|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Aliperti LA, Predina JD, Vachani A and
Singhal S: Local and systemic recurrence is the Achilles heel of
cancer surgery. Ann Surg Oncol. 18:603–607. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jiang JX, Keating JJ, Jesus EM, Judy RP,
Madajewski B, Venegas O, Okusanya OT and Singhal S: Optimization of
the enhanced permeability and retention effect for near-infrared
imaging of solid tumors with indocyanine green. Am J Nucl Med Mol
Imaging. 5:390–400. 2015.PubMed/NCBI
|
|
4
|
Tansi FL, Rüger R, Böhm C, Kontermann RE,
Teichgraeber UK, Fahr A and Hilger I: Potential of activatable
FAP-targeting immunoliposomes in intraoperative imaging of
spontaneous metastases. Biomaterials. 88:70–82. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fedor D, Johnson WR and Singhal S: Local
recurrence following lung cancer surgery: Incidence, risk factors,
and outcomes. Surg Oncol. 22:156–161. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zaman M, Bilal H, Woo CY and Tang A: In
patients undergoing video-assisted thoracoscopic surgery excision,
what is the best way to locate a subcentimetre solitary pulmonary
nodule in order to achieve successful excision? Interact Cardiovasc
Thorac Surg. 15:266–272. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chella A, Lucchi M, Ambrogi MC, Menconi G,
Melfi FM, Gonfiotti A, Boni G and Angeletti CA: A pilot study of
the role of TC-99 radionuclide in localization of pulmonary nodular
lesions for thoracoscopic resection. Eur J Cardiothoracic Surg.
18:17–21. 2000. View Article : Google Scholar
|
|
8
|
Powell TI, Jangra D, Clifton JC,
Lara-Guerra H, Church N, English J, Evans K, Yee J, Coxson H, Mayo
JR and Finley RJ: Peripheral lung nodules: Fluoroscopically guided
video-assisted thoracoscopic resection after computed
tomography-guided localization using platinum microcoils. Ann Surg.
240:481–489. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eichfeld U, Dietrich A, Ott R and Kloeppel
R: Video-assisted thoracoscopic surgery for pulmonary nodules after
computed tomography-guided marking with a spiral wire. Ann Thorac
Surg. 79:313–317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Licha K, Riefke B, Ebert B and Grötzinger
C: Cyanine dyes as contrast agents in biomedical optical imaging.
Acad Radiol. 9 Suppl 2:S320–S322. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Luker GD and Luker KE: Optical imaging:
Current applications and future directions. J Nucl Med. 49:1–4.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
van Dam GM, Themelis G, Crane LM, Harlaar
NJ, Pleijhuis RG, Kelder W, Sarantopoulos A, de Jong JS, Arts HJ,
van der Zee AG, et al: Intraoperative tumor-specific fluorescence
imaging in ovarian cancer by folate receptor-α targeting: First
in-human results. Nat Med. 17:1315–1319. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Polom K, Murawa D, Rho YS, Nowaczyk P,
Hünerbein M and Murawa P: Current trends and emerging future of
indocyanine green usage in surgery and oncology: A literature
review. Cancer. 117:4812–4822. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
van Leeuwen FW, Hardwick JC and van Erkel
AR: Luminescence-based imaging approaches in the field of
interventional molecular imaging. Radiol. 276:12–29. 2015.
View Article : Google Scholar
|
|
15
|
KleinJan GH, Bunschoten A, van den Berg
NS, Olmos RA, Klop WM, Horenblas S, van der Poel HG, Wester HJ and
van Leeuwen FW: Fluorescence guided surgery and tracer-dose, fact
or fiction? Eur J Nucl Med Mol Imaging. 43:1857–1867. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brülisauer M, Moneta G, Jager K and
Bollinger A: Infrared fluorescence videomicroscopy with indocyanine
green (Cardiogreen). Adv Exp Med Biol. 220:219–221. 1987.PubMed/NCBI
|
|
17
|
Chen CY, Fancher RM, Ruan Q, Marathe P,
Rodrigues AD and Yang Z: A liquid chromatography tandem mass
spectrometry method for the quantification of indocyanine green in
dog plasma and bile. J Pharm Biomed Anal. 47:351–359. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Engel E, Schraml R, Maisch T, Kobuch K,
König B, Szeimies RM, Hillenkamp J, Bäumler W and Vasold R:
Light-induced decomposition of indocyanine green. Invest Ophthalmol
Vis Sci. 49:1777–1783. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van der Vorst JR, Schaafsma BE, Hutteman
M, Verbeek FP, Liefers GJ, Hartgrink HH, Smit VT, Löwik CW, van de
Velde CJ, Frangioni JV and Vahrmeijer AL: Near-infrared
fluorescence-guided resection of colorectal liver metastases.
Cancer. 119:3411–3418. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yokoyama N, Otani T, Hashidate H, Maeda C,
Katada T, Sudo N, Manabe S, Ikeno Y, Toyoda A and Katayanagi N:
Real-time detection of hepatic micrometastases from pancreatic
cancer by intraoperative fluorescence imaging: Preliminary results
of a prospective study. Cancer. 118:2813–2819. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rajaraman P, Schwartz BS, Rothman N,
Yeager M, Fine HA, Shapiro WR, Selker RG, Black PM and Inskip PD:
Delta-aminolevulinic acid dehydratase polymorphism and risk of
brain tumors in adults. Environ Health Perspect. 113:1209–1211.
2005. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Iida G, Asano K, Seki M, Ishigaki K,
Teshima K, Yoshida O, Edamura K and Kagawa Y: Intraoperative
identification of canine hepatocellular carcinoma with indocyanine
green fluorescent imaging. J Small Anim Pract. 54:594–600. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gotoh K, Yamada T, Ishikawa O, Takahashi
H, Eguchi H, Yano M, Ohigashi H, Tomita Y, Miyamoto Y and Imaoka S:
A novel image-guided surgery of hepatocellular carcinoma by
indocyanine green fluorescence imaging navigation. J Surg Oncol.
100:75–79. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ishizawa T, Masuda K, Urano Y, Kawaguchi
Y, Satou S, Kaneko J, Hasegawa K, Shibahara J, Fukayama M, Tsuji S,
et al: Mechanistic background and clinical applications of
indocyanine green fluorescence imaging of hepatocellular carcinoma.
Ann Surg Oncol. 21:440–448. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cherrick GR, Stein SW, Leevy CM and
Davidson CS: Indocyanine green: Observations on its physical
properties, plasma decay, and hepatic extraction. J Clin Invest.
39:592–600. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cornelius CE, Ben-Ezzer J and Arias IM:
Binding of sulfobromophthalein sodium (BSP) and other organic
anions by isolated hepatic cell plasma membranes in vitro.
Proc Soc Exp Biol Med. 124:665–667. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hunton DB, Bollman JL and Hoffman HN:
Studies of hepatic function with indocyanine green.
Gastroenterology. 39:713–724. 1960.PubMed/NCBI
|
|
28
|
Leevy CM and Bender J: Physiology of dye
extraction by the liver: Comparative studies of sulfobromophthalein
and indocyanine green. Ann NY Acad Sci. 111:161–176. 1963.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shibasaki Y, Sakaguchi T, Hiraide T,
Morita Y, Suzuki A, Baba S, Setou M and Konno H: Expression of
indocyanine green-related transporters in hepatocellular carcinoma.
J Surg Res. 193:567–576. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Holt D, Okusanya O, Judy R, Venegas O,
Jiang J, DeJesus E, Eruslanov E, Quatromoni J, Bhojnagarwala P,
Deshpande C, et al: Intraoperative near-infrared imaging can
distinguish cancer from normal tissue but not inflammation. PLoS
One. 9:e1033422014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kosaka N, Mitsunaga M, Longmire MR, Choyke
PL and Kobayashi H: Near infrared fluorescence-guided real-time
endoscopic detection of peritoneal ovarian cancer nodules using
intravenously injected indocyanine green. Int J Cancer.
129:1671–1677. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Maeda H, Nakamura H and Fang J: The EPR
effect for macromolecular drug delivery to solid tumors:
Improvement of tumor uptake, lowering of systemic toxicity, and
distinct tumor imaging in vivo. Adv Drug Deliv Rev. 65:71–79. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Madajewski B, Judy BF, Mouchli A, Kapoor
V, Holt D, Wang MD, Nie S and Singhal S: Intraoperative
near-infrared imaging of surgical wounds after tumor resections can
detect residual disease. Clin Cancer Res. 18:5741–5751. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Shin EH, Li Y, Kumar U, Sureka HV, Zhang X
and Payne CK: Membrane potential mediates the cellular binding of
nanoparticles. Nanoscale. 5:5879–5886. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Matsumura Y and Maeda H: A new concept for
macromolecular therapeutics in cancer chemotherapy: Mechanism of
tumoritropic accumulation of proteins and the antitumor agent
smancs. Cancer Res. 46:6387–6392. 1986.PubMed/NCBI
|
|
36
|
Heneweer C, Holland JP, Divilov V, Carlin
S and Lewis JS: Magnitude of enhanced permeability and retention
effect in tumors with different phenotypes: 89Zr-albumin as a model
system. J Nucl Med. 52:625–633. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
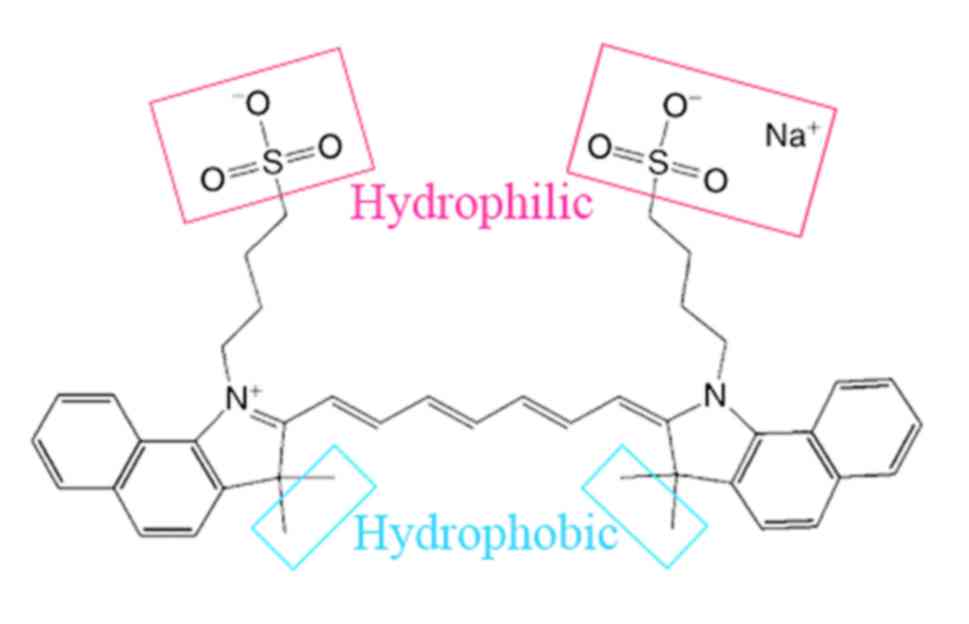
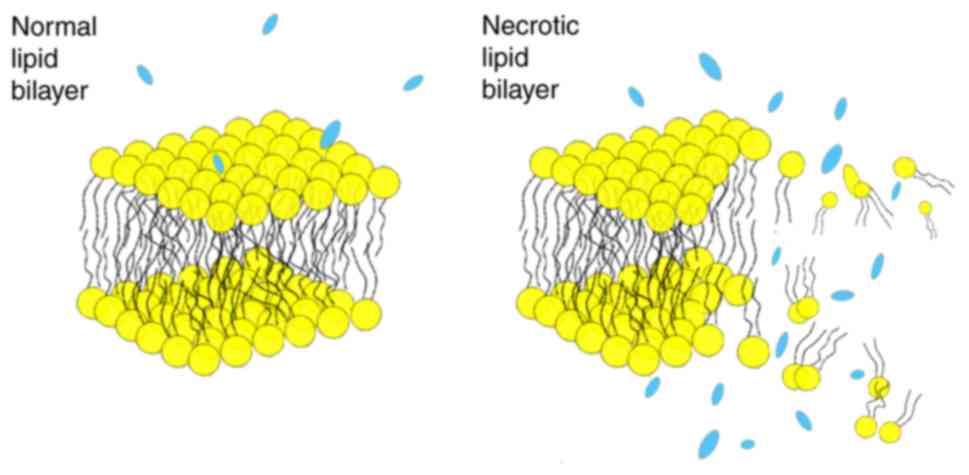
Fang C, Wang K, Zeng C, Chi C, Shang W, Ye
J, Mao Y, Fan Y, Yang J, Xiang N, et al: Illuminating necrosis:
From mechanistic exploration to preclinical application using
fluorescence molecular imaging with indocyanine green. Sci Rep.
6:210132016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hyun H, Park MH, Owens EA, Wada H, Henary
M, Handgraaf HJ, Vahrmeijer AL, Frangioni JV and Choi HS:
Structure-inherent targeting of near-infrared fluorophores for
parathyroid and thyroid gland imaging. Nat Med. 21:192–197. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yoneya S, Saito T, Komatsu Y, Koyama I,
Takahashi K and Duvoll-Young J: Binding properties of indocyanine
green in human blood. Invest Ophthalmol Vis Sci. 39:1286–1290.
1998.PubMed/NCBI
|
|
40
|
Baker KJ: Binding of sulfobromophthalein
(BSP) sodium and indocyanine green (ICG) by plasma alpha-1
lipoproteins. Proc Soc Exp Biol Med. 122:957–963. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Janecki J and Krawcynski J: Labeling with
indocyanine green of serum protein from normal persons and patients
with acute viral hepatitis. Clin Chem. 16:1008–1011.
1970.PubMed/NCBI
|
|
42
|
Desmettre T, Devoisselle JM and Mordon S:
Fluorescence properties and metabolic features of indocyanine green
(ICG) as related to angiography. Surv Ophthalmol. 45:15–27. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Onda N, Kimura M, Yoshida T and Shibutani
M: Preferential tumor cellular uptake and retention of indocyanine
green for in vivo tumor imaging. Int J Cancer. 139:673–682. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
von Kleist L, Stahlschmidt W, Bulut H,
Gromova K, Puchkov D, Robertson MJ, MacGregor KA, Tomilin N,
Pechstein A, Chau N, et al: Role of the clathrin terminal domain in
regulating coated pit dynamics revealed by small molecule
inhibition. Cell. 146:471–484. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kaibori M, Matsui K, Ishizaki M, Iida H,
Okumura T, Sakaguchi T, Inoue K, Ikeura T, Asano H and Kon M:
Intraoperative detection of superficial liver tumors by
fluorescence imaging using indocyanine green and 5-aminolevulinic
acid. Anticancer Res. 36:1841–1849. 2016.PubMed/NCBI
|
|
46
|
Hill TK, Abdulahad A, Kelkar SS, Marini
FC, Long TE, Provenzale JM and Mohs AM: Indocyanine green-loaded
nanoparticles for image-guided tumor surgery. Bioconjug Chem.
26:294–303. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
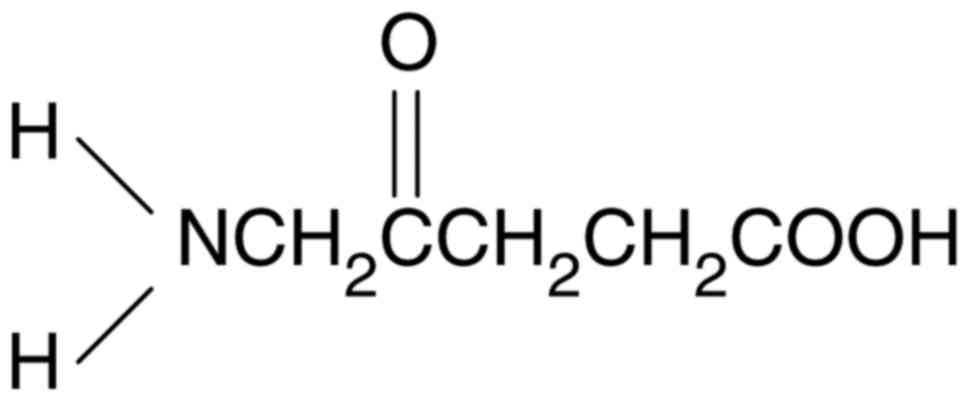
Ishizuka M, Abe F, Sano Y, Takahashi K,
Inoue K, Nakajima M, Kohda T, Komatsu N, Ogura S and Tanaka T:
Novel development of 5-aminolevurinic acid (ALA) in cancer
diagnoses and therapy. Int Immunopharmacol. 11:358–365. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Nakamura M, Nishikawa J, Hamabe K, Goto A,
Nishimura J, Shibata H, Nagao M, Sasaki S, Hashimoto S, Okamoto T
and Sakaida I: Preliminary study of photodynamic diagnosis using
5-aminolevulinic acid in gastric and colorectal tumors. World J
Gastroenterol. 21:6706–6712. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
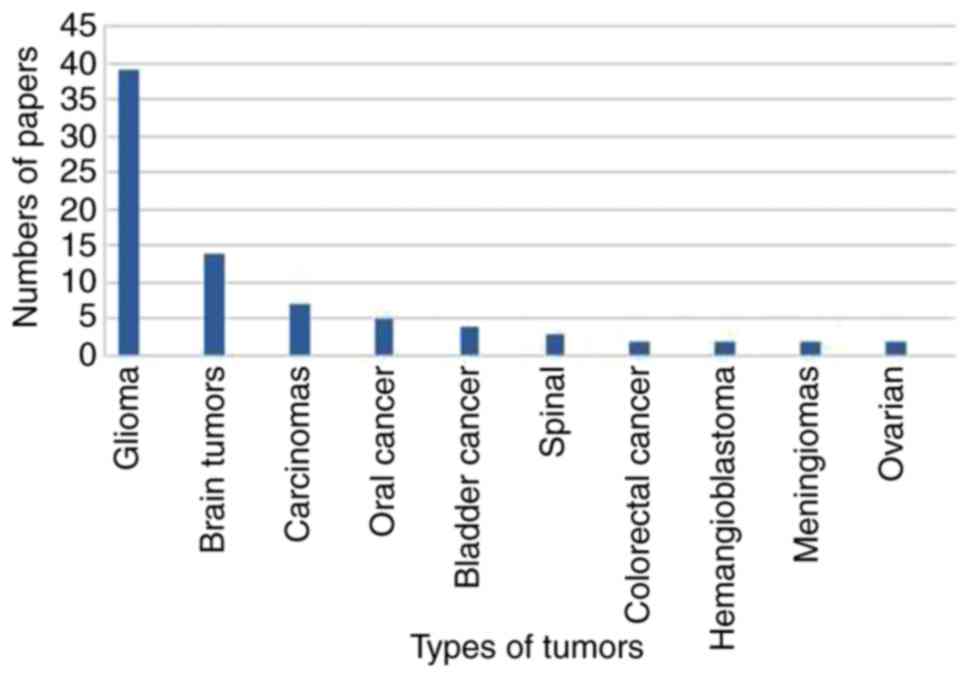
Leroy HA, Vermandel M, Lejeune JP, Mordon
S and Reyns N: Fluorescence guided resection and glioblastoma in
2015: A review. Lasers Surg Med. 47:441–451. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kitada M, Ohsaki Y, Matsuda Y, Hayashi S
and Ishibashi K: Photodynamic diagnosis of pleural malignant
lesions with a combination of 5-aminolevulinic acid and intrinsic
fluorescence observation systems. BMC Cancer. 15:1742015.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Friesen SA, Hjortland GO, Madsen SJ,
Hirschberg H, Engebraten O, Nesland JM and Peng Q: 5-Aminolevulinic
acid-based photodynamic detection and therapy of brain tumors
(review). Int J Oncol. 21:577–582. 2002.PubMed/NCBI
|
|
52
|
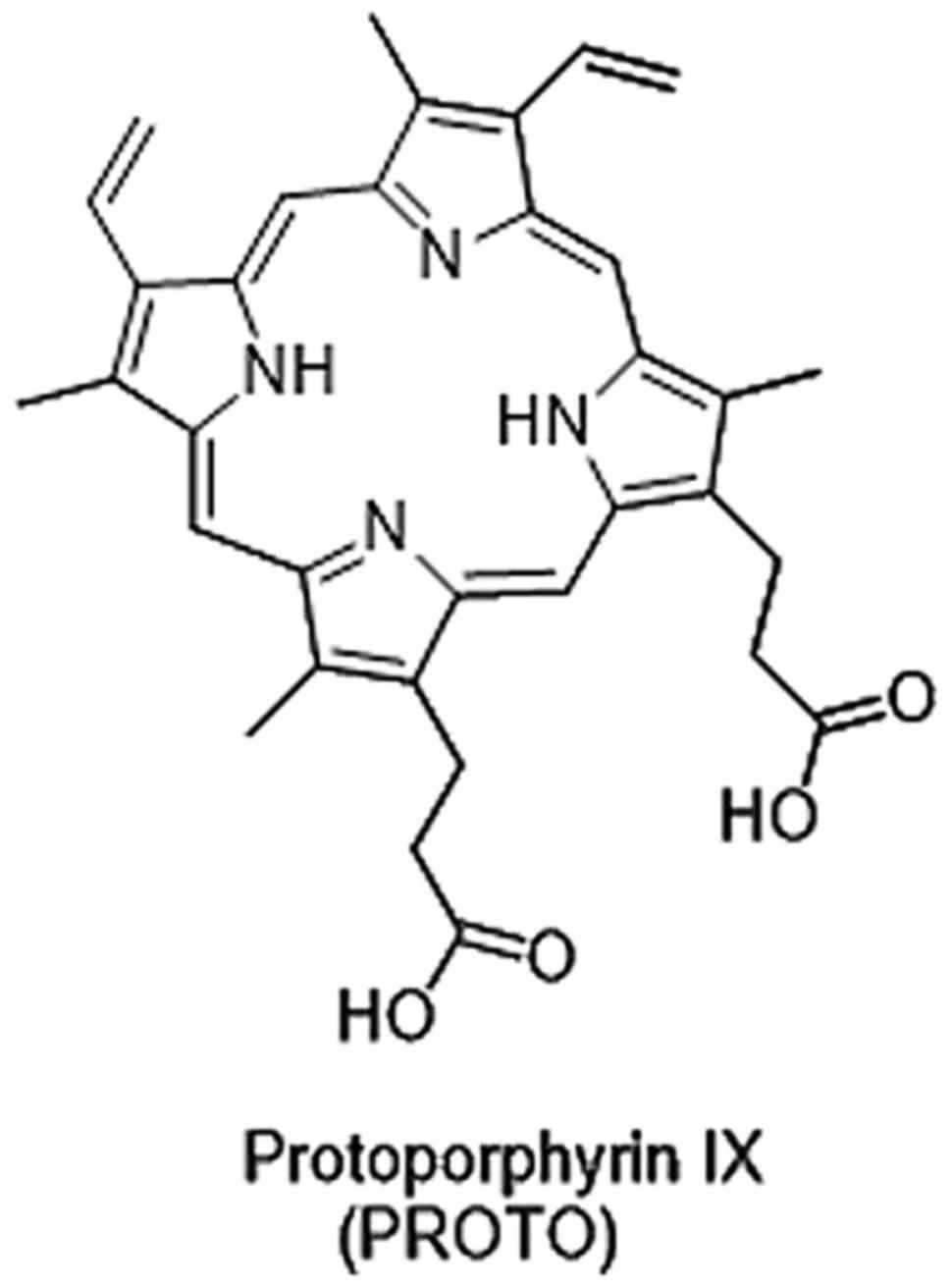
Colditz MJ and Jeffree RL: Aminolevulinic
acid (ALA)-protoporphyrin IX fluorescence guided tumour resection.
Part 1: Clinical, radiological and pathological studies. J Clin
Neurosci. 19:1471–1474. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Colditz MJ, Leyen K and Jeffree RL:
Aminolevulinic acid (ALA)-protoporphyrin IX fluorescence guided
tumour resection. Part 2: Theoretical, biochemical and practical
aspects. J Clin Neurosci. 19:1611–1616. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Eljamel S: 5-ALA fluorescence image guided
resection of glioblastoma multiforme: A meta-analysis of the
literature. Int J Mol Sci. 16:10443–10456. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Nokes B, Apel M, Jones C, Brown G and Lang
JE: Aminolevulinic acid (ALA): Photodynamic detection and potential
therapeutic applications. J Surg Res. 181:262–271. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yang X, Palasuberniam P, Kraus D and Chen
B: Aminolevulinic acid-based tumor detection and therapy: Molecular
mechanisms and strategies for enhancement. Int J Mol Sci.
16:25865–25880. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Ponka P: Cell biology of heme. Am J Med
Sci. 318:241–256. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kemmner W, Wan K, Rüttinger S, Ebert B,
Macdonald R, Klamm U and Moesta KT: Silencing of human
ferrochelatase causes abundant protoporphyrin-IX accumulation in
colon cancer. FASEB J. 22:500–509. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Hooda J, Cadinu D, Alam MM, Shah A, Cao
TM, Sullivan LA, Brekken R and Zhang L: Enhanced heme function and
mitochondrial respiration promote the progression of lung cancer
cells. PloS One. 8:e634022013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Gonçalves TL, Erthal F, Corte CL, Müller
LG, Piovezan CM, Nogueira CW and Rocha JB: Involvement of oxidative
stress in the pre-malignant and malignant states of cervical cancer
in women. Clin Biochem. 38:1071–1075. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Neslund-Dudas C, Levin AM, Rundle A,
Beebe-Dimmer J, Bock CH, Nock NL, Jankowski M, Datta I, Krajenta R,
Dou QP, et al: Case-only gene-environment interaction between ALAD
tagSNPs and occupational lead exposure in prostate cancer.
Prostate. 74:637–646. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Navone NM, Polo CF, Frisardi AL, Andrade
NE and Battle AM: Heme biosynthesis in human breast cancer-mimetic
‘in vitro’ studies and some heme enzymic activity levels. Int J
Biochem. 22:1407–1411. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Krieg RC, Fickweiler S, Wolfbeis OS and
Knuechel R: Cell-type specific protoporphyrin IX metabolism in
human bladder cancer in vitro. Photochem Photobiol.
72:226–233. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Krieg RC, Messmann H, Rauch J, Seeger S
and Knuechel R: Metabolic characterization of tumor cell-specific
protoporphyrin IX accumulation after exposure to 5-aminolevulinic
acid in human colonic cells. Photochem Photobiol. 76:518–525. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Hinnen P, de Rooij FW, van Velthuysen ML,
Edixhoven A, van Hillegersberg R, Tilanus HW, Wilson JH and
Siersema PD: Biochemical basis of 5-aminolaevulinic acid-induced
protoporphyrin IX accumulation: A study in patients with
(pre)malignant lesions of the oesophagus. Br J Cancer. 78:679–682.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Hinnen P, de Rooij FW, Terlouw EM,
Edixhoven A, van Dekken H, van Hillegersberg R, Tilanus HW, Wilson
JH and Siersema PD: Porphyrin biosynthesis in human Barrett's
oesophagus and adenocarcinoma after ingestion of 5-aminolaevulinic
acid. Br J Cancer. 83:539–543. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Misawa Y, Tojo A and Shibuya M: Isolation
of genes highly expressed in early and late stages of Friend
virus-induced erythroleukemia in mice. Biochem Biophys Res Commun.
170:39–45. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ito E, Yue S, Moriyama EH, Hui AB, Kim I,
Shi W, Alajez NM, Bhogal N, Li G, Datti A, et al: Uroporphyrinogen
decarboxylase is a radiosensitizing target for head and neck
cancer. Sci Transl Med. 3:67ra672011. View Article : Google Scholar
|
|
69
|
Dailey HA and Smith A: Differential
interaction of porphyrins used in photoradiation therapy with
ferrochelatase. Biochem J. 223:441–445. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Miyake M, Ishii M, Kawashima K, Kodama T,
Sugano K, Fujimoto K and Hirao Y: siRNA-mediated knockdown of the
heme synthesis and degradation pathways: Modulation of treatment
effect of 5-aminolevulinic acid-based photodynamic therapy in
urothelial cancer cell lines. Photochem Photobiol. 85:1020–1027.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Teng L, Nakada M, Zhao SG, Endo Y,
Furuyama N, Nambu E, Pyko IV, Hayashi Y and Hamada JI: Silencing of
ferrochelatase enhances 5-aminolevulinic acid-based fluorescence
and photodynamic therapy efficacy. Br J Cancer. 104:798–807. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yang X, Li W, Palasuberniam P, Myers KA,
Wang C and Chen B: Effects of silencing heme biosynthesis enzymes
on 5-aminolevulinic acid-mediated protoporphyrin IX fluorescence
and photodynamic therapy. Photochem Photobiol. 91:923–930. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Frezza C, Zheng L, Folger O, Rajagopalan
KN, MacKenzie ED, Jerby L, Micaroni M, Chaneton B, Adam J, Hedley
A, et al: Haem oxygenase is synthetically lethal with the tumour
suppressor fumarate hydratase. Nature. 477:225–228. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Ward PS and Thompson CB: Metabolic
reprogramming: A cancer hallmark even warburg did not anticipate.
Cancer Cell. 21:297–308. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ohgari Y, Nakayasu Y, Kitajima S, Sawamoto
M, Mori H, Shimokawa O, Matsui H and Taketani S: Mechanisms
involved in delta-aminolevulinic acid (ALA)-induced
photosensitivity of tumor cells: Relation of ferrochelatase and
uptake of ALA to the accumulation of protoporphyrin. Biochem
Pharmacol. 71:42–49. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Gibson SL, Nguyen ML, Havens JJ, Barbarin
A and Hilf R: Relationship of delta-aminolevulinic acid-induced
protoporphyrin IX levels to mitochondrial content in neoplastic
cells in vitro. Biochem Biophys Res Commun. 265:315–321.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Gibson SL, Havens JJ, Foster TH and Hilf
R: Time-dependent intracellular accumulation of
delta-aminolevulinic acid, induction of porphyrin synthesis and
subsequent phototoxicity. Photochem Photobiol. 65:416–421. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Nakanishi T, Ogawa T, Yanagihara C and
Tamai I: Kinetic evaluation of determinant factors for cellular
accumulation of protoporphyrin IX induced by external
5-aminolevulinic acid for photodynamic cancer therapy. J Pharm Sci.
104:3092–3100. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Krishnamurthy PC, Du G, Fukuda Y, Sun D,
Sampath J, Mercer KE, Wang J, Sosa-Pineda B, Murti KG and Schuetz
JD: Identification of a mammalian mitochondrial porphyrin
transporter. Nature. 443:586–589. 2006.PubMed/NCBI
|
|
80
|
Zhao SG, Chen XF, Wang LG, Yang G, Han DY,
Teng L, Yang MC, Wang DY, Shi C, Liu YH, et al: Increased
expression of ABCB6 enhances protoporphyrin IX accumulation and
photodynamic effect in human glioma. Ann Surg Oncol. 20:4379–4388.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Paterson JK, Shukla S, Black CM, Tachiwada
T, Garfield S, Wincovitch S, Ernst DN, Agadir A, Li X, Ambudkar SV,
et al: Human ABCB6 localizes to both the outer mitochondrial
membrane and the plasma membrane. Biochemistry. 46:9443–9452. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Tsuchida M, Emi Y, Kida Y and Sakaguchi M:
Human ABC transporter isoform B6 (ABCB6) localizes primarily in the
Golgi apparatus. Biochem Biophys Res Commun. 369:369–375. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Matsumoto K, Hagiya Y, Endo Y, Nakajima M,
Ishizuka M, Tanaka T and Ogura S: Effects of plasma membrane ABCB6
on 5-aminolevulinic acid (ALA)-induced porphyrin accumulation in
vitro: Tumor cell response to hypoxia. Photodiagnosis Photodyn
Ther. 12:45–51. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Robey RW, Steadman K, Polgar O and Bates
SE: ABCG2-mediated transport of photosensitizers: Potential impact
on photodynamic therapy. Cancer Biol Ther. 4:187–194. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Barron GA, Moseley H and Woods JA:
Differential sensitivity in cell lines to photodynamic therapy in
combination with ABCG2 inhibition. J Photochem Photobiol B.
126:87–96. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Ogawa M, Kosaka N, Choyke PL and Kobayashi
H: H-type dimer formation of fluorophores: A mechanism for
activatable, in vivo optical molecular imaging. ACS Chem Biol.
4:535–546. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Tansi F, Kallweit E, Kaether C, Kappe K,
Schumann C, Hilger I and Reissmann S: Internalization of
near-infrared fluorescently labeled activatable cell-penetrating
peptide and of proteins into human fibrosarcoma cell line HT-1080.
J Cell Biochem. 116:1222–1231. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Rizzo LY, Theek B, Storm G, Kiessling F
and Lammers T: Recent progress in nanomedicine: Therapeutic,
diagnostic and theranostic applications. Curr Opin Biotechnol.
24:1159–1166. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Tansi FL, Rüger R, Rabenhold M, Steiniger
F, Fahr A, Kaiser WA and Hilger I: Liposomal encapsulation of a
near-infrared fluorophore enhances fluorescence quenching and
reliable whole body optical imaging upon activation in vivo. Small.
9:3659–3669. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Rüger R, Tansi FL, Rabenhold M, Steiniger
F, Kontermann RE, Fahr A and Hilger I: In vivo near-infrared
fluorescence imaging of FAP-expressing tumors with activatable
FAP-targeted, single-chain Fv-immunoliposomes. J Control Release.
186:1–10. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Kalluri R and Zeisberg M: Fibroblasts in
cancer. Nat Rev Cancer. 6:392–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Huang Y, Simms AE, Mazur A, Wang S, León
NR, Jones B, Aziz N and Kelly T: Fibroblast activation
protein-alpha promotes tumor growth and invasion of breast cancer
cells through non-enzymatic functions. Clin Exp Metastasis.
28:567–579. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Lee HO, Mullins SR, Franco-Barraza J,
Valianou M, Cukierman E and Cheng JD: FAP-overexpressing
fibroblasts produce an extracellular matrix that enhances invasive
velocity and directionality of pancreatic cancer cells. BMC Cancer.
11:2452011. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zhi K, Shen X, Zhang H and Bi J:
Cancer-associated fibroblasts are positively correlated with
metastatic potential of human gastric cancers. J Exp Clin Cancer
Res. 29:662010. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Tommelein J, Verset L, Boterberg T,
Demetter P, Bracke M and De Wever O: Cancer-associated fibroblasts
connect metastasis-promoting communication in colorectal cancer.
Front Oncol. 5:632015. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Garin-Chesa P, Old LJ and Rettig WJ: Cell
surface glycoprotein of reactive stromal fibroblasts as a potential
antibody target in human epithelial cancers. Proc Natl Acad Sci
USA. 87:7235–7239. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Albert MB, Steinberg WM and Henry JP:
Elevated serum levels of tumor marker CA19-9 in acute cholangitis.
Dig Dis Sci. 33:1223–1225. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Benamouzig R, Buffet C, Fourre C, Ink O,
Moati F and Etienne JP: Serum levels of carbohydrate antigenic
determinant (CA 19.9) in obstructive jaundice. Dig Dis Sci.
34:1640–1642. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Encabo G and Ruibal A: Seric CA 19.9
levels in patients with non tumoral pathologies. Our experience in
892 cases. Bull Cancer. 73:256–259. 1986.PubMed/NCBI
|
|
100
|
Gupta MK, Arciaga R, Bocci L, Tubbs R,
Bukowski R and Deodhar SD: Measurement of a
monoclonal-antibody-defined antigen (CA19-9) in the sera of
patients with malignant and nonmalignant diseases. Comparison with
carcinoembryonic antigen. Cancer. 56:277–283. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Haglund C, Roberts PJ, Jalanko H and
Kuusela P: Tumour markers CA 19-9 and CA 50 in digestive tract
malignancies. Scand J Gastroenterol. 27:169–174. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Loy TS, Sharp SC, Andershock CJ and Craig
SB: Distribution of CA 19-9 in adenocarcinomas and transitional
cell carcinomas. An immunohistochemical study of 527 cases. Am J
Clin Pathol. 99:726–728. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Makovitzky J: The distribution and
localization of the monoclonal antibody-defined antigen 19-9
(CA19-9) in chronic pancreatitis and pancreatic carcinoma. An
immunohistochemical study. Virchows Arch B Cell Pathol Incl Mol
Pathol. 51:535–544. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Magnani JL, Steplewski Z, Koprowski H and
Ginsburg V: Identification of the gastrointestinal and pancreatic
cancer-associated antigen detected by monoclonal antibody 19-9 in
the sera of patients as a mucin. Cancer Res. 43:5489–5492.
1983.PubMed/NCBI
|
|
105
|
Girgis MD, Kenanova V, Olafsen T, McCabe
KE, Wu AM and Tomlinson JS: Anti-CA19-9 diabody as a PET imaging
probe for pancreas cancer. J Surg Res. 170:169–178. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Sawada R, Sun SM, Wu X, Hong F, Ragupathi
G, Livingston PO and Scholz WW: Human monoclonal antibodies to
sialyl-Lewis (CA19.9) with potent CDC, ADCC, and antitumor
activity. Clin Cancer Res. 17:1024–1032. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Houghton JL, Zeglis BM, Abdel-Atti D,
Aggeler R, Sawada R, Agnew BJ, Scholz WW and Lewis JS:
Site-specifically labeled CA19.9-targeted immunoconjugates for the
PET, NIRF, and multimodal PET/NIRF imaging of pancreatic cancer.
Proc Natl Acad Sci USA. 112:15850–15855. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Li CH, Kuo TR, Su HJ, Lai WY, Yang PC,
Chen JS, Wang DY, Wu YC and Chen CC: Fluorescence-guided probes of
aptamer-targeted gold nanoparticles with computed tomography
imaging accesses for in vivo tumor resection. Sci Rep. 5:156752015.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Góra J and Latajka R: Involvement of
cysteine proteases in cancer. Curr Med Chem. 22:944–957. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Ofori LO, Withana NP, Prestwood TR,
Verdoes M, Brady JJ, Winslow MM, Sorger J and Bogyo M: Design of
protease activated optical contrast agents that exploit a latent
lysosomotropic effect for use in fluorescence-guided surgery. ACS
Chem Biol. 10:1977–1988. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Kelemen LE: The role of folate receptor
alpha in cancer development, progression and treatment: Cause,
consequence or innocent bystander? Int J Cancer. 119:243–250. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Low PS and Antony AC: Folate
receptor-targeted drugs for cancer and inflammatory diseases. Adv
Drug Deliv Rev. 56:1055–1058. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Low PS, Henne WA and Doorneweerd DD:
Discovery and development of folic-acid-based receptor targeting
for imaging and therapy of cancer and inflammatory diseases. Acc
Chem Res. 41:120–129. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Low PS and Kularatne SA: Folate-targeted
therapeutic and imaging agents for cancer. Curr Opin Chem Biol.
13:256–262. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Lu Y, Sega E and Low PS: Folate
receptor-targeted immunotherapy: Induction of humoral and cellular
immunity against hapten-decorated cancer cells. Int J Cancer.
116:710–719. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Lu Y, Xu LC, Parker N, Westrick E, Reddy
JA, Vetzel M, Low PS and Leamon CP: Preclinical pharmacokinetics,
tissue distribution, and antitumor activity of a folate-hapten
conjugate-targeted immunotherapy in hapten-immunized mice. Mol
Cancer Ther. 5:3258–3267. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
O'Shannessy DJ, Yu G, Smale R, Fu YS,
Singhal S, Thiel RP, Somers EB and Vachani A: Folate receptor alpha
expression in lung cancer: Diagnostic and prognostic significance.
Oncotarget. 3:414–425. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
De Jesus E, Keating JJ, Kularatne SA,
Jiang J, Judy R, Predina J, Nie S, Low P and Singhal S: Comparison
of folate receptor targeted optical contrast agents for
intraoperative molecular imaging. Int J Mol Imaging.
2015:4690472015. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Srinivasarao M, Galliford CV and Low PS:
Principles in the design of ligand-targeted cancer therapeutics and
imaging agents. Nat Rev Drug Discov. 14:203–219. 2015. View Article : Google Scholar : PubMed/NCBI
|