Introduction
Thoracolumbar fracture is a common clinical
traumatic vertebral trauma. Conservative treatment is mainly for
simple vertebral compression fractures, while open reduction and
internal fixation are often applied to patients with more than 1/2
high compression of the vertebral body or with reduced spinal canal
sagittal diameter. However, there are some shortcomings in these
two treatment types. Simple conservative treatment often causes
complications such as instability of spine, chest and back pain,
limited mobility, aggravation of compression and kyphosis, while
the open surgery may lead to paravertebral muscle damage and
denervation due to soft tissue exfoliation and distraction exposure
(1). As a result, some patients have
low confidence in the treatment or feel dissatisfied with the
efficacy because of the intraoperative blood loss and
post-operative residual back pain (2).
Therefore, how to get good curative effect with the
lowest trauma becomes the focus of the research. It is in this
background that minimally invasive surgery appears to overcome the
shortcomings of traditional conservative treatment and open
surgery, making it easier for patients to accept.
In this study, minimally invasive percutaneous
pedicle screws osteosynthesis (MIPPSO) and traditional open pedicle
screws osteosynthesis (TOPSO) were used to treat 120 patients with
simple thoracolumbar fractures and achieved good results. MIPPSO
has been proved not only safe, reliable and effective in curing
thoracolumbar fracture, but also has the advantages of small trauma
and rapid recovery after treatment.
Patients and methods
General information
A retrospective case-control study was conducted in
60 patients with single-stage thoracolumbar fracture in the
Affiliated Jiangyin Hospital of Southeast University Medical School
(Jiangyin, China) from January 2013 to September 2014 and treated
with minimally invasive percutaneous pedicle screw fixation (the
minimally invasive group). At the same time, 60 patients with
thoracolumbar fracture undergoing conventional incision surgery
were selected (the open group). As more patients underwent incision
surgery during the same period than patients with minimally
invasive surgery, we selected patients with similar condition and
injury stage in these two groups. The two surgeries were performed
by the same chief surgeon and his medical team, and all patients
underwent follow-up of no less than one year with a mean follow-up
of 14 months. In addition, the patients were all single
thoracolumbar fracture with no symptoms of lower extremity nerve
damage. This study was approved by the Ethics Committee of the
Affiliated Jiangyin Hospital of Southeast University Medical School
(Jiangyin, China) and the Affiliated Changzhou No. 2 People's
Hospital with Nanjing Medical University (Changzhou, China). Signed
informed consents were obtained from all participants before the
study. The criteria of the enrolled patients were as follows: i)
Patients with unstable thoracolumbar fracture; ii) patients with
thoracolumbar fracture without injury of spinal or spinal nerve;
iii) patients with non-burst fracture or thoracolumbar burst
fracture without spinal canal involved; and iv) patients without
spinal hematoma, foreign body in spinal canal.
Minimally invasive fixation group included 60 cases,
35 males and 25 females aged 23–56 with mean age of 42.8±10.8
years. Injured segments were as follows: T11, 8 cases; T12, 10
cases; L1, 18 cases; L2, 8 cases; L3, 10 cases; and L4, 6 cases.
Causes of injury were 22 cases falling from a height, 26 cases
traffic accidents and 12 cases falling.
Open reduction and internal fixation group consisted
of 60 cases, 36 males and 24 females aged 18–60, with mean age of
43.6±11.2 years. Injured segments were as follows: T11, 8 cases;
T12, 10 cases; L1, 18 cases; L2, 8 cases; L3, 10 cases; and L4, 6
cases. Causes of injury were 24 cases falling from a height, 26
cases traffic accidents and 10 cases falling.
Surgical methods
Prone position was used in minimally invasive group
after general anesthesia with in vitro positioning to
determine and mark the injured vertebra and adjacent vertebra. The
puncture needle was located at 1.0–2.0 cm next to the spinous
process, then 1.5 cm skin incision was cut in each puncture
position. As soon as the articular process was probed by hollow
locator with a core needle, and location and angle confirmed by
C-arm fluoroscopy, we hammered the locator into the vertebral
pedicle ~1.0–1.5 cm deep. Then we pulled the needle out, inserted
Kirschner wire of the same size as the core needle. Protection of
the erector spina muscle was finished by the Kirschner wire,
guiding three sleeve channels through it; the inner two layers of
sleeves were then extracted. After the cutting cone piercing the
vertebral pedicle, we pierced the open cone into thoracic vertebra
for 3.5 cm and lumbar spine for 4.0 cm, then screwed the upper and
lower pedicle screw, respectively. According to the angle needed to
be reset, we pre-bended the longitudinal connecting rod and
penetrated into the longitudinal bar after percutaneous stripping
of muscle under the C-arm fluoroscopy. The plane mark showing
concave toward was applied in the two ends of the connecting rod,
which makes it easy to find if the bar was in the correct position
and direction, then the vertebral body was propped up. Finally the
nut was tightened and fixed with the perspective satisfactorily;
screw tail was then removed and the wound sutured.
Patients in open reduction group took prone position
after general anesthesia, and a posterior midline incision was
made, centered on the injured level. Wiltse approach (3) was performed from the gap between the
multi-muscle and the longest muscle to reveal the injured vertebra
and vertebral facet joint. The location of pedicle screw
implantation was determined by ‘herringbone crest’. Posterior
fixation with a screw rod was directly performed on subjects who
suffered from thoracolumbar burst fractures without neurological
symptoms or simple compression fractures. Once the height of the
vertebral body was satisfactory after being propped up, the wound
was flushed and the drainage tube placed, incision was sutured
layer by layer.
Evaluation indicators
Perioperative data: Perioperative and follow-up
indicators are as follows: the operation time, intraoperative and
post-operative blood loss, the incision length, post-operative
ambulation time and hospital stay, were all used to evaluate the
conditions of the subjects.
Imaging evaluation
i) The anterior vertebral height ratio was measured
pre-operatively at three days, one and 12 months post-operatively
[anterior height ratio of vertebral body = anterior height of
fractured vertebral body/reference anterior height of vertebral
body × l00%; reference anterior height of vertebral body =
(anterior height of superior vertebra + anterior height of inferior
vertebral body)/2]; ii) Cobb's angle was measured respectively,
pre-operative, and 3 days, one and 12 months after the patients
underwent the operation.
Inflammation-related indicators
Serum levels of C-reactive protein (CRP) and
creatine kinase (CK) were measured pre-operatively, 24 and 48 h,
post-operatively.
Assessment of pain
The pain degree was evaluated by visual analog scale
(VAS), and the patient's symptoms were assessed by Oswestry
disability index (ODI).
Statistical analysis
The data were analyzed by SPSS 19.0 (SPSS, Inc.,
Chicago, IL, USA) statistical software. Enumeration data were
analyzed with χ2 test and measurement data presented as
mean ± standard deviation (mean ± SD) with t-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of basic data between the
two groups
Sample number, age, sex, body mass index (BMI) and
injured segments of patients in the two groups have no significant
difference (Table I).
 | Table I.Comparisons of general conditions of
two groups of patients. |
Table I.
Comparisons of general conditions of
two groups of patients.
| Items | MIPPSO group | TOPSO group | P-value |
|---|
| Sex (male/female,
n) | 35/25 | 36/24 | >0.05 |
| Age (mean ± SD,
years) | 42.8±10.8 | 43.6±11.2 | >0.05 |
| BMI
(kg/m2) | 23.3±0.72 | 24.0±0.68 | >0.05 |
| Injured segment
(n) |
| T11 | 8 | 8 |
|
| T12 | 10 | 10 |
|
| L1 | 18 | 18 | 1 |
| L2 | 8 | 8 |
|
| L3 | 10 | 1 |
|
| L4 | 6 | 6 |
|
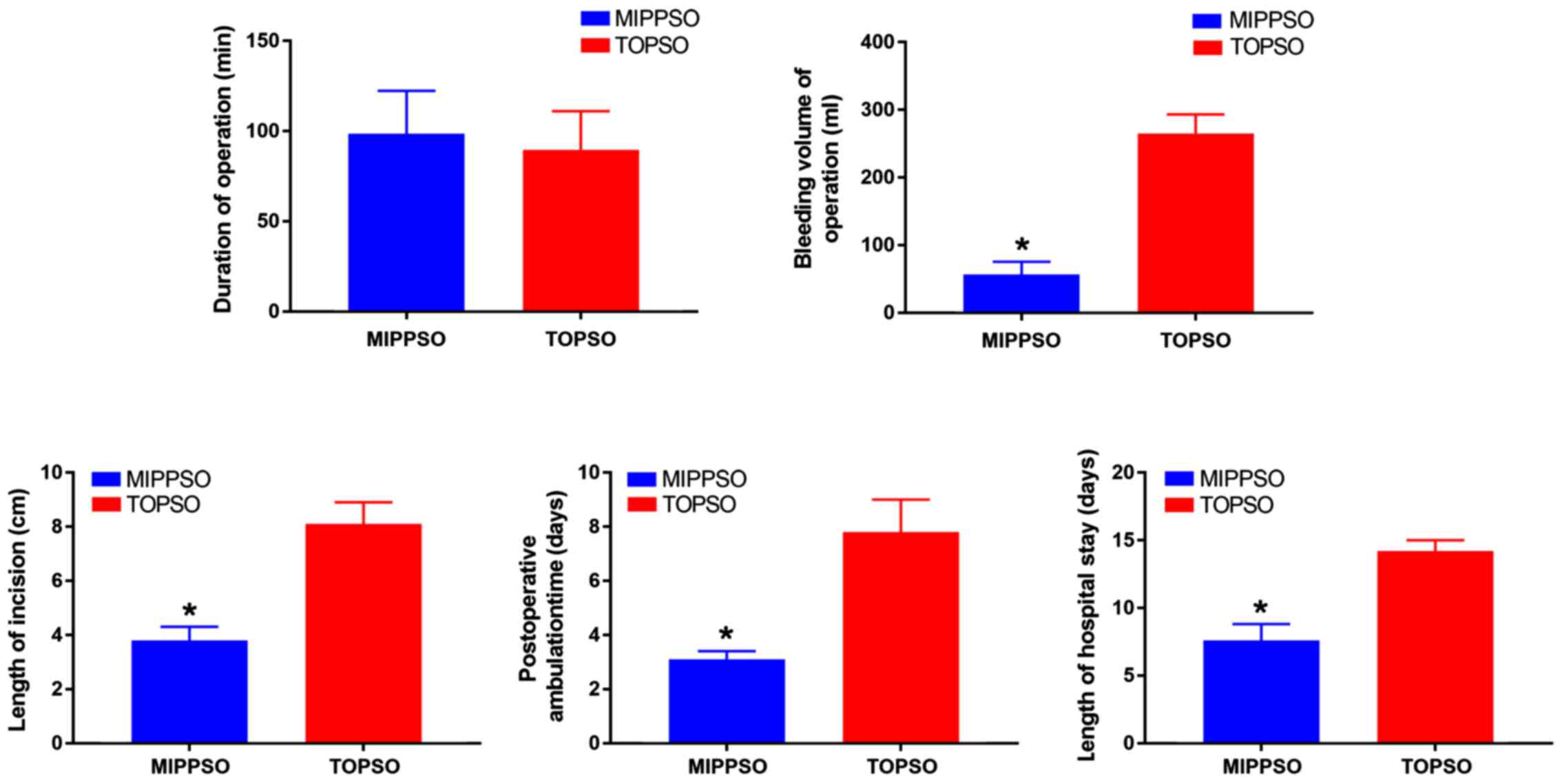
Perioperative data
The operation time in the minimally invasive group
was slightly longer than that in the traditional incision group,
but the difference was not statistically significant. As for the
perioperative blood loss (including intraoperative blood loss and
post-operative drainage), surgical incision length, post-operative
bed rest time and total hospital stay, the minimally invasive group
was superior to the open incision group. The difference was
statistically significant (Fig.
1).
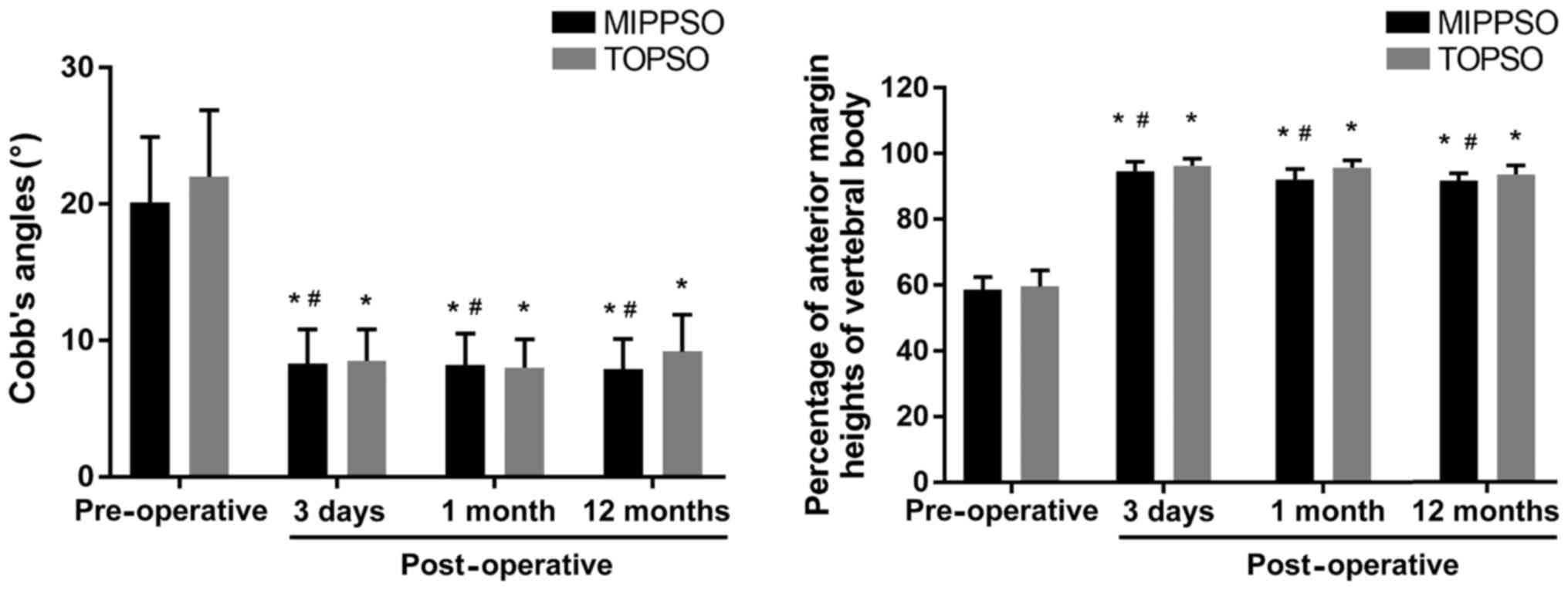
Imageological assessment
The height of the anterior vertebral body and Cobb's
angle of kyphosis were significantly improved in three days, one
and 12 months after operation in both groups. Paired t-test was
used to analyze the post-operative and pre-operative time-points in
both groups; as a result, the difference was statistically
significant (P<0.05). Two independent samples t-test was used to
analyze the difference between the two groups at the same
time-points, and the difference was not statistically significant
(P>0.05) (Fig. 2).
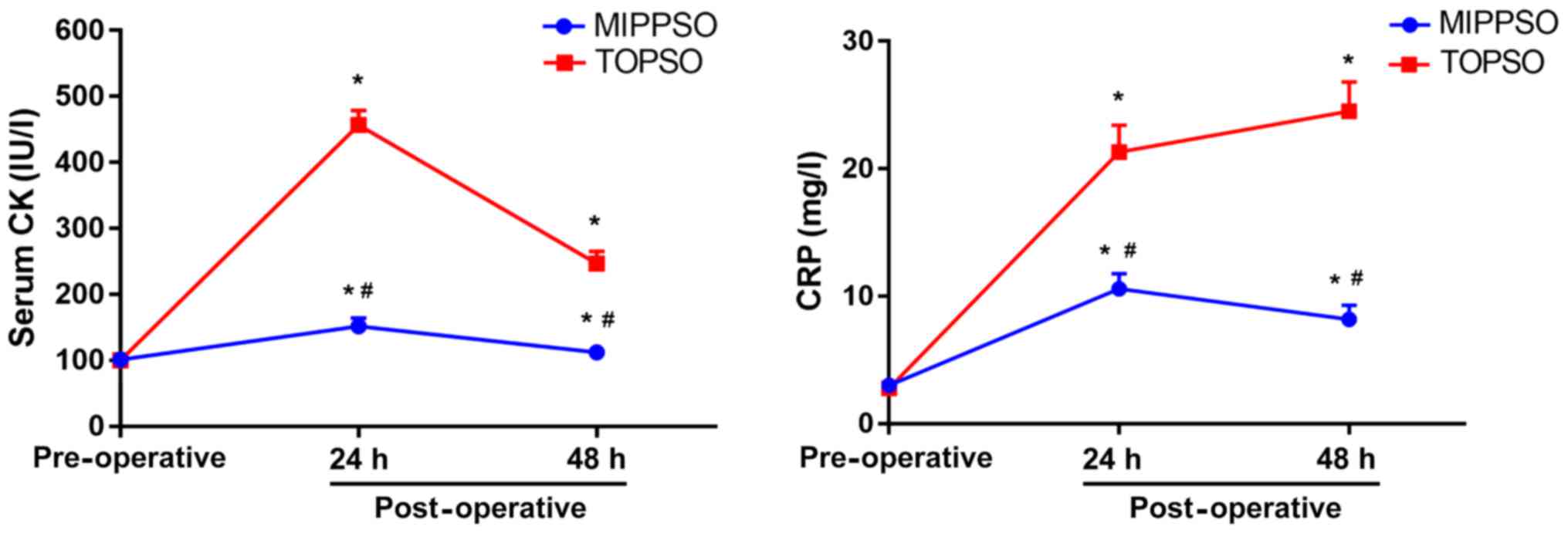
Inflammation-related indicators
There was no conspicuous difference in serum CRP and
CK between the two groups before operation (P>0.05). However, at
24 and 48 h after operation, serum CRP and CK of patients in the
minimally invasive group were significantly lower than those in
open incision group (P<0.05) (Fig.
3).
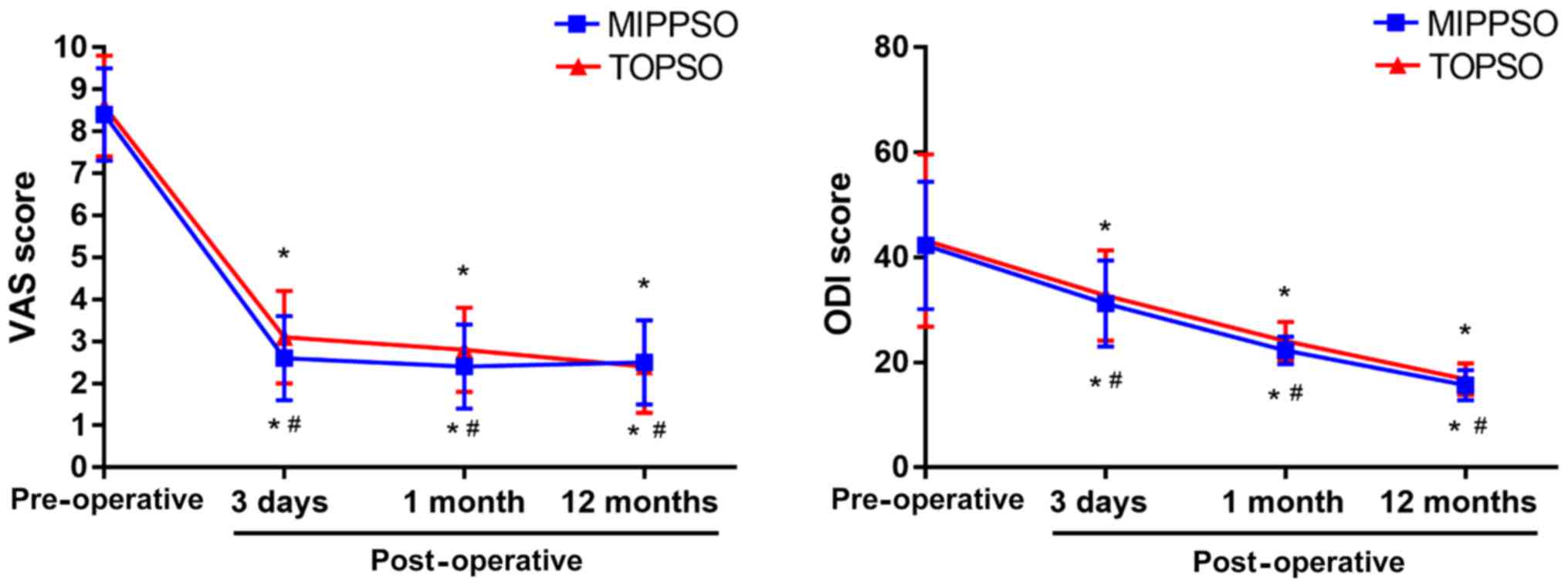
Pain assessment
There were no significant differences in VAS and ODI
scores between the two groups before surgery (P>0.05). However,
VAS and ODI scores of 3 days, 1 month and 12 months after operation
were significantly improved compared with those before operation.
Paired t-test was used to analyze the post-operative and
pre-operative time-points in both groups, and the difference was
statistical significant (P<0.05). Two independent samples t-test
was used to analyze the difference between the two groups at the
same time-points, and the difference was not statistically
significant (P>0.05) (Fig.
4).
Discussion
In the past, TOPSO were mainly applied for the
treatment of lumbar and thoracic fractures, but clinical study
found significant lumbar dysfunction and pain at follow-up after
surgery. Most scholars believe that muscle fibrosis caused by long
time traction of muscle fiber can give rise to the patient's muscle
function decline, muscle fiber edema, and nerve changes (4).
With the continuous development of minimally
invasive medical technology, nerve damage can be avoided in
patients treated with MIPPSO, so that MIPPSO is increasingly widely
used in treatment of lumbar and thoracic fractures. The
pathological area in which the nail is put in does not contain the
main dominant nerve. In addition, this way of treatment does not
require a long time separation and traction of muscle fibers,
avoiding damage to muscle function and muscle fibers as well as
promoting post-operative recovery of patients (5). Lowery and Kulkarni (6) conducted percutaneous minimally invasive
internal fixation and traditional open internal fixation for the
treatment of thoracolumbar fractures. Comparative study showed that
the former operation is simple, safe and reliable with less trauma,
less bleeding, faster recovery, shorter hospital stay, less
complications after internal fixation, under the premise of
strictly taking charge of indications.
Moreover, the effect of deformity correction and
internal fixation in the injured vertebral of MIPPSO was equivalent
to that of traditional open reduction.
Magerl (7) used
MIPPSO for the treatment of thoracolumbar fractures; as a result,
all patients had a good reduction and the vertebral height
maintained well at the final follow-up. Oh et al (8) demonstrated that accuracy of screw
placement of percutaneous minimally invasive fixation system had no
difference with open reduction and internal fixation, which further
proved the safety of the former. Prokop et al (9) compared the efficacy of percutaneous
minimally invasive internal fixation system and traditional open
reduction and internal fixation in the treatment of unstable spinal
fractures. The results showed that operative time and hospital stay
were significantly shorter in the minimally invasive group. Schmidt
et al (10) proved that
transdermal fixation system has advantages for the treatment of
patients with acute thoracolumbar spine trauma. Its short operative
time and minimal blood loss make it suitable for the treatment of
patients who cannot tolerate traditional surgery due to severe
trauma or high surgical risk. The results of our study also
indicate that percutaneous minimally invasive internal fixation
system has the merits of short treatment time, less intraoperative
blood loss, shorter hospital stay, and equal orthodontic effect to
open reduction and internal fixation. This proves again that the
minimally invasive system is feasible and practical.
Compared with open reduction and internal fixation,
requirements for surgeon's skill are higher in the process of
percutaneous minimally invasive internal fixation. The operating
points are as follows: i) The most important is positioning before
internal fixation, so the C-arm performance should be checked and
adjusted to the clearest state. ii) C-arm should be adjusted to
horizontal position after patients adopt prone position. With C-arm
fluoroscopy, the positive phase requires the spinous process to be
located in the bilateral pedicle center to avoid puncture errors.
iii) As soon as the U-shaped groove gets to the articular process,
the screw should be stopped to maintain the universal property.
Putting the screw in too deeply will lead to the difficulty of
linking the connecting rod. iv) Screw extension rod should be kept
universal and the tail end kept a similar length as far as possible
for complete match. v) Intraoperative distraction reduction is
limited, so that it needs to be repeated a few times.
Intraoperative pressure reduction or traction reduction are applied
with distraction. This group of patients are all cooperated with
manual distraction.
In addition to the many advantages, percutaneous
minimally invasive internal fixation systems also have
shortcomings: i) Although percutaneous minimally invasive internal
fixation systems provide ancillary tools for longitudinal
distraction and compression, the effect of distraction reduction of
it is not as good as open reduction and internal fixation due to
its short operable distance (11).
Therefore, it must be cooperated with manual pressing reduction
clinically. ii) Its screws are universal nail and tie rod that
cannot be assembled between the connecting rod, zygapophysis fusion
cannot be operated in surgery, which makes the loss of the mid-long
term correction of vertebral height higher than the open reduction
group (12). In addition,
biomechanical measurements show that the strength of post-operative
vertebral in the direction of flexion and extension is weak. iii)
The system is currently mainly used for simple vertebral
compression fracture and slipping cases without decompression, so
its indications are relatively narrow. However, it is encouraging
that with the improvement of minimally invasive operation and the
joint application with minimally invasive devices, some scholars
have collaborated with the Quadrant system, MED system to
successfully accomplish spinal canal decompression and fusion, and
good effects have been achieved (13,14).
In conclusion, compared with the traditional
incision pedicle screw fixation in the treatment of lumbar and
thoracolumbar fractures, the main advantages of minimally invasive
percutaneous pedicle screw internal fixation are as follows:
shorter operation time, reduced surgical incision and amount of
bleeding, shorter hospital stay and reduced patient trauma.
Furthermore, it can also promote patients' recovery as well as
reduce their post-operative pain. According to patients who
underwent MIPPSO, their lumbar function recovery is better than
that of those who underwent TOPSO and they exhibit evident lumbar
physiological structure recovery after surgery, which suggests that
the use of MIPPSO worth further promotion in clinical
application.
In conclusion, MIPPSO for the treatment of
thoracolumbar fractures can achieve similar clinical effects as
traditional incision surgery. In addition, it has the advantages of
less trauma, less bleeding and shorter post-operative bed rest time
and hospital stay.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural and
Science Foundation (81501874), Jiangsu Province Health and Family
Planning Commission Foundation (Q201511 and QNRC2016139) (all
foundations to KR); The Project of Invigorating Health Care through
Science, Technology and Education (Jiangsu Provincial Medical Youth
Talent) and Changzhou High-level Medical Talents Training Project
(2016CZBJ029) (all foundations to LN).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KR and JT performed the operations for the patients.
XJ and LN collected the patient data. KR and YG analyzed the
patient data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the Affiliated Jiangyin Hospital of Southeast University Medical
School (Jiangyin, China) and the Affiliated Changzhou No. 2
People's Hospital with Nanjing Medical University (Changzhou,
China). Signed informed consents were obtained from the patients or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Boelderl A, Daniaux H, Kathrein A and
Maurer H: Danger of damaging the medial branches of the posterior
rami of spinal nerves during a dorsomedian approach to the spine.
Clin Anat. 15:77–81. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Agrawal A, Mizuno J, Kato Y, Inoue T and
Sano H: Minimally invasive pedicle screw placement in a case of L4
fracture: Case report with review of literature. Asian J Neurosurg.
5:64–69. 2010.PubMed/NCBI
|
|
3
|
Wiltse LL and Spencer CW: New uses and
refinements of the paraspinal approach to the lumbar spine. Spine.
13:696–706. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rodgers WB, Gerber EJ and Patterson J:
Intraoperative and early postoperative complications in extreme
lateral interbody fusion: An analysis of 600 cases. Spine.
36:26–32. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang MY, Vasudevan R and Mindea SA:
Minimally invasive lateral interbody fusion for the treatment of
rostral adjacent-segment lumbar degenerative stenosis without
supplemental pedicle screw fixation. J Neurosurg Spine. 21:861–866.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lowery GL and Kulkarni SS: Posterior
percutaneous spine instrumentation. Eur Spine J. 9 Suppl
1:S126–S130. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Magerl FP: Stabilization of the lower
thoracic and lumbar spine with external skeletal fixation. Clin
Orthop Relat Res. 189:125–141. 1984.
|
|
8
|
Oh HS, Kim JS, Lee SH, Liu WC and Hong SW:
Comparison between the accuracy of percutaneous and open pedicle
screw fixations in lumbosacral fusion. Spine J. 13:1751–1757. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Prokop A, Lohlein F, Chmielnicki M and
Volbracht J: Minimally invasive percutaneous instrumentation for
spine fractures. Unfallchirurg. 112:621–628. 2009.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schmidt OI, Strasser S, Kaufmann V,
Strasser E and Gahr RH: Role of early minimal-invasive spine
fixation in acute thoracic and lumbar spine trauma. Indian J
Orthop. 41:374–380. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang HW, Li CQ, Zhou Y, Zhang ZF, Wang J
and Chu TW: Percutaneous pedicle screw fixation through the pedicle
of fractured vertebra in the treatment of type A thoracolumbar
fractures using Sextant system: An analysis of 38 cases. Chin J
Traumatol. 13:137–145. 2010.PubMed/NCBI
|
|
12
|
Krüger A, Rammler K, Ziring E, Zettl R,
Ruchholtz S and Frangen TM: Percutaneous minimally invasive
instrumentation for traumatic thoracic and lumbar fractures: A
prospective analysis. Acta Orthop Belg. 78:376–381. 2012.PubMed/NCBI
|
|
13
|
Kang H, Cai X, Xu F and Huang Y:
Effectiveness of combined treatment of lumbar spondylolisthesis
with MED, Quadrant, and Sextant-R systems. Zhongguo Xiu Fu Chong
Jian Wai Ke Za Zhi. 27:399–403. 2013.(In Chinese). PubMed/NCBI
|
|
14
|
Sairyo K, Sakai T and Yasui N: Minimally
invasive technique for direct repair of pars interarticularis
defects in adults using a percutaneous pedicle screw and hook-rod
system. J Neurosurg Spine. 10:492–495. 2009. View Article : Google Scholar : PubMed/NCBI
|