Introduction
Coronary atherosclerotic heart disease is the
vascular occlusion after coronary atherosclerosis, which is caused
by external factors. Vascular cavity narrowing and vascular
blockage can cause myocardial cells hypoxia, leading to myocardial
cell death (1). Recent studies have
shown that coronary artery disease (CAD) is not only caused by
vascular endothelial dysfunction, but also by vasospasm and
thrombosis (2). As important
materials with important roles in stimulating endothelial function,
levels of NO and coronary heart disease (CHD) were significantly
lower in CAD patients than in healthy people (3). Further studies on CAD showed that this
disease is mainly caused by vascular obstruction, so many diseases
such as hypertension and diabetes can cause CAD (4). Statistical analysis has showed that
vascular damage is more serious in CCP patients than in CAD
patients (5). Clinical studies have
shown that trimetazidine can improve systolic function of CCP
patients, but its effect on primary hypertension is not significant
(6). As a type of quinoline alkaloid
(7), berberine has been proven to be
able to reduce blood glucose, improve insulin resistance and reduce
blood pressure (8–10). However, the effects of trimetazidine
combined with berberine on endothelial function of patients with
CPP still have not been reported. In this study, effects of
trimetazidine combined with berberine on endothelial function of
patients with CPP were studied. This study provides theoretical and
experimental basis for further studies.
Materials and methods
General information
In this study, a total of 68 patients with CCP were
selected from July 2014 to August 2016 to serve as observation
group (all patients were diagnosed as primary hypertension for the
first time, and all patients were willing to participate in this
study). The patients included 36 males and 32 females with an
average age of 65.3±7.3 years. At the same time, a total of 68
healthy people were also selected to serve as control group.
Control group included 36 males and 32 females with an average age
of 66.1±7.9 years. No significant differences in age were found
between two groups. All patients signed informed consent, and this
study was approved by the Ethics Committee of Beijing Chaoyang
Hospital (Beijing, China).
Inclusion criteria: Patients met the diagnostic
criteria of CAD through coronary angiography and primary
hypertension by monitoring of blood pressure: systolic pressure
≥140 mmHg and/or diastolic pressure ≥90 mmHg.
Exclusion criteria: i) Patients with
hypertriglyceridemia; ii) patients with other forms of
hypertension: renal hypertension, aldosteronism and
pheochromocytoma; iii) patients with CAD combined with
hypertriglyceridemia; iv) patients with CAD combined with type 2
diabetes.
In this study, trimetazidine and berberine were
purchased from Servier (Paris, France). RNA extraction kit was
purchased from Axygen (Shanghai, China). RT-PCR kit was purchased
from Takara Biotechnology Co., Ltd. (Dalian, China). NO
determination kit was purchased from Sangon (Shanghai, China). FMD
was measured by Siemens ACUSON Antares Color Doppler Ultrasound
Diagnostic System. RT-PCR instrument (StepOne Plus) was from Thermo
Fisher Scientific, Inc. (Waltham, MA, USA). Automatic biochemical
analyzer (LX-20) was purchased from Beckman Coulter, Inc., (Brea,
CA, USA). All other reagents and supplies were from Zhejiang Baorui
Pharmaceutical Co., Ltd. (Zhejiang, China).
Sample collection
Elbow vein blood (5 ml) was extracted from each
participant of both observation and control groups, and 2 ml blood
was used to determine the content of NO in plasma, and the other 3
ml was used for RNA extraction to determine the expression of eNOS
mRNA.
RT-PCR
Total RNA was extracted from blood samples of both
control and observation groups using RNA extraction kit. The
expression of eNOS mRNA in different samples was determined by
RT-PCR kit. Primers are shown in Table
I.
 | Table I.Primers used in PCR reaction. |
Table I.
Primers used in PCR reaction.
| Name | Primer sequences |
|---|
| eNOS | F:
CGATGCTAGCTAGCTATACGATC |
|
| R:
ATGCTGAGCTGATAGCATCGATG |
| ACT | F:
TGAGGCTAGCTAGAGATAGTC |
|
| R:
CTGGATGCTCAGCTAGATTAGCTC |
Determination of NO in plasma
In this study, 5 ml of fasting elbow vein blood was
collected from each participant of observation and control groups.
NO content in the blood of the control and observation groups was
determined by nitric acid reductase method. Nitric acid reductase
first reduced NO3− to
NO2−, and then NO content in each sample was
determined by an automated biochemical analyzer (11).
Brachial artery flow-mediated
vasodilation (FMD) determination
Brachial artery of observation and control groups
was ultrasonically detected by Siemens ACUSON Antares color Doppler
ultrasound system. Inside diameter of brachial artery was measured
(D1), and the artery was compressed with a sphygmomanometer, and
inside diameter of brachial artery was measured again (D2). FMD of
each participant was calculated according to the following formula:
FMD = (D2-D1)/D1 × 100% (12).
Statistical analysis
All data in this study were processed by SPSS 20.0
software (Applied Biosystems, Foster City, CA, USA). Data were
expressed as (mean ± SD) and processed with F-test. Differences
between the before treatment and the after treatment groups were
compared using a paired Student's t-test, while differences between
the control and observation groups were compared using a Student's
t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Relative expression level of eNOS mRNA
in CCP patients and healthy people
Relative expression of eNOS mRNA in control group
and observation group (before treatment) was determined by RT-PCR.
As shown in Fig. 1, compared with
control group, expression level of eNOS mRNA in CCP patients was
significantly decreased (P<0.05).
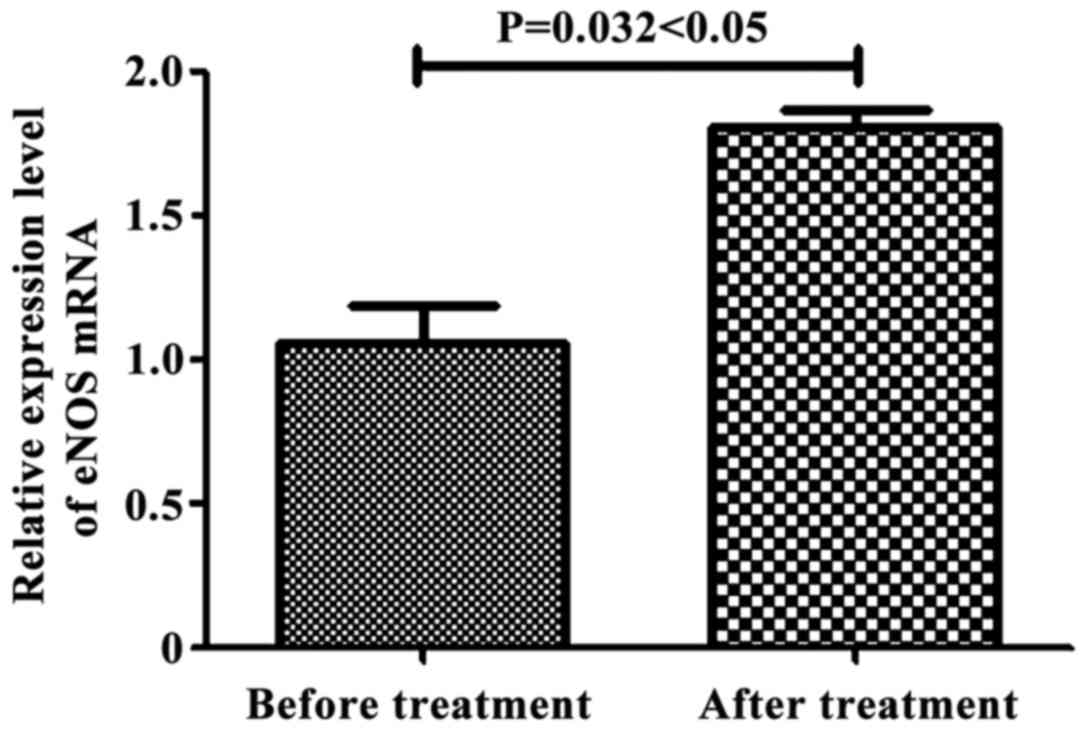
Expression of eNOS mRNA in CCP
patients before and after treatment
Expression of eNOS mRNA in observation group was
measured by RT-PCR before and after treatment. As shown in Fig. 2, after treatment with trimetazidine
and berberine, expression level of eNOS mRNA in CCP patients was
significantly increased (P<0.05), indicating that trimetazidine
combined with berberine can significantly increase the expression
of eNOS mRNA.
NO content in blood of CCP patients
and healthy people
Levels of NO in the plasma of the observation group
and control group were measured by nitric acid reductase method. As
shown in Fig. 3, NO content in blood
of CCP patients was significantly lower than that in blood of
healthy people (P<0.05). Those results were consistent with the
expression pattern of eNOS mRNA in CCP patients and healthy people
(Table II).
 | Table II.Statistical analysis of NO content in
blood of CCP patients and healthy people. |
Table II.
Statistical analysis of NO content in
blood of CCP patients and healthy people.
| Groups | Sum of squares | Mean square | F | P-value |
|---|
| Between groups | 4786.080 | 4786.080 | 3985.631 | 0.027 |
| Within a group | 135.694 | 1.201 |
|
|
| Total | 4921.774 |
|
|
|
NO content in blood of CCP patients
before and after treatment
NO content in blood of the observation group was
measured by nitric acid reductase method. As shown in Fig. 4, NO content in blood of observation
group was significantly increased after treatment, and showed no
significant difference to that of healthy people 53.28±3.09 mol/l
(P<0.05).
After treatment with trimetazidine and berberine,
content of NO in the blood of observation group was increased to
50.75±2.57 mol/l, which is significantly higher than the level
before treatment 41.06±3.63 mol/l (P=0.021<0.05, F=3582.628,
t=0.01342) (Table III).
 | Table III.Statistical analysis of NO content in
blood of patients with CCP before and after treatment. |
Table III.
Statistical analysis of NO content in
blood of patients with CCP before and after treatment.
| Groups | Sum of squares | Mean square | F | P-value |
|---|
| Between groups | 4894.294 | 4894.294 | 3582.628 | 0.021 |
| Within a group | 154.637 | 1.31 |
|
|
| Total | 4483.094 |
|
|
|
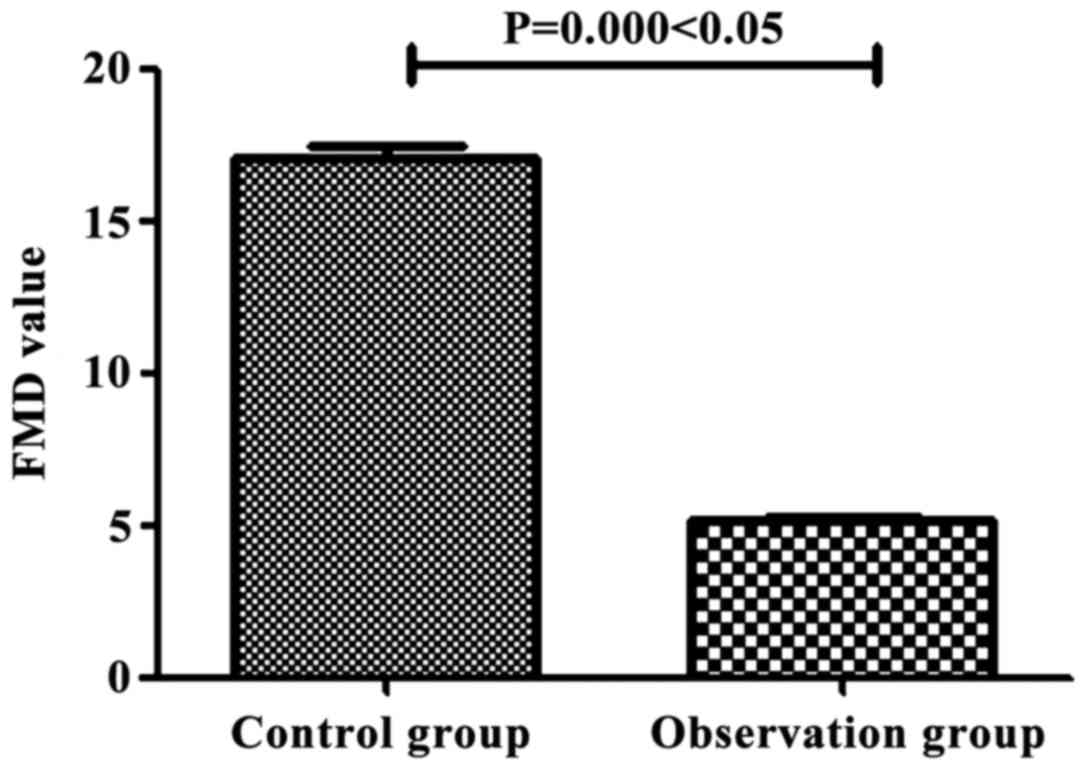
Determination of FMD value in CCP
patients and healthy people
FMD values of control group and observation group
were determined by the Siemens ACUSON Antares color Doppler
ultrasound system. As shown in Fig.
5, FMD value in CCP patients (5.03±0.95) was significantly
lower than that of healthy people (16.04±1.63) (P<0.05).
Determination of FMD in patients with
CCP before and after treatment
FMD value of CCP patients was determined after
treatment with tricamazepine and berberine. As shown in Fig. 6, FMD value of CCP patients was
significantly increased to 14.02±2.39 after treatment with
tricamazepine and berberine, which was significantly increased by
63.21±0.35% (P<0.05), indicating that tricamazepine combined
with berberine can significantly improve endothelial function of
patients with CCP.
Discussion
With the progress in the study of CAD, various
factors including poor diet structure, irregular schedule and other
factors can all contribute to the development of CAD to certain
extent (13). Clinical studies have
shown that (14), hypertension,
hyperlipoidemia, smoking and diabetes are the major causing factors
of CAD, but the mechanism is still unknown. At present, many
researchers believe that (15), as
the main factor in the incidence of CAD, vascular diameter
narrowing is now considered to be a direct cause of CAD, and
vascular diameter narrowing is mainly caused by vascular
endothelial cell telescopic dysfunction. As the barrier between
blood and blood vessels, vascular endothelial cells can sense blood
pressure, trace elements, and signaling substances in blood
(16). For example, a study has
shown that (17), vascular
endothelial cell relaxation factor, as a major cofactor in
promoting vasodilatation, plays pivotal roles in regulating the
relaxation and contraction of vascular endothelial cells. It has
been reported that vasodilator factor is mainly composed of NO and
other small molecules (18). After
entering vascular endothelial cells, NO and other small molecules
can activate intracellular gene expression, which in turn stimulate
relaxation and contraction of vascular endothelial cells. Studies
have found that (19) the increased
intravascular pressure can lead to the increased NO content in
blood, which in turn promote endothelial cell relaxation, and
increase the diameter of the blood vessels. However, NO content in
blood of CCP patients was significantly lower than that in blood of
healthy people. Those finding suggested that the reduced NO content
in blood of CCP patients can lead to vasodilatation dysfunction,
and eventually cause vasospasm or even the formation of
thrombosis.
Clinical studies have shown that (20), trimetazidine can improve CAD, but its
effects on primary hypertension is not significant, while berberine
can be used to effectively treat primary hypertension. This study
first combined the 2 drugs and we found that the combined treatment
is superior to the treatment with single drug, which is the novelty
of this study. In this study, trimetazidine and berberine were used
to treat patients with CCP. We found that trimetazidine and
berberine can significantly increase the expression level of NO
synthesis gene eNOS and increased the level of NO. As an important
factor in promoting the relaxation of vascular endothelial cells,
elevated NO content can increase FMD value. The data suggest that
trimetazidine combined with berberine has good therapeutic effect
in the treatment of CCP.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ and HN collected and analyzed the general
information of patients. HZ and XY performed RT-PCR. JC determined
NO in plasma. XW and XY extracted RNA. HZ was responsible for
brachial artery flow-mediated vasodilation determination. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Beijing Chaoyang Hospital (Beijing, China), and all patients signed
informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ma X, Liu H, Foyil SR, Godar RJ,
Weinheimer CJ, Hill JA and Diwan A: Impaired autophagosome
clearance contributes to cardiomyocyte death in
ischemia/reperfusion injury. Circulation. 125:3170–3181. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peng L, Zhuang X, Liao L, He X, Li J, Chen
X, Lu G, Ma H and Gao X: Changes in cell autophagy and apoptosis
during age-related left ventricular remodeling in mice and their
potential mechanisms. Biochem Biophys Res Commun. 430:822–826.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee G, Ramirez CN, Kim H, Zeltner N, Liu
B, Radu C, Bhinder B, Kim YJ, Choi IY, Mukherjee-Clavin B, et al:
Large-scale screening using familial dysautonomia induced
pluripotent stem cells identifies compounds that rescue IKBKAP
expression. Nat Biotechnol. 30:1244–1248. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
L'vova NV, Tupitsyna IuIu, Badalov NGL,
Krasnikov VE and Lebedeva OD: The influence of carbon dioxide baths
differing in the total mineralization levels on the functional
state of the cardiovascular system of the patients presenting with
hypertensive disease associated with coronary heart disease. Vopr
Kurortol Fizioter Lech Fiz Kult. 6:14–17. 2013.(In Russian).
|
|
5
|
Şentürk T, Çavun S, Avcı B, Yermezler A,
Serdar Z and Savcı V: Effective inhibition of cardiomyocyte
apoptosis through the combination of trimetazidine and
N-acetylcysteine in a rat model of myocardial ischemia and
reperfusion injury. Atherosclerosis. 237:760–766. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yamashita K, Kondo T, Muramatsu T,
Matsushita K, Nagahiro T, Maeda K, Shintani S and Murohara T:
Effects of valsartan versus amlodipine in diabetic hypertensive
patients with or without previous cardiovascular disease. Am J
Cardiol. 112:1750–1756. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ussher JR, Jaswal JS and Lopaschuk GD:
Pyridine nucleotide regulation of cardiac intermediary metabolism.
Circ Res. 111:628–641. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Egan BM, Zhao Y, Li J, Brzezinski WA,
Todoran TM, Brook RD and Calhoun DA and Calhoun DA: Prevalence of
optimal treatment regimens in patients with apparent
treatment-resistant hypertension based on office blood pressure in
a community-based practice network. Hypertension. 62:691–697. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dedkova EN, Seidlmayer LK and Blatter LA:
Mitochondria-mediated cardioprotection by trimetazidine in rabbit
heart failure. J Mol Cell Cardiol. 59:41–54. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lopez-Jaramillo P, Lopez-Lopez J,
Lopez-Lopez C and Rodriguez-Alvarez MI: The goal of blood pressure
in the hypertensive patient with diabetes is defined: Now the
challenge is go from recommendations to practice. Diabetol Metab
Syndr. 6:312014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Al-Shabanah OA, Aleisa AM, Hafez MM,
Al-Rejaie SS, Al-Yahya AA, Bakheet SA, Al-Harbi MM and Sayed-Ahmed
MM: Desferrioxamine attenuates doxorubicin-induced acute
cardiotoxicity through TFG-β/Smad p53 pathway in rat model. Oxid
Med Cell Longev. 2012:6191852012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roĭtberg GE, Artamonova EA and Ushakova
TI: State of the brachial artery wall in patients with and without
metabolic syndrome. Angiol Sosud Khir. 12:23–27. 2006.(In Russian).
PubMed/NCBI
|
|
13
|
Zemljic G, Bunc M and Vrtovec B:
Trimetazidine shortens QTc interval in patients with ischemic heart
failure. J Cardiovasc Pharmacol Ther. 15:31–36. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hu J, Chai Y, Wang Y, Kheir MM, Li H, Yuan
Z, Wan H, Xing D, Lei F and Du L: PI3K p55γ promoter activity
enhancement is involved in the anti-apoptotic effect of berberine
against cerebral ischemia-reperfusion. Eur J Pharmacol.
674:132–142. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhou X, Li C, Xu W and Chen J:
Trimetazidine protects against smoking-induced left ventricular
remodeling via attenuating oxidative stress, apoptosis, and
inflammation. PLoS One. 7:e404242012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Soliman EZ, Lopez F, O'Neal WT, Chen LY,
Bengtson L, Zhang ZM, Loehr L, Cushman M and Alonso A: Atrial
fibrillation and risk of ST-segment-elevation versus
non-ST-segment-elevation myocardial infarction: The Atherosclerosis
Risk in Communities (ARIC) study. Circulation. 131:1843–1850. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vitale C, Spoletini I, Malorni W,
Perrone-Filardi P, Volterrani M and Rosano GM: Efficacy of
trimetazidine on functional capacity in symptomatic patients with
stable exertional angina - the VASCO-angina study. Int J Cardiol.
168:1078–1081. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jones LW, Hornsby WE, Goetzinger A, Forbes
LM, Sherrard EL, Quist M, Lane AT, West M, Eves ND, Gradison M, et
al: Prognostic significance of functional capacity and exercise
behavior in patients with metastatic non-small cell lung cancer.
Lung Cancer. 76:248–252. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pathak RK, Middeldorp ME, Lau DH, Mehta
AB, Mahajan R, Twomey D, Alasady M, Hanley L, Antic NA, McEvoy RD,
et al: Aggressive risk factor reduction study for atrial
fibrillation and implications for the outcome of ablation: The
ARREST-AF cohort study. J Am Coll Cardiol. 64:2222–2231. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Montalescot G, Sechtem U, Achenbach S,
Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di
Mario C, et al: Document Reviewers: 2013 ESC guidelines on the
management of stable coronary artery disease: The Task Force on the
management of stable coronary artery disease of the European
Society of Cardiology. Eur Heart J. 34:2949–3003. 2013. View Article : Google Scholar : PubMed/NCBI
|