Introduction
Endoscopic retrograde cholangio-pancreatography
(ERCP) is the main method for the diagnosis and treatment of
biliary diseases, but there are still some shortcomings for this
technique. ERCP is performed under X-ray, limiting its use for
breast-feeding or pregnant women as well as immunocompromised
populations (1). ERCP cannot be used
to directly obtain pathological specimens from cholangiocarcinoma
lesions, so the diagnosis is difficult. Residual stones after ERCP
are usually observed. Choledochoscope can be used to achieve direct
vision biopsy and treatment of bile duct lesions, and plays an
important role in the diagnosis and treatment of biliary system
diseases, especially in the identification of benign and malignant
biliary strictures. The application of early oral cholecystectomy
and novel SpyGlass choledochoscopy are challenged by the tedious
operation, high costs, heavy equipment, and poor image quality
(2,3). In recent years, direct oral
cholecystoscopy (using non-specific endoscopy, ultrafine endoscopy
is usually directly inserted into the common bile duct) has
attracted increasing attention. This technique does not require
special endoscopic biliary system, and operation is simple and
image quality is high. Working aperture is large. With this
technique, clear images can be obtained and biopsy
histopathological diagnosis can be performed. Besides that,
lithotripsy, stone removal and argon coagulation can also be
performed in common bile duct. However, studies on this technique
are rare. Therefore, 55 patients were included in this study to
explore the clinical value and safety of the use of ordinary
gastroscopy or ultrafine endoscopy as oral choledochoscopy in the
treatment of biliary diseases.
Materials and methods
Clinical data
In total, 55 patients who underwent gastroscopy at
the Department of Gastroenterology, Shunde Hospital of Southern
Medical University (Foshan, China) from July 2012 to February 2018
were collected. Those patients included 26 males and 29 females,
with an average age of 65.1±12.6 years. Inclusion criteria: i)
Patients with biliary obstruction or stenosis; ii) patients with
radiographic evidence of biliary filling defects; iii) patients
with residual stone after ERCP; iv) patients with biliary
hemorrhage; v) common bile duct diameter >8 mm. Exclusion
criteria: i) Patients with bleeding tendency (INR >1.5 or
platelet count <50,000/ml); ii) patients with diffuse common
bile duct stricture; iii) patients with pancreatic and ampullary
tumors of the duodenum; iv) patients with contraindications of
ERCP.
Surgical methods
Non-X-ray ERCP: Non-X-ray ERCP technology is a type
of duodenoscopy successfully established by our department
(1). After conventional sedation,
duodenal side-view mirror (Olympus-TJF260V; Olympus Corporation,
Tokyo, Japan) was inserted to reach the lower part, and the mirror
body was removed, and the position of the nipple was adjusted to
the right center of the visual field. Clever knife intubation
(catheter was indwelled with 0.035 zebra guide wire) was performed
without the guidance of X-ray. A sudden drop in resistance or
disappearance of resistance indicates the entry of tube into
pancreaticobiliary duct. Observation of yellow-green or dark green
bile outflow after pulling back the catheter indicates the entry of
tube into common bile duct. While observation of pancreatic juice
indicates the entry of the tube into pancreatic duct, and the tube
should be pulled back and re-intubation should be performed. After
the successful intubation, guide wire was inserted into the 10-15
cm of common bile duct. Duodenal sphincterotomy (EST) and
endoscopic papillary large balloon dilation (EPLBD) were performed
according to the size of the duodenal papilla opening. Finally,
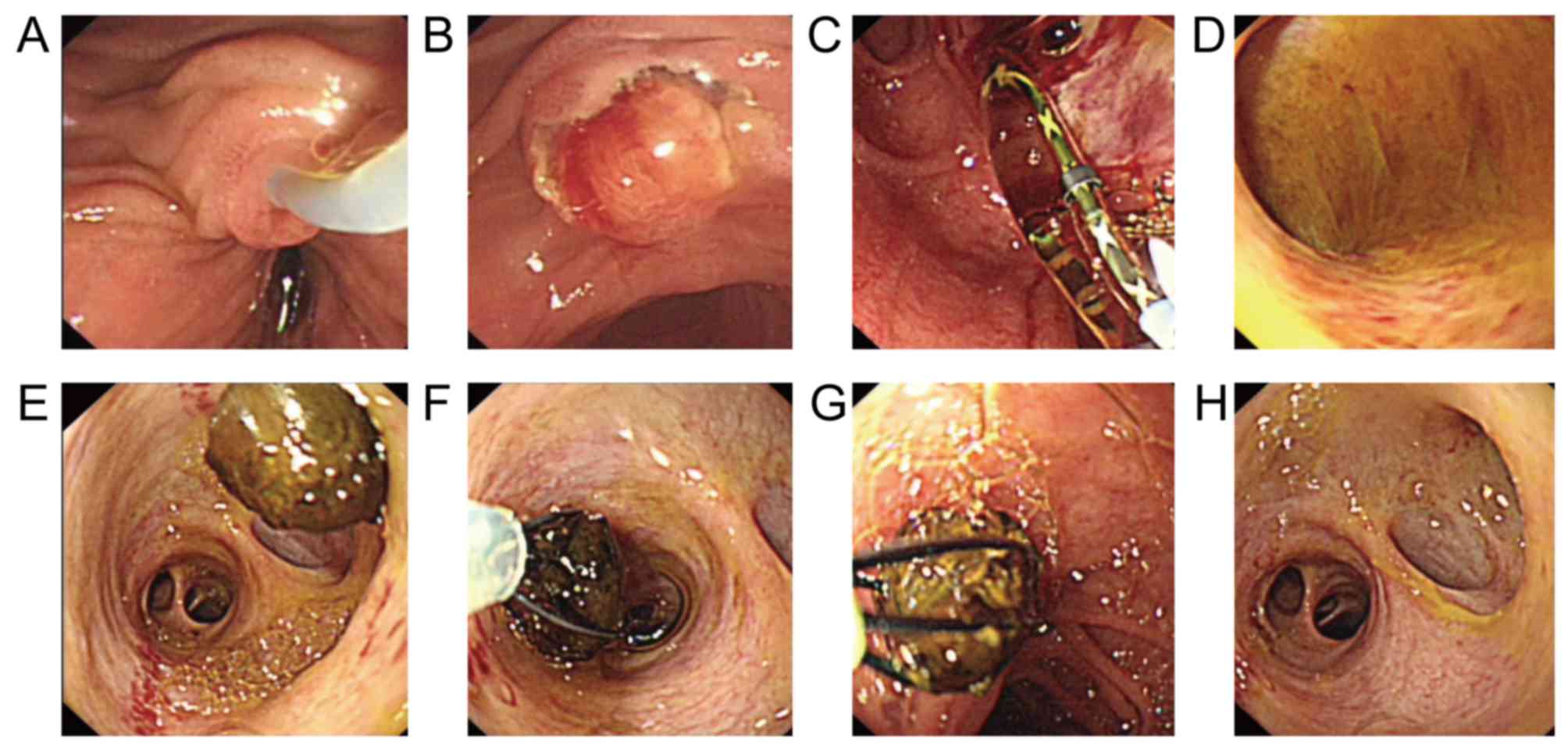
duodenoscope was removed (Fig.
1).
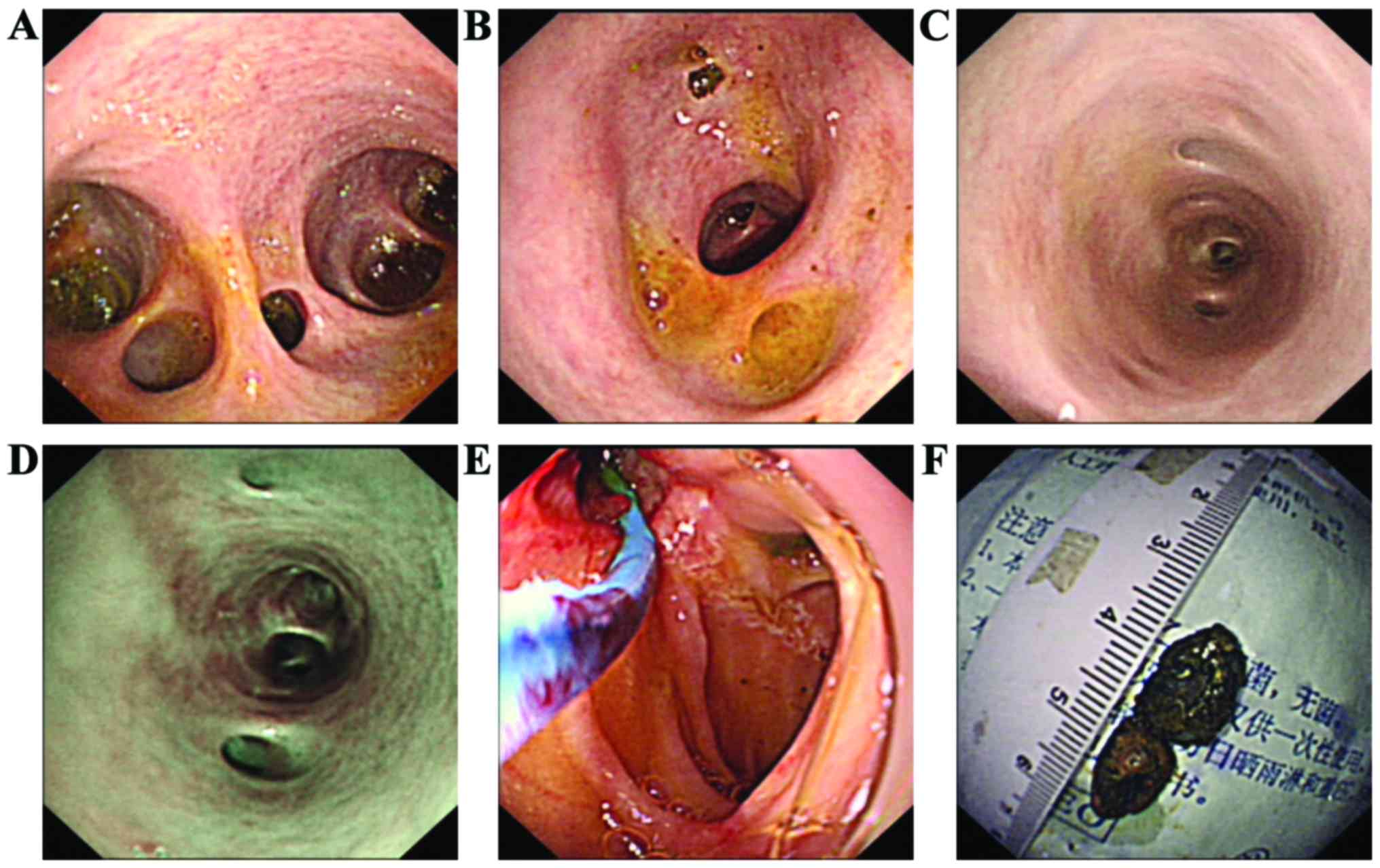
The use of gastroscopy as oral choledochoscopy to
explore the bile duct: Simple direct oral cholecystoscopy by hand
is usually performed during ERCP. Specific operation is as follows:
Conventional gastroscope (Olympus-GIF-Q260) or ultrafine
gastroscope (Olympus-GIF-XP260) was inserted along the biliary
guide wire to reach duodenal bulb and nipple. By pulling and
rotating the mirror body into the lower part of the common bile
duct, and then promoting the endoscope to the bile duct. Under
direct vision of gastroscopy, saline was used to wash out
sediment-like stones, and big stones were removed by using snare or
basket (Fig. 2). Biopsy forceps were
used for suspicious lesions of the bile duct to perform lesion
biopsy. In the event of biliary hemorrhage, argon plasma
coagulation therapy or balloon compression can be performed under
endoscopic direct vision. In the present study, endoscopic
insertion is simply hand-insertion, without the help of enteroscopy
tube, snare, balloon anchoring and other assistive technology, and
the requirements on operating skills are high. All operations were
performed by physicians who have experience in phallus and ERCP.
Types of gastroscope were decided based on the size of nipple
openings, common bile duct dilatation and other factors.
Observation indicators
Types of gastroscopy, size of duodenal papilla
incision, size of balloon dilatation, the success rate of mirror
entry, entry depth of bile duct, endoscopic diagnosis,
postoperative complications such as fever, bleeding, perforation,
high amylasemia, pancreatitis, cholecystitis and cholangitis.
Results
This study included 55 patients, and the average
diameter of the common bile duct was 17.1±7.6 mm. Among them, 12
cases (21.8%) had biliary stricture, 40 cases (72.7%) had biliary
exploration after ERCP, 1 case (1.8%) had biliary filling defect
and 2 cases (3.6%) had biliary bleeding (Table I).
 | Table I.Basic information and clinical
indications of patients. |
Table I.
Basic information and clinical
indications of patients.
| Total number of
patients (n) | 55 |
|---|
| Age (years) | 65.1±12.6 |
| Sex (n, %) |
|
| Male | 26 (47.3) |
|
Female | 29 (52.7) |
| Common bile duct
diameter (mm) (range) | 17.1±7.6 (5–45) |
| POC clinical
indications (n, %) |
|
| Bile duct
stenosis exploration | 12 (21.8) |
| ERCP postoperative
bile duct exploration | 40 (72.7) |
| Bile duct
filling defect | 1 (1.8) |
| Biliary
bleeding | 2 (3.6) |
| POC final diagnosis
(n, %) |
|
| Residual
bile duct stones after ERCP | 25 (45.5) |
| Benign
stenosis | 9 (16.4) |
| Malignant
stenosis | 2 (3.6) |
|
Cholangiocarcinoma | 3 (5.5) |
|
Duodenal papillary
cancer | 1 (1.8) |
| Biliary
bleeding | 2 (3.6) |
| No abnormalities in
biliary exploration | 13 (23.6) |
There were 46 cases of duodenal papilla incision,
including large incision in 19 cases, moderate incision in 20
cases, and small incision in 7 cases. Duodenal papillae balloon
dilatation was performed for 46 cases, including balloon diameter
≤10 mm in 5 cases, ≤14 mm in 28 cases, >14 mm in 13 cases.
Insertion into common bile duct was successfully achieved in 53
patients, and overall technical success rate was 96.4%. Among them,
gastroscopy was performed for 16 cases (29.1%) and 39 cases (70.9%)
received ultrafine gastroscopy. Insertion into the middle and lower
common bile duct was achieved in 23 cases (41.8%); insertion into
the upper common bile duct was achieved in 16 cases (29.1%);
insertion into left and right hepatic duct in 9 cases (16.4%), and
insertion into intrahepatic bile duct in 7 cases (12.7%).
Endoscopic diagnosis: Twenty-five cases (45.5%) were diagnosed with
residual bile duct stones after ERCP, and direct gastroscopic
irrigation was performed to remove appendage stones and
sediment-like stones, and big incarcerated stones were subjected to
laser lithotripsy under endoscopy or reined by snare, then smashed
and removed gradually by snare, basket or biopsy forceps. The 11
cases of bile duct stenosis included 9 cases of benign stenosis and
2 cases of malignant stenosis. Lower bile duct and duodenal
papillary biopsy were performed, and patients were diagnosed as
‘cholangiocarcinoma’ or ‘duodenal papilla well-differentiated
adenocarcinoma’. Two patients (3.6%) had hemorrhage of the biliary
tract, and balloon dilatation or argon ion coagulation was
performed under intraoperative endoscopy to stop hemostasis. No
obvious abnormalities were observed in 13 patients (23.6%) through
gastroscopic biliary exploration. Complications occurred in 15 of
them, with an incidence rate of 27.3%. Complications included 2
cases of cholangitis (3.6%), 8 cases of hyper amylase (14.6%) and 4
cases of acute pancreatitis (7.3%). All complications were cured.
One case (1.8%) of biliary perforation was observed and treated
with conservative treatment. No thrombosis, or other serious
complications were observed (Table
II).
 | Table II.Successful rate of the use of
gastroscopy as oral choledochoscopy and postoperative
complications. |
Table II.
Successful rate of the use of
gastroscopy as oral choledochoscopy and postoperative
complications.
| Overall operation
success rate (n, %) | 53 (96.4) |
|---|
| Gastroscopy type (n,
%) |
|
| Ordinary
gastroscopy | 16 (29.1) |
| Ultrafine
gastroscopy | 39 (70.9) |
| Incision size (n,
%) |
|
| Big
incision | 19 (34.5) |
| Moderate
incision | 20 (36.3) |
| Small
incision | 7 (12.7) |
| No
incision | 9 (16.5) |
| Papillary balloon
dilatation diameter (n, %) |
|
| No
dilatation | 9 (16.4) |
| ≤10
mm | 5 (9.1) |
| ≤14
mm | 28 (50.9) |
| >14
mm | 13 (23.6) |
| Positions in bile
duct (n, %) |
|
| Lower or
middle section of common bile duct | 23 (41.8) |
| Upper
section of common bile duct | 16 (29.1) |
| Left and
right hepatic duct | 9 (16.4) |
|
Intrahepatic bile duct | 7 (12.7) |
| Postoperative
complications (n, %) |
|
|
Cholangitis | 2 (3.6) |
| High
amylasemia | 8 (14.6) |
|
Pancreatitis | 4 (7.3) |
|
Perforation | 1 (1.8) |
| No
complications | 40 (72.7) |
Discussion
Compared with the early choledochoscope system,
ordinary endoscopy and ultrafine gastroscopy have the advantages of
non-specialized endoscopy, single-person operation, high-quality
biliary tract imaging and larger working aperture. The outer
diameter of ultrafine gastroscopy is only 5.9 mm, so the entry into
biliary tract can be easily achieved as long as duodenal papilla
incision is fully expanded. For patients with high common bile duct
dilatation, general gastroscopy may be a better choice. With the
use of conventional endoscopy, screening and treatment of biliary
system diseases under endoscopy can be performed through some
existing endoscopic accessories, including biopsy,
electro-hydraulic laser lithotripsy, residual stone removal, argon
ion coagulation and photodynamic therapy (4–7). In the
present study, gastroscopy was used as oral choledochoscopy in the
diagnosis of biliary diseases. Twenty-five cases (45.5%) were
diagnosed with residual bile duct stones after ERCP, and direct
gastroscopic irrigation was performed to remove sediment-like
stones, and big incarcerated stones were subjected to laser
lithotripsy under endoscopy or reined, smashed and removed by
snare. Nine cases of benign stenosis and 2 cases of malignant
stenosis were found, and patients were diagnosed as
‘cholangiocarcinoma’ or ‘duodenal papilla well-differentiated
adenocarcinoma’ by biopsy. Bleeding was stopped in 2 cases of
biliary tract hemorrhage under endoscopy. No significant
abnormalities were observed among 13 cases with suspicious residual
stones by gastroscopy biliary tract exploration. Thus, the use of
endoscopy as an endoscopic choledochoscope has great clinical value
in the diagnosis and treatment of biliary diseases.
However, it is not trivial to insert a gastroscope
into the common bile duct, especially the insertion of an ultrafine
gastroscope is more difficult. Due to the acute angle of the
duodenum and bile ducts, ultrafine gastroscopy is also difficult to
align with the nipple at the maximum bending angle. Direct
insertion is difficult, and if the nipple is not adequately incised
and expanded, the entrance of the gastroscope will be limited.
Ultrafine gastroscope mirror body is soft and can easily be bent in
stomach cavity, so that the intensity cannot be effectively
transmitted to the front end of the endoscope, so the entrance into
common bile duct or deep bile duct will be difficult. Therefore,
accessories assisted ultrafine endoscopy has been developed. Larghi
and Waxman (8) reported the use of
conventional ERCP laminectomy guidewire guided gastroscope into the
biliary duct, however, the success rate was lower than 50%. Moon
et al (9) used biliary
catheter guidewire-guided method to increase the success rate of
ultrafine endoscopy entering into biliary duct to 95%. However, in
some cases, especially in cases of diffuse biliary strictures or
significant dilatation of the bile duct, the balloon is difficult
to anchor in the bile duct. In addition, when withdrawing the
balloon catheter, the gastroscope may be displaced, and entrance
and treatment cannot be continued. Choi et al (10) introduced the earliest application of
small bowel tube assisted fixation of ultrafine gastroscope mirror
body. This technique avoided the coil of ultrafine gastroscope
mirror body in stomach and increased the successful rate of the
entry into biliary tract. However, the diameter and length of the
tube that can be used now are too large and too long compared with
the ultrafine endoscopy, and the ultrafine endoscopy is not stable
and the operation is difficult. Studies (11,12)
showed the method of snare assisted insertion, sending the upper
part of endoscope to middle or upper section of common bile duct
using fine caliber snare to tighten up the bending section of
superfine gastroscope, and the successful rate achieved 100% (8/8,
24/24). In this study, simple direct cholangiopancreatography was
used, and success rate of entering the bile duct was 96.4% (53/55),
which was similar to that reported by Kim et al (13) (5/5). Two cases of failure were caused
by the coiled ultrafine gastroscope in stomach and common bile duct
severe stenosis. Simple hand insertion technology is not assisted
by guide wire, balloon, snare, casing and other accessories, and is
limited by the controllability of endoscopy and the size of the
nipple opening. Duodenal nipple openings should be fully opened and
bile duct dilatation should also be performed to facilitate the
entrance of gastroscope. In this study, direct endoscopic
cholangioscopy was the first choice of general endoscopy in
patients with highly enlarged common bile duct, which not only
prevented the appearance of coiled mirror in the stomach cavity,
but also increased the feasibility of interventional therapy.
Previous studies in China have shown that the use of
gastroscopy as direct oral choledochoscopy was characterized with
good security, and low incidence of complications (7,14). In
this study, complications occurred in 15 cases, with an incidence
rate of 27.3%. Complications included 2 cases of cholangitis
(3.6%), 8 cases of hyper amylase (14.6%) and 4 cases of acute
pancreatitis (7.3%). All complications were cured. One case (1.8%)
of biliary perforation was observed and discharged after
conservative treatment, and it may be correlated with nipple
incision and balloon dilatation. Therefore, this also reflects the
limitations of gastroscopy as a direct choledochoscopy. Nipple
incision and expansion will inevitably increase the risk of
bleeding and perforation. At present, there is no clear standard
for indications and contraindications of direct oral
choledochoscopy. We think this technique is safe for patients with
obvious expansion of extrahepatic bile duct or those who previously
received ERCP.
Endoscopy as a direct cholangioscopy in the
diagnosis and treatment of biliary diseases has unique advantages,
especially for the treatment of stones, biliary obstruction and
bile duct cancer, which cannot be achieved by traditional ERCP.
However, there are still many operational difficulties and some
rare serious complications. The use of superfine gastroscopy,
general gastroscopy and general colonoscopy as oral choledochoscopy
each has its limitations, which limits the the popularity of the
technique to a certain extent and needs further improvement.
Therefore, research and developing a new type of oral
choledochoscope with the advantages of being fine, long, hard and
angle matching is needed to improve the safety and success
rate.
Acknowledgements
Not applicable.
Funding
This study was supported by Guangdong provincial
Science and Technology Project (2015A070707005).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SH and XL conceived and designed this study. GD and
WC collected and analyzed the data. SH were in charge of the
operation. WR was responsible for clinical design and revising the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Shunde Hospital of Southern Medical University (Foshan, China).
Signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
García-Cano J, Palomo Sánchez JC and Gómez
Ruiz CJ: ERCP without fluoroscopy in a pregnant woman with a common
bile duct stone. Rev Esp Enferm Dig. 100:100–101. 2008.(In
Spanish). PubMed/NCBI
|
|
2
|
Shim CS, Neuhaus H and Tamada K: Direct
cholangioscopy. Endoscopy. 35:752–758. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Manta R, Frazzoni M, Conigliaro R, Maccio
L, Melotti G, Dabizzi E, Bertani H, Manno M, Castellani D,
Villanacci V, et al: SpyGlass single-operator peroral
cholangioscopy in the evaluation of indeterminate biliary lesions:
A single-center, prospective, cohort study. Surg Endosc.
27:1569–1572. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lau JY, Leow CK, Fung TM, Suen BY, Yu LM,
Lai PB, Lam YH, Ng EK, Lau WY, Chung SS, et al: Cholecystectomy or
gallbladder in situ after endoscopic sphincterotomy and bile duct
stone removal in Chinese patients. Gastroenterology. 130:96–103.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cotton PB: Endoscopic management of bile
duct stones; (apples and oranges). Gut. 25:587–597. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pohl J and Ell C: Direct cholangioscopy:
New horizons for complex intraductal treatments under direct
high-resolution visualization. Gastroenterology. 144:270–271. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim HI, Moon JH, Choi HJ, Lee JC, Ahn HS,
Song AR, Lee TH, Cho YD, Park SH and Kim SJ: Holmium laser
lithotripsy under direct peroral cholangioscopy by using an
ultra-slim upper endoscope for patients with retained bile duct
stones (with video). Gastrointest Endosc. 74:1127–1132. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Larghi A and Waxman I: Endoscopic direct
cholangioscopy by using an ultra-slim upper endoscope: A
feasibility study. Gastrointest Endosc. 63:853–857. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moon JH, Ko BM, Choi HJ, Hong SJ, Cheon
YK, Cho YD, Lee JS, Lee MS and Shim CS: Intraductal balloon-guided
direct peroral cholangioscopy with an ultraslim upper endoscope
(with videos). Gastrointest Endosc. 70:297–302. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Choi HJ, Moon JH, Ko BM, Hong SJ, Koo HC,
Cheon YK, Cho YD, Lee JS, Lee MS and Shim CS:
Overtube-balloon-assisted direct peroral cholangioscopy by using an
ultra-slim upper endoscope (with videos). Gastrointest Endosc.
69:935–940. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Park JS, Kwon CI, Jeong S, Kim K, Moon JH
and Lee DH: Development of a swine bile duct dilation model using
endoclips or a detachable snare under cap-assisted endoscopy.
Gastrointest Endosc. 80:325–329. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aiura K, Imaeda H, Kitajima M and Kumai K:
Balloon-catheter-assisted endoscopic snare papillectomy for benign
tumors of the major duodenal papilla. Gastrointest Endosc.
57:743–747. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim TK, Kim BS, Kim JH, Ha HK, Kim PN, Kim
AY and Lee MG: Diagnosis of intrahepatic stones: Superiority of MR
cholangiopancreatography over endoscopic retrograde
cholangiopancreatography. AJR Am J Roentgenol. 179:429–434. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mori A, Ohashi N, Nozaki M and Yoshida A:
Feasibility of duodenal balloon-assisted direct cholangioscopy with
an ultrathin upper endoscope. Endoscopy. 44:1037–1044. 2012.
View Article : Google Scholar : PubMed/NCBI
|