Introduction
In recent years, acute ischemic cerebral injury has
become a kind of disease with an extremely high incidence rate and
poor prognosis, and for some severe conditions, it can even be
life-threatening (1). Generally, it
is originated from the cerebral thrombosis and embolism, and, after
onset of ischemia, timely recovery of blood supply is critical to
the reduction of apoptosis in neurons and repair of neurological
functions. Ischemic angiogenesis is closely related to the
progression and outcome of cerebrovascular diseases. However,
current treatment method for acute ischemic cerebral injury
requires further research and development (2–4).
Granulocyte colony-stimulating factor (G-CSF), as a
member of hematopoietic growth factor family, can promote the
proliferation, differentiation and survival of hematopoietic stem
cells with the obvious protective effect on neurons in peripheral
and central nerve system (5). In the
present study, we aimed to establish the models of acute ischemic
cerebral injury in rats to investigate the changes in early growth
response-1 (Egr-1) and vascular endothelial growth factor (VEGF) in
cerebral tissues after intervention with G-CSF, thereby exploring
the potential mechanism of G-CSF in protecting nerves, and
providing new pathways for clinical treatment of acute ischemic
cerebral injury.
Materials and methods
Materials
Experiment animals and grouping
After Sprague-Dawley (SD) rats (180–220 g) were
acclimatized to the environment, they were randomly divided into
the sham group (n=10), the model group (n=10) and the G-CSF group
(100 µg/kg, n=10). G-CSF was given through neck subcutaneous
injection once per day for 7 consecutive days. Subsequently, access
of food to rats was forbidden for 12 h but they had free access to
water. The rats were kept in cage with controlled temperature and
light cycles (24°C and 12/12 light cycles). Longas method was
applied to establish the middle cerebral artery occlusion models in
rats. The humidity was 60±10%. The study was approved by the Ethics
Committee of Zhongshan Torch Development Zone Hospital (Zhongshan,
China).
Major reagents
TRIzol extraction kit for total RNA (Tiangen, Co.,
Ltd., Beijing, China); real-time polymerase chain reaction (RT-PCR)
kit for reverse transcription (Tiangen); bicinchoninic acid (BCA)
kit for protein quantification (Beyotime Institute of
Biotechnology, Shanghai, China); extraction kit for total protein
(Nanjing KeyGen Biotech, Co., Ltd., Nanjing, China);
immunopreticipation (IP) lysis kit (Beyotime Institute of
Biotechnology); lactate dehydrogenase (LDH) kit (Nanjing Jiancheng
Biotech Co., Ltd., Nanjing, China); primary
anti-glyceraldehyde-phosphate dehydrogenase (GAPDH), Egr-1
monoclonal antibodies and the relevant secondary antibodies (Cell
Signaling Technology, Boston, MA, USA) and VEGF monoclonal antibody
(ProteinTech Group, Inc., Wuhan, China) were used in the present
study.
Experiment methods
Measurement of the volume of cerebral
infarction and relevant indicators
After rats in each group were anesthetized, they
were immediately sacrificed and brain tissue was removed. Samples
were then stained for 30 min at 37°C in the dark in 1%
triphenyltetrazolium chloride (TTC), and then fixed in 10%
formaldehyde. The infarction area in each layer was then
calculated, and LDH content in brain tissues in the three groups
was assayed in accordance with the LDH kit.
Histopathological examination
Brain tissues in each group were embedded in
paraffin to prepare the paraffin samples which were later sliced
into sections of 5 µm. After hematoxylin and eosin (H&E)
staining, the sections were placed under a microscope (×100) (Roche
Diagnostics, Basel, Switzerland) for histopathological
observation.
Immunofluorescence analysis
Paraffin sections of brain tissues were collected
from each group, and, after dewaxing with xylene and dehydration
using alcohol of gradient concentration, the antigen retrieval was
carried out. Sections were then rinsed with 0.01 M
phosphate-buffered saline (PBS, pH 7.4) 3 times (5 min/time), and
blocked in a wet box containing 10% bull serum albumin (BSA) for 30
min. Subsequently, on sections, fluorescence-labeled antibodies
that were diluted appropriately (1:70) were placed in the wet box
and the sections were then incubated at 4°C overnight. After
sections were rinsed with PBS (pH 7.4) 3 times, fluorescent
secondary antibodies (1:100) were added onto the sections in the
dark, and placed in the wet box for incubation for 2 h at 37°C. The
sections were then observed and photographed under the fluorescent
microscopes (Olympus Corporation, Tokyo, Japan).
RT-PCR analysis
Brain tissues that were collected from each group
were rapidly transferred to the Eppendorf (EP) tubes containing
RNAiso Plus extraction solution and placed at room temperature for
5 min for sufficient lysis. After centrifugation at 12,000 × g and
4°C for 5 min, the supernatant was well mixed with 0.2 ml
chloroform and placed at room temperature for 5 min. The solution
was centrifuged again at 12,000 × g and 4°C for 15 min, and,
isopropanol of the same volume was added and well mixed to the
supernatant. After being placed at room temperature for 10 min, it
was centrifuged at 12,000 × g and 4°C for 10 min, and sediment was
preserved while the supernatant was discarded. In the sediment, 1
ml 75% alcohol was added and mixed well followed by centrifugation
at 12,000 × g and 4°C for 5 min, which was repeated once after the
supernatant was then removed. After RNA sediment was fully removed
through rinsing, the liquid was replaced with RNase-free water.
Some of the total RNA solution was extracted and diluted with
RNase-free water to a concentration of 1 µg/µl. In accordance with
the requirement of the PrimeScript® RT reagent kit with
gDNA Eraser, reaction solution for reverse transcription was
prepared, and cDNA was obtained through reverse transcription with
the RNA samples and preserved at −20°C. Thereafter, according to
the instruction of SYBR® Premix Ex Taq™ II (Tli RNaseH
Plus), we detected the level of mRNA expression. The relevant RNA
primer sequences used in this procedure are shown in Table I.
 | Table I.Primer sequences of relevant genes in
RT-PCR analysis. |
Table I.
Primer sequences of relevant genes in
RT-PCR analysis.
| Gene name | Primer sequence |
|---|
| Egr-1 | 5′-3′
TCGGCTCCTTTCCTCACTCA |
|
| 3′-5′
CTCATAGGGTTGTTCGCTCGG |
| VEGF | 5′-3′
ATGGCAGAAGGAGGAGGG |
|
| 3′-5′
CGAAACGCTGAGGGAGGCT |
| β-actin | 5′-3′
GAGCCGGGAAATCGTGCGT |
|
| 3′-5′
GGAAGGAAGGCTGGAAGATG |
Western blotting assay
Brain tissues collected from all the groups were
rinsed with icy normal saline followed by measurement of protein
concentration with BCA kit and preservation at −80°C for later use.
According to the instructions of total protein extraction kit, the
IP lysis buffer supplemented with phenylmethanesulfonyl fluoride
(PMSF) and protease inhibitor was added in the tissues which were
later ground on ice. Tissue samples were then centrifuged at 4°C
and 12,000 × g for 10 min of homogenization, and the supernatant
was taken for centrifugation at 4°C and 12,000 × g for 20 min. With
the supernatant, protein samples containing the same content of
total protein, after protein quantification according to the
relevant kit instruction, were loaded in the sampling holes for
electrophoresis under a constant voltage of 220 V. Electrophoresis
was stopped until the bromophenol blue reached the bottom of gel.
Based on the molecular weight of targeting proteins, gel was
trimmed and placed in the transfer buffer. Polyvinylidene fluoride
(PVDF) membrane was also trimmed in accordance with the size of the
gel, and then soaked in methanol for 10 sec. The PVDF membrane and
filter paper were placed in the transfer buffer, and later, those
materials were all placed in the transfer machine in the following
sequence: positive electrode, filter paper, PVDF membrane, gel,
filter paper and negative electrode. Membrane transfer was then
carried out under a constant voltage of 110 V for appropriate time
until the protein on the gel was transferred on the PVDF membrane.
Thereafter, PVDF membrane with protein was blocked in 5% skimmed
milk on a shaker for 3 h, and the rabbit anti-rat Egr-1, and GAPDH
monoclonal antibodies (1:1,000; cat. nos. 4154 and 2118), rabbit
anti-rat VEGF monoclonal antibody (1:1,000; cat. no. 19003-1-AP)
was added on the membrane for incubation at 4°C overnight. The next
day, membrane was sufficiently washed by Tween-20 + Tris-buffer
saline (TTBS) 3 times (10 min/time), and then incubated with goat
anti-rabbit secondary polyclonal antibody (1:2,000; cat. no. 7074)
for 1 h at room temperature. Enhanced chemiluminescence (ECL)
reagent was added for color development and photographing after the
membrane was washed with TTBS 3 times (10 min/time).
Statistical analysis
Statistical Product and Service Solutions (SPSS)
17.0 software (SPSS, Inc., Chicago, IL, USA) was applied in
statistical analysis, and experiment data were presented as mean ±
standard deviation (SD). Data analysis was carried out through
analysis of variance and the post hoc test was LSD test for
multiple comparisons or t-test for intergroup comparisons.
P<0.05 suggested that the difference had statistical
significance.
Results
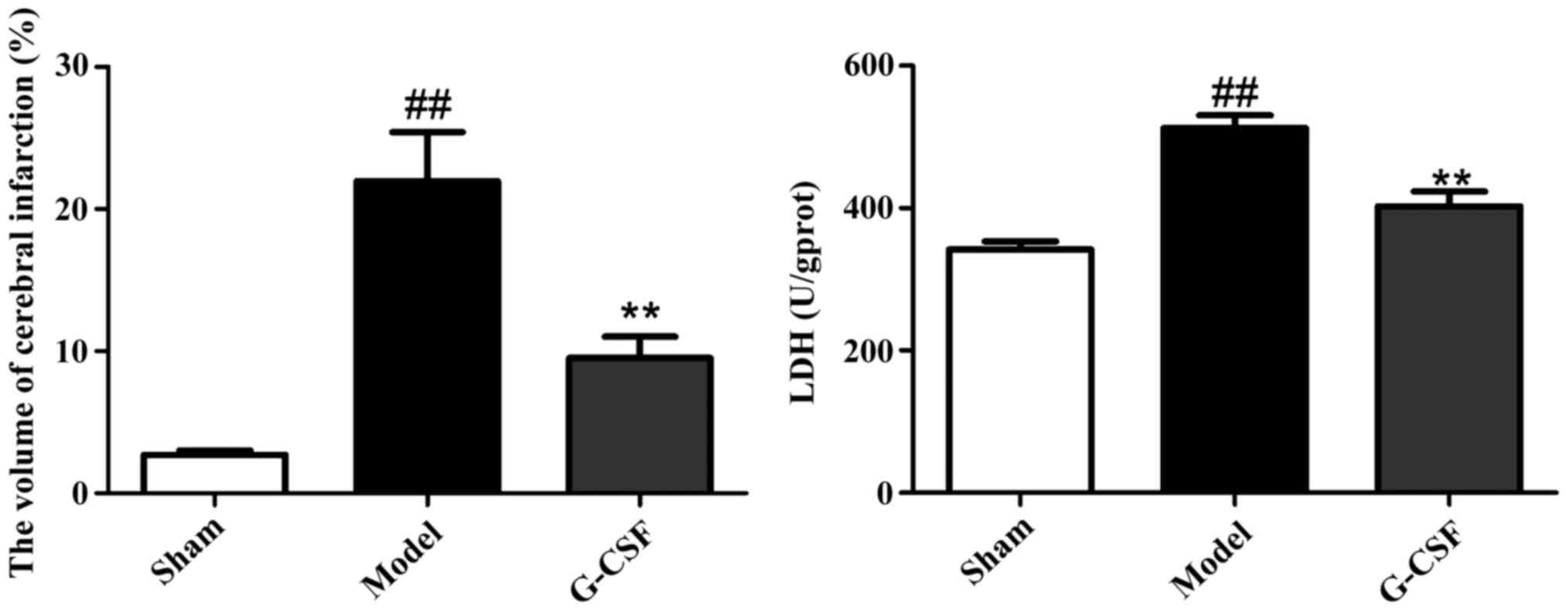
Effect of G-CSF on the volume of
cerebral infarction and LDH content in brain tissues in rats
As shown in Fig. 1 in
comparison with the sham group, the volume of cerebral infarction
in rats of the model group was significantly enlarged. By contrast,
compared with the model group, a significant decrease was
identified in the volume of cerebral infarction in rats of the
G-CSF group. In addition, G-CSF could reduce the level of LDH in
brain tissues significantly.
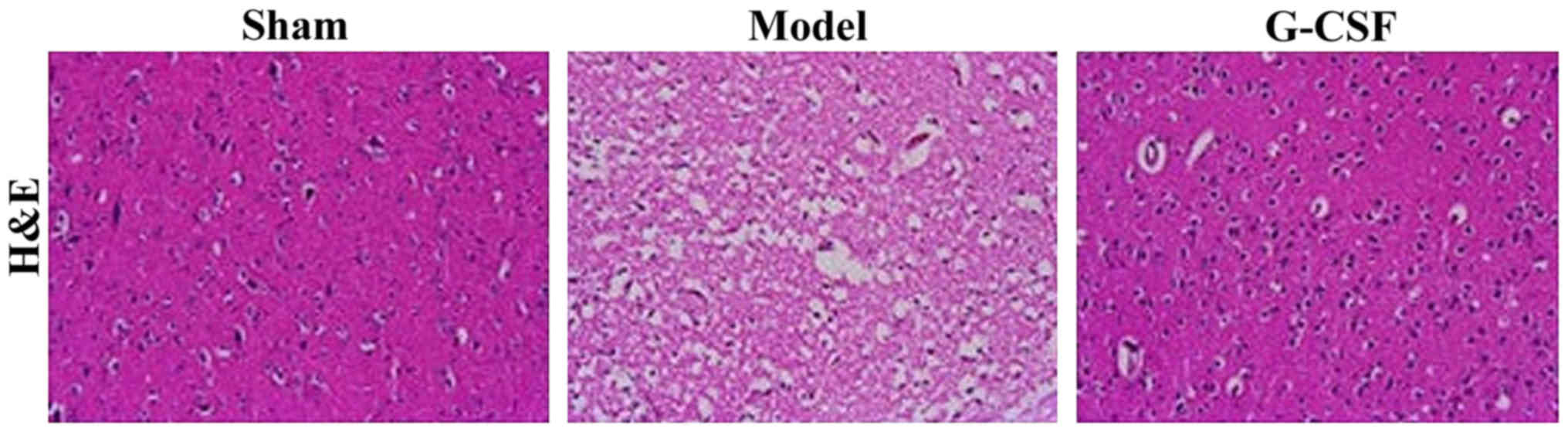
Effect of G-CSF on the
histopathological examination of rats with acute ischemic cerebral
injury
The H&E staining results of histopathological
examination of brain tissues are shown in Fig. 2. In the sham group, the brain
structure of rats appeared to be integral, while rats in the model
group manifested massive necrotic cells, and destructed molecular
structures. Compared with the model group, we found that the
necrotic area was reduced in the G-CSF group, suggesting the
cerebral injury was ameliorated.
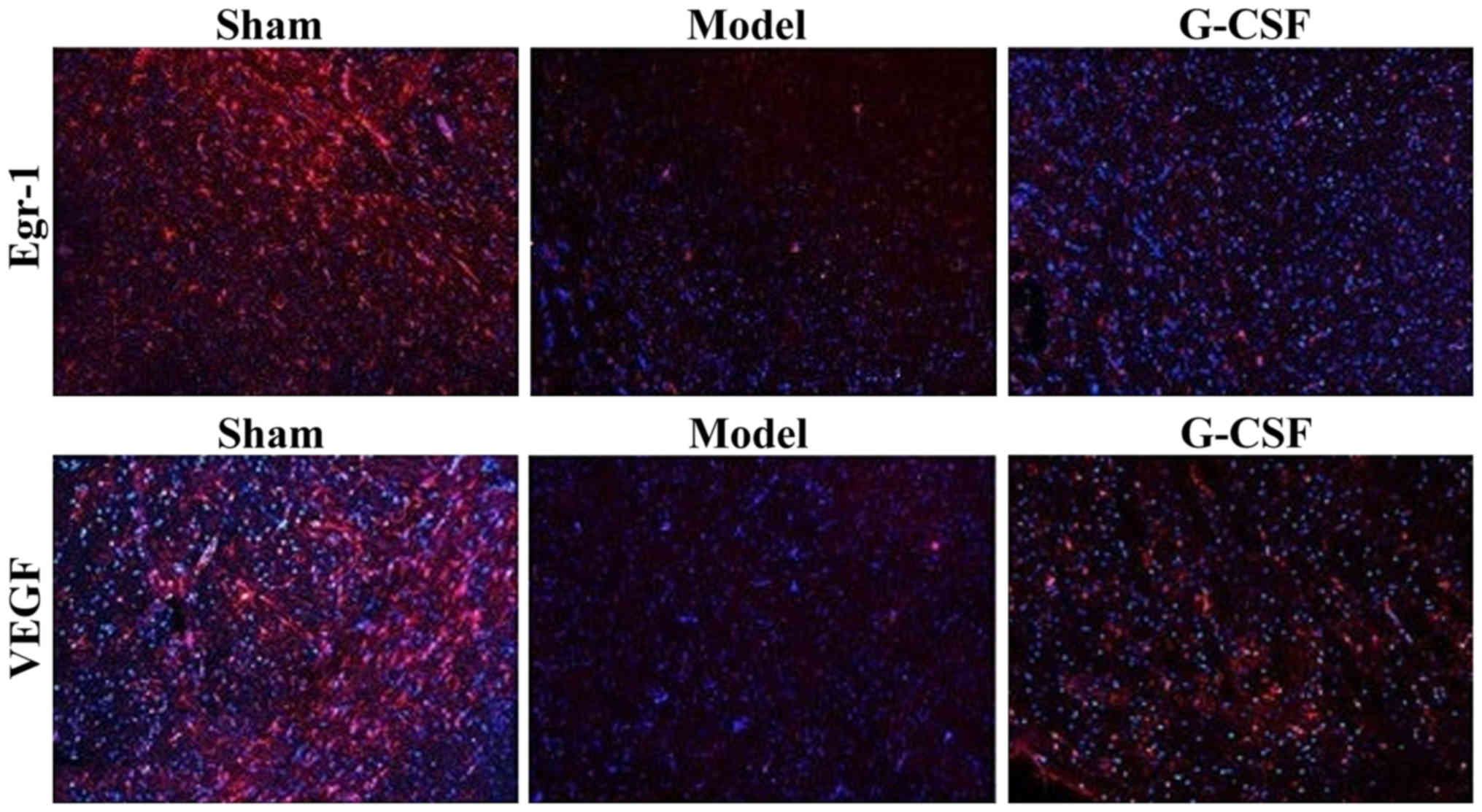
Immunofluorescent staining results of
Egr-1 and VEGF
The immunofluorescence analysis revealed that
compared with the sham group, the protein expressions of Egr-1 and
VEGF in brain tissues of rats in the model group were reduced
significantly, while those in the G-CSF group were increased
evidently (P<0.01) (Fig. 3).
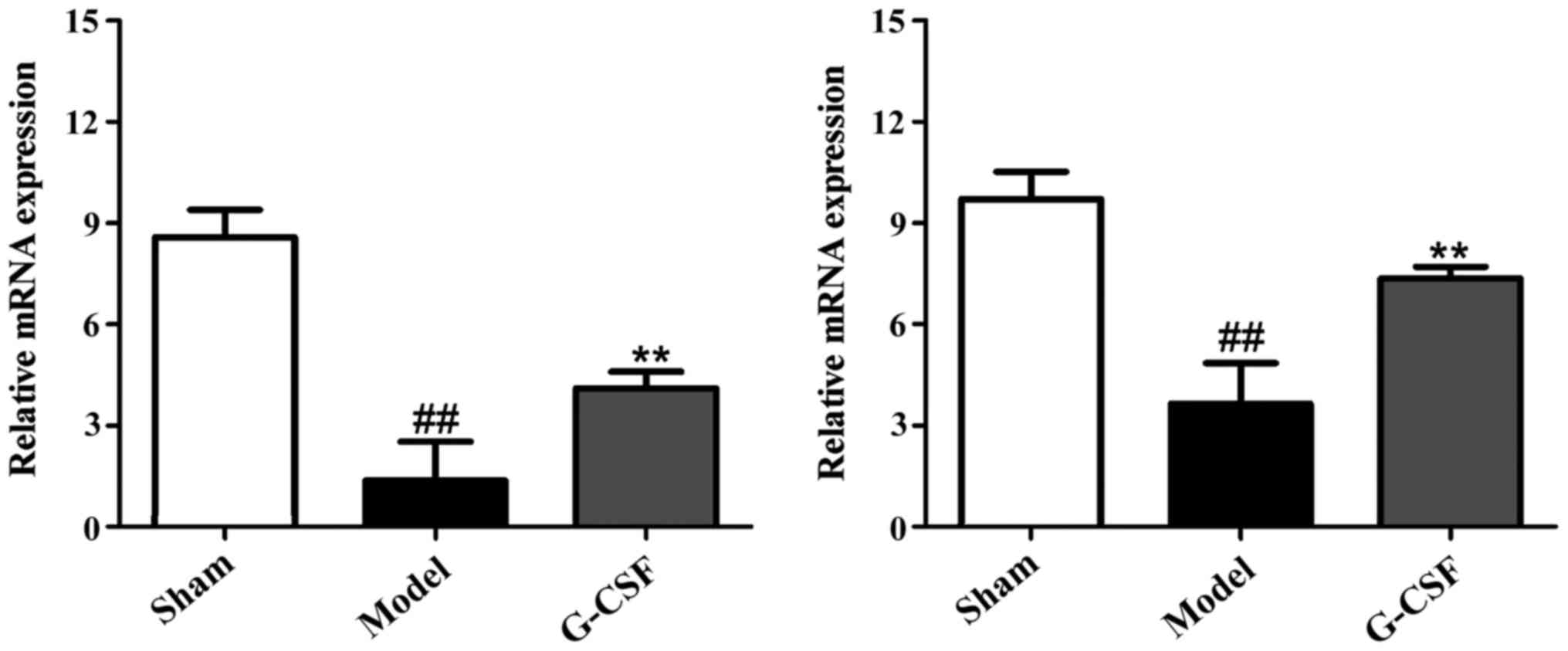
RT-PCR results of the effect of G-CSF
on mRNA expression of Egr-1 and VEGF in MCAO rats
As shown in Fig. 4,
the RT-PCR results revealed that compared with the sham group, the
mRNA expressions of Egr-1 and VEGF in brain tissues of rats in the
model group were reduced significantly. By contrast, in comparison
with the model group, the mRNA expression of Egr-1 and VEGF was
increased significantly in brain tissues of rats in the G-CSF
group.
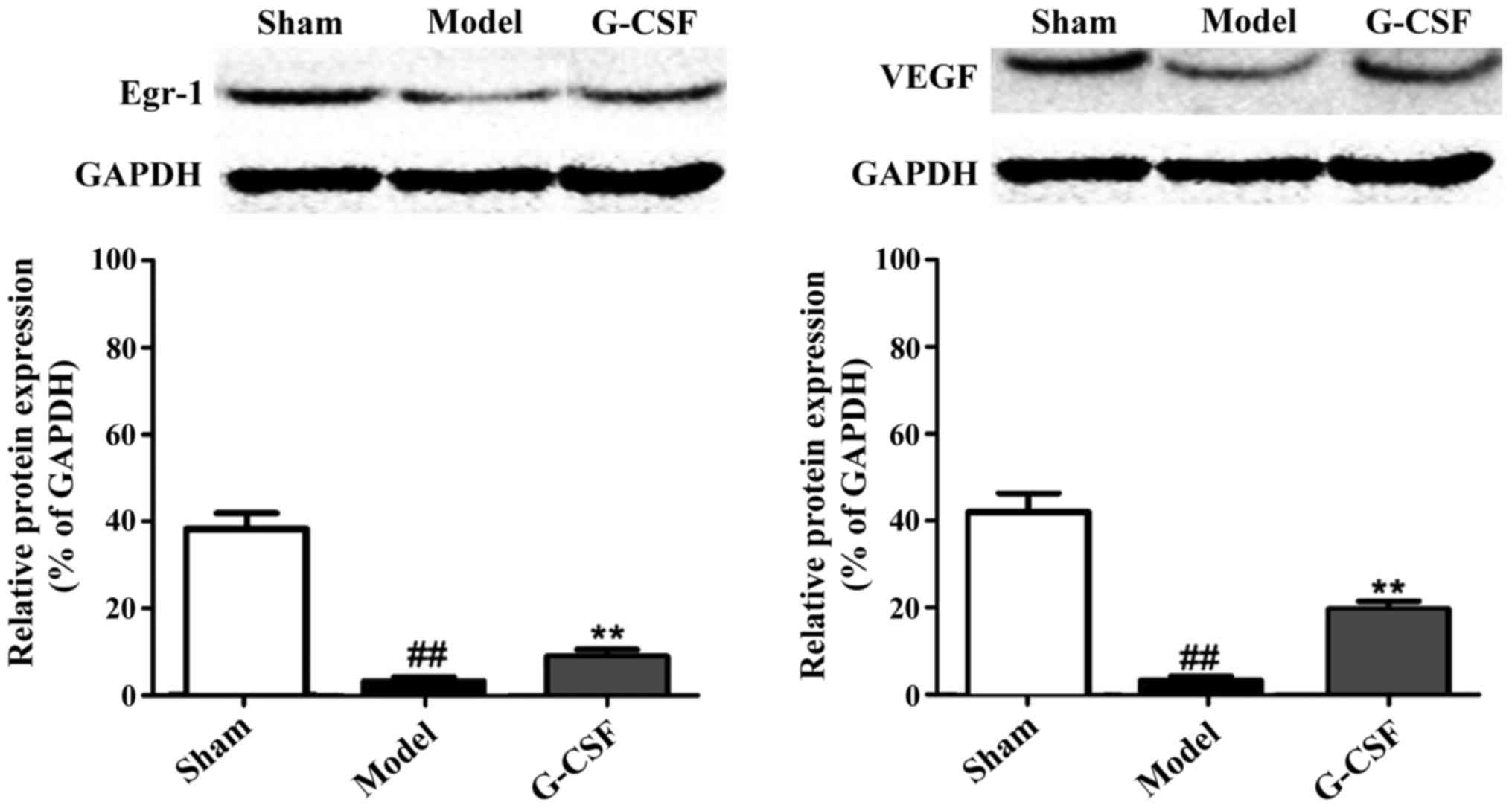
Western blot analysis results of the
effect of G-CSF on the protein expression of Egr-1 and VEGF in MCAO
rats
In Fig. 5, the
western blot analysis revealed that in comparison with the sham
group, protein expression of Egr-1 and VEGF in the brain tissues of
rats in the model group was significantly reduced. Compared with
the model group, the protein expression of Egr-1 and VEGF in brain
tissues of rats in the G-CSF group was significantly elevated. This
result confirmed that G-CSF can ameliorate the acute ischemic
cerebral injury by regulating the expressions of Egr-1 and
VEGF.
Discussion
Acute ischemic cerebral injury has gradually become
a global killer with characteristics including high incidence rate,
high mortality rate and high morbidity rate (6,7).
Cerebral ischemia can damage the brain cells, and once the blood
perfusion is recovered, ischemic injury is further aggravated,
known as cerebral ischemia-reperfusion injury (8–10).
Pathogenesis leading to acute ischemic cerebral injury remains
elusive, which makes the search for effective, reliable and
feasible treatment methods for this disease more urgent. In recent
years, G-CSF has gained more and more attention of researchers for
its special effect (11).
G-CSF, as a kind of cytokine in hematopoietic stem
cells, can promote the survival, proliferation and maturity of
neutrophilic cell lines. G-CSF exists mostly in the bone marrow
stem cell of patients (12–14). Previous findings have shown that
G-CSF has a promising protective effect on nerves, and it can
promote angiogenesis and exert an anti-inflammatory effect by
regulating varying molecular mechanisms, such as mobilizing the
generation of hematopoietic stem cells, inhibiting their apoptosis,
facilitating the differentiation of neurons and antagonizing the
inflammatory responses (15–18). Previous findings have shown that
Egr-1 and VEGF have key roles in the regulation of growth and
development of vessels, and are also critical to ischemic diseases.
Additionally, they can facilitate the migration of hematopoietic
stem cells with protective effects on nerves (19,20).
In this study, male SD rats used as subjects, were
divided the sham, model and G-CSF groups to measure the effect of
G-CSF on the volume of cerebral infarction and level of LDH in
rats. The H&E staining method was performed for
histopathological examination. Through RT-PCR and western blot
analysis, we detected the mRNA and protein expressions of Egr-1 and
VEGF in different groups. Furthermore, SPSS 17.0 software was
applied to detect the differences in expression of Egr-1 and VEGF
between the two groups. Results showed that compared with the sham
group, the volume of cerebral infarction and LDH content in the
model group were significantly elevated, whereas in the model
group, those indicators in the G-CSF group were obviously
decreased. H&E staining results also showed that G-CSF could
decrease the necrotic area in cerebral infarction and the incidence
of inflammation, and sustain the integrity of molecular structure.
Immunofluorescence staining results revealed that the protein
expression of Egr-1 and VEGF in the model group were all
significantly decreased, while those in the G-CSF group were
significantly elevated. RT-PCR and western blot analysis revealed
that the mRNA and protein expression of Egr-1 and VEGF in the model
group was decreased obviously, but those in the G-CSF group were
elevated significantly.
Taken together, G-CSF manifests a significant
protective effect on acute ischemic cerebral injury, which is
generated through its impact on the expression of Egr-1 and VEGF.
The results of this study are expected to provide new therapeutic
procedures for treatment of acute ischemic cerebral injury, and
other effects of G-CSF on acute ischemic cerebral injury require
more in-depth studies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DGZ measured the volume of cerebral infarction and
relevant indicators. YHS helped with histopathological examination.
DGZ and YQC were reponsible for immunofluorescence, analysis and
PCR. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhongshan Torch Development Zone Hospital (Zhongshan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Du H, Naqvi H and Taylor HS:
Ischemia/reperfusion injury promotes and granulocyte-colony
stimulating factor inhibits migration of bone marrow-derived stem
cells to endometrium. Stem Cells Dev. 21:3324–3331. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fan L, Chen L, Chen X and Fu F: A
meta-analysis of stem cell mobilization by granulocyte
colony-stimulating factor in the treatment of acute myocardial
infarction. Cardiovasc Drugs Ther. 22:45–54. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dai W, Hale SL, Martin BJ, Kuang JQ, Dow
JS, Wold LE and Kloner RA: Allogeneic mesenchymal stem cell
transplantation in postinfarcted rat myocardium: Short- and
long-term effects. Circulation. 112:214–223. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fuchs S, Baffour R, Zhou YF, Shou M,
Pierre A, Tio FO, Weissman NJ, Leon MB, Epstein SE and Kornowski R:
Transendocardial delivery of autologous bone marrow enhances
collateral perfusion and regional function in pigs with chronic
experimental myocardial ischemia. J Am Coll Cardiol. 37:1726–1732.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schneider A, Krüger C, Steigleder T, Weber
D, Pitzer C, Laage R, Aronowski J, Maurer MH, Gassler N, Mier W, et
al: The hematopoietic factor G-CSF is a neuronal ligand that
counteracts programmed cell death and drives neurogenesis. J Clin
Invest. 115:2083–2098. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schäbitz WR, Kollmar R, Schwaninger M,
Juettler E, Bardutzky J, Schölzke MN, Sommer C and Schwab S:
Neuroprotective effect of granulocyte colony-stimulating factor
after focal cerebral ischemia. Stroke. 34:745–751. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kawamoto A, Gwon HC, Iwaguro H, Yamaguchi
JI, Uchida S, Masuda H, Silver M, Ma H, Kearney M, Isner JM, et al:
Therapeutic potential of ex vivo expanded endothelial progenitor
cells for myocardial ischemia. Circulation. 103:634–637. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Murry CE, Soonpaa MH, Reinecke H, Nakajima
H, Nakajima HO, Rubart M, Pasumarthi KBS, Virag JI, Bartelmez SH,
Poppa V, et al: Haematopoietic stem cells do not transdifferentiate
into cardiac myocytes in myocardial infarcts. Nature. 428:664–668.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Olivetti G, Capasso JM, Meggs LG,
Sonnenblick EH and Anversa P: Cellular basis of chronic ventricular
remodeling after myocardial infarction in rats. Circ Res.
68:856–869. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Park KI, Hack MA, Ourednik J, Yandava B,
Flax JD, Stieg PE, Gullans S, Jensen FE, Sidman RL, Ourednik V, et
al: Acute injury directs the migration, proliferation, and
differentiation of solid organ stem cells: Evidence from the effect
of hypoxia-ischemia in the CNS on clonal ‘reporter’ neural stem
cells. Exp Neurol. 199:156–178. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pastuszko P1, Liu H, Mendoza-Paredes A,
Schultz SE, Markowitz SD, Greeley WJ, Wilson DF and Pastuszko A:
Regulatory pathways to neuronal injury or survival are dependent on
the rate of low flow cardiopulmonary bypass following circulatory
arrest in newborn piglets. Eur J Cardiothorac Surg. 31:899–905.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rosenstrauch D, Poglajen G, Zidar N and
Gregoric ID: Stem celltherapy for ischemic heart failure. Tex Heart
Inst J. 32:339–347. 2005.PubMed/NCBI
|
|
13
|
Tang YL, Zhao Q, Qin X, Shen L, Cheng L,
Ge J and Phillips MI: Paracrine action enhances the effects of
autologous mesenchymal stem cell transplantation on vascular
regeneration in rat model of myocardial infarction. Ann Thorac
Surg. 80:229–236, discussion 236–237. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiao BG, Lu CZ and Link H: Cell biology
and clinical promise of G-CSF: Immunomodulation and
neuroprotection. J Cell Mol Med. 11:1272–1290. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pastuszko P, Schears GJ, Pirzadeh A,
Greeley WJ, Wilson DF and Pastuszko A: Effect of granulocyte colony
stimulating factor (G-CSF) on expression of select proteins
involved in apoptosis in a neonatal piglet brain following
cardiopulmonary bypass (CPB) and deep hypothermic circulatory
arrest (DHCA). J Thorac Cardiovasc Surg. 143:1436–1442. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gibson CL, Bath PM and Murphy SP: G-CSF
reduces infarct volume and improves functional outcome after
transient focal cerebral ischemia in mice. J Cereb Blood Flow
Metab. 25:431–439. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee ST, Chu K, Jung KH, Ko SY, Kim EH,
Sinn DI, Lee YS, Lo EH, Kim M and Roh JK: Granulocyte
colony-stimulating factor enhances angiogenesis after focal
cerebral ischemia. Brain Res. 1058:120–128. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tang YL, Zhao Q, Zhang YC, Cheng L, Liu M,
Shi J, Yang YZ, Pan C, Ge J and Phillips MI: Autologous mesenchymal
stem cell transplantation induce VEGF and neovascularization in
ischemic myocardium. Regul Pept. 117:3–10. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cheng Z, Liu X, Ou L, Zhou X, Liu Y, Jia
X, Zhang J, Li Y and Kong D: Mobilization of mesenchymal stem cells
by granulocyte colony-stimulating factor in rats with acute
myocardial infarction. Cardiovasc Drugs Ther. 22:363–371. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Su H, Lu R and Kan YW: Adeno-associated
viral vector-mediated vascular endothelial growth factor gene
transfer induces neovascular formation in ischemic heart. Proc Natl
Acad Sci USA. 97:13801–13806. 2000. View Article : Google Scholar : PubMed/NCBI
|