFA) is mainly used in the clinical diagnosis of CSC
due to the advantages of high accuracy and specificity, but the
detection time is longer and the cost is high, and it may cause
some damage to patient's retina (7).
Platelet (PLT) and serum total bilirubin (TBIL) are sensitive
indicators of inflammatory reactions in the body, and have been
proved to be with promising diagnostic values for macular
degeneration (8). It is inferred
that the combination of PLT and TBIL can also be used to improve
the diagnosis of CSC. Therefore, this study was aimed to provide a
simpler and faster diagnostic method for clinical practices through
analysis of experiments.
Patients and methods
General data
A total of 537 patients with CSC, including 294
males and 243 females with an average age of 45.5±17.8 years,
treated in the Department of Ophthalmology of Yantai Hospital of
Traditional Chinese Medicine and the Department of Ophthalmology of
Yantai Liuhuangding Hospital (Yantai, China) from June 2012 to
August 2016, were included and their clinical data were
retrospectively analyzed. At the same time, 182 routine physical
checkup people, including 103 males and 79 females with an average
age of 43.6±15.2 years, were selected as the control group. This
study was approved by the Ethics Committee of Yantai Hospital of
Traditional Chinese Medicine (Yantai, China). Signed informed
consents were obtained from the patients or guardians.
Inclusion and exclusion criteria
Inclusion criteria for CSC group: patients diagnosed
with CSC by FFA; patients without other ophthalmic diseases;
patients receiving laser photocoagulation treatment in Yantai
Hospital; patients with complete clinical data. Exclusion criteria:
patients with other cardiovascular diseases; patients with acute
infection; patients who received surgery during treatment; patients
with diseases that may affect PLT and SB; patients receiving
treatments in other hospitals during treatment. People with normal
physical conditions were included as the control group.
Grouping and methods
Venous blood (2 ml) was collected from each CSC
patient before and at day 15 after laser photocoagulation
treatment. Blood samples were collected by using anticoagulant and
common tubes, respectively. Blood in anticoagulant tubes was used
for blood routine test by using BC-6800 automatic hematology
analyzer (Shenzhen Mindray Bio-Medical Electronics Co., Ltd.,
Shenzhen, China). Blood in common tubes was kept at room
temperature for ~10–15 min, followed by centrifugation at at 3,250
× g for 5 min to collect serum samples. Serum samples were
subjected to biochemistry test by using ES-408 automatic
biochemistry analyzer (E-LAB Biological Science & Technology
Co., Ltd., Nanjing, China). PLT and biochemistry TBIL counts were
recorded and compared between CSC and control groups.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
23.0 software (IBM Corp., Armonk, NY, USA) was used for data
analysis. Regression analysis and receiver operating characteristic
(ROC) curve analysis were also conducted to study the values of PLT
and TBIL in the diagnosis of CSC. Measurement data were expressed
as mean ± standard deviation (SD), and comparisons between the two
groups were performed by t-test. Enumeration data were expressed as
rate, and comparisons between the two groups were performed by
Chi-square test. Correlation analysis was performed by using the
logistic regression analysis. Student's t-test was used for
comparing the variables before and after treatment. P<0.05
indicated that the difference was statistically significant.
Results
Clinical data of patients
The clinical data of patients were compared, and the
results showed no significant differences in sex, age, smoking,
drinking, exercise and sleep, degree of education, place of
residence, myopia or hyperopia between the two groups (p>0.05)
(Table I).
 | Table I.Clinical data of patients [n (%)]. |
Table I.
Clinical data of patients [n (%)].
| Variables | CSC group
(n=537) | Control group
(n=182) | P-value |
|---|
| Sex |
| Male | 294 (54.7) | 103 (56.6) | 0.324 |
|
Female | 243 (45.3) | 79
(43.4) |
|
| Age (years) |
|
<55 | 304 (56.6) | 96
(52.7) | 0.287 |
| ≥55 | 233 (43.4) | 86
(47.3) |
|
| Smoking history |
| Yes | 221 (41.2) | 70
(38.5) | 0.256 |
| No | 316 (58.8) | 112 (61.5) |
|
| Drinking |
| Yes | 153 (28.5) | 61
(33.5) | 0.463 |
| No | 384 (71.5) | 121 (66.5) |
|
| Exercise habit |
| Yes | 318 (59.2) | 74
(40.7) | 0.312 |
| No | 219 (40.8) | 108 (59.3) |
|
| Sleeping habit |
| Early to
bed | 314 (58.5) | 94
(51.6) | 0.342 |
| Late to
bed | 223 (41.5) | 88
(48.4) |
|
| Myopia or
hyperopia |
| Yes | 167 (31.1) | 78
(42.9) | 0.263 |
| No | 370 (68.9) | 104 (57.1) |
|
| Degree of
education |
| <
senior middle school | 267 (49.7) | 87
(47.8) | 0.527 |
| ≥ senior
middle school | 270 (50.3) | 95
(52.2) |
|
| Place of
residence |
| City | 294 (54.7) | 116 (63.7) | 0.416 |
|
Countryside | 243 (45.3) | 66
(36.3) |
|
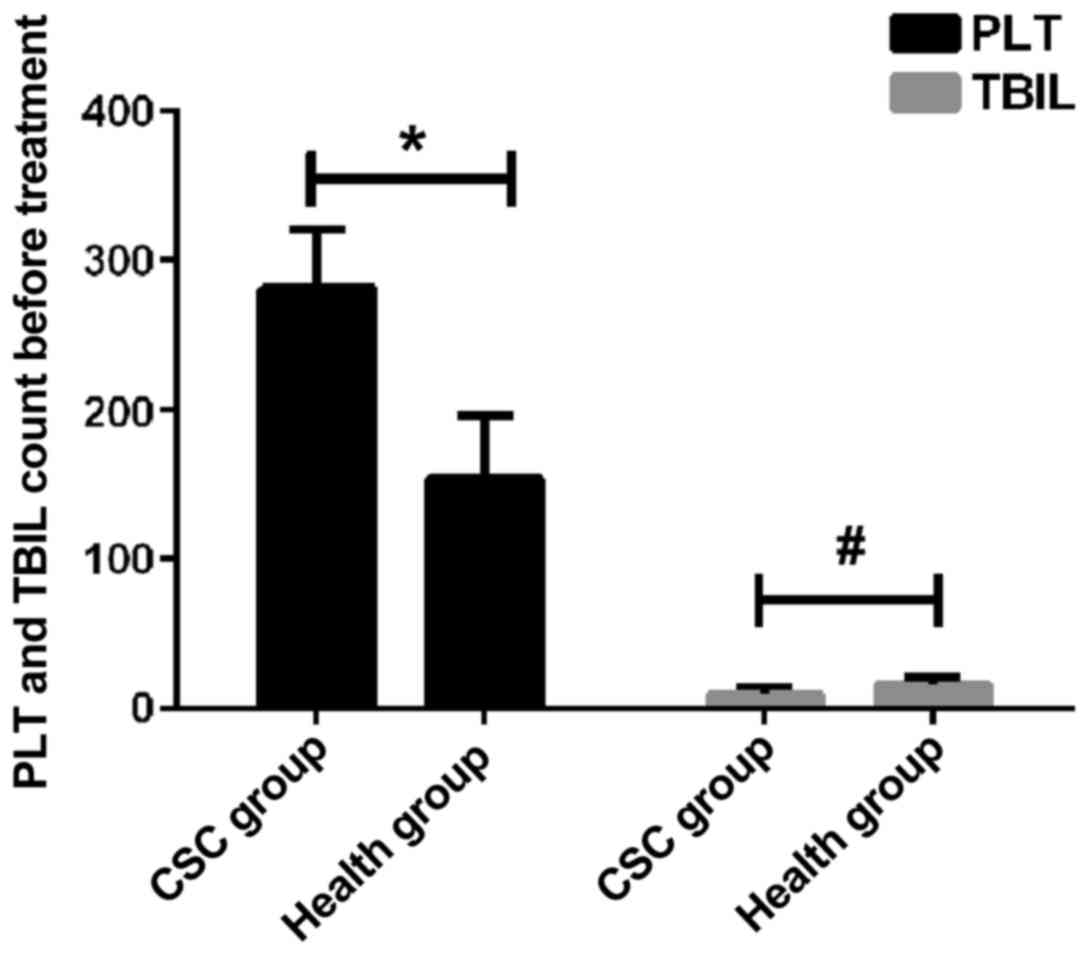
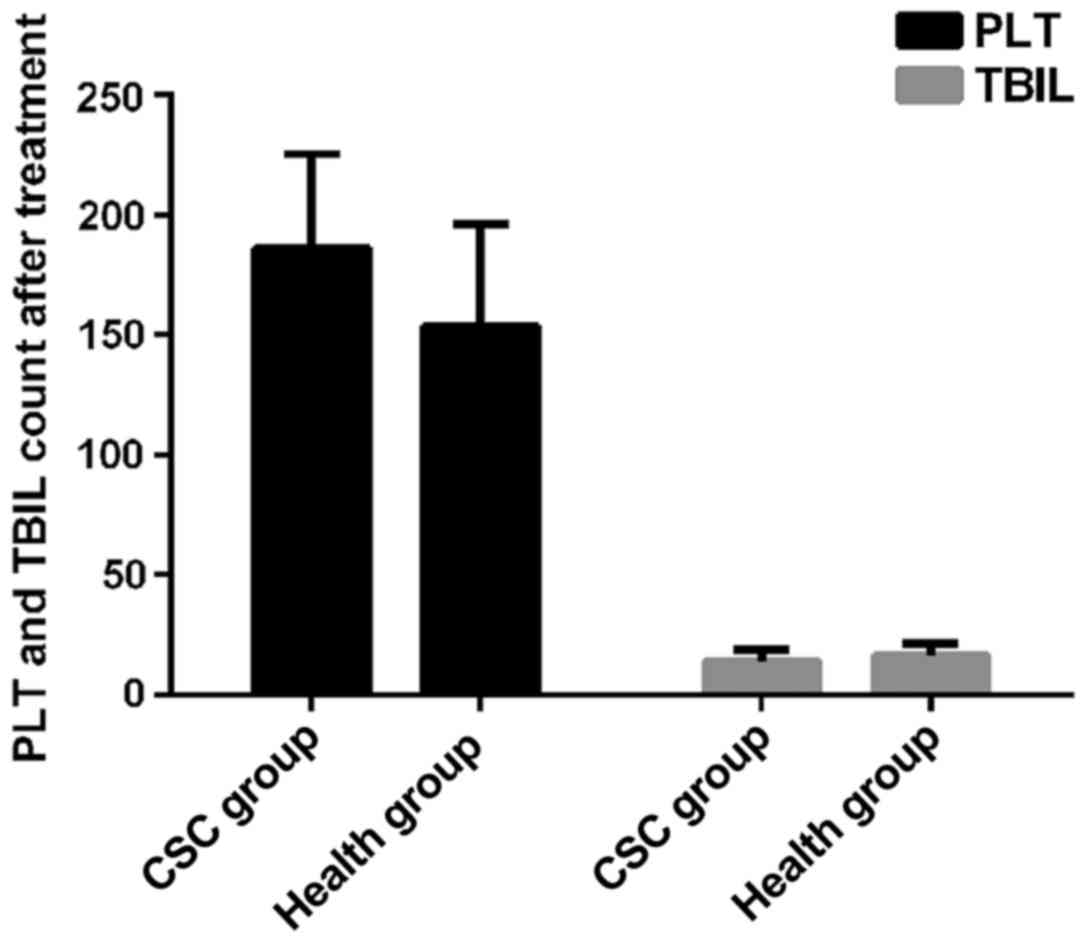
PLT and TBIL counts of patients before
and after treatment
PLT count of CSC group before treatment was
(280.79±39.68) ×109/l, which was significantly higher
than that of the control group (153.52±42.62) ×109/l,
(p<0.05). TBIL count in CSC group was 9.16±5.13 µmol/l, which
was significantly lower than that in the control group, 16.24±4.64
µmol/l (p<0.01). After treatment, PLT and TBIL in CSC group were
(185.83±39.58) ×109/l and 13.88±4.65 µmol/l,
respectively, and no significant differences were found between CSC
and the control group (p>0.05) (Figs.
1 and 2).
Association of PLT and TBIL with
CSC
Logistic regression analyses showed that PLT was a
risk factor for CSC, and TBIL was a protective factor for CSC
(Table II).
 | Table II.Logistic regression analyses on PLT
and TBIL. |
Table II.
Logistic regression analyses on PLT
and TBIL.
| Groups | Association
coefficient | Relative risk
value | 95% CI | P-value |
|---|
| PLT | 0.241 | 1.209 | 1.062–1.124 | 0.023 |
| TBIL | −0.154 | 0.919 | 0.876–0.943 | 0.019 |
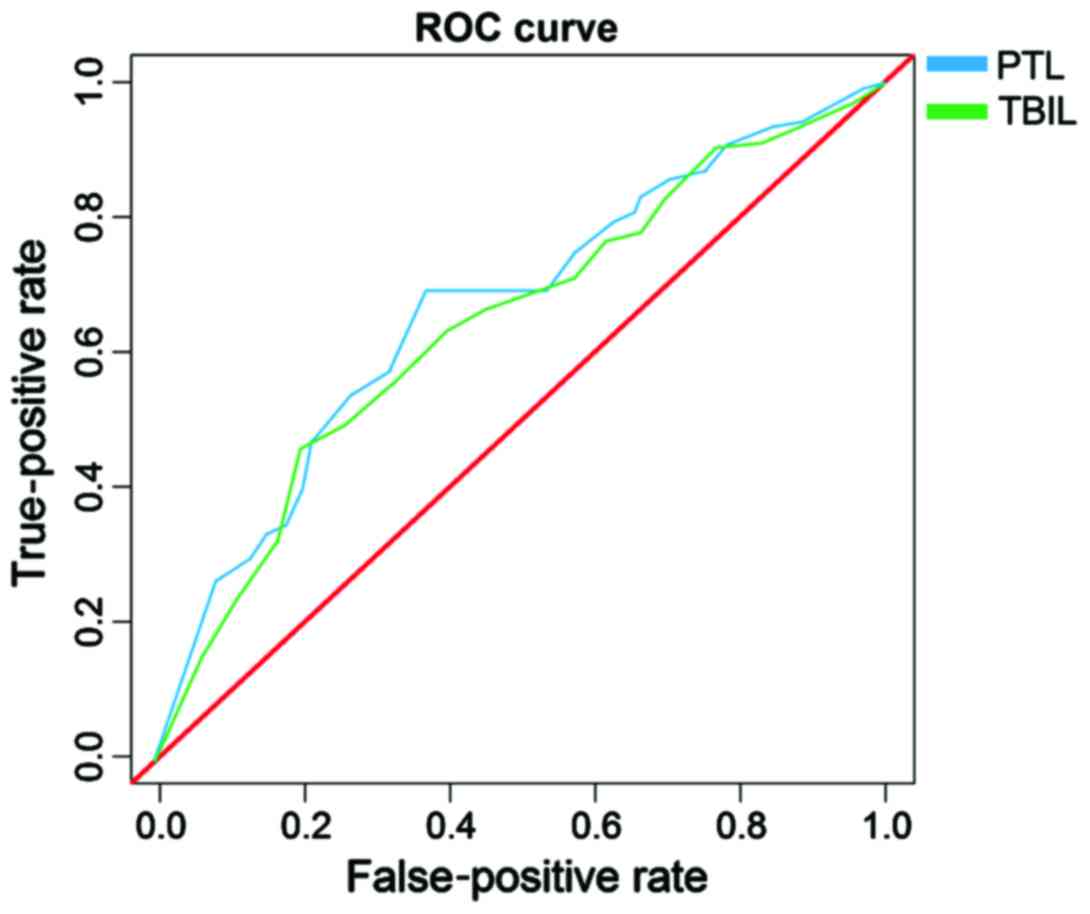
ROC curve analysis
Areas under the curve of PLT and TBIL were 0.728
(95% CI, 0.629–0.779) and 0.693 (95% CI, 0.614–0.757),
respectively; the sensitivity and specificity of PLT were 75.2 and
65.8%, respectively, in the diagnosis of CSC, and the sensitivity
and specificity of TBIL in the diagnosis of CSC were 72.7 and
63.3%, respectively (Fig. 3).
Discussion
CSC is caused by the failure of barrier function of
posterior retina pigment epithelium (RPE), which can lead to serous
RPE or neural retinal detachment (9). Pathological manifestations of CSC
include leakage of pigment epithelium, and serous retinal
detachment. As CSC has the possibility of self-healing, patients
will improve by themselves within 4–6 months after acute onset.
However, most self-healing patients may develop recurrent disease,
and some patients, once the disease recurs, may have a
significantly prolonged disease course and even suffer from
permanent relative scotoma in the center of retina and eyeball
distortion. In serious cases, blindness can occur (10,11). As
CSC has the possibility of self-healing, oral drugs such as
Acetazolamide, Mifepristone, Aspirin and Finasteride are often used
in the clinical treatment as adjuvant therapy to shorten the course
of disease without affecting vision and recurrence. Yet there are
still a small number of patients ending with delayed healing or
aggravation (12,13). Laser photocoagulation treatment is a
surgical therapy to coagulate RPE leakage point through the thermal
effect of the laser based on the RPE leakage point after FFA
examination, and it is the most effective and stable method in the
clinical treatment of CSC at present (14). Laser photocoagulation treatment can
shorten the course of disease, decrease recurrence rate, and
benefit the recovery of patients' visual acuity with a
postoperative recovery period of 2–4 weeks. Thus, it is necessary
to select proper treatment according to patients' individual
situation and willingness to clinical treatment.
In clinical practice, imaging methods such as FFA,
central serous ICGA and OCT are mainly used in the diagnosis of CSC
(15). FFA is very useful for the
detection of classic RPE leakage points, and it is also the most
common method; ICGA can show the dilation and leakage of choroidal
vessels in lesion area; OCT has outstanding performance in the
detection of posterior serous retinal detachment (16,17). It
has high accuracy rate of FFA in diagnosis, but detection time is
too long and the cost is high, and it may also cause some damage to
patient's retina. CSC has little effect on first-episode patients
and is easy to treat, so that most patients were diagnosed by the
combination of clinical symptoms, manifestations and visual
conditions. As a very common inflammatory marker, PLT can
sensitively reflect any obvious inflammatory response in the body
(18,19). TBIL as a natural antioxidant in the
human body and is highly sensitive to oxidative stress (20). Detection of PLT and TBIL is extremely
convenient, detection time is short, and patients have less injury.
Therefore, PLT and TBIL are commonly used in early detection of
some inflammatory diseases. However, the use of PLT and TBIL in the
diagnosis of CSC still has not been reported. This report aimed to
investigate the expression levels of PLT and TBIL in CSC patients
and find the differences from healthy individuals to analyze the
values of PLT and TBIL in the diagnosis of CSC, thus to provide a
simpler, faster and more economical diagnostic method for clinical
practice.
Comparison of clinical data of patients showed no
significant differences in sex, age, smoking and drinking, exercise
and sleep, degree of education, place of residence, myopia or
hyperopia between the two groups. PLT in CSC patients was
significantly higher than that in the control group, while TBIL was
significantly lower in CSC patients than in the control group.
However, these two indexes in patients recovered to normal levels
after receiving laser photocoagulation treatment. As an
antioxidant, bilirubin is synthesized in human body. Bilirubin has
the functions of anti-inflammation, anti-injury and antioxidative
stress. In addition, bilirubin plays a vital role in maintaining
normal metabolism of low-density lipoprotein lipid (21). Resonance double-bond system
originally existing in bilirubin molecule can promote indirect
bilirubin to absorb oxygen free radicals and its asymmetric
combination with serum protein molecule can allow the hydrogen to
be converted into active hydrogen atom (22). Thus, when direct bilirubin (DBIL)
level decreases, oxidation resistance will decline and retinal cell
metabolism will be disrupted due to oxidation, which results in
function barrier, eventually leading to the occurrence of CSC.
Therefore, TBIL is a protective factor for CSC. PLT, as a kind of
pluripotent cell, has the features of adhesion, aggregation and
contraction, which plays an important role in the expedite
circulation of blood (23). With the
stimulation caused by retinal microangiopathy and basement membrane
thickening of capillaries, CSC patients are in a hypercoagulable
state. In addition, with the activation and release of excessive
PLT, which will be accumulated in blood vessels, microthrombosis
will occur and the injury of vascular endothelium and ischemia or
anoxia will be exacerbated (24).
The more severe CSC is, the stronger the PLT activation will be,
which will form a vicious circle, eventually leading to
angionecrosis or even blindness. Therefore, PLT is a risk factor
for CSC. The results of ROC curve indicated that when the optimal
critical value was 124.3, and the sensitivity of PLT and TBIL in
the diagnosis of CSC were 75.2 and 72.7%, respectively, and the
specificity of PLT and TBIL were 65.8 and 63.3%, respectively,
suggesting that PLT and TBIL can be used in the clinical diagnosis
of CSC.
Few studies on the effects of TBIL on the
pathogenesis of CSC have been reported, therefore, further and more
detailed studies on the involvement of TBIL in CSC are needed. In
addition, studies are also needed to investigate the associations
between the expression of PLT and TBIL with different types as well
as different length of disease courses.
In conclusion, PLT in CSC patients was significantly
higher than that in the control group, but TBIL in CSC patients is
lower than that in the control group. However, they both gradually
recovered to normal levels after treatment. Therefore, PTL and TBIL
may serve as diagnostic indicators for CSC in the future.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
QZ and WW designed the study and performed the
experiments. CD and WW collected the data. QZ and CD analyzed the
data. QZ and WW prepared the manuscript. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yantai Hospital of Traditional Chinese Medicine (Yantai, China).
Signed informed consents were obtained from the patients or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Schachat AP: Ophthalmology retina.
Ophthalmol Retina. 1:22017. View Article : Google Scholar
|
|
2
|
Ding H, Smith RG, Poleg-Polsky A, Diamond
JS and Briggman KL: Species-specific wiring for direction
selectivity in the mammalian retina. Nature. 535:105–110. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vecino E, Rodriguez FD, Ruzafa N, Pereiro
X and Sharma SC: Glia-neuron interactions in the mammalian retina.
Prog Retin Eye Res. 51:1–40. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tan SM, Deliyanti D, Figgett WA, Talia DM,
de Haan JB and Wilkinson-Berka JL: Ebselen by modulating oxidative
stress improves hypoxia-induced macroglial Müller cell and vascular
injury in the retina. Exp Eye Res. 136:1–8. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lin J and Chen RWS: Central serous
chorioretinopathyManual of Retinal Diseases. Medina CA, Townsend JH
and Singh AD: 1st edition. Springer International Publishing; Cham:
pp. 421–426. 2016, View Article : Google Scholar
|
|
6
|
Lavinsky D and Palanker D: Nondamaging
photothermal therapy for the retina: Initial clinical experience
with chronic central serous retinopathy. Retina. 35:213–222. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Breukink MB, den Hollander AI, Keunen JE,
Boon CJ and Hoyng CB: The use of eplerenone in therapy-resistant
chronic central serous chorioretinopathy. Acta Ophthalmol.
92:e488–e490. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Keles S, Ates O, Kartal B, Alp HH, Ekinci
M, Ceylan E, Ondas O, Arpali E, Dogan S, Yildirim K, et al:
Evaluation of cardiovascular biomarkers in patients with
age-related wet macular degeneration. Clin Ophthalmol. 8:1573–1578.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yau G, Almeida DRP, Chin EK and Park SS:
Acquired macular disordersHandbook of Vitreo-Retinal Disorder
Management: A Practical Reference Guide. Park SS: 1st edition.
World Scientific Publishing Co.; Singapore: pp. 31–70. 2015
|
|
10
|
Marcuson J and Thomas R: Central serous
chorioretinopathy. Optometry. 79:241–251. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liegl R and Ulbig MW: Central serous
chorioretinopathy. Ophthalmologica. 232:65–76. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wolf S and Wolf-Schnurrbusch U:
Spectral-domain optical coherence tomography use in macular
diseases: A review. Ophthalmologica. 224:333–340. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Daruich A, Matet A, Dirani A, Bousquet E,
Zhao M, Farman N, Jaisser F and Behar-Cohen F: Central serous
chorioretinopathy: Recent findings and new physiopathology
hypothesis. Prog Retin Eye Res. 48:82–118. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lim JW, Kang SW, Kim YT, Chung SE and Lee
SW: Comparative study of patients with central serous
chorioretinopathy undergoing focal laser photocoagulation or
photodynamic therapy. Br J Ophthalmol. 95:514–517. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Costanzo E, Cohen SY, Miere A, Querques G,
Capuano V, Semoun O, El Ameen A, Oubraham H and Souied EH: Optical
coherence tomography angiography in central serous
chorioretinopathy. J Ophthalmol. 2015:1347832015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Maftouhi Quaranta-El M, El Maftouhi A and
Eandi CM: Chronic central serous chorioretinopathy imaged by
optical coherence tomographic angiography. Am J Ophthalmol.
160(581–587): e12015.
|
|
17
|
McClintic SM, Jia Y, Huang D and Bailey
ST: Optical coherence tomographic angiography of choroidal
neovascularization associated with central serous
chorioretinopathy. JAMA Ophthalmol. 133:1212–1214. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Herrera Siklódy C, Arentz T, Minners J,
Jesel L, Stratz C, Valina CM, Weber R, Kalusche D, Toti F, Morel O,
et al: Cellular damage, platelet activation, and inflammatory
response after pulmonary vein isolation: A randomized study
comparing radiofrequency ablation with cryoablation. Heart Rhythm.
9:189–196. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kaya MG, Yarlioglues M, Gunebakmaz O,
Gunturk E, Inanc T, Dogan A, Kalay N and Topsakal R: Platelet
activation and inflammatory response in patients with non-dipper
hypertension. Atherosclerosis. 209:278–282. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hileman C, Longenecker C, Carman T, Milne
G, Labbato DE, Storer Nj, White C and McComsey G: Relationship
between total bilirubin and endothelial function, inflammation and
oxidative stress in HIV-infected adults on stable antiretroviral
therapy. HIV Med. 13:609–616. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Akboga MK, Canpolat U, Sahinarslan A,
Alsancak Y, Nurkoc S, Aras D, Aydogdu S and Abaci A: Association of
serum total bilirubin level with severity of coronary
atherosclerosis is linked to systemic inflammation.
Atherosclerosis. 240:110–114. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liao SL: The role of bilirubin and
phototherapy in the oxidative/antioxidant balance. Pediatr
Neonatol. 56:77–78. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Widowati W, Herlina T, Ratnawati H, Mozef
T and Immanuel V: Potency of antioxidant, anticholesterol and
platelet antiaggregation of black tea (Camelia sinensis).
Bul Littro. 22:74–83. 2011.
|
|
24
|
Sadiq MA, Hanout M, Sarwar S, Hassan M,
Agarwal A, Sepah YJ, Do DV and Nguyen QD: Platelet-derived growth
factor inhibitors: A potential therapeutic approach for ocular
neovascularization. Dev Ophthalmol. 55:310–316. 2016. View Article : Google Scholar : PubMed/NCBI
|