Introduction
In orthopedic surgery, flap grafting is the most
commonly used method for organ reconstruction or repair of tissue
defect and deformity. However, in this process part or whole of the
flap may undergo necrosis, which is a serious consequence due to
ischemia-reperfusion injury (1).
Although the exact mechanism underlying
ischemia-reperfusion injury has not been confirmed thus far, a
variety of protective therapies against ischemia-reperfusion injury
were reported, such as applications of low temperature, hydrogen,
or antioxidants (2–5). In addition, it was found that
activation of the p38 MAPK signaling pathway led to increased
expression of NF-κB and promoted the secretion and release of
inflammatory factors (such as IL-6, and TNF-α), which played an
important role in the occurrence and progression of
ischemia-reperfusion injury (6,7).
SB202190 is a specific inhibitor of the P38 MAPK signaling pathway
(8).
In this study, the mechanism underlying flap
ischemia-reperfusion injury was explored by treatment of flap
ischemia-reperfusion injury rat models with SB202190. The mRNA and
protein expression levels of NF-κB and IL-6 in the flap, as well as
the IL-6 concentration in serum were measured.
Materials and methods
Materials
The following materials were purchased from
different sources: 48 healthy specific pathogen-free (SPF) male
Sprague-Dawley rats weighing 250–300 g from Jiangsu University
Animal Center; the enzyme-linked immunosorbent assay reader from
BioTek Instruments, Inc. (Winooski, VT, USA); the optical
microscopy and image acquisition system from Olympus Corporation,
Tokyo, Japan; the rat IL-6 enzyme-linked immunosorbent assay
(ELISA) kit and RT-PCR kit from R&D Systems, Inc. (Minneapolis,
MN, USA); the internal reference β-actin, NF-κB p65, IL-6 primary
and secondary antibodies from Abcam (Cambridge, UK); the cDNA
synthesis kit from Tiangen Biotech Co. Ltd. (Beijing, China); the
BCA kit from Beyotime Biotechnology (Shanghai, China); SB202190
from Cayman Chemical Company (Ann Arbor, MI, USA); and TRIzol and
RIPA lysate from Invitrogen; Thermo Fisher Scientific, Inc.,
(Waltham, MA, USA).
Methods
Establishment of animal models
Rats were anesthetized via an intraperitoneal
injection of ketamine (100 mg/kg), followed by fixation on the
operating plate. After treatment of abdominal hair removal and
alcohol disinfection, the superficial inferior epigastric
arteriovenous flap was constructed according to literature
(9). A rectangular flap with a size
of 3×6 cm was created by dissection of the whole skin layer to the
fascia on the abdominal wall with a scalpel. Attention was paid not
to injure the superficial inferior epigastric artery pedicle,
because the superficial inferior epigastric artery and vein were
the only vessels for blood circulation in the flap.
Experimental grouping and
treatments
Forty-eight rats were randomly divided into four
groups of 12 each. In the control group, after a flap was created
the incision was sutured in situ with the 3-0 silk thread.
In the ischemia-reperfusion group, after a flap was created the
superficial inferior epigastric artery and vein were clamped with
microvascular clips for 8 h of ischemia. Following removal of the
vessel clips and restoration of normal blood flow, the flap
incision was sutured in situ. In the saline group, the rats
received an intraperitoneal injection of normal saline (2 ml/kg) on
the 2nd, 4th and 6th day after undergoing the same treatment as the
ischemia-reperfusion group. In the inhibitor group, the rats
received an intraperitoneal injection of SB202190 (2 µg/kg) on the
2nd, 4th and 6th day after undergoing the same treatment as the
ischemia-reperfusion group. This study was approved by the Animal
Ethics Committee of Jinan Municipal Hospital of Traditional Chinese
Medicine (Jinan, China).
Observed indicators
Flap survival rate
On the 7th day after surgery, an image of the flap
was taken with a digital camera for rats in all the groups. The
flap survival rate was obtained by analysis of the image with the
Image-Pro Plus. V6.0 software (Olympus) using the equation:
survival rate = flap survival area / total area × 100%.
IL-6 concentration in serum
On the 7th day after surgery, 2 ml of blood was
extracted from the superficial inferior epigastric vein for rats in
all the groups. The serum was obtained after centrifugation at
3,000 × g for 10 min at 27°C, in which the IL-6 concentration was
measured using enzyme-linked immunosorbent assay.
Measurement of NF-κB and IL-6 levels
in flap tissue
On the 7th day after operation, the appropriate
amount of flap tissue was harvested from rats in each group, and
was treated with the appropriate amount of TRIzol reagent to
extract total RNA. Then cDNA was synthesized from RNA using cDNA
synthesis kit. Amplification of IL-6, NF-κB and internal reference
β-actin was achieved by RT-PCR. The RT-PCR reaction conditions
were: 95°C for 2 min; then 40 cycles of 95°C for 20 sec, 56°C for
20 sec, 72°C for 20 sec; 72°C for 5 min; 95°C for 15 sec; 60°C for
15 sec; 60–95°C for 20 min; and finally 95°C for 15 sec. The mRNA
expression levels of NF-κB and IL-6 were calculated by using the
amplification curve. The primer sequences of each gene are listed
in Table I. In a separate
experiment, an appropriate amount of flap tissue was harvested and
homogenized in appropriate amount of RIPA lysis butter. Total
protein was extracted from the homogenate, and the protein
concentration was measured using a BCA kit. A sample containing 100
µg of proteins was applied to SDS-PAGE gel electrophoresis and
transferred to the PVDF membrane using a wet system. The rabbit
anti-rat NF-κB, IL-6, β-actin primary polyclonal antibodies (1:500;
cat. nos. 14220-1-AP, 21865-1-AP, 20536-1-AP, respectively;
ProteinTech Group, Inc., Wuhan, China) was added after the membrane
was blocked with 5% BSA at room temperature for 2 h followed by
incubation at 4°C overnight. The membrane was rinsed a few times,
followed by the addition of the goat anti-rabbit secondary
polyclonal antibody (1:2,000; cat. no. SA00001-2; ProteinTech
Group, Inc.) and incubation at room temperature for 2 h. After
three rinses, the ECL developer was applied to the membrane in a
dark chamber. Images were obtained using fluorescence imaging
techniques. The images were scanned, and the gray value as well as
area of each band was analyzed using the Image Pro Plus 6.0
software.
 | Table I.Primer sequences of each gene. |
Table I.
Primer sequences of each gene.
| Gene | Primer sequence |
|---|
| IL-6 | Up:
5′-GACTGATGTTGCTGACAGCCACTGC-3′ |
|
| Down:
5′-TAGCCACTGCTTCTGTGACTCTAACT-3′ |
| NF-κB | Up:
5′-CCAGGCGGACATCTACAA-3′ |
|
| Down:
5′-CAAGGCCAAATGAAAGGA-3′ |
| β-actin | Up:
5′-CCTAAGGCCAACCGTGAA-3′ |
|
| Down:
5′-CTGGAAGGTGGCAGTGAG-3′ |
Statistical analysis
The SPSS 19.0 software (Ndtimes, Beijing, China) was
used in the statistical analysis. A comparison of multiple sets of
quantitative samples was made using variance analysis. SNK-q test
was used for comparison between groups. Correlation analysis was
performed using Pearson's product-moment correlation coefficient.
The difference was statistically significant when P<0.05.
Results
Comparison of flap survival rates
The flap survival rates in each group were obtained
by image analysis (Fig. 1). The
differences were statistically significant, as indicated by
variance analysis (F = 8.214, P<0.05). The flap survival rates
in the control group [(93.56+3.15)%] and the inhibitor group
[(81.83+2.44)%] were much higher than those in the saline group
[(49.61+2.55)%] and the ischemia-reperfusion group [(41.47+3.28)%]
(P<0.05). There was also a significant difference between the
control group and the inhibitor group (P<0.05).
Serum IL-6 concentration
The serum concentrations of IL-6 in the
ischemia-reperfusion group (91.18±3.52 ng/l) and the saline group
(82.82±3.25 ng/l) were nearly double the concentration in the
control group (47.45±2.85 ng/l) (P<0.05). The serum IL-6
concentration in the inhibitor group (59.66±2.27 ng/l) was much
lower than those in the ischemia-reperfusion group and the normal
saline group (P<0.05), but higher than that in the control group
(P<0.05). The detailed data were listed in Table II.
 | Table II.Serum IL-6 concentrations in the four
groups (mean ± SD). |
Table II.
Serum IL-6 concentrations in the four
groups (mean ± SD).
|
| Groups |
|---|
|
|
|
|---|
| Variables | Control |
Ischemia-reperfusion | Saline | Inhibitor |
|---|
| n | 12 | 12 | 12 | 12 |
| IL-6 concentration
(ng/l) | 47.45±2.85 |
91.18±3.52a |
82.82±3.25a |
59.66±2.27a,b |
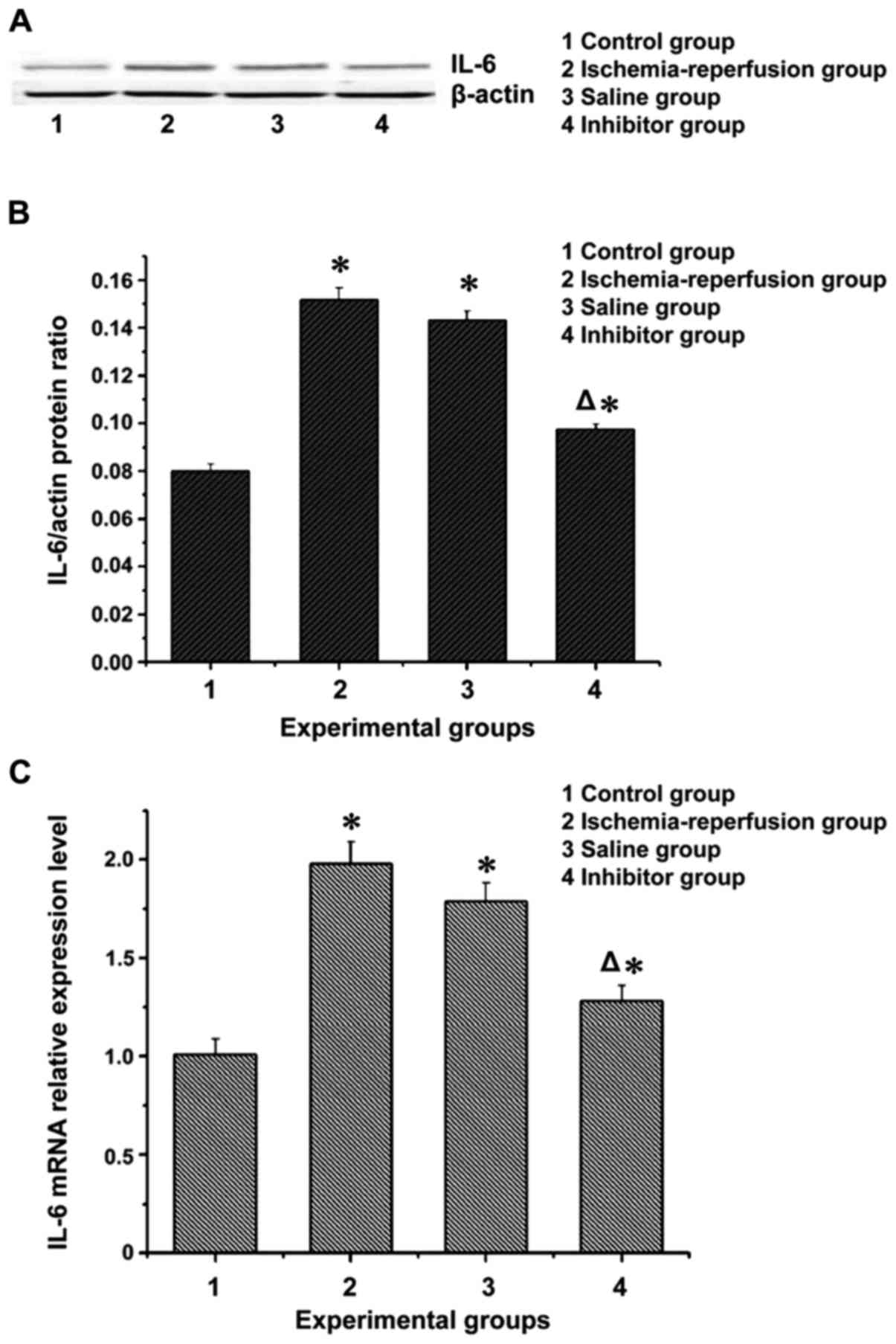
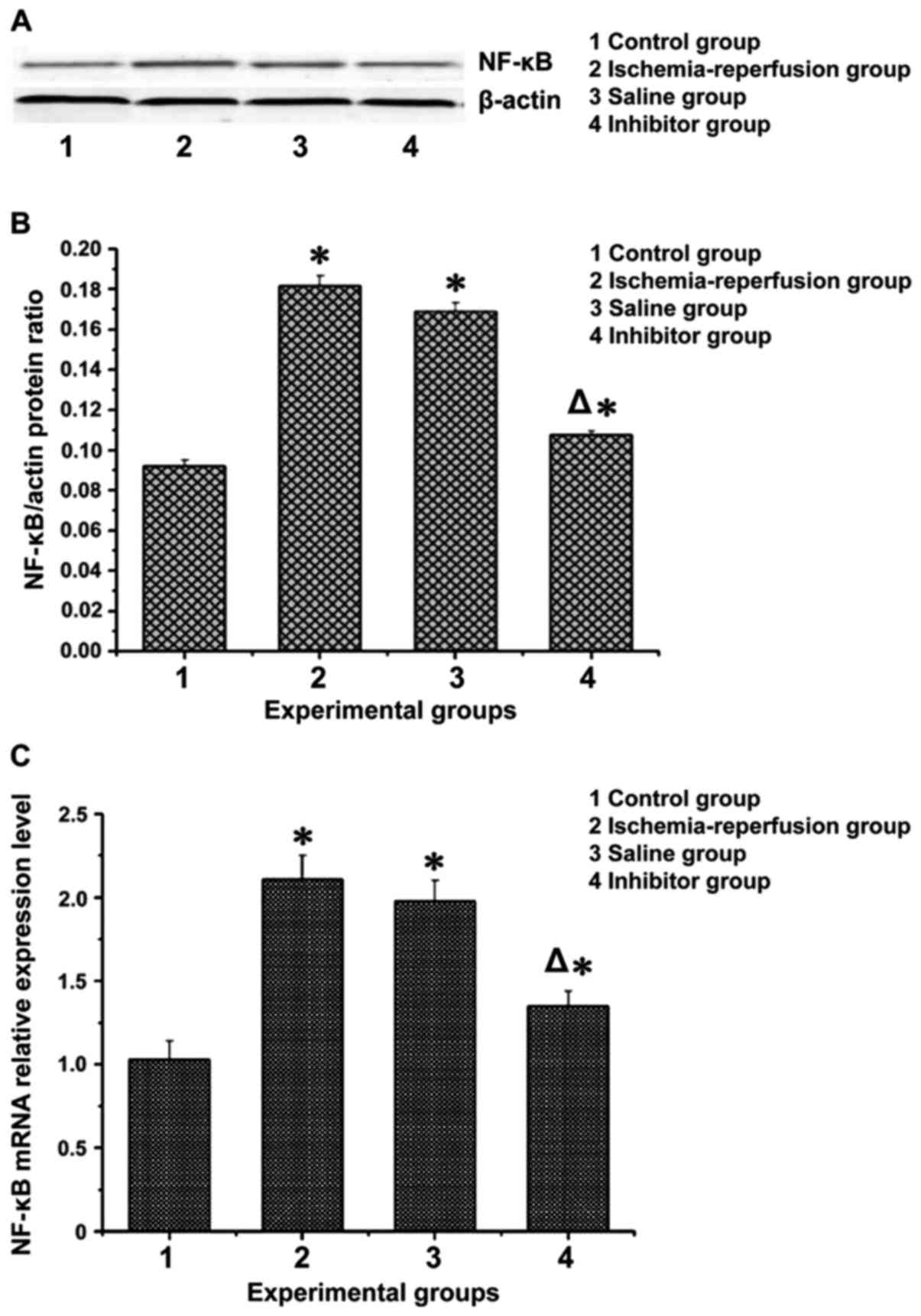
mRNA and protein expression levels of
NF-κB and IL-6 in flap tissues
The expression levels of inflammatory factor IL-6
and nuclear transcription factor NF-κB in the flap of each group
were processed and are shown in Figs.
2 and 3. Apparently, the mRNA
and protein expression levels of IL-6 and NF-κB in the
ischemia-reperfusion group and the saline group were significantly
higher than those in the control group (P<0.05). These levels in
the inhibitor group were lower than those in the
ischemia-reperfusion group and the saline group (P<0.05), but
higher than those in the control group (P<0.05).
Discussion
Flap ischemia-reperfusion injury is the leading
cause of necrosis after flap transplantation. It was found that
cell inflammatory factors played an important role in
ischemia-reperfusion injury, which can lead to tissue morphological
damage and dysfunction (10,11). Therefore, anti-inflammatory response
is a major research focus aiming to alleviate ischemia-reperfusion
injury and improve flap survival rate (12). Studies have shown that the MAPK
pathways that promote occurrence and progression of inflammation
were activated in ischemia-reperfusion injuries of a variety of
tissues and organs (13). The p38
MAPK pathway, an important member in the MAPK family, played a
major role in regulation of intracellular inflammatory response
(14,15). In order to understand the role of p38
MAPK signaling pathway in flap ischemia-reperfusion injury and the
underlying mechanism, a successfully constructed flap
ischemia-reperfusion injury animal model was treated with SB202190,
a specific inhibitor of the p38 MAPK pathway. Relevant indicators
were measured in the flap, which were used to demonstrate if
inhibition of the p38 MAPK pathway had a protective effect in flap
ischemia and reperfusion injury.
IL-6 is one of the most common immune cytokines. It
is also an important inflammatory mediator of ischemia-reperfusion
injury, which can lead to inflammatory injury of tissues and
organs. The concentration of IL-6 in serum is an important clinical
reference to diagnose inflammatory injury and determine its
severity (16–18). Nuclear transcription factor NF-κB is
a transcriptional regulator of a variety of cytokine genes. It is
also an important transcriptional regulator of the intracellular
inflammatory gene, and plays an important role in the inflammatory
response (19). Activation of the
p38 MAPK pathway leads to elevated expression of NF-κB, which binds
to DNA on specific binding sites after entering into the nucleus
and upregulate the expression of some inflammatory factors, such as
IL-6 and TNF-α (7,20). In this study it was found that in the
ischemia-reperfusion model the flap survival rate was lower, but
the concentration of IL-6 in serum and the mRNA and protein
expression levels of NF-κB and IL-6 in the flap tissue were all
higher than the corresponding indicators in the control group. This
result was similar to previous reports (17,20).
Inflammation leads to an increase in serum IL-6 concentration and
an increase in expression levels of NF-κB and IL-6 in tissues of
ischemia-reperfusion injury. The flap survival rate in the
inhibitor group which was treated with SB202190 was significantly
higher than that in the ischemia-reperfusion and saline groups. The
concentration of IL-6 in serum and the mRNA and protein
concentrations of NF-κB and IL-6 in the flap tissues were
significantly decreased. This is similar to previous experimental
results (6,14). When the p38 MAPK signaling pathway
was inhibited, the expression levels of inflammatory factors
decreased, alleviating the inflammatory response in the flap. This
finding suggests that SB202190 has a protective effect on flap
ischemia-reperfusion injury, which may be achieved by reducing the
inflammatory response during the process.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KG and JM designed the study. WL established the
animal models. KG and JM performed western blotting. KG prepared
the manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Animal Ethics
Committee of Jinan Municipal Hospital of Traditional Chinese
Medicine (Jinan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cheng HF, Feng Y, Jiang DM, Tao KY and
Kong MJ: Protective function of tocilizumab in human cardiac
myocytes ischemia reperfusion injury. Asian Pac J Trop Med.
8:48–52. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khalil AA, Aziz FA and Hall JC:
Reperfusion injury. Plast Reconstr Surg. 117:1024–1033. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Uchida Y, Freitas MC, Zhao D, Busuttil RW
and Kupiec-Weglinski JW: The protective function of neutrophil
elastase inhibitor in liver ischemia/reperfusion injury.
Transplantation. 89:1050–1056. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kanemoto S, Matsubara M, Noma M, Leshnower
BG, Parish LM, Jackson BM, Hinmon R, Hamamoto H, Gorman JH III and
Gorman RC: Mild hypothermia to limit myocardial
ischemia-reperfusion injury: Importance of timing. Ann Thorac Surg.
87:157–163. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu YQ, Liu YF, Ma XM, Xiao YD, Wang YB,
Zhang MZ, Cheng AX, Wang TT, Li JL, Zhao PX, et al: Hydrogen-rich
saline attenuates skin ischemia/reperfusion induced apoptosis via
regulating Bax/Bcl-2 ratio and ASK-1/JNK pathway. J Plast Reconstr
Aesthet Surg. 68:e147–e156. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ashraf MI, Ebner M, Wallner C, Haller M,
Khalid S, Schwelberger H, Koziel K, Enthammer M, Hermann M,
Sickinger S, et al: A p38MAPK/MK2 signaling pathway leading to
redox stress, cell death and ischemia/reperfusion injury. Cell
Commun Signal. 12:62014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Uemura T, Tsujii M, Akeda K, Iino T,
Satonaka H, Hasegawa M and Sudo A: Transfection of nuclear
factor-kappaB decoy oligodeoxynucleotide protects against
ischemia/reperfusion injury in a rat epigastric flap model. J Gene
Med. 14:623–631. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Grossi V, Liuzzi M, Murzilli S, Martelli
N, Napoli A, Ingravallo G, Del Rio A and Simone C: Sorafenib
inhibits p38α activity in colorectal cancer cells and synergizes
with the DFG-in inhibitor SB202190 to increase apoptotic response.
Cancer Biol Ther. 13:1471–1481. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Manson PN, Anthenelli RM, Im MJ, Bulkley
GB and Hoopes JE: The role of oxygen-free radicals in ischemic
tissue injury in island skin flaps. Ann Surg. 198:87–90. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Al-Juboori MJ: Flap designs for
implant-related surgical procedures: A review. Implant Dent.
25:845–854. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Silva JJ, Pompeu DG, Ximenes NC, Duarte
AS, Gramosa NV, Carvalho KM, Brito GA and Guimarães SB: Effects of
kaurenoic acid and arginine on random skin flap oxidative stress,
inflammation, and cytokines in rats. Aesthetic Plast Surg.
39:971–977. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Joshi YB and Praticò D: The 5-lipoxygenase
pathway: Oxidative and inflammatory contributions to the
Alzheimer's disease phenotype. Front Cell Neurosci. 8:4362015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Patten RD, Pourati I, Aronovitz MJ, Baur
J, Celestin F, Chen X, Michael A, Haq S, Nuedling S, Grohe C, et
al: 17beta-estradiol reduces cardiomyocyte apoptosis in vivo and in
vitro via activation of phospho-inositide-3 kinase/Akt signaling.
Circ Res. 95:692–699. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ju J, Wu J and Hou R: Role of the p38
mitogen-activated protein kinase signaling pathway in
estrogen-mediated protection following flap ischemia-reperfusion
injury. Cell Biochem Funct. 34:522–530. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Han HH, Lim YM, Park SW, Lee SJ, Rhie JW
and Lee JH: Improved skin flap survival in venous
ischemia-reperfusion injury with the use of adipose-derived stem
cells. Microsurgery. 35:645–652. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Denes A, Thornton P, Rothwell NJ and Allan
SM: Inflammation and brain injury: Acute cerebral ischaemia,
peripheral and central inflammation. Brain Behav Immun. 24:708–723.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Suzuki S, Tanaka K and Suzuki N:
Ambivalent aspects of interleukin-6 in cerebral ischemia:
Inflammatory versus neurotrophic aspects. J Cereb Blood Flow Metab.
29:464–479. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Clark WM, Rinker LG, Lessov NS, Hazel K,
Hill JK, Stenzel-Poore M, Eckenstein F and Haley EC: Lack of
interleukin-6 expression is not protective against focal central
nervous system ischemia. Stroke. 31:1715–1720. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu SF and Malik AB: NF-kappa B activation
as a pathological mechanism of septic shock and inflammation. Am J
Physiol Lung Cell Mol Physiol. 290:L622–L645. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang J, Min P, Grassetti L, Lazzeri D,
Zhang YX, Nicoli F, Innocenti M, Torresetti M, Levin LS and
Persichetti P: Preliminary outcomes of distal IMAP and SEAP flaps
for the treatment of unstable keloids subject to recurrent
inflammation and infections in the lower sternal and upper
abdominal areas. J Reconstr Microsurg. 31:621–630. 2015. View Article : Google Scholar : PubMed/NCBI
|