Introduction
Thromboangiitis obliterans (TAO) is a common
peripheral vascular disease, which is endarteritis jointly caused
by T cell-mediated cellular immunity and B cell-mediated humoral
immunity (1,2). The vascular endothelial cell functions
of TAO patients are severely damaged, among which the expression of
intercellular adhesion molecule-1 (ICAM-1) and vascular cell
adhesion molecule-1 (VCAM-1) are increased in thickened vascular
endothelial cells and some inflammatory cells, seriously harming
life and health (3,4). Cilostazol is a phosphodiesterase
inhibitor, which inhibits cyclic adenosine monophosphate (cAMP)
degradation and transformation by inhibiting the cAMP
phosphodiesterase activity in platelets and smooth muscle cells,
ultimately leading to the increased cAMP level in platelets and
blood vessels (5). Cilostazol has
significant effects of dilating blood vessels and inhibiting
platelet aggregation, but its role in TAO has not been reported
yet.
In the present study, the effects of cilostazol on
the expression of ICAM-1, VCAM-1 and inflammatory factors in plasma
in TAO patients were investigated to clarify the roles of
cilostazol in the occurrence and development of TAO.
Patients and methods
Patients
Patients in the TAO and cilostazol groups were
diagnosed with TAO in the Affiliated Hospital of Shandong
University of Traditional Chinese Medicine (Jinan, China). It was
confirmed by color Doppler flow imaging instrument that all
patients suffered from peripheral arterial ischemia to varying
degrees. In the TAO group, there were 23 patients, including 13
males and 10 females, aged 34–55 years. In the cilostazol group,
there were 20 patients, 12 males and 8 females, aged 32–56 years,
who were treated with administration of cilostazol (50 mg/time,
twice a day). In the control group, there were 22 healthy subjects,
including 12 males and 10 females, aged 35–50 years; patients with
hypertension, hyperlipidemia or cardiovascular and cerebrovascular
organic diseases were eliminated. There were no significant
differences in the sample size, sex and the age of subjects among
the three groups. The study was approved by the Ethics Committee of
Affiliated Hospital of Shandong University of Traditional Chinese
Medicine (Shandong, China). Signed written informed consents were
obtained from the patients and/or guardians.
Main reagents
Enzyme-linked immunosorbent assay (ELISA) kits were
obtained from R&D Systems (Minneapolis, MN, USA); the
bicinchoninic acid (BCA) protein quantification kit was purchased
from Beyotime Institute of Biotechnology (Shanghai, China); TRIzol
total RNA extraction kits were obtained from Tiangen Biotech, Co.,
Ltd., (Beijing, China); reverse transcription-polymerase chain
reaction (RT-PCR) kits were purchased from Tiangen Biotech;
glyceraldehyde-3-phosphate dehydrogenase (GAPDH), as well as ICAM-1
and VCAM-1 monoclonal antibodies were obtained from Cell Signaling
Technology (Danvers, MA, USA).
Experimental methods
Blood routine examinations
Fasting elbow venous blood (4 ml) was drawn from all
the subjects in the control, TAO and cilostazol groups in the early
morning. Heparin sodium was used for anticoagulation of samples
used in blood rheology examination; the plasma viscosity,
fibrinogen, total cholesterol (TC) and triglyceride (TG) levels in
each group were detected, respectively, and the differences among
the three groups were compared.
Detection of ICAM-1 and VCAM-1
expression levels via ELISA
The ICAM-1 and VCAM-1 expression levels in the
control, TAO and cilostazol groups were detected using the human
ICAM-1 and VCAM-1 ELISA kits, and the expression differences were
recorded.
RT-PCR analyses of
inflammation-related factors
Appropriate number of tissues in the control, TAO
and cilostazol groups were quickly transferred into 1 ml TRIzol
reagent for full tissue grinding to prodcue homogenate. After 5-min
standing at room temperature, the sample was completely cleaved,
followed by centrifugation at 12,000 × g at 4°C for 5 min. The
supernatant was carefully removed, added with chloroform and mixed
evenly, and after 5-min standing at room temperature, the mixture
was centrifuged at 12,000 × g at 4°C for 15 min. The supernatant
was carefully taken and added with the same volume of isopropanol,
and after 10-min standing at room temperature, the mixture was
centrifuged at 12,000 × g at 4°C for 10 min. The sediment was
retained, added with 75% ethanol and mixed evenly to wash the RNA
sediment. Finally, RNase-free water was added to fully dissolve the
sediment. The optical density (OD)260/OD280
ratio and the RNA concentration were measured. The amplification
was performed step by step based on the primer sequences shown in
Table I according to the protocol,
and the RT-PCR analyses were performed for reaction products.
 | Table I.Primer sequences in RT-PCR. |
Table I.
Primer sequences in RT-PCR.
| Genes | Forward primer
(5–3) | Reverse primer
(5–3) |
|---|
| Human β-actin |
GAGCCGGGAAATCGTGCGT |
GGAAGGAAGGCTGGAAGATG |
| Human IL-1β |
CTGAGCACCTTCTTTCCCTTCA |
TGGACCAGACATCACCAAGCT |
| Human IL-6 |
TGGCTGAAAAAGATGGATGCT |
TCTGCACAGCTCTGGCTTGT |
| Human TNF-α |
TGTAGCCCATGTTGTAGCAAACC |
GAGGACCTGGGAGTAGATGAGGTA |
RT-PCR analyses of ICAM-1 and
VCAM-1
Tissues in the control, TAO and cilostazol groups
were transferred into an Eppendorf (EP) tube containing RNAiso Plus
extract. After 5-min standing at room temperature, the sample was
completely cleaved, followed by centrifugation at 12,000 × g at 4°C
for 5 min. Then, the supernatant was added with 0.2 ml chloroform
and mixed evenly, and after 5-min standing at room temperature, the
mixture was centrifuged at 12,000 × g at 4°C for 15 min. The
supernatant was added with the same volume of isopropanol, and
after 10-min standing at room temperature, the mixture was
centrifuged at 12,000 × g at 4°C for 10 min; the supernatant was
removed carefully and the sediment was retained, added with 1 ml
75% ethanol and mixed evenly, followed by centrifugation at 12,000
× g at 4°C for 5 min. Then the supernatant was removed carefully,
and the above procedures were repeated once. After RNA sediment was
washed, the solution was discarded, and RNase-free water was added.
Part of total RNA solution was diluted into 1 µg/µl, and the
reverse transcription reaction solution was prepared according to
instructions of PrimeScript® RT Reagent kit with gDNA
Eraser, and the corresponding RNA samples were added for reverse
transcription to obtain complementary DNA (cDNA). cDNA was stored
at −20°C, and the mRNA level was detected according to the
instructions of the SYBR® Premix Ex Taq™ II (Tli RNaseH
Plus) kit. Primer sequences used were: ICAM-1: 5′-3′AGGTGTGATATCCGG
TAGAA; 3′-5′ CCTTCTAAGTGGTTGGAACA; VCAM-1: 5′-3′
TCTACGCTGACAATGAATCC; 3′-5′ ACTTGACTG TGATCGGCTTC.
Western blot analysis of ICAM-1 and
VCAM-1
Tissues in the control, TAO and cilostazol groups
were taken and washed with ice cold normal saline. According to the
instructions of the whole protein extraction kit,
immunoprecipitation (IP) lysate containing phenylmethanesulfonyl
fluoride (PMSF) and protease inhibitors was added and tissues were
fully ground on ice. Then, the tissue homogenate was centrifuged at
12,000 × g at 4°C for 10 min; the supernatant was taken and
centrifuged at 12,000 × g at 4°C for 20 min, and the supernatant
was collected again. After protein quantification according to the
instructions of the protein kit, the protein sample containing the
same amount of total protein was added into each well, followed by
sodium dodecyl sulfate polyacrylamide gel electrophoresis
(SDS-PAGE) under constant pressure of 220 V, until the bromophenol
blue reached the bottom of the gel. Based on the molecular weight
of the target protein, the gel was cut and the isolated protein was
transferred onto the polyvinylidene fluoride (PVDF) membrane. The
protein-attached PVDF membrane was sealed in 5% skim milk powder at
room temperature for 3 h on a shaker and incubated with the
corresponding primary antibody (1:1,000) at 4°C overnight. The next
day, the membrane was fully washed with TTBS (10 min/time, 3
times), incubated with the secondary antibody (1:2,000) at room
temperature for 1 h, and washed again with TTBS (10 min/time, 3
times), followed by color development using ECL developing solution
and photography. Finally, the bands were analyzed and data were
processed.
Statistical analysis
Experimental data are presented as mean ± standard
deviation (SD). Statistical Product and Service Solutions (SPSS)
17.0 software (SPSS, Inc., Chicago, IL, USA) was used for the
statistical analysis of experimental results. The t-test was used
for the comparison of means between two groups. One-way analysis of
variance (ANOVA) followed by post hoc test (Least Significant
Difference) was used for the comparison of means among groups.
P-test was used for the pairwise comparison. P<0.05 indicated
the difference was statistically significant.
Results
Effects of cilostazol on TAO-induced
abnormalities in routine blood tests
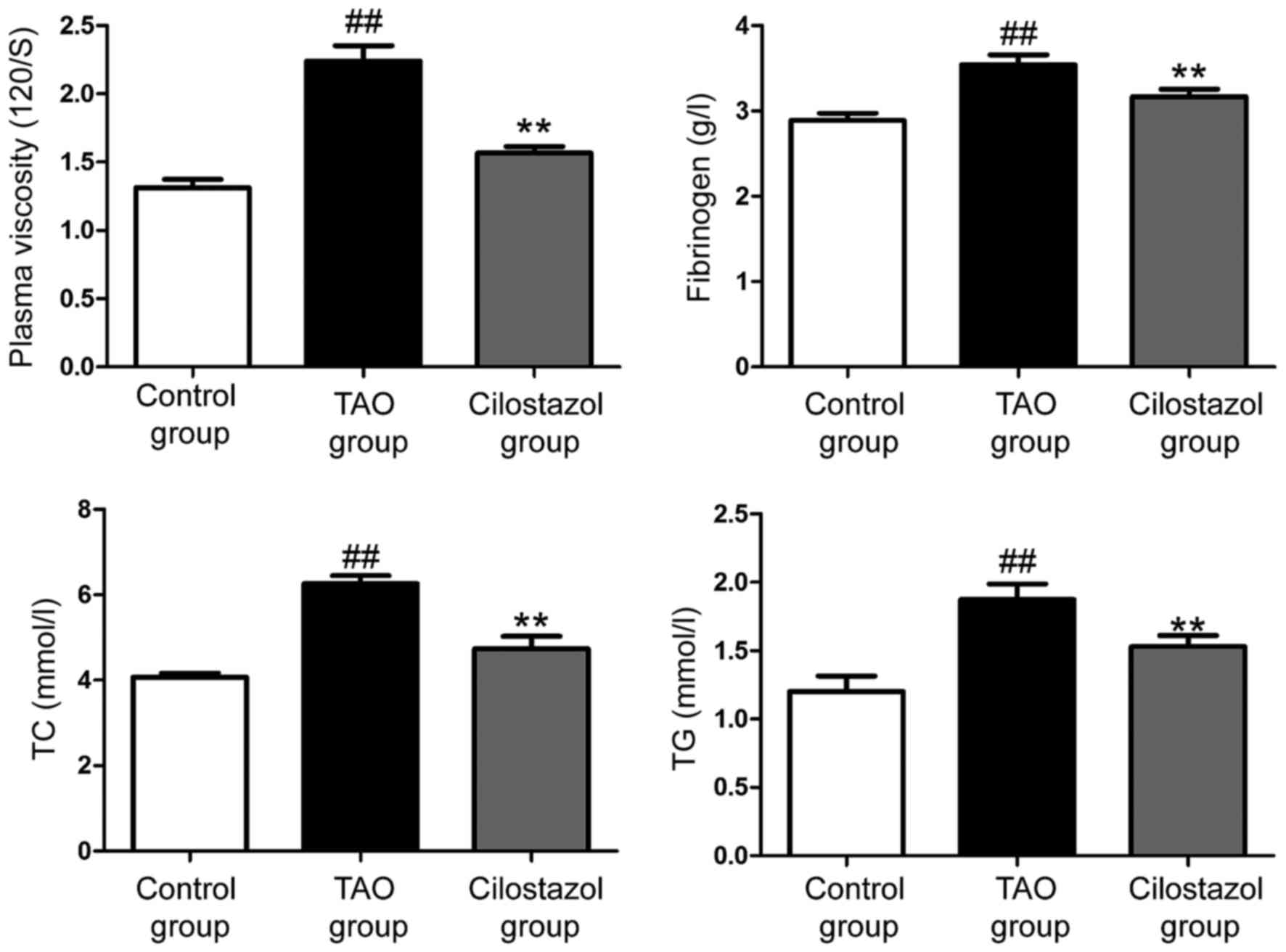
Compared with those in the control group, the plasma
viscosity, fibrinogen, TC and TG levels in the TAO group were
significantly increased. Compared with those in the TAO group, the
plasma viscosity, fibrinogen, TC and TG levels in the cilostazol
group were significantly decreased, suggesting that cilostazol can
effectively affect the TAO-induced abnormalities in routine blood
tests and improve TAO (Fig. 1).
Detection of ICAM-1 and VCAM-1
expression in each group via ELISA
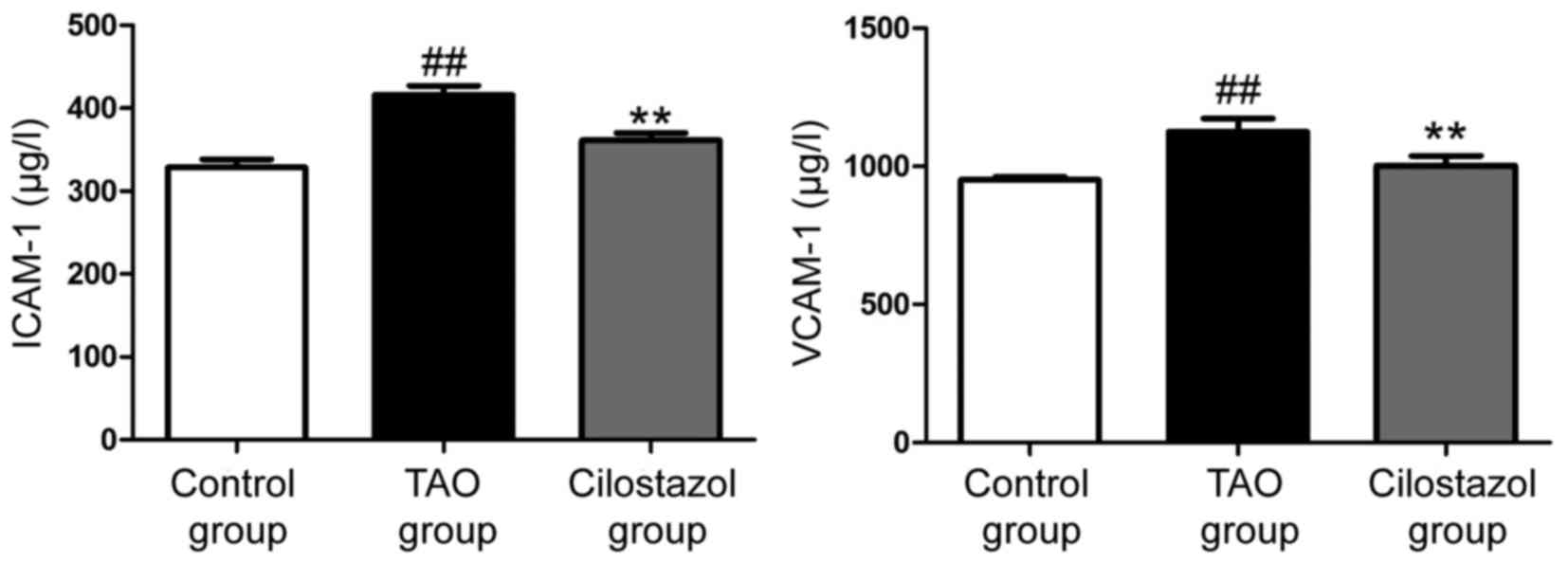
The expression of ICAM-1 and VCAM-1 in the control,
TAO and cilostazol groups were detected using the ELISA kit. The
results showed that ICAM-1 and VCAM-1 expression levels in the TAO
group were obviously increased compared with those in the control
group. ICAM-1 and VCAM-1 expression levels in the cilostazol group
were obviously decreased compared with those in the TAO group,
indicating that cilostazol can reduce the TAO-induced abnormal
expression of ICAM-1 and VCAM-1 (Fig.
2).
RT-PCR results of inflammation-related
factors
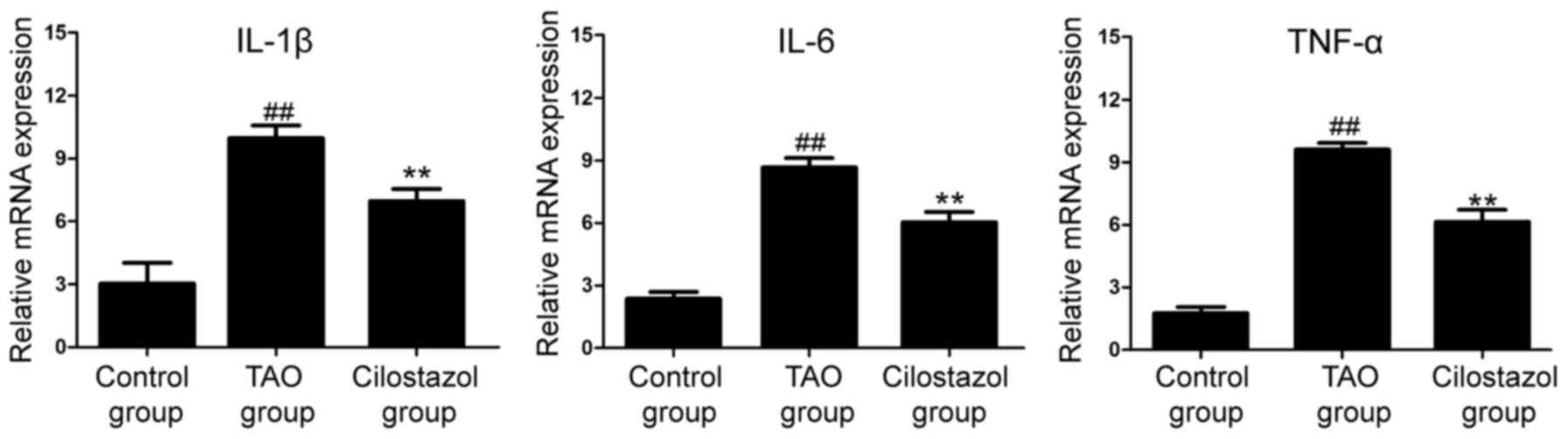
Total RNA was extracted from the control group, the
TAO group and the cilostazol group, and RT-PCR was performed. The
results revealed that the mRNA expression levels of IL-1β, IL-6 and
TNF-α in the TAO group were significantly higher than those in the
control group, while the levels in the cilostazol group were
significantly decreased compared with those in the TAO group
(Fig. 3).
RT-PCR results of ICAM-1 and
VCAM-1
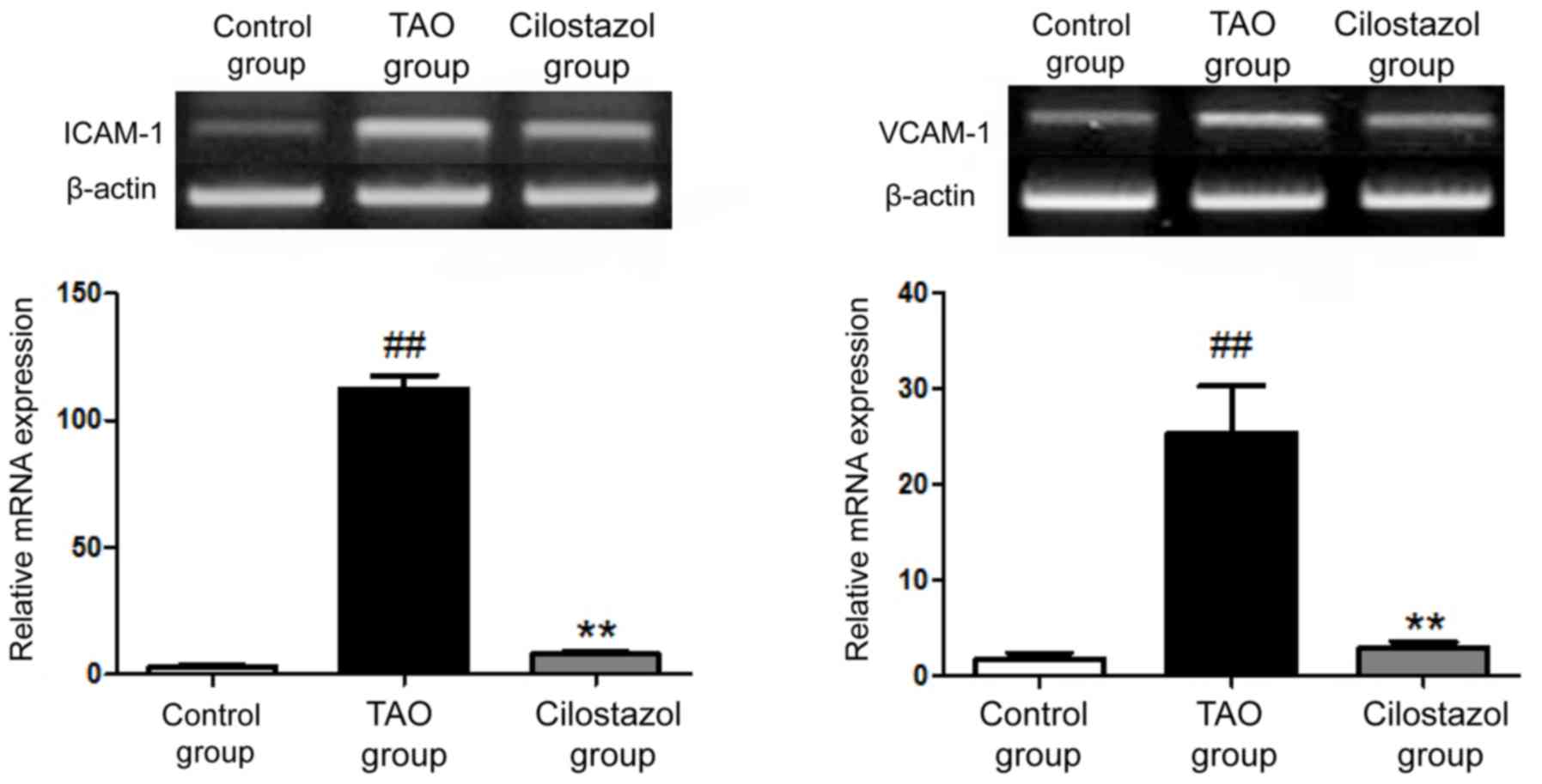
RT-PCR showed that the mRNA expression of ICAM-1 and
VCAM-1 in the TAO group was significantly increased, which was
effectively reversed after administration of cilostazol (Fig. 4).
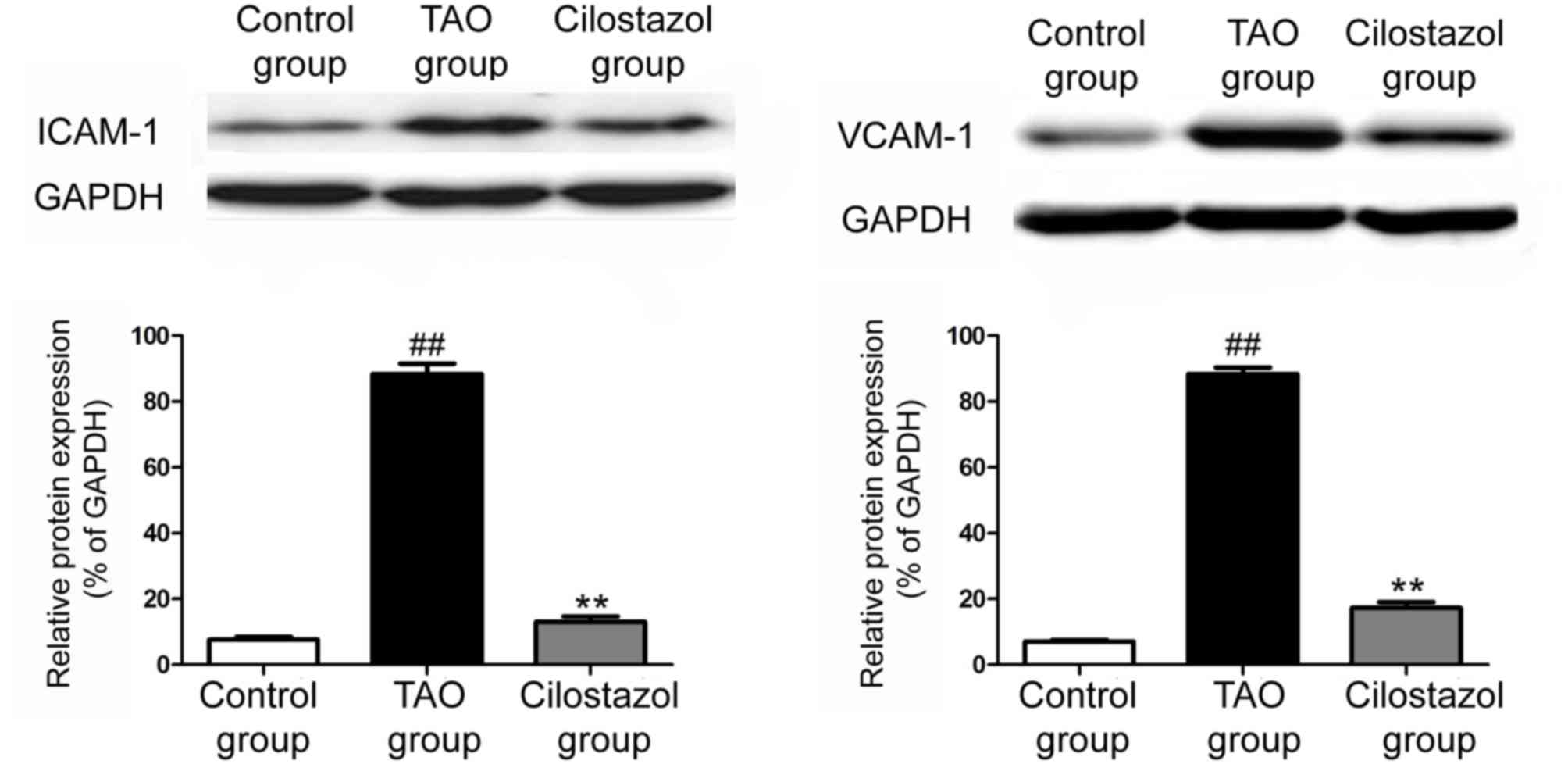
Western blot results of ICAM-1 and
VCAM-1
The protein expression of ICAM-1 and VCAM-1 in the
control group, the TAO group and the cilostazol group were detected
via western blotting. The results revealed that the protein
expressions of ICAM-1 and VCAM-1 in the TAO group were
significantly increased, which were obviously decreased after
administration of cilostazol (Fig.
5).
Discussion
Thromboangiitis obliterans (TAO) is a disease with
unknown cause and mechanism, mainly involving the middle and small
arteries and veins in upper and lower limbs (6). TAO seriously endangers people's lives,
therefore effective treatment for TAO has been investigated to
clarify its molecular mechanism (7–9).
Cilostazol, as a selective PDE-III inhibitor, is clinically widely
used in the treatment of peripheral vascular diseases caused by
metabolic syndrome and intermittent claudication (10,11),
which can significantly reduce the levels of soluble adhesion
molecules (such as ICAM-1 and VCAM-1) in plasma in diabetic
patients, thereby delaying the development of microvascular disease
(12).
With the deepening of study using immune biochemical
techniques, a variety of factors have been found to be involved in
the occurrence and development of TAO, such as inflammation,
apoptosis, oxidative stress, macrophages and lymphocytes (13–15).
ICAM-1 is expressed on the vascular endothelium and binds to the
ligand to promote the firm adhesion between monocytes and
endothelial cells (16–18). Moreover, ICAM-1 is highly expressed
in TAO, which is closely related to the TAO-induced increased
expression of inflammatory factors, such as IL-1β, IL-6 and TNF-α.
In addition, VCAM-1 is expressed in vascular endothelial cells,
which mediates the adhesion among lymphocytes, monocytes and
endothelial cells and participates in many important
pathophysiological processes, and it may be an important indicator
for vascular dysfunction or vascular disease progression. It has
been reported that the incidence of TAO is closely related to
ICAM-1 and VCAM-1 (19,20).
In this study, routine blood examinations (plasma
viscosity, fibrinogen, TC and TG levels) were performed for the
control group, the TAO group and the cilostazol group,
respectively. The routine blood examination results showed that
compared with those in the control group, the plasma viscosity,
fibrinogen, TC and TG levels in TAO group were significantly
increased; compared with those in the TAO group, the plasma
viscosity, fibrinogen, TC and TG levels in the cilostazol group
were significantly decreased. Then the differences of ICAM-1 and
VCAM-1 expression in the three groups were detected via ELISA. The
results showed that ICAM-1 and VCAM-1 expression levels in the TAO
group were obviously increased compared with those in the control
group; ICAM-1 and VCAM-1 expression levels in the cilostazol group
were obviously decreased compared with those in the TAO group.
Besides, the mRNA expression of IL-1β, IL-6 and TNF-α in the three
groups were detected via RT-PCR. The results revealed that the mRNA
expression levels of IL-1β, IL-6 and TNF-α in the TAO group were
significantly higher than those in the control group, while the
levels in the cilostazol group were significantly decreased
compared with those in the TAO group. The mRNA and protein
expressions of ICAM-1 and VCAM-1 in the three groups were detected
via RT-PCR and western blotting, respectively. It was found that
both mRNA and protein expression of ICAM-1 and VCAM-1 in the TAO
group were significantly increased, which were obviously decreased
after administration of cilostazol. Moreover, the results of ANOVA
showed that the differences of ICAM-1 and VCAM-1 expression were
statistically significant among the control group, the TAO group
and the cilostazol group.
In conclusion, cilostazol can significantly reduce
the TAO-induced abnormal increase in ICAM-1, VCAM-1 and
inflammatory factor expression in plasma of patients. It was proven
that cilostazol has a good anti-TAO effect. We expect that
cilostazol, as an anti-inflammatory drug, can provide a new,
feasible and effective solution for the prevention and treatment of
TAO in the future.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
FS and BJ designed the study. TC and FS collected
the patient data. BJ and TC analyzed the patient data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Affiliated Hospital of Shandong University of Traditional Chinese
Medicine (Jinan, China). Signed written informed consents were
obtained from the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
References
|
1
|
Wysokinski WE, Kwiatkowska W,
Sapian-Raczkowska B, Czarnacki M, Doskocz R, Kowal-Gierczak B and
Wysokinski WE: Sustained classic clinical spectrum of
thromboangiitis obliterans (Buergers disease). Angiology.
51:141–150. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tse TS, Mcbane RD, Stanson AW, Ballman KV,
Mikhail MA and Cooper LT: Secular trends and long-term survival in
thromboangiitis obliterans. J Am Coll Cardiol. 39:2652002.
View Article : Google Scholar
|
|
3
|
Sasaki S, Sakuma M and Yasuda K: Current
status of thromboangiitis obliterans (Buergers disease) in Japan.
Int J Cardiol. 75 Suppl 1:S175–S181. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sun XL, Law BY, de Seabra Rodrigues Dias
IR, Mok SWF, He YZ and Wong VK: Pathogenesis of thromboangiitis
obliterans: Gene polymorphism and immunoregulation of human
vascular endothelial cells. Atherosclerosis. 265:258–265. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marchetti C, Poggi P, Cornaglia AI, Farina
A and Rizzo S: Morphologic characteristics of initial lymphatics of
the healthy and diseased human gingiva. Anat Rec. 255:175–179.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Iwai T: Periodontal bacteremia and various
vascular diseases. J Periodontal Res. 44:689–694. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen YW, Nagasawa T, Wara-Aswapati N,
Ushida Y, Wang D, Takeuchi Y, Kobayashi H, Umeda M, Inoue Y, Iwai
T, et al: Association between periodontitis and anti-cardiolipin
antibodies in Buerger disease. J Clin Periodontol. 36:830–835.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen Z, Takahashi M, Naruse T, Nakajima T,
Chen YW, Inoue Y, Ishikawa I, Iwai T and Kimura A: Synergistic
contribution of CD14 and HLA loci in the susceptibility to Buerger
disease. Hum Genet. 122:367–372. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maslowski L, McBane R, Alexewicz P and
Wysokinski WE: Antiphospholipid antibodies in thromboangiitis
obliterans. Vasc Med. 7:259–264. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Undas A, Nowakowski T, Cieśla-Dul M and
Sadowski J: Abnormal plasma fibrin clot characteristics are
associated with worse clinical outcome in patients with peripheral
arterial disease and thromboangiitis obliterans. Atherosclerosis.
215:481–486. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zheng P, Chen SJ and Shao HZ: Studies on
hypercoagulation state in thromboangiitis obliterans. Chin Med J
(Engl). 102:67–71. 1989.PubMed/NCBI
|
|
12
|
Avcu F, Akar E, Demirkiliç U, Yilmaz E,
Akar N and Yalçin A: The role of prothrombotic mutations in
patients with Buergers disease. Thromb Res. 100:143–147. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Brodmann M, Renner W, Stark G, Winkler M,
Pabst E, Hofmann C and Pilger E: Prothrombotic risk factors in
patients with thrombangitis obliterans. Thromb Res. 99:483–486.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dellalibera-Joviliano R, Joviliano EE and
Evora PR: Determination of kininogens levels and
kallikrein/kininase II activities in patients with thromboangiitis
obliterans. Scand J Immunol. 72:128–133. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Idei N, Nishioka K, Soga J, Hidaka T, Hata
T, Fujii Y, Fujimura N, Maruhashi T, Mikami S, Teragawa H, et al:
Vascular function and circulating progenitor cells in
thromboangitis obliterans (Buergers disease) and atherosclerosis
obliterans. Hypertension. 57:70–78. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Azizi M, Boutouyrie P, Bura-Rivière A,
Peyrard S, Laurent S and Fiessinger JN: Thromboangiitis obliterans
and endothelial function. Eur J Clin Invest. 40:518–526. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Halacheva K, Gulubova MV, Manolova I and
Petkov D: Expression of ICAM-1, VCAM-1, E-selectin and TNF-α on the
endothelium of femoral and iliac arteries in thromboangiitis
obliterans. Acta Histochem. 104:177–184. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Luo Y, Feng J, Xu Q, Wang W and Wang X:
NSun2 deficiency protects endothelium from inflammation via mRNA
methylation of ICAM-1. Circ Res. 118:944–956. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Slavov ES, Stanilova SA, Petkov DP and
Dobreva ZG: Cytokine production in thromboangiitis obliterans
patients: New evidence for an immune-mediated inflammatory
disorder. Clin Exp Rheumatol. 23:219–226. 2005.PubMed/NCBI
|
|
20
|
Małecki R, Zdrojowy K and Adamiec R:
Thromboangiitis obliterans in the 21st century: a new face of
disease. Atherosclerosis. 206:328–334. 2009. View Article : Google Scholar : PubMed/NCBI
|