Introduction
Various case reports have described congenital
abnormalities of the unilateral hematocolpos and ipsilateral renal
agenesis (1–3). In 1985, Bian named this condition
congenital vaginal oblique septum syndrome (CVOS) (4) and it is also known as
Herlyn-Werner-Wunderlich syndrome (3,5,6). CVOS is usually caused by congenital
malformation in the vagina, which results in the development of a
double uterus and cervix (6). There
is also an oblique diaphragm from the cervical side to the bottom
of unilateral vaginal wall, known as the vaginal oblique septum,
which blocks lateral cervical pathways (7). The effusion lacuna caused by
obstruction is known as behind-septum vaginal cavity (7). Renal agenesis usually occurs in
patients with the malformation on the oblique septum side due to
embryonal dysplasia (7). Clinically,
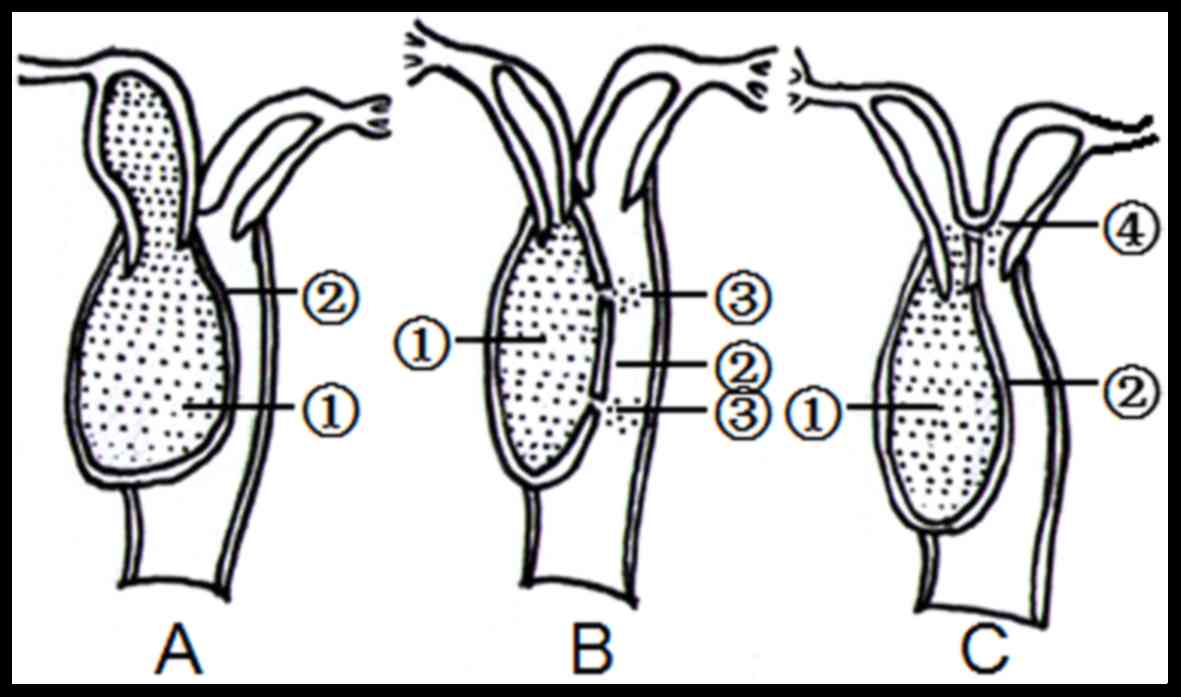
there are three types of CVOS: Types I, II and III (4,6).
Patients with type I CVOS do not possess a hole in the oblique
septum and the attachment of the uterus to the vagina is normal
(6,8). However, these patients have an
additional uterus behind the septum that is entirely isolated from
the contralateral uterus (6,8). Menstrual blood is retained behind the
septum vaginal cavity and in certain cases, the uterine cavity.
Patients with type II CVOS exhibit a hole several mm thick in the
reclined septum through which menstrual blood can flow (6,8).
Patients with type III CVOS possess no hole in the oblique septum,
but exhibit a cervical fistula between the two lateral cervixes or
between the cavity behind the septum and contralateral cervix
(6,8). Menstrual blood on the oblique septum
may drain through the contralateral cervix (4). As CVOS is a very rare syndrome, it is
easily misdiagnosed and the treatment is often delayed (6). Early accurate diagnosis and resection
of the oblique vaginal septum are therefore important, emphasizing
the need to recognize the syndrome early (6). The purpose of the current study was to
identify the features of CVOS detected by ultrasound, classify the
lesion types of CVOS and to compare the results of the ultrasound
with the intraoperative and pathology results.
Patients and methods
Patients
Between December 1996 and September 2015, 21 female
patients with suspected CVOS were included in the current
retrospective study from the Provincial Hospital Affiliated to
Shandong University (Jinan, Shandong), the People's Hospital of
Linyi City (Linyi, Shandong) and Heze Municipal Hospital (Heze,
Shandong). These patients included 15 already included in a
previous study (8). For the present
study, a further 6 patients were identified based on sonogram and
one of them who underwent magnetic resonance imaging examination
showed the same result. The mean age of the patients was 17.29±5.69
years old (range, 13–32 years). Patients without typical ultrasonic
features were excluded. A grey-scale pelvic ultrasound was
performed to evaluate the uterus, vagina and kidneys prior to
surgery. A total of 15 patients with type I CVOS received surgery
immediately following the confirmation of diagnosis. Excluding a
patient with type III CVOS who received surgery whilst 17 weeks
pregnant, the remainder of patients also underwent surgery once the
diagnosis was confirmed. Transvaginal resection of the reclined
septum was performed in all patients. All 15 patients with type I
CVOS had both normal menstrual cycles and dysmenorrheal unilateral
abdominal pain. Dysmenorrhea was preliminarily less severe, but
increased in severity over time. The mean duration from the first
menstruation to operation was 6.67±2.06 months in type I (mean
duration of dysmenorrhea, 3.60±1.68 months), 27.00±13.60 months in
type II (mean duration of symptoms, 23.2±12.42 months) and 134
months in type III (excluding the pregnant patient). Excluding
dysmenorrhea, the remaining 6 patients with type II and type III
also exhibited menstrual extension and vaginal purulent drainage.
Vaginal or rectal examination revealed masses of various sizes
beside the normal vagina in all patients.
Ultrasonic examination
Grey-scale ultrasound imaging was performed
trans-abdominally with a LogiqE8 or LogiqE9 (GE Healthcare,
Chicago, IL, USA), an HDI 3500 (ATL; Philips Healthcare, Andover,
MA, USA) or an Envision HD system (Philips Healthcare), with
multi-frequency (3–6 MHz) convex transducers. Pelvic organs were
routinely scanned when the bladders of patients were moderately
filled to provide an optimal imaging window. Following ultrasound,
the appearance of the uterus, cervix, vagina and ovaries were
assessed and documented. Any abnormal findings were also recorded.
When a mass within the vagina was detected, the association between
the mass and adjacent organs was investigated; the size of the mass
was measured in three dimensions: d1, d2 and d3 [meaning length
(longitudinal section), width (cross section) and thickness
(anteroposterior section), respectively] using the scales on each
ultrasound machine. The volume of the mass was calculated using the
following formula: V=0.52 × d1 × d2 × d3. Ultrasound results were
compared with intraoperative and pathological results. Furthermore,
bilateral renal areas were scanned to identify each kidney due to
CVOS often accompanying kidney absence according to theories of
embryonic development. As computed tomography urography (CTU) and
Intravenous pyelogram (IVP) are more sensitive and comprehensive
methods for kidney examination than ultrasonography, CTU and IVP
were performed in 10 and 5 patients, respectively when ultrasonic
examination was unable to confirm kidney absence However, CTU was
not routinely utilized at the beginning of this study, so most
patients were only examined using IVP. In recent years, IVP has
been substituted for CTU in the majority of hospitals and the
patients who exhibited suspected renal dysplasia mostly underwent
CTU. In the current study, CTU was performed using a 64-detector
row CT scanner (Lightspeed VCT; GE Healthcare) by intravenously
injecting 80 ml iopromide (Ultravist. 300; 740 mg/ml) at a rate of
4 ml/sec, following 20 ml normal sodium reinjection to make optimal
use of diagnostic opacity. The data acquisition was initiated 30
min. IVP was performed using a Hitachi TU-130 (Hitachi, Ltd.,
Tokyo, Japan) and a Shimadzu NAX-500RF (Shimadzu Corporation,
Kyoto, Japan) X-ray machine by intravenously injecting 40 ml
meglumine diatrizoate (Hunan Hansen Pharmaceutical Co., Ltd.,
Yiyang, China). The renal area was photographed 7, 15 and 30 min
following injection.
Results
Ultrasonic diagnosis consisting with
surgery
Following ultrasound examination, all 21 patients
underwent surgery to remove the oblique septum and drain any blood
retained within the hematocolpos via a transvaginal approach. Based
on the characteristics of ultrasound imaging, all 21 cases were
diagnosed with CVOS prior to this surgery. All 21 patients
exhibited a double uterus and cervix with ipsilateral renal
agenesis on the oblique septum side and compensatory enlargement of
the contralateral kidney. A total of 15 patients with ipsilateral
renal agenesis were confirmed using IVP (n=10) and CTU (n=5)
following ultrasound examination, the remaining 6 patients,
confirmed using ultrasound, did not receive the first two
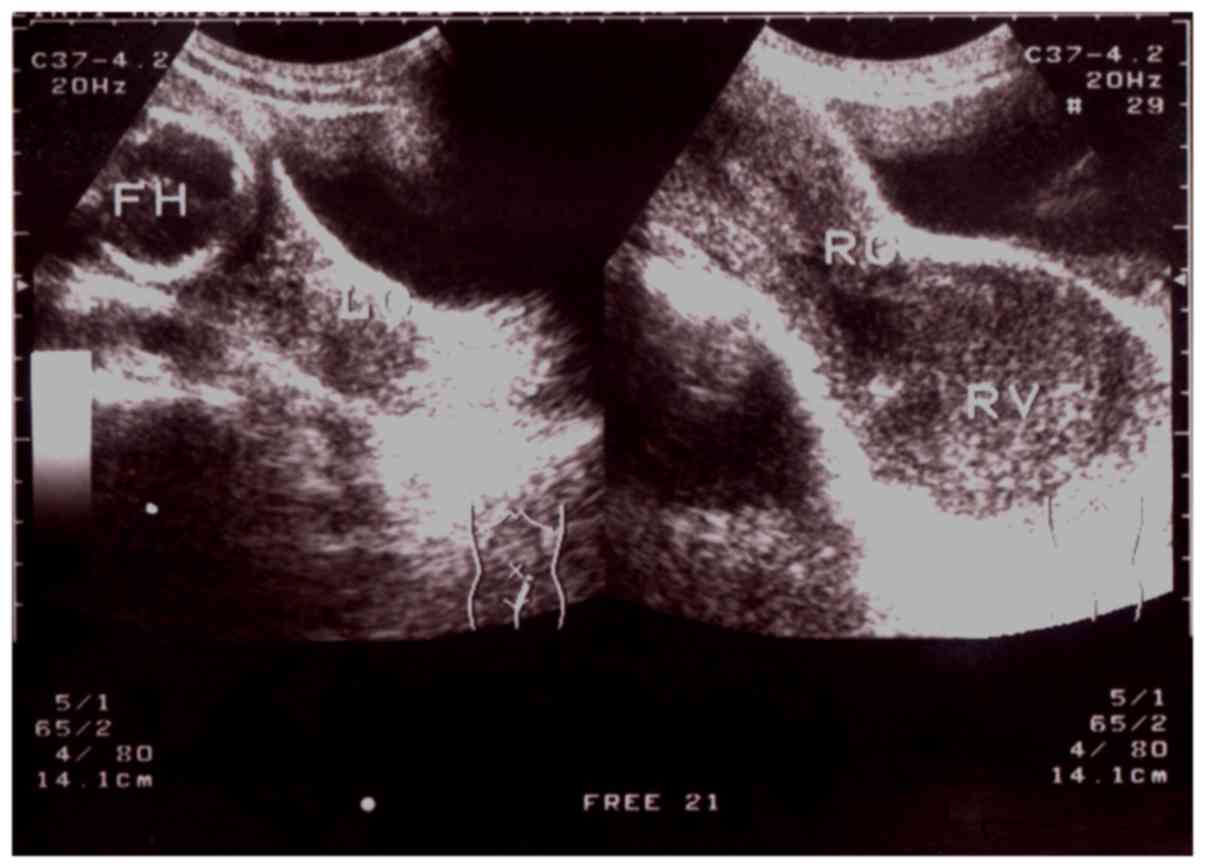
examinations as a clear image had already been obtained. Sonograms
indicated that the size and shape of bilateral ovaries of all
patients were within normal limits. Oval cystic masses of various
sizes with dense floating echogenic debris were identified on the
ultrasound images taken from all patients. There were 14
hematocolpos lesions on the right and 7 on the left of the vagina.
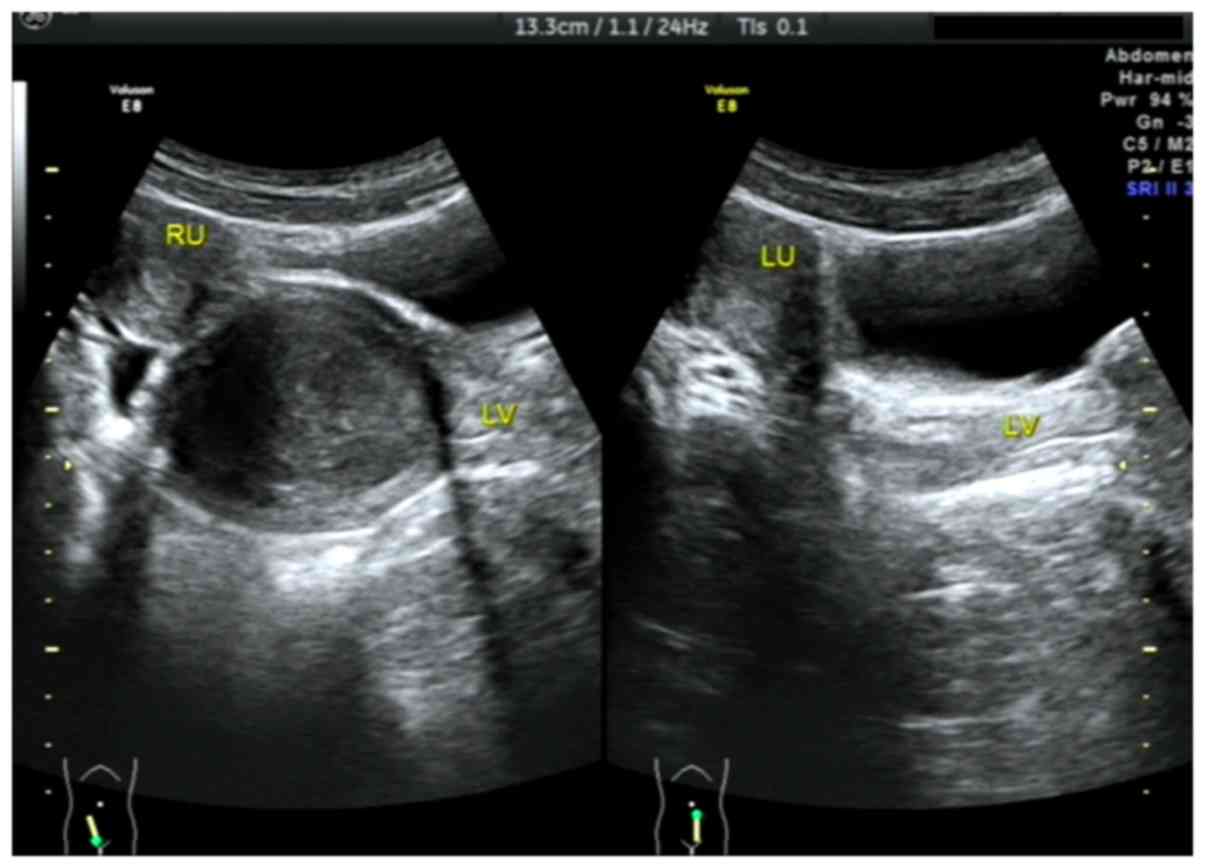
Type I CVOS was diagnosed in 15 patients with large hematocolpos
masses (volume, 64–268 ml), which was confirmed by surgery. There
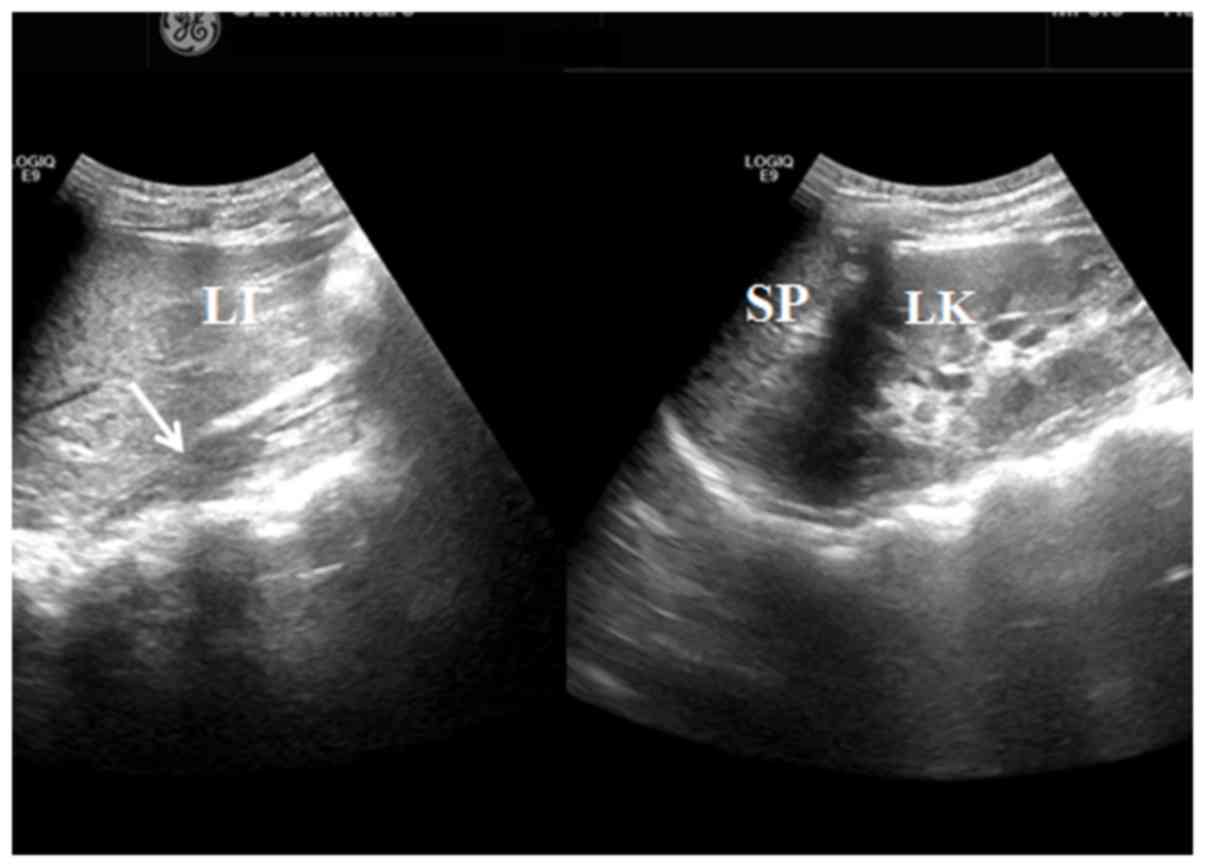
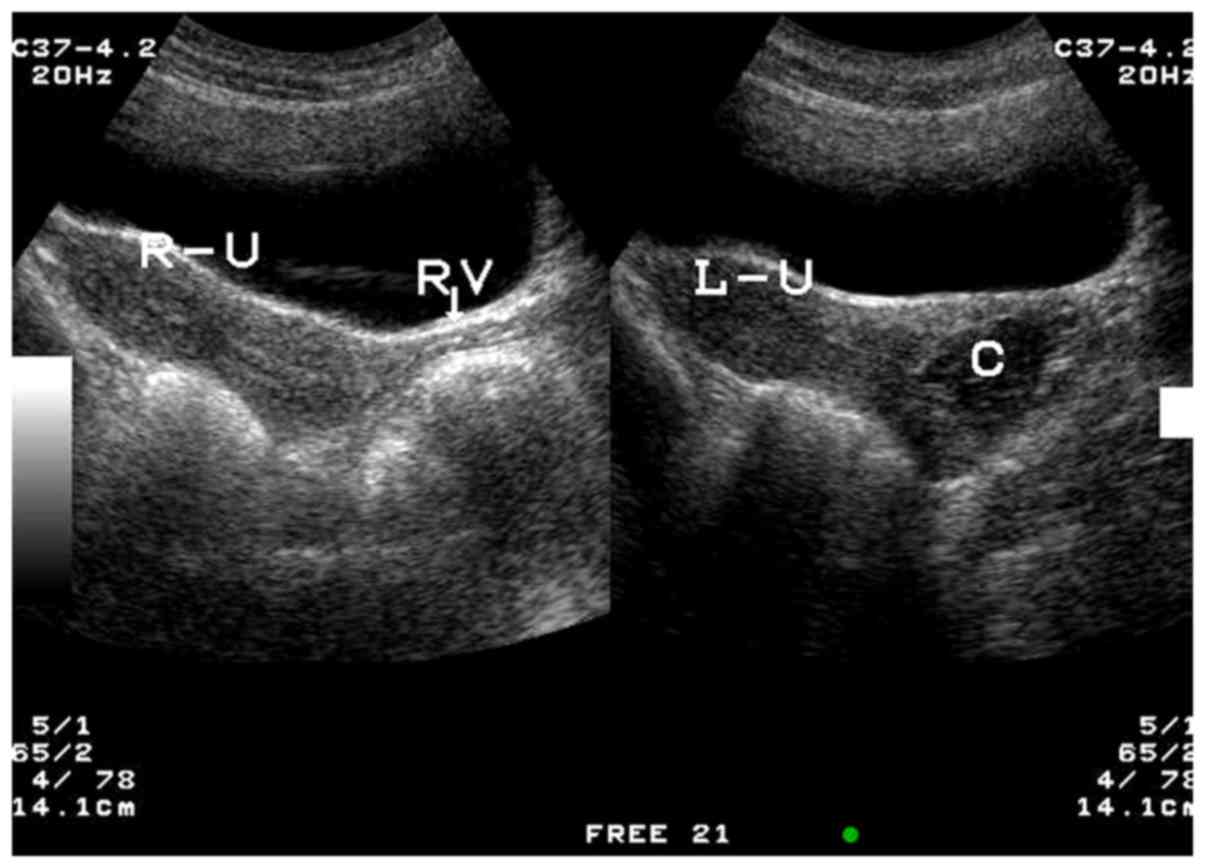
were 4 cases of type II and 2 cases of type III CVOS with small
hematocolpos lesions (volume, 5–36 ml), which were surgically
confirmed. These three types of CVOSs are demonstrated in Fig. 1.
Ultrasonic features of CVOS
Out of the 15 patients with type I CVOS, there were
9 patients with right oblique septum and 6 patients with left
oblique septum (Figs. 2–4). Among the 4 patients with type II CVOS,
3 patients had oblique septum on the right side and another on the
left of the vagina (Fig. 5). In the
2 patients with type III CVOS, the septum was on the right side of
the vagina (Fig. 6). Patients with
types II (n=4) and III (n=2) CVOS exhibited an anechoic vaginal
mass with an irregular shape and thickening wall, which was
consistent with pathological findings.
Discussion
In previous studies, patients with CVOS were divided
into 3 types, namely types I, II and III (4,6).
Patients with type I CVOS do not have a hole in the oblique septum
and the attachment of the uterus to the vagina is normal; however,
these patients have another uterus behind the septum that is
completely isolated from the contralateral uterus and do not
possess a normal vagina from which menstrual blood may flow.
Menstrual blood is retained behind the septum vaginal cavity and in
some cases the uterine cavity. Such patients experience a normal
menstrual cycle but experience periodic abdominal pain. Patients
with type II CVOS have a hole several mm thick in the reclined
septum through which menstrual blood drips out. Patients with type
III CVOS have no hole in the oblique septum; however, there is
cervical fistula between the two lateral cervixes or between the
cavity behind the septum and contralateral cervix. Menstrual blood
on the oblique septum side may drain out through the contralateral
cervix
CVOS diagnosis was previously conducted by
conducting X-ray hysterosalpinography and IVP (4). However, due to the popularization and
development of instruments to perform ultrasound, ultrasonography
has been developed as an accurate, fast, real-time and non-invasive
examination method that clearly identifies the uterus, cervix,
vaginal hemorrhage, ovarian characteristics and the presence or
absence of kidneys (8,9). Kidney absence, which is not easily
identified by ultrasound, may be detected by IVP (10).
According to theories of embryonic development, the
mullerian and Wolffian ducts originate in the urogenital ridge and
the development of mullerian duct depends on the Wolffian duct
(4). If there are developmental
disorders of the Wolffian duct, the mullerian duct on the same side
may also be affected and a series of genitourinary system
malformations may occur (4). In
patients with type I CVOS, the vaginal cavity behind the septum
exhibits hemorrhage and is expanded due to obstruction of the
vagina (6). There are specific
changes that can be detected by ultrasonograms: The big cystic mass
formed by hemorrhage in the vagina can be detected behind the
filling bladder, with a clear margin (6). Furthermore, there are point echoes in
the cystic mass due to old hemorrhages. The inside wall of the mass
is the oblique septum and the upper part is the ipsilateral side of
the uterine body connected with it and the contralateral uterine
body connected with the ipsilateral normal vagina, which probably
has normal endometrium (11). Along
with prolonging of the menstrual cycle, the expanding mass and
hemorrhage within the uterine cavity can be visualized dynamically.
However, due to the extrusion of the hemorrhage to the vagina, it
may be difficult to detect the contralateral normal vagina. In the
current study, only 5 patients exhibited the normal vagina located
in the front of the mass.
Based on the results of the current study and those
of previous studies (8,12–14), it
has been suggested that a diagnosis of type I CVOS may be made if
the following features are identified in the ultrasonogram: i)
There is a double uterus with or without uterine cavity hemorrhage
on one side, the endometrium of the uterus on the other side is
normal; ii) there is a cystic mass below the unilateral uterine
body; iii) the contralateral normal vaginal and normal uterus
connected with the vagina is identified from the images; iv) the
kidney is absent on the side of the mass; and v) the patient
undergoes a normal menstrual cycle. For patients with type II and
III CVOS, the ultrasonogram is the same as type I apart from a
smaller and lower tension of the mass, due to insufficient
menstrual blood drainage. However, secondary infection often occurs
due to obstruction of menstrual blood drainage.
Out of the patients included in the current study,
one patient aged 32 years old was diagnosed with type III CVOS
whilst pregnant. CVOS diagnosis during pregnancy is rare and the
patient's abdominal pain was reduced due to the absence of
menstruation following pregnancy. However, due to persistent
purulent secretion, part of the reclined septum was removed
transvaginally when the patient was 17 weeks pregnant. At 40 weeks
pregnancy, the fetus was in the breech position and the umbilical
cord was around the neck of the fetus; therefore, a cesarean
section was performed. During surgery, two cervical fistulas
located below the gorge and a double uterus with fallopian tubes
and ovaries on their side were identified.
Compared to type I CVOS, the other 5 patients with
type II and III CVOS demonstrated fewer small cystic masses with
thick walls and slightly triangular irregular shapes next to the
normal vagina Combined with the presence of a double uterus and
ipsilateral renal agenesis, a diagnosis of CVOS was tentatively
made. These diagnoses were confirmed by gynecological examination
and following surgery. Therefore, ultrasound imaging may be
important in aiding the diagnosis of types II and III CVOS. In the
majority of patients (14/21) included in the current study, oblique
septums were located on the right side, which is consistent with
the results of previous studies (1,15,16).
Accurate ultrasonic diagnoses may enable clinicians to perform
transvaginal resection of the reclined septum and avoid unnecessary
laparotomy to excise the uterus and fallopian tube (17).
In conclusion, the results of the current study
suggest that the key to diagnosing CVOS accurately lies in
correctly assessing the ultrasonic images of patients with CVOS and
determining the associated clinical manifestations. The results
indicate that diagnoses of CVOS may be made by performing
high-resolution ultrasound. Definite diagnoses of type I CVOS was
performed in 15 patients using ultrasonograms and helpful patient
information was provided from to aid in the timely diagnosis of the
6 patients with types II and III CVOS.
Acknowledgements
The authors of the present study would like to thank
the patients and their families for their support and
collaboration, and Dr Ji-Bin Liu (Thomas Jefferson University
Hospital, Philadelphia, PA, USA) for guidance on manuscript
preparation.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors participated in the acquisition of data
for this study. YHG and HLF were the major contributors in writing
the manuscript. All authors have read and approved this
manuscript.
Ethics approval and consent to
participate
The protocol of the study was approved by the ethics
committee of Shandong Provincial Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yoder IC and Pfister RC: Unilateral
hematocolpos and ipsilateral renal agenesis: Report of two cases
and review of the literature. Am J Roentgenol. 127:303–308. 1976.
View Article : Google Scholar
|
|
2
|
Mehra S, Chamaria K, Garga UC, Kataria A
and Ahuja A: Imaging diagnosis of herlyn-werner-wunderlich
syndrome-an extremely rare urogenital anomaly. J Clin Diagn Res.
9:Td06–Td08. 2015.PubMed/NCBI
|
|
3
|
Orazi C, Lucchetti MC, Schingo PM,
Marchetti P and Ferro F: Herlyn-Werner-Wunderlich syndrome: Uterus
didelphys, blind hemivagina and ipsilateral renal agenesis.
Sonographic and MR findings in 11 cases. Pediatr Radiol.
37:657–665. 2007.(In Chinese). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bian ML: Oblique vaginal septum: Report of
15 cases. Zhonghua Fu Chan Ke Za Zhi. 20(85–88): 1261985.(In
Chinese).
|
|
5
|
Jindal G, Kachhawa S, Meena GL and Dhakar
G: Uterus didelphys with unilateral obstructed hemivagina with
hematometrocolpos and hematosalpinx with ipsilateral renal
agenesis. J Hum Reprod Sci. 2:87–89. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang J, Zhu L, Lang J, Liu Z, Sun D, Leng
J and Fan Q: Clinical characteristics and treatment of
Herlyn-Werner-Wunderlich syndrome. Arch Gynecol Obstet.
290:947–950. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tong J, Zhu L and Lang J: Clinical
characteristics of 70 patients with Herlyn-Werner-Wunderlich
syndrome. Int J Gynaecol Obstet. 121:173–175. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gai YH, Cai SF, Wu SH, Song SL, Ding JL,
Xue Y and Zhao JZ: Ultrasonic diagnosis of congenital vaginal
reclined septum syndrome. Chin J Ultrasonogr. 13:834–836, (In
Chinese).
|
|
9
|
Yavuz A, Bora A, Kurdoglu M, Goya C,
Kurdoglu Z, Beyazal M and Akdemir Z: Herlyn-Werner-Wunderlich
syndrome: Merits of sonographic and magnetic resonance imaging for
accurate diagnosis and patient management in 13 cases. J Pediatr
Adolesc Gynecol. 28:47–52. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Costello CH and Cook CK: Intravenous
urography and imaging of the urinary tract. Hosp Med. 65:426–430.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dias JL and Jogo R:
Herlyn-Werner-Wunderlich syndrome: Pre- and post-surgical MRI and
US findings. Abdom Imaging. 40:2667–2682. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gholoum S, Puligandla PS, Hui T, Su W,
Quiros E and Laberge JM: Management and outcome of patients with
combined vaginal septum, bifid uterus, and ipsilateral renal
agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg.
41:987–992. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Moawad NS, Mahajan ST, Moawad SA and
Greenfield M: Uterus didelphys and longitudinal vaginal septum
coincident with an obstructive transverse vaginal septum. J Pediatr
Adolesc Gynecol. 22:e163–165. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
van der Byl G, di Giacomo V and Miele V:
Herlyn Werner Wunderlich syndrome (HWWS): An unusual presentation
of acuteabdominal pain: Herlyn Werner Wunderlich syndrome (HWWS):
An unusual presentation of acute abdominal pain. J Ultrasound.
17:171–174. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Acién P and Acién M: Unilateral renal
agenesis and female genital tract pathologies. Acta Obstet Gynecol
Scand. 89:1424–1431. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rock JA and Jones HW Jr: The double uterus
associated with an obstructed hemivagina and ipsilateral renal
agenesis. Am J Obstet Gynecol. 138:339–342. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eisenberg E, Farber M, Mitchell GW Jr,
Turksoy RN and Rule AH: Complete duplication of the uterus and
cervix with a unilaterally imperforate vagina. Obstet Gynecol.
60:259–262. 1982.PubMed/NCBI
|