Introduction
Arthroscopic anterior cruciate ligament (ACL)
reconstruction has become a primary method for the treatment of ACL
rupture (1). There are numerous
factors that may influence the success of ACL reconstruction,
including graft selection, the choice of surgical technique
(2), bone tunnel location, graft
fixation method and rehabilitation protocol. Biomechanical
properties of soft tissue grafts, represented by the levels of
viscoelasticity, serve a role in determining the long-term results
(1). Tendon grafts used in ACL
reconstruction relax and elongate due to viscoelasticity, which may
result in a postoperative decrease in the graft tension (3). Preconditioning is therefore recommended
prior to implantation, as a countermeasure to this undesired
effect, to minimize the viscoelasticity-induced graft elongation
and lower the risk of knee laxity in the postoperative period
(4–6).
Although the need for preconditioning of soft tissue
grafts has been well established, the optimal forces have not been
determined. Some investigators have suggested that 80 N or even
lower level preconditioning was enough to produce a rigid implant
and to limit postoperative knee laxity effectively (3,7–9). Others argued that increasing the
tension applied to the tendon grafts could decrease the loss of
tension and stiffness, and that the elongation could be eliminated
during the preconditioning processes (3,5,10). However, excessive pretension forces
may have a negative effect on the ultrastructure of collagen and
ligamentization of the grafts. A previous study demonstrated that a
500 N pretension force may result in loss of cohesion, integrity
and parallelism of the collagen fibrils (11). Furthermore, excessive graft tension
caused by the preconditioning process may lead to additional
intra-articular injuries, including cartilage degeneration
(12) and impairment of graft
revascularization (13). Therefore,
it is important to identify the suitable preconditioning forces for
different types of grafts.
The use of a tendon allograft, as a substitute for
an autograft, prevents donor-site complications and has been
commonly used in ACL reconstruction (14,15). The
majority of the tendon allografts receive γ-ray irradiation to kill
bacteria, viruses and other microorganisms, and to reduce the risk
of disease transmission (16).
However, the structures of irradiated tendons may change, resulting
in significant alternations in biomechanical properties (17,18). As
a soft tissue graft, the γ-irradiated tendon is characterized by
viscoelasticity. Therefore, preconditioning is also required to
maintain the biomechanical strength following implantation into the
knee. The present study was designed to analyze the impact of
different preconditioning forces on the stiffness and ultimate
failure at maximum load (UFML), and to improve the biomechanical
properties of the γ-irradiated deep frozen tendon allografts used
in ACL reconstruction.
Materials and methods
Graft preparation
All irradiated human hamstring tendon allografts
were supplied by a certified tissue bank, with policies for
serological and microbiological testing in accordance with
guidelines set by the American Association of Tissue Banks (Shanxi
OsteoRad Biomateral Co., Ltd., Taiyuan, China). All grafts were
stored frozen at −20°C for ≥6 months and were radiated with 25 kGy
cobalt-60 at room temperature for 12 h. The γ-irradiated deep
frozen tendon allografts were thawed to room temperature in 0.9%
saline solution for 15 min. Afterwards, every two of 72 frozen
tendons were matched into pairs to obtain 36 tendon grafts. The
tendon constructs were subsequently fixed on an ACL graft
preparation table and 20 mm of each free end was whipstitched with
Ethibond sutures (Ethibond Excel 1; Ethicon, Inc., Cincinnati, OH,
USA). Subsequently, the paired tendons were folded to form 4-strand
grafts with a diameter of 7±0.5 mm. The 36 paired grafts were
randomized into 3 preconditioning groups. The only difference
between the 3 testing groups was the pretension force, 80 N (group
1), 160 N (group 2) and 320 N (group 3), representing different
levels of load applied to the grafts.
Biomechanical testing
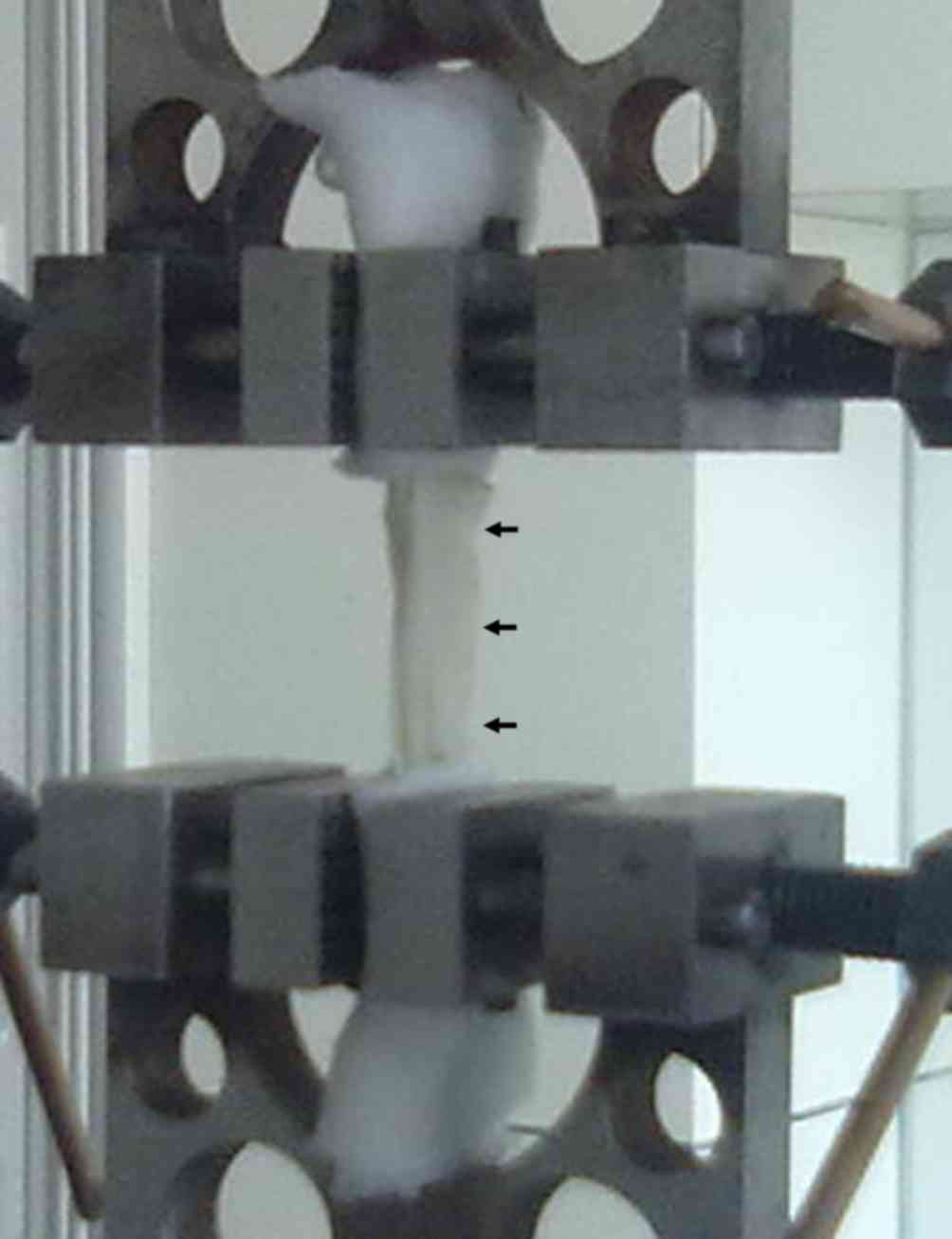
Each graft was fixed with two clamps to a
biomechanical machine (Electroforce 3520; TA Instruments, New
Castle, DE, USA) for testing, with ~35 mm of distance between the
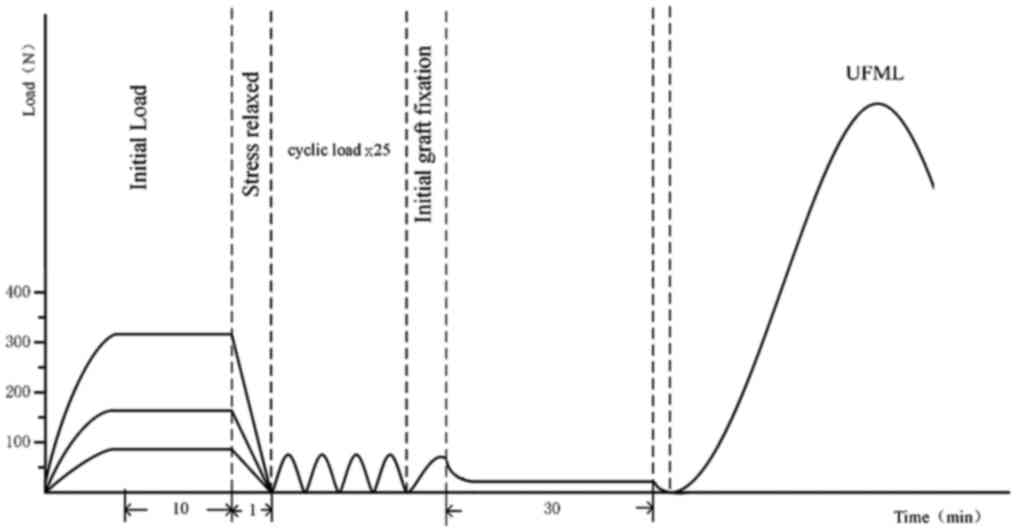
two clamps (Fig. 1). An initial load
of 80±0.28 N, 160±0.17 N and 320±0.33 N was applied to groups 1, 2
and 3, respectively, and maintained for 10 min to induce pretension
of the graft on the graft board. Grafts were gradually relaxed
until the load was reduced to 0 N and maintained for 1 min to
mirror the process of the grafts being implanted into the knee
joint. The grafts subsequently received 25 cyclic loads of 0–80 N,
modeling the passive flexion-extension motion within the knee after
femoral fixation. Following preconditioning, the grafts were
gradually loaded to 80 N and the two clamps were held in place for
30 min to simulate the application of the initially set tension of
fixing the femoral and tibial ends. Finally, the load was gradually
increased until the UFML was obtained and the load vs. displacement
curve was recorded (Wintest 4.1; TA Instruments). The loading
profile used for each graft is illustrated in Fig. 2. The stiffness was calculated as the
slope of the best fit through the load vs. displacement data.
Statistical analysis
All statistical analyses were performed using SPSS
software version 21.0 (IBM Corp., Armonk, NY, USA). Data are
presented as the mean ± standard deviation. Differences between
groups were analyzed using one-way analysis of variance and
subsequently the statistical analysis was performed using the Least
Significant Difference test between the different groups. P<0.05
was considered to indicate a statistically significant
difference.
Results
Stiffness
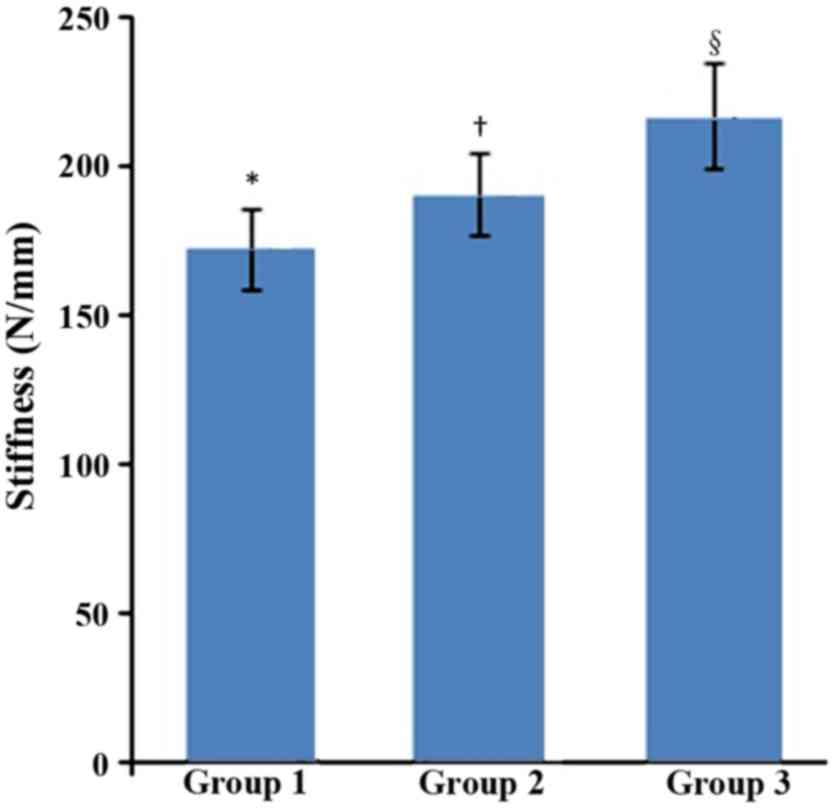
Stiffness levels of the grafts treated with
different preconditioning forces are presented in Fig. 3. Statistically significant
differences between the three groups were observed as the
preconditioning force increased (F=25.320; P<0.05).
Specifically, the stiffness of grafts in group 3 increased compared
with groups 1 and 2 (P<0.05) and the stiffness of grafts in
group 2 increased compared with group 1 (P<0.05).
UFML
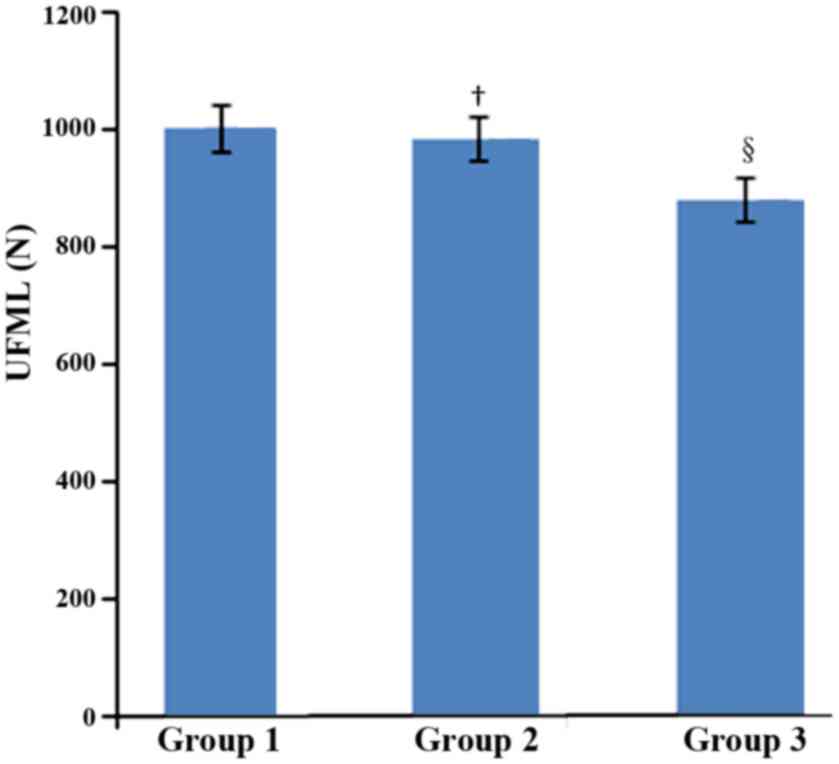
UFML values of the grafts treated with different
preconditioning forces are presented in Fig. 4. Statistically significant
differences were observed between the three groups (F=16.662;
P<0.05). Specifically, the UFML value of grafts in group 3 was
significantly lower compared with groups 1 and 2 (both P<0.05).
No significant difference was found between groups 1 and 2
(P=0.481).
Discussion
Graft selection is one of the most important factors
that influence the success of ACL reconstruction (18). Autotransplantation is routinely used
and limited by graft resources, potential functional disability and
donor site morbidity (19,20). The use of allografts is a reasonable
alternative to autografts and has become increasingly popular in
ligament construction due to an increased availability of grafts,
reduced operating time and elimination of donor-site morbidity
(18,21). However, there remain certain
potential issues associated with allotransplantation including
immune response, disease transmission and delayed ligamentization
(16,18). The γ-irradiation exhibits
bactericidal and virucidal properties and is commonly used for the
sterilization of allografts. This type of irradiation also induces
adverse effects on biomechanical properties of the allografts.
Previous studies have demonstrated a dose-dependent association
between γ-irradiation and the strength of tendon allografts
(22,23). Even a low-dose (<25 kGy) of
irradiation induces negative effects on the biomechanical
properties of the grafts (24,25). The
viscoelastic character of the tendon graft inevitably changes
following γ-irradiation (25).
Therefore, it is important to improve the performance of the
allografts used in ACL reconstruction in order to maintain the
postoperative stability of the knee. The present study investigated
the most commonly used frozen tendon grafts with 25 kGy
γ-irradiation. The aim of the present study was to investigate the
effects of different preconditioning load magnitudes on the
stiffness and tension of γ-irradiated tendon allografts, and
provide biomechanical evidence for the clinical use.
Preconditioning is considered an effective method
for eliminating graft viscoelasticity (7). As the pretension level increased during
preconditioning, the stiffness of the grafts also increased. Graft
tension and knee stability may benefit from the construct with a
high level of stiffness (3).
However, a previous study also reported that high pretension may
also lead to decreased motion, delayed vascularization and graft
failure (13). Furthermore, Suggs
et al (26) reported that a
graft with excessive stiffness may result in an overconstrained
knee and suggested that intact knee kinematics could be best
restored using a graft with similar stiffness to ACL (26). The present study demonstrated that an
increased pretension force applied to γ-irradiated deep frozen
tendon grafts during preconditioning significantly increased the
stiffness of the constructs. In addition, the preconditioning
protocols with load of 160 or 320 N seems to be more advantageous
compared with that of 80 N for the tendon stiffness. The tendon
graft stiffness preconditioned by these two protocols was closer to
the native ACL (about 182–242 N/mm) that was reported in previous
studies (27,28).
All soft tissue implants, including ACL, undergo a
similar incorporation process, including graft necrosis, cellular
repopulation, revascularization and collagen remodeling (29). A previous study indicated that
allografts were not as rapidly remodeled and incorporated into the
host tissues as autografts (30).
The tendon allograft temporarily acted as ACL prior to the
completion of ligamentization. The strength of the graft decreased
when implanted and then slowly recovered (31). Therefore, the tensile strength of the
graft serves a role in the determination of the success of an ACL
reconstruction and grafts with an increased strength are preferred
(10). Although preconditioning can
increase the stiffness of grafts to a certain extent, it may also
affect the tensile strength. Figueroa et al (10) performed an in vitro study to
determine whether tensioning altered the biomechanical properties
of grafts and reported that excessive graft tensioning decreased
tensile resistance of tendons, although it reduced the elongation
of the graft (10). The current
study indicated that the strength of γ-irradiated deep frozen
tendon grafts decreased when the pretension level reached 320 N,
implying that the tensile strength of the grafts may not improve
with the increase of the pretension level. When the pretension
level was set at 80 or 160 N, the tensile strength of tendon
allografts was closer to the native ACL at 1730–2160 N, which has
been reported previously (27,28).
The present study has certain limitations. Firstly,
only tendon allografts with a diameter of 7±0.5 mm were included.
Whether the outcomes for grafts with different diameters are
consistent with the results obtained in the presents study remains
to be elucidated. Secondly, only isotonic load was applied during
the pretension process in the present study. Whether cyclic load
protocols produce equivalent results requires further
investigation. Thirdly, in vivo studies were not carried out
and whether the clinical outcomes of ACL reconstruction could be
improved based on the present study remains to be verified.
In conclusion, the results suggested that increasing
the initial tension could effectively reduce the loss of stiffness
due to viscoelasticity for the γ-irradiated deep frozen allogeneic
tendon grafts. However, overloaded initial tension may decrease the
tensile strength.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XZ and SG made substantial contributions to
conception and design. WX and XZ performed the experiments and were
the major contributors in writing the manuscript. JG and YH
obtained the patient data regarding the diffuse brain injury. MC
and YF made substantial contributions to analysis and
interpretation of data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jiang C, Chen G, Chen P, Li W, Zhang H and
Zhang W: Double-bundle revision anterior cruciate ligament
reconstruction is effective in rescuing failed primary
reconstruction and re-introducing patients to physical exercise.
Exp Ther Med. 15:2074–2080. 2018.PubMed/NCBI
|
|
2
|
Chia ZY, Chee JN, Bin-Abd-Razak HR, Lie DT
and Chang PC: A comparative study of anterior cruciate ligament
reconstruction with double, single, or selective bundle techniques.
J Orthop Surg (Hong Kong). 26:23094990187731242018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jaglowski JR, Williams BT, Turnbull TL,
LaPrade RF and Wijdicks CA: High-load preconditioning of soft
tissue grafts: An in vitro biomechanical bovine tendon model. Knee
Surg Sports Traumatol Arthrosc. 24:895–902. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Blythe A, Tasker T and Zioupos P: ACL
graft constructs: In-vitro fatigue testing highlights the
occurrence of irrecoverable lengthening and the need for adequate
(pre)conditioning to avert the recurrence of knee instability.
Technol Health Care. 14:335–347. 2006.PubMed/NCBI
|
|
5
|
Elias JJ, Kilambi S and Ciccone WJ II:
Tension level during preconditioning influences hamstring tendon
graft properties. Am J Sports Med. 37:334–348. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Elias JJ, Rai SP and Ciccone WJ II: In
vitro comparison of tension and stiffness between hamstring tendon
and patella tendon grafts. J Orthop Res. 26:1506–1511. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nurmi JT, Kannus P, Sievänen H, Järvelä T,
Järvinen M and Järvinen TL: Interference screw fixation of soft
tissue grafts in anterior cruciate ligament reconstruction: part 2:
Effect of preconditioning on graft tension during and after screw
insertion. Am J Sports Med. 32:418–424. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arneja S, McConkey MO, Mulpuri K, Chin P,
Gilbart MK, Regan WD and Leith JM: Graft tensioning in anterior
cruciate ligament reconstruction: A systematic review of randomized
controlled trials. Arthroscopy. 25:200–207. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Numazaki H, Tohyama H, Nakano H, Kikuchi S
and Yasuda K: The effect of initial graft tension in anterior
cruciate ligament reconstruction on the mechanical behaviors of the
femur-graft-tibia complex during cyclic loading. Am J Sports Med.
30:800–805. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Figueroa D, Calvo R, Vaisman A, Meleán P
and Figueroa F: Effect of tendon tensioning: An in vitro study in
porcine extensor tendons. Knee. 17:245–258. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guillard C, Lintz F, Odri GA, Vogeli D,
Colin F, Collon S, Chappard D, Gouin F and Robert H: Effects of
graft pretensioning in anterior cruciate ligament reconstruction.
Knee Surg Sports Traumatol Arthrosc. 20:2208–2213. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yoshiya S, Andrish JT, Manley MT and Bauer
TW: Graft tension in anterior cruciate ligament reconstruction. An
in vivo study in dogs. Am J Sports Med. 15:464–470. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Peña E, Martínez MA, Calvo B, Palanca D
and Doblaré M: A finite element simulation of the effect of graft
stiffness and graft tensioning in ACL reconstruction. Clin Biomech
(Bristol, Avon). 20:636–644. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guo L, Chen H, Luo JM, Yang L, Gu LC and
Fu DJ: An arthroscopic second-look study on the effect of remnant
preservation on synovialization of bone-patellar tendon-bone
allograft in anterior cruciate ligament reconstruction.
Arthroscopy. 32:868–877. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Carter TR and Rabago MT: Allograft
anterior cruciate ligament reconstruction in patients younger than
25 years. J Knee Surg. 29:322–328. 2016.PubMed/NCBI
|
|
16
|
Tian S, Wang B, Liu L, Wang Y, Ha C, Li Q,
Yang X and Sun K: Irradiated hamstring tendon allograft versus
autograft for anatomic double-bundle anterior cruciate ligament
reconstruction: midterm clinical outcomes. Am J Sports Med.
44:2579–2588. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Curran AR, Adams DJ, Gill JL, Steiner ME
and Scheller AD: The biomechanical effects of low-dose irradiation
on bone-patellar tendon-bone allografts. Am J Sports Med.
32:1131–1135. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Vyas D, Rabuck SJ and Harner CD: Allograft
anterior cruciate ligament reconstruction: Indications, techniques,
and outcomes. J Orthop Sports Phys The. 42:196–207. 2012.
View Article : Google Scholar
|
|
19
|
Marrale J, Morrissey MC and Haddad FS: A
literature review of autograft and allograft anterior cruciate
ligament reconstruction. Knee Surg Sports Traumatol Arthrosc.
15:690–704. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shaerf DA, Pastides PS, Sarraf KM and
Willis-Owen CA: Anterior cruciate ligament reconstruction best
practice: A review of graft choice. World J Orthop. 5:23–29. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zheng X, Li T, Wang J, Dong J and Gao S:
Medial collateral ligament reconstruction using bone-patellar
tendon-bone allograft for chronic medial knee instability combined
with multi-ligament injuries: A new technique. J Orthop Surg Res.
11:852016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schwartz HE, Matava MJ, Proch FS, Butler
CA, Ratcliffe A, Levy M and Butler DL: The effect of gamma
irradiation on anterior cruciate ligament allograft biomechanical
and biochemical properties in the caprine model at time zero and at
6 months after surgery. Am J Sports Med. 34:1747–1755. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fideler BM, Vangsness CT Jr, Lu B, Orlando
C and Moore T: Gamma irradiation: Effects on biomechanical
properties of human bone-patellar tendon-bone allografts. Am J
Sports Med. 23:643–646. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ren D, Sun K, Tian S, Yang X, Zhang C,
Wang W, Huang H, Zhang J and Deng Y: Effects of gamma irradiation
and repetitive freeze-thaw cycles on the biomechanical properties
of human flexor digitorum superficialis tendons. J Biomech.
45:252–256. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
DiBartola AC, Everhart JS, Kaeding CC,
Magnussen RA and Flanigan DC: Maximum load to failure of high dose
versus low dose gamma irradiation of anterior cruciate ligament
allografts: A meta-analysis. Knee. 23:755–762. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Suggs J, Wang C and Li G: The effect of
graft stiffness on knee joint biomechanics after ACL
reconstruction-a 3D computational simulation. Clin Biomech
(Bristol, Avon). 18:35–43. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Woo SL, Hollis JM, Adams DJ, Lyon RM and
Takai S: Tensile properties of the human femur-anterior cruciate
ligament-tibia complex. The effects of specimen age and
orientation. Am J Sports Med. 19:217–225. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Noyes FR and Grood ES: The strength of the
anterior cruciate ligament in humans and Rhesus monkeys. J Bone
Joint Surg Am. 58:1074–1082. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jackson DW, Corsetti J and Simon TM:
Biologic incorporation of allograft anterior cruciate ligament
replacements. Clin Orthop Relat Res. 324:126–133. 1996. View Article : Google Scholar
|
|
30
|
Gorschewsky O, Browa A, Vogel U and
Stauffer E: Clinico-histologic comparison of allogenic and
autologous bone-tendon-bone using one-third of the patellar tendon
in reconstruction of the anterior cruciate ligament. Unfallchirurg.
105:703–714. 2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Mikami S, Yasuda K, Katsuragi R, Aoki Y,
Minami A and Tohyama H: Reduction of initial tension in the in situ
frozen anterior cruciate ligament. Clin Orthop Relat Res.
419:207–213. 2004. View Article : Google Scholar
|