Introduction
Hirschsprung's disease (HD) is characterized by the
absence of ganglion cells in the distal bowel. In recent years,
various operative modes have been developed for the surgical
treatment of HD (1–3). The incidence of HD is ~1/5,000 live
births and men are 3.5–7.8 times more likely to be affected than
women. HD usually occurs in infancy, although some people will
present with persistent, severe constipation in the later life
(4). This condition is confined to
the rectosigmoid colon in 75% of affected patients. The
rectosigmoid colon variant is the most frequent presentation, but
an extended form has also been observed. In 17% of all cases, the
aganglionic segment is observed to extend from the rectum, sigmoid
colon and colon up to part of the transverse colon. The rarest form
of the disease with the most severe clinical course is total
colonic aganglionosis (TCA), which is observed in 8% of patients
(5).
Surgical intervention for HD involves the removal of
the aganglionic bowel to provide normally innervated intestine to
the anus (6). Classical pull-through
techniques as described by Soave et al have been modified
and improved in order to reduce the surgical incision range,
minimize damage to the surrounding structures during
intra-abdominal dissection and eliminate associated complications
(5,7). The transanal endorectal pull-through
(TEPT) technique was subsequently proposed by De la Torre-Mondragon
and Ortega-Salgado, which revolutionized HD treatment (8). In 1995, the one stage
laparoscopy-assisted pull-through (LPT) approach was proposed by
Georgeson et al (9) and has
since been extensively applied for the treatment of HD. This method
has several merits, including no need for colostomy, and a lack of
intraperitoneal adherence and/or scarring (10). While LPT can be performed for
patients with different types of HD, it is more conventionally
applied to treat aganglionosis, which extends to the ascending
colon (11). At present, there are
several surgical techniques available for the treatment of HD;
however, their outcomes remain unsatisfactory (12,13).
Between September 2003 and August 2014, all patients
with HD at the Pediatric Surgery Department of The Affiliated
Hospital of Zunyi Medical College (Zunyi, China) were treated using
the stepwise and gradient muscular cuff cutting method. TEPT or LPT
surgical techniques were selected based on the preference of the
patients' families, as well as the experience of the surgeon. In
the present study, a novel type of pull-through operative method is
presented. A novel technique for refinement is also proposed and
the short- and long-term impacts of the two methods are compared
with the aim of developing a novel and effective treatment
technique for pediatric surgeons.
Materials and methods
Patients
The study protocol was formally approved by the
Ethics Committee of The Affiliated Hospital of Zunyi Medical
College. All patients' families gave their informed consent. The
medical records of 221 children admitted to the institution between
September 2003 and August 2014 with a diagnosis of HD were
retrospectively reviewed. All diagnoses were identified based on
the histological examination of rectal biopsy samples. A number of
patients were excluded, including those who had received
conventional transabdominal pull-through procedures (n=24),
patients who were diagnosed with TCA (n=7) and those who followed
up abroad halfway (n=18). Consequently, 172 patients (mean age,
13.5 months; male:female, 138:34) were examined, all of whom were
eventually treated with the stepwise and gradient muscular cuff
cutting method for HD. Ultimately, 78 and 94 children were treated
using the LPT and TEPT techniques, respectively. The data collected
includes the baseline index, clinical presentation, type of surgery
performed, systems review (i.e., mortality and quality of life),
operative details, time to oral feeding, duration of
hospitalization, length of intensive care unit (ICU) stay, early
and late postoperative complications, episodes of postoperative
enterocolitis and stooling habits (i.e., continence, frequency,
requirement of laxatives or other medications). The enterocolitis
severity was graded using a previously designed scoring system from
mild (i.e., grade I) to severe (i.e., grade III) (14). Follow-up information was obtained
from outpatient visit notes, as well as telephone questionnaire
feedback. Patient/family surveys were conducted for patients older
than 3 years and scored using an improved uniform 12-item long-term
prognosis survey following the pull-through procedure (15) (Table
I).
 | Table I.Telephone questionnaire scores for
patients older than 3 years. |
Table I.
Telephone questionnaire scores for
patients older than 3 years.
| Question | Answer | Score |
|---|
| Frequency of
defecation | Only with enema | 4 |
|
| Only with
suppository | 3 |
|
| Every 3 day or more
but spontaneous | 2 |
|
| Every 1–2 day | 1 |
|
| Normal (1–2/day) | 0 |
|
| Often (3–5/day) | 1 |
|
| 6-7/d | 2 |
|
| 8 or more
movements/day | 3 |
| Soling | Permanent (more than
6 times/day) | 3 |
|
| Often (4–6
times/day) | 2 |
|
| Occasional (1–3
times/day) | 1 |
|
| None | 0 |
| Times of soling | At night and day | 2 |
|
| At night or
activity | 1 |
|
| None | 0 |
| Is he/she fully
continent? | Not continent | 2 |
|
| Partially
(occasional accidents) | 1 |
|
| Yes | 0 |
| Stool
consistency | Liquid | 3 |
|
| Hard | 2 |
|
| Loose | 1 |
|
| Normal | 0 |
| Stool odor | Offensive odor | 1 |
|
| Normal odor | 0 |
| Loss of stool
during coughing or crying | Solid | 3 |
|
| Liquid | 2 |
|
| Gas | 1 |
|
| No | 0 |
| Requires
diapers | Continuously | 2 |
|
| Night or
activity | 1 |
|
| None | 0 |
| Sense of fullness
and evacuation after defecation | Absent sense of
fullness | 2 |
|
| Fullness but
partial evacuation | 1 |
|
| Fullness and
evacuation | 0 |
| Distension | Moderate to
severe | 2 |
|
| Mild | 1 |
|
| No | 0 |
| Need for medical
therapy to control stooling | Always | 3 |
|
| Occasionally | 2 |
|
| Long period but
finally weaned off | 1 |
|
| No | 0 |
| Recurrent attacks
of enterocolitis | More than 6
attacks | 3 |
|
| 4-6 attacks | 2 |
|
| 1-3 attacks | 1 |
|
| None | 0 |
Surgical techniques (TEPT group)
A full TEPT method was used. Patients were examined
with serial rectal lavage and anal dilation was performed via
digital dilatations prior to surgery. The final rectal washouts
contained metronidazole (25 mg/kg body weight; Shijiazhuang No. 4
Pharmaceutical Co., Ltd., Hebei, China). Third-generation
cephalosporin antibiotics (Cefotaxime Sodium for Injection; 50
mg/kg body weight; NCPC Hebei Huamin Pharmaceutical Co., Ltd.,
Hebei, China) were administered 30 min prior to surgery. Patients
were placed in a supine position with dangling legs throughout the
operation. Anal retractors were used around the anal verge to
expose the anus. A 4-0 polypropylene monofilament prolene suture
was placed through the tip of the glans as a traction suture within
0.5–1.0 cm above the dentate line. Fascicular electrocautery was
performed for the delicate dissection of rectal muscle and
hemostasis of the main vessels in an effort to avoid damage to the
pelvic nerves. In the present study, a novel technique was refined;
this involved cutting the rectal circular muscle within 1–2 cm of
the starting point of the submucosal dissection. First, the rectal
longitudinal smooth muscle was cut and the rectum ring muscle was
separated after an incision of 1–2 cm. The anal sphincter was also
protected. This differs from traditional Soave operations in which
the whole muscle cuff remains and the anal sphincter is usually
damaged (16). The surgery was
modified by the authors of the current study since the longitudinal
rectal muscle was cut 2–3 cm above the circular muscle. Using a
surgical incision of the stepwise gradient muscular cuff up towards
the peritoneal cavity, the muscular cuff remained 1–2 cm in
neonates and infants, or 3–4 cm in children. The aganglionic bowel
was pulled through the muscular cuff and the bowel was separated to
the normal zone. Once the biopsy site demonstrating normal
innervation was reached, anastomosis was performed outside the anal
cavity. The muscular cuff was then sutured with the normal bowel to
prevent mucosa prolapsing. The colonal anastomosis with the mucosa
of the dentate line exhibited a heart-shaped anastomosis, higher in
the front and lower in the back. At 2 weeks post-surgery, gentle
rectal dilatations were performed using a dilator.
LPT group
The LPT procedure was performed for patients with HD
confined to the left colon based on a preoperative barium enema
examination. All patients who received the LPT procedure were in a
similar condition prior to surgery as the patients in the TEPT
group. Three trocars were used and a transumbilical camera port
(e.g., 5 mm) and two operative ports (3 mm or 5 mm) were inserted
bilaterally two-thirds into the line from the umbilicus to the
anterior superior iliac spine. In the first step, multiple
seromuscular leveling biopsies of the bowel were obtained in order
to pathologically detect ganglion cells in the submucosal nerve
plexus. The length of abscission was also determined based on
biopsies that confirmed the absence of ganglion cells in sections
of the colon; typical histological findings for HD in a rectal
biopsy include the absence of ganglion cells in the submucosal
(Meissner's) plexus and the intermuscular (Auerbach's) plexus
(17,18). The mesentery was separated from the
rectal wall to protect the lower rectal vessels and maintain a good
blood supply to the rectal muscular sheath. Dissection was followed
to the peritoneal reflection of the rectum. Endorectal dissection
was the same as performed in the TEPT group. In the present study,
mucosectomy was frequently performed prior to the development of
the stepwise and gradient cutting muscular cuff dissected rectum
method.
Post-surgical care
Following, surgery, all patients received
intravenous broad-spectrum antibiotics and an injection of
metronidazole (25 mg/kg) to prevent enterocolitis. In the majority
of patients, an anal supporting tube was inserted and maintained
for 5–7 days to prevent anastomotic stricture and enterocolitis. At
2 weeks post-surgery, patients received a routine anal expanding
program with a Hegar dilator for 2 months.
Statistical analysis
All data are expressed as the mean ± standard
deviation and statistical analysis was performed using SPSS
software version 19.0 (IBM SPSS Software, Armonk, NY, USA). The
Student's t-test was used to compare different parameters (i.e.,
age, weight, operative time, intraoperative blood loss, anal
dissection time, oral feeding time and duration of hospitalization)
between the LPT and TEPT groups. Sex, aganglionic segment, early
post-operative complications, late post-operative complications and
bowel movements were also compared using the chi-squared test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Patient characteristics
In the present study, 172 patients over a 10-year
period underwent surgery using a stepwise and gradient cutting
muscular cuff method with a pull-through procedure. Their general
clinical data are presented in Table
II. No significant differences were observed in sex, age or
weight. Aganglionic segments were discovered extending to the
rectosigmoid, descending colon, transverse colon and ascending
colon in the two groups.
 | Table II.Clinical and demographic
characteristics. |
Table II.
Clinical and demographic
characteristics.
| Parameter | TEPT (n=94) | LPT (n=78) | P-value |
|---|
| Age at surgery
(months) | 15.4±15.7 | 11.5±12.7 | 0.081 |
| Sex
(male:female) | 78:16 | 60:18 | 0.321 |
| Weight at surgery
(kg) | 8.7±4.0 | 7.6±3.6 | 0.074 |
| Aganglionic
segment |
|
|
|
|
Ultrashort | 21 | 10 | 0.106 |
|
Rectosigmoid | 45 | 35 | 0.694 |
|
Descending colon | 24 | 17 | 0.567 |
|
Transverse colon | 4 | 12 | 0.017 |
|
Ascending colon | 0 | 4 | 0.026 |
Operative data
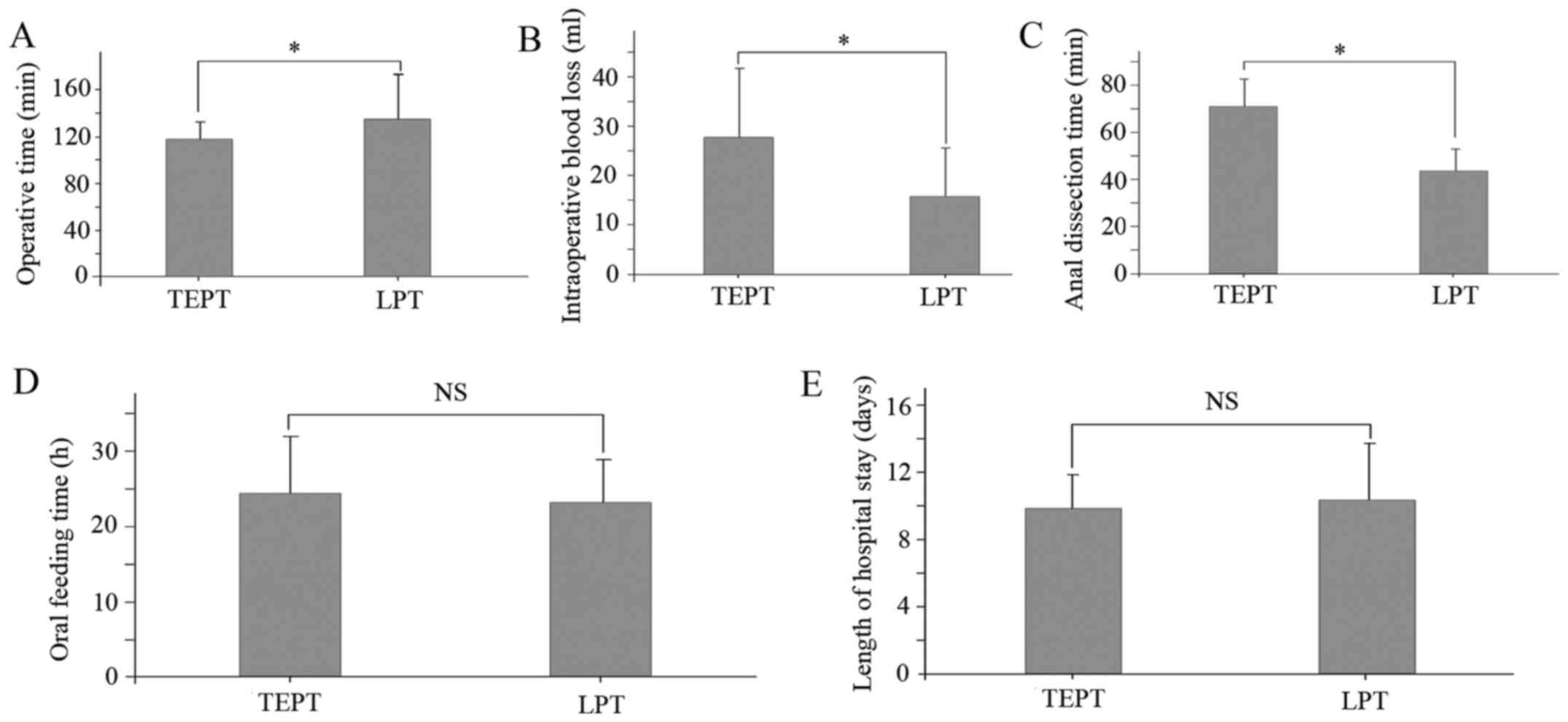
The operative data and post-operative outcomes are
presented in Fig. 1. Patients in the
TEPT group had significantly shorter operative times (117.6±16.0
min) compared with the LPT group (135.5±35.0 min; P<0.05;
Fig. 1A). However, in the LPT group
intraoperative blood loss (15.8±10.0 ml vs. 27.9±14.1 ml;
P<0.05; Fig. 1B) and anal
dissection times (44.4±7.5 min vs. 71.4±9.6 min; P<0.05;
Fig. 1C) were significantly
decreased compared with the TEPT group. No significant differences
were observed in oral feeding time or duration of hospitalization
(Fig. 1D and E).
Post-operative complications
The early post-operative complications are listed in
Table III. A total of 27 patients
(25.6%) in the TEPT group and 20 patients (28.7%) in the LPT group
presented with perianal dermatitis in the early post-operative
period. There was no significant difference in the incidence of
perianal dermatitis between the two groups. There were 4 patients
(4.3%) in the TEPT group and 2 patients (2.6%) in the LPT group who
exhibited post-operative uroschesis; however, no significant
difference was observed. No patients were diagnosed with
anastomotic leakage or anastomotic structures. Additionally, 2
patients in the LPT group had recurrent intestinal obstruction
caused by adhesion and 1 patient exhibited intestinal volvulus of
the pull-through rectal area in the early post-operative period,
which was treated using adhesiolysis and colonic anastomosis
through laparotomy; none of these events were recorded in the TEPT
group (P=0.055).
 | Table III.Early postoperative
complications. |
Table III.
Early postoperative
complications.
| Complication | TEPT (n=94) | LPT (n=78) | P-value |
|---|
| Perianal
dermatitis, n (%) | 27 (25.6) | 20 (28.7) | 0.652 |
| Uroschesis, n
(%) | 4
(4.3) | 2
(2.6) | 0.547 |
| Anastomotic
leakage, n (%) | 0
(0) | 0
(0) | <0.001 |
| Anastomotic
strictures, n (%) | 0
(0) | 0
(0) | <0.001 |
| Early intestinal
obstruction, n (%) | 0
(0) | 3
(3.8) | 0.055 |
| Enterocolitis rate,
n (%) | 19 (20.2) | 25 (32.1) | 0.076 |
| Enterocolitis
grade, n (%) |
|
|
|
| I | 12 (12.8) | 14 (17.9) | 0.345 |
| II | 6
(6.4) | 9
(11.5) | 0.283 |
|
III | 1
(1.1) | 4
(5.1) | 0.178 |
Enterocolitis occurred in both groups, with 19
(20.2%) and 25 (32.1%) cases in the TEPT and LPT groups,
respectively (P=0.076). The severity of these episodes did not
significantly differ between the two groups. Symptoms were improved
following metronidazole administration via a coloclyster,
gastrointestinal decompression, antibiotic treatment, parenteral
nutritional support and regulation of intestinal microflora.
Follow-up
Patients were followed up post-operatively for
36–120 months. Long-term post-operative complications are listed in
Table IV. A total of 8 patients in
the TEPT group (8.5%) and 7 patients in the LPT group (9.0%) had
recurrent anastomotic strictures in the late post-operative period
(P=0.915). Furthermore, 2 patients in the TEPT group and 12
patients in the LPT group experienced soiling in the long-term
post-operative period. The incidence of soiling in the TEPT group
(2.1%) was significantly lower compared with the LPT group (15.6%;
P<0.05). This problem was improved within 6–12 months of
functional training and bowel management.
 | Table IV.Late postoperative complications. |
Table IV.
Late postoperative complications.
|
| TEPT (n=94) | LPT (n=78) | P-value |
|---|
| Anastomotic
strictures, n (%) | 8
(8.5) | 7
(9.0) | 0.915 |
| Incidence of
soiling, n (%) | 2
(2.1) | 12 (15.6) | 0.001 |
| Constipation, n
(%) | 16 (17.0) | 5
(6.4) | 0.034 |
| Incontinence in
children >5 years, n (%) | 0
(0) | 0
(0) | <0.001 |
| Enterocolitis rate,
n (%) | 9
(9.6) | 14 (17.9) | 0.108 |
| Enterocolitis
grade, n (%) |
|
|
|
| I | 8
(8.5) | 9
(11.5) | 0.610 |
| II | 1
(1.1) | 4
(5.1) | 0.178 |
|
III | 0
(0) | 1
(1.3) | 0.453 |
Reports of recurrent long-term constipation in were
significantly lower in the LPT group (6.4%) compared with the TEPT
group (17.0%; P<0.05). No incontinence was reported for either
group. In addition, 9 patients (9.6%) in the TEPT group and 14
(17.9%) in the LPT group experienced recurrent enterocolitis in the
late post-operative period (P=0.108). There were 8 cases of grade I
enterocolitis (8.5%) in the TEPT group and 9 cases (11.5%) in the
LPT group (P=0.610); 1 case (1.1%) of grade II enterocolitis in the
TEPT group and 4 cases (5.1%) in the LPT group (P=0.178); and 1
case (1.3%) of grade III enterocolitis in the LPT group and 0 cases
in the TEPT group (P=0.453).
The patients' parents participated in telephone
interviews regarding stooling patterns following surgery. A
complete long-term outcome questionnaire was obtained for 116
patients with HD, including 64/94 patients in the TEPT group and
52/78 patients in the LPT group. A total of 114 patients (98.3%)
provided scores in the good-to-excellent range. A total of 90
patients (77.6%) had an excellent score, among which 52 patients
(81.3%) were in the TEPT group and 38 patients (73.1%) were in the
LPT group; 24 patients (20.7%) achieved a good score, with 12
patients (18.8%) in the TEPT group and 12 patients (23.1%) in the
LPT group; 2 patients (1.7%) had a fair score, which only occurred
in the LPT group (3.8%). There was no significant difference
between groups in the questionnaire outcome (Table V). Furthermore, no significant
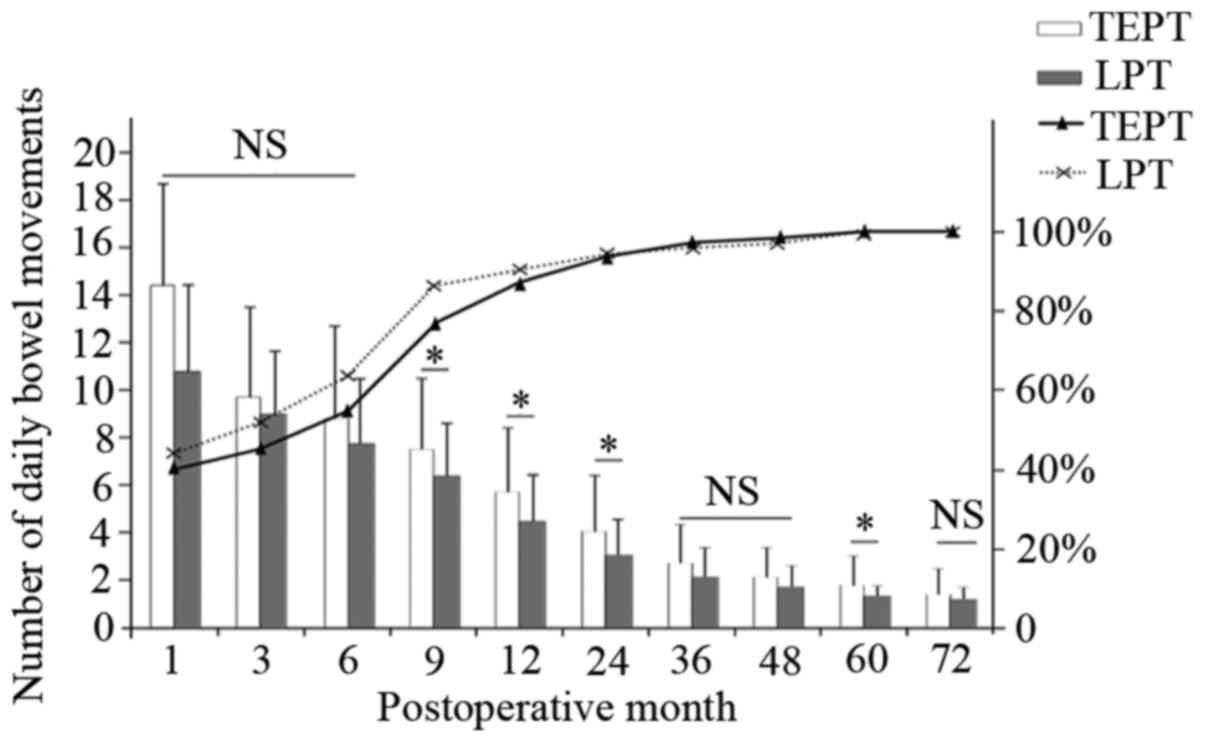
differences were observed in post-operative daily bowel movements
for 6 months (P>0.05). However, for the 9 months to 2 years
period, significantly more daily bowel movements were reported in
the TEPT group compared with the LPT group (P<0.05). For both
procedures, the number of daily bowel movements decreased each
year; by 6 years, there was no significant difference between the
two groups (Fig. 2).
 | Table V.Total stooling scores of various
groups. |
Table V.
Total stooling scores of various
groups.
|
| n (%) | TEPT, n (%) | LPT, n (%) |
|---|
| Excellent
(0–10) | 90 (77.6) | 52 (81.3) | 38 (73.1) |
| Good (11–20) | 24 (20.7) | 12 (18.8) | 12 (23.1) |
| Fair (21–30) | 2
(1.7) | 0 (0) | 2 (3.8) |
Discussion
In recent decades, there have been a number of
improvements to surgical methods (13,19,20).
This study presents important refinements for stepwise and gradient
cutting muscular cuff methods. From September 2003 to August 2014,
172 patients were admitted to the Department of Pediatric Surgery
at The Affiliated Hospital of Zunyi Medical College and treated
using one of two procedures. Prior to the start of the study, the
surgeons involved had gained equal experience in LPT and TEPT, had
mastered the various specifications and protocols of these two
procedures and had gained the same level of expertise in performing
both techniques. Short- and long-term survival outcomes of patients
with HD treated with TEPT and LPT were evaluated in this study. To
standardize the post-operative long-term evaluation of HD patients,
a questionnaire was designed containing 12 questions to assess
long-term complications and families of patients who were ≥3 years
old were asked to judge bowel habits and continence ability.
TEPT and LPT procedures are becoming increasingly
essential techniques for pediatric surgery, the most important
advantage of which is the low risk of post-operative scarring
(21). However, it remains uncertain
which method is the best choice; selections are typically made
based on the surgeon's skill and experience. At the Affiliated
Hospital of Zunyi Medical College, TEPT was the preferred procedure
between 2003 and 2009, whereas LPT is now the favored procedure.
The Soave technique has potential issues with the muscular cuff
remaining and damage to the anal sphincter, which may lead to
constipation, soiling and incontinence (16). As such, the Soave procedure was
modified in the present study to the stepwise and gradient cutting
muscular cuff method, allowing the retention of 1–2 cm rectal
muscular cuff in neonates and infants, or 3–4 cm in children with
HD. The results revealed that the short-term outcomes were
successful and the safety and effectiveness of the transanal
procedure has been well documented. In addition, transanal
endorectal coloanal anastomosis appears to be simpler and easier to
perform with minimal dissection, resulting in less damage to the
anal sphincter and pelvic nerves, which is vital for normal
defecation (13). Furthermore,
opportunities for surgery remain if the transitional zone is at or
proximal to the splenic flexure, even in patients with total
colonic aganglionosis (6). Starting
with laparoscopy is helpful for dividing the right or middle colic
vessels, leaving a generous arcade of marginal vessels along the
colon and completely dissected colonic ligaments, avoiding
over-tension of the pull-though and ischemic colitis (22). The modified Soave method may be
applicable for all patients with HD where LPT would have been used
before, whereas TEPT can only be adapted to patients for whom the
extent of aganglionosis is within the lower rectum or sigmoid
colon. The results of the present study suggest that LPT is
superior to TEPT in terms of intraoperative blood loss and anal
dissection time and that TEPT has a shorter operative time.
In this study, the type and rate of complications
were similar in both experimental groups. Although a cited benefit
of laparoscopic surgery is the reduction of intestinal obstruction
and constipation, three cases of intestinal obstruction were
reported; one was colonic volvulus of the pull-through and two were
paralytic intestinal obstruction. These occurred in cases of
aganglionosis that had extended further than the descending colon
and required further ascending colon reversal; the patient with
colonic volvulus required further surgery. As previously reported
in a 29-year tracked review of long-term results following
treatments for HD (23), up to 40%
of patients reported persistent constipation. However, in the
present study the rate of constipation in the LPT group was
significantly lower compared with the TEPT group (5 vs. 16). The
incidence rate recorded in this study was concordant with previous
reports, ranging from 6–27% (24–26). The
most common reason for recurrence was a segment of the aganglionic
bowel remaining post-surgery (27).
LPT is the preferred technique at the Affiliated Hospital of Zunyi
Medical College as, apart from the excellent cosmetic results, it
allows for biopsies to be obtained immediately and provides
adequate post-operative long-term mobilization of the bowel.
Therefore, we dissected the pathological colon with stricture and
full expansion of the colon, to allow the mobilization of the colon
as much as possible. In the TEPT group, 4 patients underwent
further surgery as their post-operative biopsy specimens revealed
that the reason for constipation was residual aganglionosis of the
bowel. All other patients were conservatively treated using
comprehensive measures, including diet control, laxatives or anal
dilation for >1 year.
The incidence of perianal dermatitis and soiling in
our cohort was within the range described in other publications
(28). Rescorla et al
(29) suggested that 88% of patients
experienced some difficulties within <5 years after a
pull-through operation, including temporary soiling and perianal
dermatitis. However, the soiling and perianal dermatitis improved
in nearly 99% of patients with a follow-up >3 years, which
indicates that a better prognosis is possible over time.
One major complication of the traditional transanal
Soave technique is the risk of post-operative anastomotic
obstruction (30). A procedure
modification involving a short muscular cuff anastomosis and dorsal
splitting of the muscular wall is advised (31). Simultaneously, performing the
heart-shaped anastomosis of the ganglionated proximal end 0.5–1.0
cm above the dentate line can effectively avoid post-operative
anastomotic stricture. In the present study, a stepwise and
gradient cutting muscular cuff technique was performed, which left
a short cuff remaining. All patients were treated with routine anal
dilation for >6 months and none required further surgery because
of the anastomotic obstruction. If anastomotic obstruction was
serious and did not alleviate with routine anal dilation, the
patients required additional surgery.
The recently reported incidence rates for
enterocolitis range from 4.6–54% in multiple studies (30,32). Kim
et al (30) reported a
multicenter study with long-term results, in which the rate of
enterocolitis was 22% with a complete transanal pull-through
procedure. In the present study, the rate of enterocolitis was
comparable to a previously reported systematic review and
meta-analysis that compared a total transanal endorectal
pull-through (22.5%) with a pull-through with any form of
laparoscopic assistance (28.1%) in infants with HD (10).
Although the incidence of enterocolitis in the
present study did not significantly differ between the groups, a
slightly higher incidence was observed in the LPT group, which may
be partially attributed to the long segments of aganglionosis. The
immaturity of the gastrointestinal immune system in aganglionic
segments is certainly an important factor in the occurrence and
development of enterocolitis (33).
Although the association between these covariates and enterocolitis
is unknown, it could be postulated that, in patients with
anastomotic stricture, obstruction may lead to the development of
bacterial overgrowth and enterocolitis. The variable rates of
enterocolitis reported may be associated with inconsistent
definitions between studies. Conservative treatments for
enterocolitis were successful in the majority of patients, whereas
further surgical treatment was required in the remaining 3
patients. The present study reveals that the modified technique is
a safe and less-invasive procedure than the traditional Soave
method, with a low incidence of post-operative enterocolitis
compared with previous surgical techniques.
The present study demonstrates that the stepwise and
gradient cutting muscular cuff method results in a good functional
outcome for extended HD. A transient increase in the frequency of
bowel motions during the early post-operative weeks was reported.
Bowel movements resulted in average of 7–10 stools/day at 6 months
post-surgery, whereas just 5–6 stools were reported in other
studies (25). This is probably
caused by damage to the anal sphincter during mucosectomy when
pulling through the hypertrophic colon. Similar to previous
studies, stooling pattern scores and the frequency of bowel
movements herein tended to improve with time and may eventually
return to a normal range (20). In
the present study, it was observed that the number of bowel
movements reported in the LPT group was significantly higher
compared with the TEPT group from 9 months to 2 years post-surgery.
It could be speculated that laparoscopy allows dissection below the
peritoneal reflection, which may decrease anal dissection time and
avoid injury to the anal sphincter.
In conclusion, the stepwise and gradient cutting
muscular cuff method should be considered as an acceptable and safe
procedure for the treatment of HD. It was demonstrated that the LPT
procedure is feasible for short-segment, classic and extended HD;
however, the TEPT procedure is more feasible for short-segment HD.
These results demonstrate that LPT is a better surgical approach
for children with HD and may be a superior choice to TEPT in the
future.
Acknowledgements
The authors are grateful to all study
participants.
Funding
The present study was funded by the National Natural
Science Fund of China (grant no. 81650029).
Availability of data and materials
The technical appendix and statistical datasets are
available from the corresponding author. No additional data are
available.
Authors' contributions
ZZ, FZ and ZJ performed the majority of experiments.
MG, YM and YQ analyzed the data. YL conceived and designed the
experiments and contributed reagents, methods and analysis tools.
All authors authored and reviewed drafts of the paper, and approved
the final draft.
Ethics approval and consent to
participate
The Ethics Committee of Zunyi Medical University has
reviewed and approved this study. Prior to signing the consent form
by the parents, they were fully informed about the surgical
procedure, associated risks and possibility for conversion to the
open surgical technique.
Patient consent for publication
All the participants gave informed consent for data
sharing when they enrolled in this study.
Competing interests
The authors report no relevant competing
interest.
Authors' information
Dr. Zebing Zheng, Department of Pediatric General
Thoracic and Urinary Surgery, Affiliated Hospital of Zunyi Medical
College. 149 Dalian Road, Zunyi, Guizhou 563000, P.R. China.
E-mail: Zebing1988@sina.com. Telephone:
+86-851-28608446.
References
|
1
|
Stensrud KJ, Emblem R and Bjonland K: Anal
endosonography and bowel function in patients undergoing different
types of endorectal pull-through procedures for Hirschsprung
disease. J Pediatr Surg. 50:1341–1346. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang S, Li J, Wu Y, Hu Y, Duan C, Wang M
and Gai Z: Comparison of laparoscopic-assisted operations and
laparotomy operations for the treatment of hirschsprung disease:
evidence from a meta-analysis. Medicine (Baltimore). 94:e16322015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tomuschat C, Zimmer J and Puri P:
Laparoscopic-assisted pull-through operation for Hirschsprung's
disease: A systematic review and meta-analysis. Pediatr Surg Int.
32:751–757. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xiong X, Chen X, Wang G and Feng J: Long
term quality of life in patients with Hirschsprung's disease who
underwent heart-shaped anastomosis during childhood: A twenty-year
follow-up in China. J Pediatr Surg. 50:2044–2047. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Puri P: Hirschsprung's diseasePediatric
Surgery. Puri P and Höllwarth M: Springer; Berlin: pp. 275–288.
2005
|
|
6
|
Zhang JS, Li L, Hou WY, Liu SL, Diao M,
Zhang J, Ming AX and Cheng W: Transanal rectal mucosectomy and
partial internal anal sphincterectomy for Hirschsprung's disease. J
Pediatr Surg. 49:831–834. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Langer JC, Minkes RK, Mazziotti MV,
Skinner MA and Winthrop AL: Transanal one-stage Soave procedure for
infants with Hirschsprung's disease. J Pediatr surg. 34:148–151.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
De La Torre L and Ortega A: Transanal
versus open endorectal pull-through for Hirschsprung's disease. J
Pediatr surg. 35:1630–1632. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Georgeson KE, Cohen RD, Hebra A, Jona JZ,
Powell DM, Rothenberg SS and Tagge EP: Primary
laparoscopic-assisted endorectal colon pull-through for
Hirschsprung's disease: A new gold standard. Ann Surg. 229:678–683.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Thomson D, Allin B, Long AM, Bradnock T,
Walker G and Knight M: Laparoscopic assistance for primary
transanal pull-through in Hirschsprung's disease: A systematic
review and meta-analysis. BMJ Open. 5:e0060632015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Granström AL, Husberg B, Nordenskjöld A,
Svensson PJ and Wester T: Laparoscopic-assisted pull-through for
Hirschsprung's disease, a prospective repeated evaluation of
functional outcome. J Pediatr surg. 48:2536–2539. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Khazdouz M, Sezavar M, Imani B, Akhavan H,
Babapour A and Khademi G: Clinical outcome and bowel function after
surgical treatment in Hirschsprung's disease. Afr J Paediatr Surg.
12:143–147. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang SC, Bai YZ, Wang W and Wang WL:
Clinical outcome in children after transanal 1-stage endorectall
pull-through operation for Hirschsprung's disease. J Pediatr Surg.
40:1307–1311. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Elhalaby EA, Teitelbaum DH, Coran AG and
Heidelberger KP: Enterocolitis associtated with Hirschsprung's
disease: A clinical histopathological correlative study. J Pediatr
Surg. 30:1023–1027. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
El-Sawaf MI, Drongowski RA, Chamberlain
JN, Coran AG and Teitelbaum DH: Are the long-term results of the
transanal pull-through equal to those of the transabdominal
pull-through? A comparison of the 2 approaches for Hirschsprung's
disease. J Pediatr Surg. 42:41–47. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dickie BH, Webb KM, Eradi B and Levitt MA:
The problematic Soave cuff in Hirschsprung disease: Manifestations
and treatment. J Pediatr Surg. 49:77–80. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rouzrokh M, Jadali F, Gharib A,
Khaleghnejad-Tabari A, Tavassoli A and Mohajerzadeh L: Can we rely
on frozen sections of a rectal biopsy for one-stage trans-anal
pull-through operation in hirschsprung's disease? Iran J Pediatr.
21:72–76. 2011.PubMed/NCBI
|
|
18
|
Agrawal RK, Kakkar N, Vasishta RK, Kumari
V, Samujh R and Rao KL: Acetylcholinesterase histochemistry
(AChE)-A helpful technique in the diagnosis and in aiding the
operative procedures of Hirschsprung disease. Diagn Pathol.
10:2082015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Podevin G, Lardy H, Azzis O, Branchereau
S, Petit T, Sfeir R, Weil D, Heloury Y and Fremond B: Technical
problems and complications of transanal pull-through for
Hirschsprung's disease. Eur J Pediatr Surg. 16:104–108. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ishihara M, Yamataka A, Kaneyama K, Koga
H, Kobayashi H, Lane GJ and Miyano T: Prospective analysis of
primary modified Georgeson's laparoscopy-assisted endorectal
pull-through for Hirschsprung's disease: Short-to mid-term results.
Pediatr Surg Int. 21:878–882. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tang ST, Wang GB, Cao GQ, Wang Y, Mao YZ,
Li SW, Li S, Yang Y, Yang J and Yang L: 10 years of experience with
laparoscopic-assisted endorectal Soave pull-through procedure for
Hirschsprung's disease in China. J Laparoendosc Adv Surg Tech A.
22:280–284. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Aubdoollah TH, Li K, Zhang X, Li S, Yang
L, Lei HY, Dolo PR, Xiang XC, Cao GQ, Wang GB and Tang ST: Clinical
outcomes and ergonomics analysis of three laparoscopic techniques
for Hirschsprung's disease. World J Gastroenterol. 21:8903–8911.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Menezes M, Corbally M and Puri P:
Long-term results of bowel function after treatment for
Hirschsprung's disease: A 29-year review. Pediatr Surg Int.
22:987–990. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Huang Y, Zheng S and Xiao X: A follow-up
study on postoperative function after a transanal Soave 1-stage
endorectal pull-through procedure for Hirschsprung's disease. J
Pediatr Surg. 43:1691–1695. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ishikawa N, Kubota A, Kawahara H, Hasegawa
T, Okuyama H, Uehara S and Mitani Y: Transanal mucosectomy for
endorectal pull-through in Hirschsprung's disease: Comparison of
abdominal, extraanal and transanal approaches. Pediatr Surg Int.
24:1127–1129. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dahal GR, Wang JX and Guo LH: Long-term
outcome of children after single-stage transanal endorectal
pull-through for Hirschsprung's disease. World J Pediatr. 7:65–69.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Van de Ven TJ, Sloots CE, Wijnen MH,
Rassouli R, van Rooij I, Wijnen RM and de Blaauw I: Transanal
endorectal pull-through for classic segment Hirschsprung's disease:
With or without laparoscopic mobilization of the rectosigmoid? J
Pediatr Surg. 48:1914–1918. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Y, Nah SA, Laksmi NK, Ong CC, Chua
JH, Jacobsen A and Low Y: Transanal endorectal pullthrough versus
transabdominal approach for Hirschsprung's disease: A systematic
review and meta-analysis. J Pediatr Surg. 48:642–651. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rescorla FJ, Morrison AM, Engles D, West
KW and Grosfeld JL: Hirschsprung's disease. Evaluation of mortality
and long-term function in 260 cases. Arch Surg. 127:934–942. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kim AC, Langer JC, Pastor AC, Zhang L,
Sloots CE, Hamilton NA, Neal MD, Craig BT, Tkach EK, Hackam DJ, et
al: Endorectal pull-through for Hirschsprung's disease-a
multicenter, long-term comparison of results: Transanal vs
transabdominal approach. J Pediatr Surg. 45:1213–1220. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Miyano G, Koga H, Okawada M, Doi T,
Sueyoshi R, Nakamura H, Seo S, Ochi T, Yamada S, Imaizumi T, et al:
Rectal mucosal dissection commencing directly on the anorectal line
versus commencing above the dentate line in laparoscopy-assited
transanal pull-through for Hirschsprung's disease: prospective
medium-term follow-up. J Pediatr Surg. 50:2041–2043. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Giuliani S, Betalli P, Narciso A, Grandi
F, Midrio P, Mognato G and Gamba P: Outcome cpmparison among
laparoscopic Duhamel, laparotomic Duhamel and transanal endorectal
pull-through: A single-center, 18-year experience. J Laparoendosc
Adv Surg Tech A. 21:859–863. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yan Z, Poroyko V, Gu S, Zhang Z, Pan L,
Wang J, Bao N and Hong L: Characterization of the intestinal
microbiome of Hirschsprung's disease with and without
enterocolitis. Biochem Biophys Res Commun. 445:269–274. 2014.
View Article : Google Scholar : PubMed/NCBI
|