Introduction
Periodontic-endodontic combined lesions are diseases
of dental pulp tissue, regularly caused by bacterial infection from
severe dental caries, periodontitis, tooth fracture or traumatic
injuries (1,2). Infected dental pulp may lead to severe
pain or clinical symptoms, such as abscess. It has the possibility
to turn lethal, thus requires cautious and thorough treatment
(2). The control of plaque is an
early stage periodontal treatment method (3). The strict control of plaque is a
necessary measure for periodontal treatment as excessive plaque may
limit the effectiveness of other treatments. Therefore plaque
control is important in the treatment of periodontal disease and is
managed throughout the whole process (3). Patients with periodontic-endodontic
combined lesions are treated with pulp therapy without periodontal
treatment when the cases have typical pulp symptoms, such as a
sudden, intense pain in the mouth (4). If the underlying cause is not treated,
although clinical symptoms may improve following dental pulp
treatment, periodontal disease may continue to develop,
consequentially lowering the effective rate of treatment (4).
Mineral trioxide aggregate (MTA) (4) has attracted attention since it was
first reported by Lee et al (5) in 1993. Certification for its clinical
use was granted by the Food and Drug Administration in 1993 and it
was adopted in dental therapy in following years (6). MTA has low cytotoxicity, agreeable
biocompatibility and has been certified in vivo and in
vitro (7,8). When MTA is used as a repair material in
the apical zone, it has been observed to induce almost no
inflammatory reaction, and almost all samples with MTA surfaces
demonstrate new cementum formation (8). It has been demonstrated that when MTA
is applied as a repair material in a treatment group, cementum was
observed in the perforation area with almost no inflammation;
however, necrosis of periodontal tissues was observed in the
control groups that were treated with other materials (9). In addition, almost all the periodontal
tissues in the treatment group were restored in 6 months, and
cellular cementum had formed between cementum and alveolar bone,
accompanied by the formation of periodontal ligaments (9). MTA has been applied directly for pulp
capping and pulp cutting, which has been indicated to induce almost
no inflammatory reaction and promoted the development of the root
(10). MTA has received much
attention due to its favorable tissue compatibility, high
bioactivity and low cytotoxicity (11). Additionally, MTA effectively reduces
the production of micro leakage in dental diseases, increases the
success rate of root canal therapy, promotes the proliferation of
dental pulp stem cells to preserve the vitality of the pulp and
also improves the success rate of root tip induction (11,12).
However, the application of MTA has shortcomings, including a slow
cure rate and its application requires sterile conditions, which
limits its application to the clinic.
In the affected tooth, the mixed infection of
anaerobic bacteria predominantly exists in the periodontal pocket
and pulp, both of which affect and spread the infection and disease
to each other, which increases the difficulty of clinical treatment
(13). Minocycline is the main
constituent of minocycline hydrochloride ointment (MHO), which has
a wide antibacterial spectrum, strong antibacterial activity, high
efficiency and long lasting effects (14). Furthermore, its antibacterial effect
is three times stronger than that of the single tetracycline
antibiotic (14,15). As a kind of local periodontal
sustained release drug, MHO becomes a hard layer of membrane when
it encounters water, allowing it to slowly release the drug into
the periodontal pocket. The high local concentration of MHO
significantly relieves clinical periodontal symptoms (16,17).
However, MHO may induce dysbacteriosis, which may lead to vitamin
deficiency. Severe vitamin deficiency cases may result in liver
damage, kidney damage and other adverse reactions, which require
replacement of the treatment type or a combination therapy that
ameliorates the outcome (16).
Periodontic-endodontic combined lesions are fairly
common clinically, and the periodontal tissue and dental pulp
tissue communicate with each other anatomically, making treatment
difficult. MHO is a highly efficient, long-lasting, strong
broad-spectrum antimicrobial with sustained-release preparations,
and MTA has high histocompatibility, edge sealing, high biological
activity and low cytotoxicity. However, the side effects of MHO
cannot be dismissed. Thus, the present research aimed to determine
the effectiveness and feasibility of MHO and MTA combination
treatment in severe periodontic-endodontic combined lesions.
Patients and methods
Patients
Ethical approval was granted by the Medical Ethics
Committee of Shanghai Jiaotong University (Shanghai, China;
reference no. JTRT2010051531). Informed signed consent was gathered
from the participants prior to initiation of the study. Patients
with periodontic-endodontic combined lesions were selected from the
Department of Stomatology, Shanghai Ninth People's Hospital
(Shanghai, China) between August 2010 and July 2014. The diagnosis
was performed by two independent researchers. Inclusion criteria
were as follows: i) Periodontitis: 3–10 mm of periodontal pocket
depth, 1–3° of tooth mobility (16),
1–3° of root furcation and loss of lamina as shown in X-ray
examination; and ii) pulpitis and periapical periodontitis:
Continuous dental malaise, dull or negative in test for pulp
vitality and periapical sparse area as shown in X-ray examination.
Exclusion criteria were as follows: i) Patients with deciduous
teeth; ii) patients unable to take root canal therapy; iii)
patients unable to take timely reexamination; iv) according to two
researchers with clinical experience, patients with systemic
diseases that affect the treatment effect, including severe kidney
disease, diabetes, hyperthyroidism and acquired immune deficiency
syndrome (18); and v) patients that
had received other therapies in last 3 months.
A total of 212 patients were selected for the
present study. There were 92 males and 116 females, with an age
range of 20–80 years. A total of 294 teeth were included in the
present experiment: 168 anterior teeth and 126 posterior teeth. The
patients were randomly divided into four groups: Control group (56
cases and 75 teeth), MTA group (52 cases and 73 teeth), MHO group
(52 cases and 71 teeth) and combination group (52 cases and 75
teeth). There were three types of etiology according to the cause
of the disease: Type I, periodontal lesions caused by endodontic
diseases; type II, endodontic lesions caused by periodontal
diseases; and type III, coexistence of two lesions. The
pathological changes of pulp were classified into four grades
according to the standard reported by Mazur and Massler (18), including grade I, grade II, grade III
and grade IV. The teeth were divided into four levels according to
the pulp pathological grade: Level I, II, III and IV (18). These levels and grades indicate
increasingly severe pathological damage.
Experimental materials
2% MHO (trade name, Perioline) was purchased from
Sunstar, Inc., (Osaka, Japan). MTA was purchased from Dentsply
Sirona (York, PA, USA).
Specimen preparation and hematoxylin
and eosin staining
For patients who decided to remove affected teeth
regardless of severity, the extraction was performed following
additional signed consent by the patient. Subsequent to tooth
extraction, the teeth were fixed in 10% neutral formalin for 3 days
and then washed using water flushing. Following this, the relative
two axial surfaces of the teeth were evenly ground along the tooth
body using a high-speed turbine with diamond sand until the
complete morphology of the marrow cavity was clearly visible
through the hard tissue of the tooth. The teeth were fixed in 10%
neutral formalin at room temperature for 1 week to ensure that the
pulp was fully fixed. The teeth were removed when they were soft
enough to perforate with an expanding needle, and then washed with
flowing water. The tooth slices were removed from the 10%
formaldehyde solution and douched with 0.85% saline. The liquid on
the surface was wiped away carefully with filter paper.
Subsequently, the samples were dehydrated with 95–100% alcohol in
an automatic hydroextractor overnight. A pathological tissue
embedding machine (cat no. 8330; Thermo Fisher Scientific, Inc.,
Waltham, MA, UAS) was utilized to slice the paraffin embedded tooth
tissue into slices of 3 µm. The slices were tweezed onto a glass
slide gently and the folds were stretched out. The ready-made slice
was dewaxed twice using xylene, for 10 min each, and then douched
in saline. The resultant slice was stained for 5 min at room
temperature using hematoxylin. The glass slide was douched and then
0.5% eosin was used for staining for 30 sec at room temperature.
The slice was dehydrated with alcohol again and dealcoholized with
xylene. Neutral gum (cat. no. BD5044; Bioworld Technology, Inc.,
St. Louis Park, MN, USA) was dropped on the slice so that the cover
slip was replaced. The resultant slice was observed under a light
microscope at magnification ×200 and images were captured.
Treatment method
Local treatment on the lesion, including rinsing and
disinfection, was performed prior to the treatment method of the
present study. At the same time, 500 mg broad-spectrum
antimicrobial agents Amoxicillin Capsules (cat. no. A662203; Sangon
Biotech Co., Ltd., Shanghai, China) and 400 mg metronidazole (cat.
no. A600633; Sangon Biotech Co., Ltd.) was taken orally, three
times a day for 1 week prior to the present study. Root canal
preparation and root canal disinfection were performed in the four
groups. Routine root canal therapy was performed in the four study
groups. Following disinfection, a drug conveyor was inserted into
the front end of the root tip ~1/5 deep, which injected the tip of
the tooth with the desired drug. When the MTA paste [Zinc oxide
glycerin paste (Desitin Pharma Ltd., Milton Keynes, UK) for the
control group] was overflown from the root canal orifice, injection
and simultaneous extraction of the conveyer was continued gently.
Excess paste was removed using a cotton pad. Zinc oxide glycerin
paste and apical root canal was used for filling in the control
group. All procedures were performed by the same senior
specialist.
Evaluation of curative effect
standard
Clinical effects were collected and evaluated in
patients following treatment, according to associated literature
(18,19), as follows: Cured, periodontal pockets
are shallower, no conspicuous exsertion was noticed in the
bifurcation area, no loosening in percussion, good masticatory
function, no shallow areas as shown in X-ray examination and the
formation of new lamina dura; effective, periodontal pockets
shallowed but not conspicuous, 1° exsertion in bifurcation area, 1°
loosening in percussion, unable to chew hard food, shrunken shallow
areas as demonstrated in an X-ray and partial formation of lamina
dura; and ineffective, depth of periodontal pockets not changed,
positive results in percussion, poor masticatory function, and same
or enlarged shallow area in periapical and periodontal area. The
proportion of cured and effective teeth was recorded as the total
effective rate.
Probing depth (PD) and gingival index (GI) were
recorded as clinical indices for periodontal condition (18). Evaluation of therapeutic effect was
as follows: Significantly effective, PD declining >2 mm, GI
decreasing to 1/2, no clinical symptoms and a reduced degree of
loosening; effective, PD declining >1 mm, GI decreasing to
1/3-1/2, no improvement in the degree of loosening and no clinical
symptoms; and ineffective, no improvement in clinical symptoms, no
improvement in PD or GI and no improvement in degree of
loosening.
Follow-up
The patients were followed up every quarter of a
year for 2 years after treatment and statistically analyzed by
their conditions. Evaluation standard was performed as
aforementioned.
Statistical analysis
SPSS (version 21; IBM Corp., Armonk, NY, USA) was
used for data analysis. Measurement data were presented as the mean
± standard deviation. Analysis of variance followed by the
Dunnett's post hoc multiple comparisons test were applied to
analyze multiple groups. The χ2 test was used for
comparison between the groups. Factors affecting the root filling
effect, including age, sex, tooth position, etiology, medical
history, root canal filling, root filling method and periapical
situation, were analyzed by logistic regression analysis. P<0.05
was considered to indicate a statistically significant
difference.
Results
Pathological changes of chronic
periodontic-endodontic combined lesions
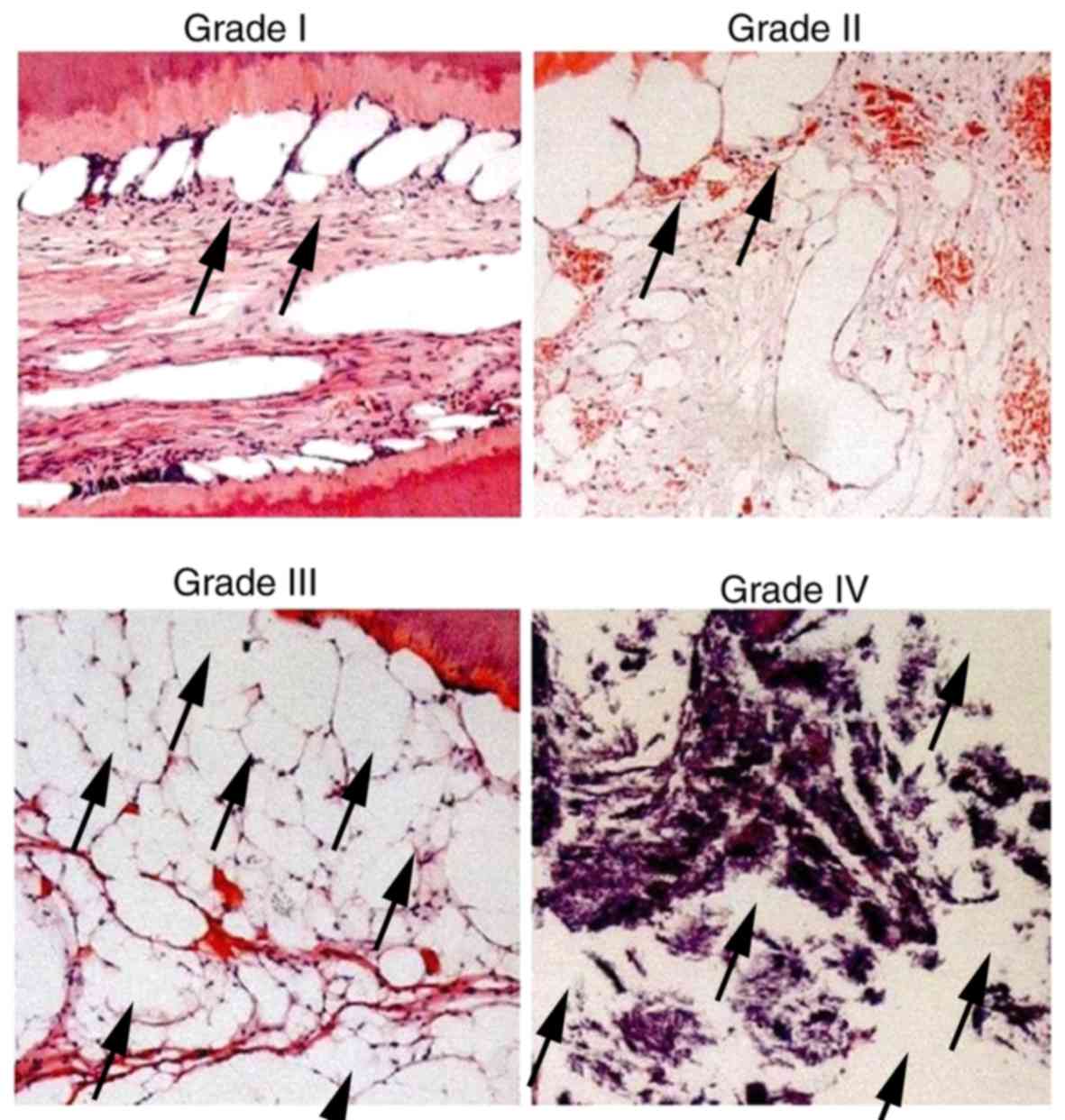
The pathological changes of the dental pulp tissue
were observed under a microscope, the typical images of each grade
are demonstrated in Fig. 1. The data
indicated that the pathological changes of dental pulp in patients
with mild periodontitis were the highest in grade I and II, grade
III was slightly less and grade IV was the lowest. In addition, the
severe periodontitis group suffering from the most notable dental
pathological changes (including periodontal cysts) were present in
level IV, level I demonstrated the least pathological changes, and
grade II and III demonstrated slightly more changes than grade I.
Representative images was taken at magnification ×200. The number
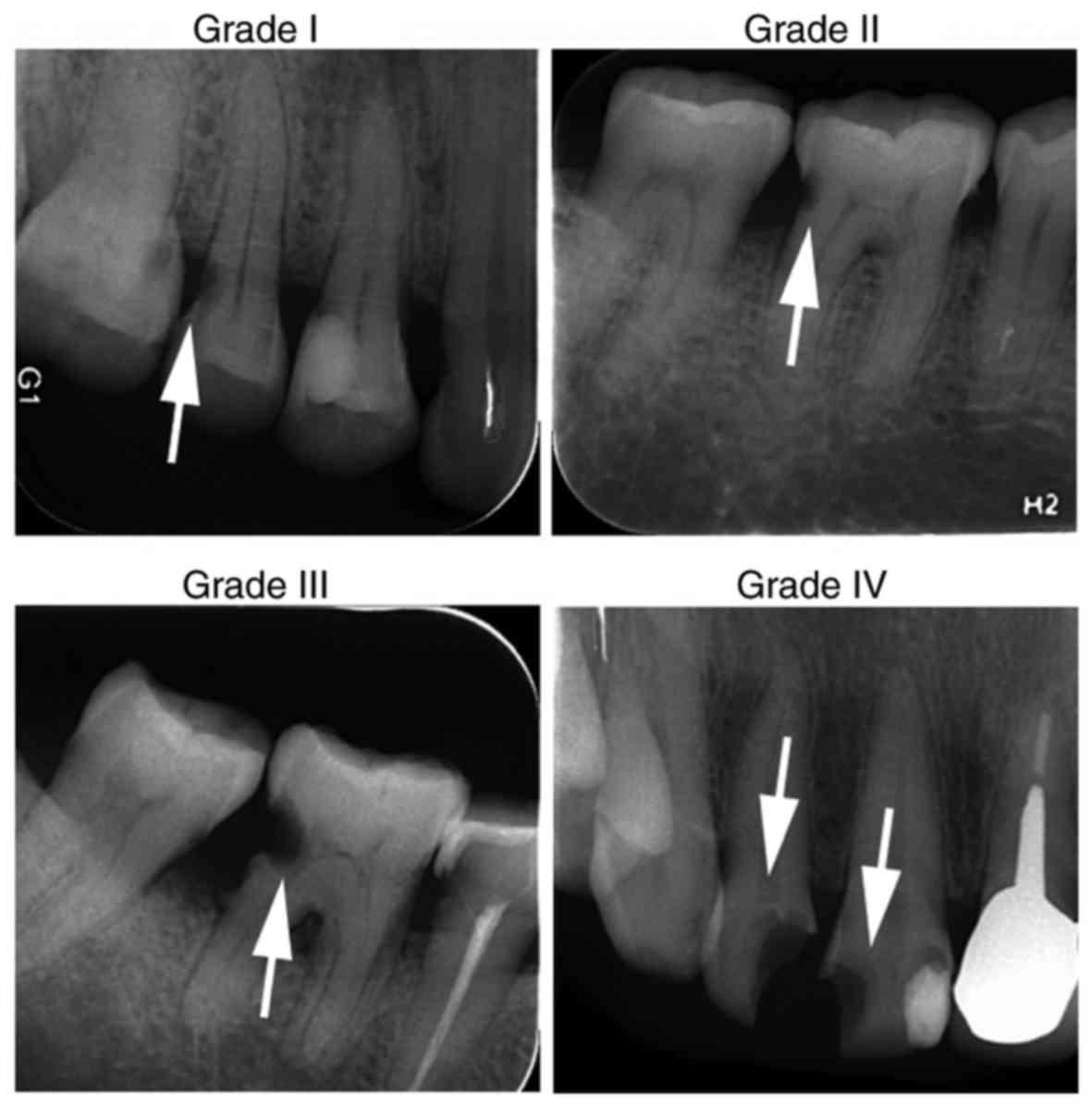
of periodontal cysts increased from Grade I to IV. In Fig. 2, X-ray images captured prior to
treatment of patients' teeth were used for classification according
to their pathological damage. The white arrows indicate lesions of
different grades; the lesions become larger and occur in larger
numbers at higher grades. These data implied that mild
periodontitis may be associated with mild dental pulp stimulation
while severe periodontitis may be associated with stronger
stimulation. Of note, the staining of all samples in Fig. 1 was the same. The inhomogeneous
staining of the grade IV sample may be due to the restore condition
of the slide, which may contaminate the tissue color. This does not
affect the outcome.
Medical history, root filling and
periapical condition are critical factors in treatment of
periodontic-endodontic combined lesions
In the present study, patients with severe
periodontic-endodontic combined lesions were the main focus and
related factors were further studied. Factors affecting the root
filling effect, including age, sex, tooth position, etiology,
medical history, root canal filling, root filling method and
periapical situation, were analyzed by logistic regression
analysis. The results demonstrated that medical history (P=0.023),
periapical situation (P=0.009) and root canal filling (P=0.347)
were closely related to clinical efficacy. Other factors, including
age, sex, tooth position, etiological factor and root filling
method, were not observed to be significantly associated with
clinical efficacy (Table I). These
results suggest that these indexes affect the joint lesion of
periodontal pulp, which may enable further improvement of the
treatment effect.
 | Table I.Factors relevant to patients with
severe periodontic- endodontic combined lesions analyzed by
logistic regression. |
Table I.
Factors relevant to patients with
severe periodontic- endodontic combined lesions analyzed by
logistic regression.
| Factor | Β regression
coefficient |
X2 | P-value |
|---|
| Age | 0.082 |
0.285 | 0.781 |
| Sex | 0.352 |
1.529 | 0.263 |
| Tooth position | 0.423 |
0.011 | 0.118 |
| Etiology | 0.769 |
0.075 | 0.904 |
| Medical history | 1.966 |
9.832 | 0.023 |
| Medical expense | 3.350 | 18.923 | 0.012 |
| Root canal filling
measure | 0.967 |
1.781 | 0.347 |
| Periapical
condition | 1.542 | 23.109 | 0.009 |
Efficacy of combination therapy for
anterior and posterior teeth is greater than that of MTA or MHO
therapy alone in patients with severe periodontic-endodontic
combined lesions
In order to study the curative effect of combination
therapy in patients with severe periodontic-endodontic lesions, the
various therapy strategies were used to treat the patients and
statistical analysis was performed to compare the effects in the
different groups. The results demonstrated that the curative effect
for the anterior and posterior teeth did not differ significantly
in patients in the control group and three experimental groups
(P>0.05). Subsequently, the curative effect between the
different experimental groups was analyzed. The data indicated that
the curative effect for the anterior and posterior teeth of the
patients in the experimental groups was significantly increased
compared with the effects observed in the control group (P<0.05;
Table II). The present data also
revealed that the curative effect for the anterior and posterior
teeth of the patients in the MTA group and MHO group was not
statistically significant (P>0.05). However, the curative effect
for the anterior and posterior teeth of the patients in the
combined treatment group was significantly increased compared with
the effects observed in the MTA and MHO groups (P<0.05; Table II). These data suggest that there
was no significant difference between the effects on the anterior
and posterior teeth of the patients when the patients were treated
with MTA or MHO alone. However, the curative effect for the
anterior and posterior teeth of the patients was significantly
improved when the patients received the combined treatment,
indicating that the combination therapy had a superior curative
effect for the anterior and posterior teeth of the patients with
severe periodontic-endodontic lesions.
 | Table II.Comparison of clinical effects of
treatment on anterior and posterior teeth in patients with severe
periodontic-endodontic combined lesions. |
Table II.
Comparison of clinical effects of
treatment on anterior and posterior teeth in patients with severe
periodontic-endodontic combined lesions.
|
|
|
| Treatment effect, n
(%) |
|
|---|
|
|
|
|
|
|
|---|
| Group | Tooth | n | Cured | Effective | Ineffective | Total effective
rate, n (%) |
|---|
| Control | Anterior | 40 | 13 (32.5) | 8 (20) | 19 (47.5) | 21 (52.5) |
|
| Posterior | 35 | 6 (31.6) | 9 (25.7) | 20 (57.1) | 15 (42.9) |
| MTA | Anterior | 38 | 17 (44.7) | 11 (28.9) | 10 (26.3) | 28
(73.7)a |
|
| Posterior | 35 | 14 (40.0) | 7 (20.0) | 14 (40.0) | 21
(60.0)b |
| MHO | Anterior | 37 | 19 (52.4) | 8 (21.6) | 10 (27.0) | 27
(73.0)a |
|
| Posterior | 34 | 12 (35.3) | 10 (29.4) | 12 (35.3) | 22
(64.7)b |
| Combination | Anterior | 39 | 25 (64.1) | 12 (30.8) | 2 (12.8) | 37
(94.9)a,c,e |
|
| Posterior | 36 | 20 (55.6) | 13 (36.1) | 3 (8.3) | 33
(91.7)b,d,f |
Combination treatment is more
effective in patients with pathological types I, II and III severe
periodontic-endodontic combined lesions
In order to study the curative effect on patients
with severe periodontic-endodontic combined lesions, the curative
effect on various disease types following treatment with different
strategies was analyzed. The results revealed that the curative
effects for the type I, II and III periodontal pulp joint lesions
of the patients in the control group or experimental groups were
not statistically significant (P>0.05). Subsequently, the
curative effect between the different experimental groups was
analyzed. The data revealed that the curative effect for the type
I, II and III periodontal pulp joint lesions of the patients in the
experimental groups was significantly increased compared with the
type I, II and III periodontal pulp joint lesions in the control
group, respectively (P<0.05; Table
III). The present data also indicated that the curative effect
for the type I, II and III periodontal pulp joint lesions of the
patients in the MTA group and MHO group was not statistically
significant (P>0.05). However, the curative effects for the type
I, II and III periodontal pulp joint lesions of the patients in the
combined treatment group were significantly increased compared with
those in the MTA and MHO groups, respectively (P<0.05; Table III). These data imply that there
was rarely a significant difference for the type I, II and III
periodontal pulp joint lesions of the patients when the patients
were treated with MTA or MHO alone; however, the curative effect
for the type I, II and III periodontal pulp joint lesions of the
patients was significantly improved when the patients received
combined treatment. This suggests that the combination therapy had
a superior curative effect for the different types of periodontal
pulp joint lesions of the patients with severe
periodontic-endodontic lesions.
 | Table III.Clinical effects of treatments in
patients with different pathological types of
periodontic-endodontic combined lesions. |
Table III.
Clinical effects of treatments in
patients with different pathological types of
periodontic-endodontic combined lesions.
|
|
|
| Treatment effect, n
(%) |
|
|
|
|
|
|
|
| Group | Pathological
type | n | Cured | Effective | Ineffective | Total effective
rate, n (%) |
|---|
| Control | I | 28 | 9 (32.1) | 5 (17.9) | 14 (50.0) | 14 (50.0) |
|
| II | 30 | 7 (23.3) | 6 (20.0) | 17 (56.7) | 13 (43.3) |
|
| III | 17 | 7 (41.2) | 2 (11.8) | 8 (47.1) | 9 (52.9) |
| MTA | I | 27 | 11 (40.7) | 5 (18.5) | 11 (40.7) | 16
(59.2)a |
|
| II | 29 | 12 (41.4) | 8 (27.6) | 9 (31.0) | 20
(69.0)b |
|
| III | 17 | 8 (47.1) | 4 (23.5) | 5 (29.4) | 13
(70.6)c |
| MHO | I | 27 | 13 (48.1) | 5 (18.5) | 9 (33.3) | 18
(66.7)a |
|
| II | 26 | 9 (34.6) | 8 (30.8) | 9 (34.6) | 17
(65.4)b |
|
| III | 18 | 8 (44.4) | 6 (33.3) | 4 (22.2) | 14
(77.8)c |
| Combination | I | 29 | 23 (79.3) | 4 (13.8) | 2 (6.9) | 27
(93.1)a,d,g |
|
| II | 30 | 22 (73.3) | 6 (20.0) | 2 (6.7) | 28
(93.3)b,e,h |
|
| III | 16 | 12 (75.0) | 3 (18.8) | 1 (6.3) | 15
(93.8)c,f,i |
Combination treatment decreases the PD
and GI index in patients with severe periodontic-endodontic
combined lesions
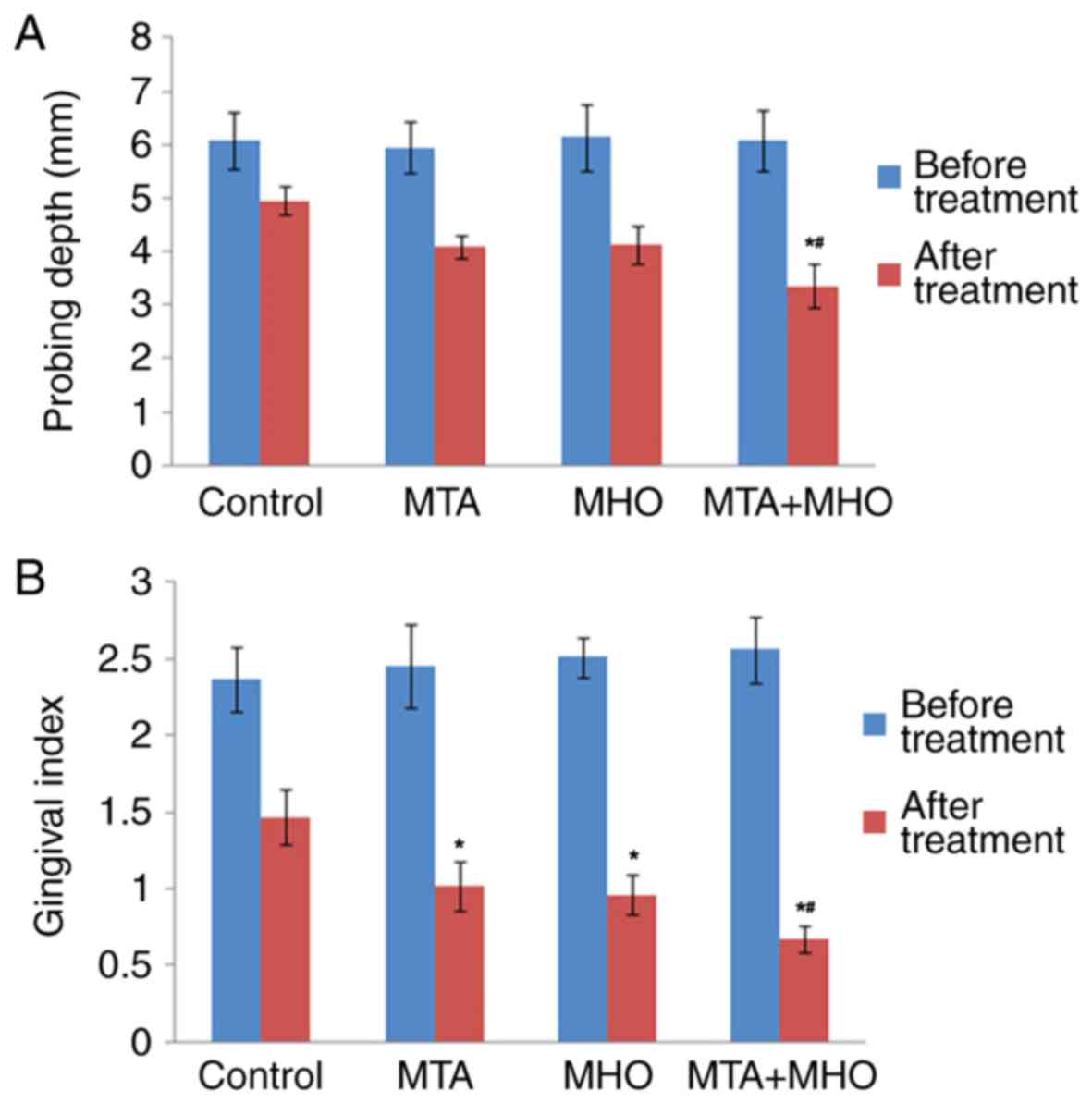
In order to explore the efficacy of treatment
strategies for patients with severe periodontic-endodontic combined
lesions, GI and PD were further statistically analyzed prior to and
following treatment in patients. As demonstrated in Fig. 3, there was no significant difference
between the experimental groups and the control group prior to
treatment (P>0.05), which implied that the experimental results
were comparable. In addition, the data revealed that the GI was
decreased significantly in each treatment group compared with that
in the control group after 4 weeks of treatment (P<0.05). PD was
not significantly different in the MTA and MHO groups compared with
the control group following 4 weeks of treatment. These results
indicated that various treatment strategies could remarkably
alleviate symptoms in patients with periodontic-endodontic combined
lesions. Furthermore, the data indicated that the GI and PD were
not significantly different between the MTA group and MHO group
(P>0.05). However, the GI and PD in the combined treatment group
were significantly decreased compared with those in the MTA and MHO
groups (P<0.05; Fig. 3). These
results suggest that the combination therapy had a superior
curative effect for the patients with severe periodontic-endodontic
combined lesions.
Combination treatment demonstrates
superior effects to single treatments for patients with severe
periodontic-endodontic combined lesions at follow-up
In order to explore the long-term efficacy of
treatment strategies for patients with severe
periodontic-endodontic combined lesions, the curative efficacy 2
years after treatment was statistically analyzed. The data
demonstrated that the total effective rates were significantly
increased 2 years after treatment in the experimental groups
compared with that in the control group (P<0.05; Table IV), indicating that the treatment
strategies used in the experimental groups had a long-term effect.
The data also revealed that the total effective rate in the MHO
group was not significantly different to that of the MTA group
(P>0.05; Table IV). However, the
total effective rate was significantly increased in the combined
treatment group 2 years after treatment compared with that in the
MTA and MHO groups, respectively (P<0.05; Table IV). These results suggest that the
long-term efficacy was not significant between MTA treatment and
MHO treatment; however, long-term efficacy was improved
significantly when the combined treatment was adopted, indicating
that the combination therapy has a superior curative effect.
 | Table IV.Clinical effect in 2-year
follow-up. |
Table IV.
Clinical effect in 2-year
follow-up.
|
|
| Treatment effect, n
(%) |
|
|---|
|
|
|
|
|
|---|
| Group | n | Cured | Effective | Ineffective | Total effective
rate, n (%) |
|---|
| Control | 56 | 13 (23.2) | 11 (19.6) | 32 (57.1) | 24 (42.9) |
| MTA | 52 | 21 (39.6) | 10 (18.9) | 21 (40.4) | 31
(58.5)a |
| MHO | 52 | 20 (36.4) | 14 (25.5) | 18 (34.6) | 34
(60.7)a |
| Combination | 52 | 33 (57.9) | 14 (26.9) | 5 (9.6) | 47
(90.3)a–c |
Discussion
Periodontal pulp syndrome involves combined lesions
that occur in the pulp and periodontal tissues, which is usually
accompanied by severe periodontal injures (1). The clinical manifestation of
periodontic-endodontic combined lesions is complicated, the course
of the disease and treatment are relatively long, and its clinical
prognosis is relatively poor (19,20).
Therefore, the clinical treatment of periodontic-endodontic
combined lesions is based on the initial cause of the disease to
develop the corresponding treatment plan. Dental pulp disease is a
common disease within oral medicine and root canal filling or
mummification of pulp treatment is widely used in clinics; dental
adhesive, zinc oxide and phenolic resin are commonly used as root
canal filling materials (21–23).
In the present study, the patients with 3–10 mm
depth of periodontal pocket with severe periodontal damage were
selected. Firstly, various factors affecting the treatment effect
of the patients with periodontic-endodontic combined lesions were
statistically analyzed using logistic regression analysis. The
results demonstrated that medical history, root filling and
periapical condition were the critical factors affecting the
treatment of patients with periodontic-endodontic combined lesions,
suggesting that these factors should be taken into account when
treating this disease. Then, a combination of MHO and MTA was used
for the treatment of periodontic-endodontic combined lesions, and
the results revealed that the total curative efficiency of the
anterior and posterior teeth was significantly increased in the
combined treatment group compared with either treatment alone. This
implied that combination therapy was significantly effective. In
addition, the present study indicated that type I, II and III
disease was significantly improved when the patients received
combined treatment. All of these data suggest that the curative
effect of the patients with periodontic-endodontic combined lesions
was improved significantly when a combination treatment of MHO and
MTA was utilized. Furthermore, GI and PD are two important indexes
used to measure the comprehensive curative effect of patients with
severe periodontic-endodontic combined lesions (24–26). The
GI and PD of patients in the present study were measured prior to
and following treatment and the results were statistically
analyzed. The data demonstrated that PD and GI were decreased
significantly in the combined treatment group compared with the
levels in the MTA or MHO groups, the total effective rate was
significantly excelled when compared with that in the control
group, and the use of the drugs rarely caused local or systemic
adverse reactions (data not shown). These results illustrate that
following the use of MHO and MTA in combination, not only damage of
the periodontal tissue was reduced, but also the tissue healed
quickly, which may be related to the inhibition of collagenase
activity and prevention of periodontal tissue destruction (27–31).
In conclusion, the present study utilized MTA
combined with MHO for the treatment of severe
periodontic-endodontic combined lesions. The data suggested that
the treatment efficacy of pulp necrosis in patients was
significantly improved and a therapeutic effect on the patients
with apical inflammation was observed following combination
treatment. Therefore, this combination treatment may be valuable in
clinics for the treatment of patients with periodontic-endodontic
combined lesions.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Research
project of Shanghai Municipal Health and Family Planning Commission
(grant no. 201440401).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to the protection of
patient's privacy but are available from the corresponding author
on reasonable request.
Authors' contributions
FX, ZXX and YW analyzed and interpreted the patient
data regarding the hematological disease and the transplant. RHR
and WS performed the histological examination of the teeth and WS
was a major contributor in writing the manuscript. YQW is head of
the department and helped design the study. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Ethical approval was granted by the Medical Ethics
Committee of Shanghai Jiaotong University (Shanghai, China;
reference no. JTRT2010051531). Informed signed consent was gathered
from the participants prior to initiation of the study.
Consent for publication
In the present study, the patient, parent, guardian
or next of kin as appropriate provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Raheja J, Tewari S, Tewari S and Duhan J:
Evaluation of efficacy of chlorhexidine intracanal medicament on
the periodontal healing of concomitant endodontic-periodontal
lesions without communication: An interventional study. J
Periodontol. 85:1019–1026. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Huffaker SK, Safavi K, Spangberg LS and
Kaufman B: Influence of a passive sonic irrigation system on the
elimination of bacteria from root canal systems: A clinical study.
J Endod. 36:1315–1318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zimet PO and Endo C: Preservation of the
roots-management and prevention protocols for cracked tooth
syndrome. Ann R Australas Coll Dent Surg. 15:319–324.
2000.PubMed/NCBI
|
|
4
|
Torabinejad M, Watson TF and Ford Pitt TR:
Sealing ability of a mineral trioxide aggregate when used as a root
end filling material. J Endod. 19:591–595. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee SJ, Monsef M and Torabinejad M:
Sealing ability of a mineral trioxide aggregate for repair of
lateral root perforations. J Endod. 19:541–544. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sluyk SR, Moon PC and Hartwell GR:
Evaluation of setting properties and retention characteristics of
mineral trioxide aggregate when used as a furcation perforation
repair material. J Endod. 24:768–771. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Karygianni L, Proksch S, Schneider S, Vach
K, Hellwig E, Steinberg T, Schulz SD, Tchorz JP and Altenburger MJ:
The effects of various mixing solutions on the biocompatibility of
mineral trioxide aggregate. Int Endod J. 49:561–573. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Prasad A, Pushpa S, Arunagiri D, Sawhny A,
Misra A and Sujatha R: A comparative evaluation of the effect of
various additives on selected physical properties of whitemineral
trioxide aggregate. J Conserv Dent. 18:237–241. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moore A, Howley MF and O'Connell AC:
Treatment of open apex teeth using two types of white mineral
trioxide aggregate after initial dressing with calcium hydroxide in
children. Dent Traumatol. 27:166–173. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Agamy HA, Bakry NS, Mounir MM and Avery
DR: Comparison of mineral trioxide aggregate and formocresol as
pulp-capping agents in pulpotomized primary teeth. Pediatr Dent.
26:302–309. 2004.PubMed/NCBI
|
|
11
|
Challenger H, Lane J, Becker R,
Nassiripour S and Torabinejad M: Dye leakage and modification of
fast-setting mineral trioxide aggregate. J Calif Dent Assoc.
43:82–86. 2015.PubMed/NCBI
|
|
12
|
Ravindran S and George A: Biomimetic
extracellular matrix mediated somatic stem cell differentiation:
Applications in dental pulptissue regeneration. Front Physiol.
6:1182015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Giovanella LB, Barletta FB, Felippe WT,
Bruno KF, De Alencar AH and Estrela C: Assessment of oxygen
saturation in dental pulp of permanent teeth with periodontal
disease. J Endod. 40:1927–1931. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xia X, Huang BX, Zhu WD and Meng HX:
Effect of minocycline hydrochloride ointment on cell attachment and
proliferation on titanium disks. Zhonghua Kou Qiang Yi Xue Za Zhi.
47:518–522. 2012.(In Chinese). PubMed/NCBI
|
|
15
|
Nakao R, Takigawa S, Sugano N, Koshi R,
Ito K, Watanabe H and Senpuku H: Impact of minocycline ointment for
periodontal treatment of oral bacteria. Jpn J Infect Dis.
64:156–160. 2011.PubMed/NCBI
|
|
16
|
Shigeyama M, Ohgaya T, Kawashima Y,
Takeuchi H and Hino T: Modification of the physicochemical
properties of minocycline hydrochloride ointment with
cyclodextrines for optimum treatment of bedsore. Chem Pharm Bull
(Tokyo). 48:617–622. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shigeyama M, Ohgaya T, Kawashima Y,
Takeuchi H and Hino T: Mixed base of hydrophilic ointment and
purified lanolin to improve the drug release rate and absorption of
water of minocycline hydrochloride ointment for treatment of
bedsores. Chem Pharm Bull (Tokyo). 47:744–748. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mazur B and Massler M: Influence of
periodontal diseases on the dental pulp. Oral Surg Oral Med Oral
Pathol. 17:592–603. 1964. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rotstein I and Simon JH: Diagnosis,
prognosis and decision-making in the treatment of combined
periodontal-endodontic lesions. Periodontol 2000. 34:165–203. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Walter C, Krastl G and Weiger R: Step-wise
treatment of two periodontal-endodontic lesions in a heavy smoker.
Int Endod J. 41:1015–1023. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Marques JH, Silva-Sousa YT, Rached-Júnior
FJ, Mazzi-Chaves JF, Miranda CE, Da Silva SR, Steier L and
Sousa-Neto MD: New methodology to evaluate bond strength of
root-end filling materials. Braz Dent J. 26:288–291. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lahor-Soler E, Miranda-Rius J,
Brunet-Llobet L, Farré M and Pumarola J: In vitro study of the
apical microleakage with resilon root canal filling using different
final endodontic irrigants. J Clin Exp Dent. 7:e212–e217. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Prestegaard H, Portenier I, Ørstavik D,
Kayaoglu G, Haapasalo M and Endal U: Antibacterial activity of
various root canal sealers and root-end filling materials in dentin
blocks infected ex vivo with Enterococcus faecalis. Acta Odontol
Scand. 72:970–976. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Patel SP, Kalra N, Pradeep AR, Martande
SS, Naik SB, Raju AP and Singh P: Association of metabolic syndrome
and periodontal disease in an Indian population. J Int Acad
Periodontol. 16:98–1028. 2014.PubMed/NCBI
|
|
25
|
AL Shayeb KN, Turner W and Gillam DG:
Accuracy and reproducibility of probe forces during simulated
periodontal pocket depthmeasurements. Saudi Dent J. 26:50–55. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ishihata K, Wakabayashi N, Wadachi J,
Akizuki T, Izumi Y, Takakuda K and Igarashi Y: Reproducibility of
probing depth measurement by an experimental periodontal probe
incorporating optical fiber sensor. J Periodontol. 83:222–227.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Geng S, Cao C and Chen Z: The effect of
non-surgical periodontal and adjunctive minocycline-HCL treatments
on collagenase activity. Zhonghua Kou Qiang Yi Xue Za Zhi.
35:336–339. 2000.(In Chinese). PubMed/NCBI
|
|
28
|
Hajishengallis G, Abe T, Maekawa T,
Hajishengallis E and Lambris JD: Role of complement in host-microbe
homeostasis of the periodontium. Semin Immunol. 25:65–72. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Anand PS, Kamath KP, Bansal A, Dwivedi S
and Anil S: Comparison of periodontal destruction patterns among
patients with and without the habit of smokeless tobacco use-a
retrospective study. J Periodontal Res. 48:623–631. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Messora MR, Oliveira LF, Foureaux RC, Taba
M JR, Zangerônimo MG, Furlaneto FA and Pereira LJ: Probiotic
therapy reduces periodontal tissue destruction and improves the
intestinal morphology in rats with ligature-induced periodontitis.
J Periodontol. 84:1818–1826. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Konermann A, Al-Malat R, Skupin J, Keilig
L, Dirk C, Karanis R, Bourauel C and Jäger A: In vivo determination
of tooth mobility after fixed orthodontic appliance therapy with a
novel intraoral measurement device. Clin Oral Investig.
21:1283–1289. 2017. View Article : Google Scholar : PubMed/NCBI
|