Introduction
Sepsis is a systemic inflammatory response syndrome
(SIRS) that occurs as a result of infection. Severe sepsis and
septic shock are important risk factors for mortality in critically
ill patients following major surgery (1–4).
Urine-derived sepsis is diagnosed when there is clear evidence of
urinary tract infection and SIRS (5). Early intervention for sepsis and SIRS
may rapidly and effectively influence inflammatory responses, which
is important for the prevention and treatment of multiple organ
dysfunction syndrome (6,7). A number of signaling molecules have
been implicated in the pathogenesis of urine-derived sepsis; one of
which is the gaseous signaling molecule, H2S (8,9).
H2S is produced primarily via the sulfur
amino acid metabolism signaling pathway, whereby L-cysteine is
catalyzed by cystathionine-β-synthase (CBS) and
cystathionine-γ-lyase (CSE) (10).
Endogenous H2S has been demonstrated to be extensively
involved in a variety of physiological and pathological processes
in vivo, such as inflammatory responses (11,12).
Previous studies have indicated that CBS and CSE expression is
detectable in kidney tissues, and that the endogenous production of
H2S serves an important role in the kidney function
(13,14). It has been demonstrated that low
concentrations of H2S reduce lipopolysaccharide
(LPS)-induced SIRS (15), and
increased endogenous H2S generation inhibits airway
inflammation to a certain degree (16). In addition, treatment with NaHS has
been demonstrated to inhibit LPS-induced inflammatory lesions in
endothelial cells (17), and prevent
intestinal ischemia-associated inflammatory injury (18). Furthermore, H2S
accelerates the migration of neutrophils (19) and alleviates acute lung injuries
induced by sepsis, thus increasing the survival rate of septic mice
(20). A previous study suggested
that exogenous H2S treatment may downregulate the
expression of nuclear factor-κB (NF-κB) and tumor necrosis factor
(TNF)-α and upregulate the expression of IL-10, to alleviate
urine-derived sepsis-induced kidney injury (21).
In the present study, the effects of endogenous
H2S on the inflammatory response in kidneys following
urine-derived sepsis-induced injury were investigated. A rabbit
model of urine-derived sepsis was first established by the
injection of bacteria, and DL-propargylglycine (PAG), an inhibitor
of CSE that reduces endogenous H2S production, was used
to treat the rabbits. The expression levels of
inflammation-associated cytokines, NF-κB, transforming growth
factor-β1 (TGF-β1), and interleukin-6 (IL-6), in the kidney tissues
of rabbits were subsequently detected and analyzed.
Materials and methods
Animal grouping and modeling
A total of 32 male rabbits (age, 4–5 months; weight,
1.80–2.20 kg), were provided by the Department of Experimental
Animals in University of South China (Hengyang, China). The rabbits
were housed at room temperature in 50–60% humidity with one rabbit
per cage in a 12 h dark/light cycle. The rabbits were provided with
water and commercial rabbit pellets ad libitum. The animals
were divided at random into control, sham, sepsis and PAG groups
(n=8 rabbits/group). All animal experiments were approved by the
Ethics Committee of The Second Affiliated Hospital of Nanhua
University (Hengyang, China).
The rabbit model of urine-derived sepsis was
established as described previously (21). Briefly, a vertical incision was made
along the left abdominal rectus muscle, and the middle section of
ureter was freed and ligated. A suspension of Escherichia
coli [E. coli; 108 cells/ml; ATCC, 25922;
American Type Culture Collection, Manassas, VA, USA;] was then
injected into the ureter at the proximal end of the ligation site
at a dose of 0.5 ml/kg body weight. The incision was subsequently
sutured and rabbits were fed a normal diet. Food was given at the
indicated time points but the rabbits had free access to water. The
urine-derived sepsis model was additionally established in rabbits
in the PAG group, with the addition of a single intraperitoneal
injection of 37.5 mg/kg body weight PAG immediately following the
surgical operation (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany).
The same surgical procedure was performed in rabbits in the sham
group, excluding the injection of the bacteria. Rabbits in the
control group were fed on normal diet without any additional
treatments.
Monitoring of vital signs
For each rabbit, the rectal temperature (using a
rectal thermometer), heart rate (using a watch and stethoscope) and
respiratory rate (by counting the nose hair swing frequency) were
recorded prior to surgery, and at 12, 24, 36 and 48 h following
surgery.
White blood cell counts
A total of 1–2 ml peripheral blood samples were
collected from the ear vein prior to surgery, and at 12, 24, 36 and
48 h following surgery. White blood cells were counted using a
hemocytometer.
Kidney function test
Peripheral blood samples were collected prior to
surgery, and at 12, 24, 36 and 48 h following surgery. The levels
of creatinine and urea nitrogen were measured using an automatic
biochemical analyzer (AU800; Olympus Corporation, Tokyo,
Japan).
Hematoxylin and eosin (H&E)
staining
At 48 h following surgery, the rabbits were
anesthetized and their left kidneys were removed. Kidney tissues
were subsequently fixed with 4% formaldehyde at room temperature
for 24–48 h, embedded in paraffin and cut into 5-µm-thick sections.
Tissues were then subject to H&E staining at 60°C for 30 min,
and visualized under a light microscope at magnification, ×400. In
total, 10 fields of view were randomly selected and observed from
each section.
Serum H2S
concentration
At 48 h following surgery, the rabbits were
anesthetized, and approximately 5–7 ml venous blood from the left
kidney was collected and centrifuged at 1,500 × g at room
temperature for 10 min. A total of 0.5 ml zinc acetate solution
(1%) was subsequently added to 0.1 ml test plasma, followed by 0.5
ml dimethyl-p-phenylenediamine sulfate/HCl solution (20 mM/7.2 M)
and 0.4 ml ferric chloride/HCl solution (30 mM/1.2 M). The solution
was incubated at room temperature for 20 min, and 1 ml
trichloroacetic acid (10%) and 2.5 ml ddH2O were
subsequently added. Samples were then centrifuged at 2,500 × g at
room temperature for 8 min, the supernatant was collected and the
absorbance at 679 nm was read using a spectrophotometer. The
H2S concentration was calculated according to a standard
curve.
CSE activity
At 48 h following surgery, rabbits were anesthetized
and the left kidneys were removed. A total of ~200 mg tissue was
mixed with 10% (w/v) 50 mM/l potassium phosphate buffer (pH 6.8),
and then homogenized on ice. Following centrifugation at 4°C at
2,500 × g at room temperature for 10 min, the supernatant was
collected, and 80 µl L-cysteine (0.5 M) plus 3.52 ml 5-pyridoxal
phosphate (0.5%) was added to 400 µl tissue homogenate. A total of
0.5 ml zinc acetate (1%) was then added to the central chamber; in
which folded filter paper was placed. The reaction system and the
central chamber were placed in a 25-ml conical flask filled with
nitrogen, and incubated in a water bath at 37°C for 90 min. The
reaction was terminated by adding 0.5 ml trichloroacetic acid
(50%), and the flask was sealed with a paraffin membrane. Following
a further 60 min incubation at 37°C, the mixture in the central
chamber was transferred to a fresh tube containing 3.5 ml
ddH2O. A total of 0.5 ml dimethyl-p-phenylenediamine
sulfate/HCl solution (20 mM/7.2 M) and 0.4 ml ferric chloride/HCl
solution (30 mM/1.2 M) was added, and the solution was incubated at
37°C for 20 min prior to centrifugation at 1,500 × g at 37°C for 5
min. The absorbance at 670 nm was read using a spectrophotometer,
and the H2S concentration was calculated according to a
standard curve. CSE activity (nM/min/mg) was set as the
concentration of H2S produced during 1 min in 1 mg
kidney tissue.
Western blot analysis
The expression levels of NF-κB, IL-6, and TGF-β1 in
kidney tissues were determined by western blot analysis. The kidney
tissue (harvested 48 h post surgery) was lysed with a PBS lysis
buffer (0.24 g potassium dihydrogen phosphate, 1.44 g disodium
hydrogen phosphate, 0.2 g potassium chloride, 8 g sodium chloride
in 1,000 ml solution; pH 7.4) and total protein was extracted
according to the manufacturer's protocol. Sample protein
concentrations were determined using the bicinchoninic acid assay
method (Beyotime Institute of Biotechnology, Shanghai, China). A
total of 50 µg protein sample was loaded per lane and separated by
10% SDS-PAGE, and then electronically transferred onto a
polyvinylidene difluoride membrane. The membranes were subsequently
blocked with 5% non-fat milk at 37°C for 1 h prior to incubation
with primary antibodies against NF-κB (bsm-33117M; 1:500 dilution),
IL-6 (bs-4587M; 1:500 dilution), TGF-β1 (bsm-33287M; 1:500
dilution), or β-actin (bsm-33036M; 1:5,000 dilution) (all purchased
from BIOSS, Beijing, China) at 4°C overnight. Following washing
with Tris-buffered saline and Tween-20 solution, the membrane was
incubated with a goat anti-mouse immunoglobulin M/horseradish
peroxidase antibodies (bs-0368G-HRP; 1:10,000; BIOSS) at room
temperature for 2 h. Protein bands were visualized using an
enhanced chemiluminescence method (Beyotime Institute of
Biotechnology), according to the manufacturer's protocol and band
densities were analyzed using the GSD8000 image analysis system
(UVP, Cambridge, UK).
Statistical analysis
The results are expressed as the mean ± standard
deviation. The SPSS software program (version, 18.0; SPSS, Inc.,
Chicago, IL, USA) was used to perform statistical analyses. The
results were analyzed by one-way analysis of variance followed by a
post hoc least significant difference test. P<0.05 was
considered to indicate a statistically significant difference.
Results
PAG exacerbates pathophysiological
alterations in a rabbit model of urine-derived sepsis
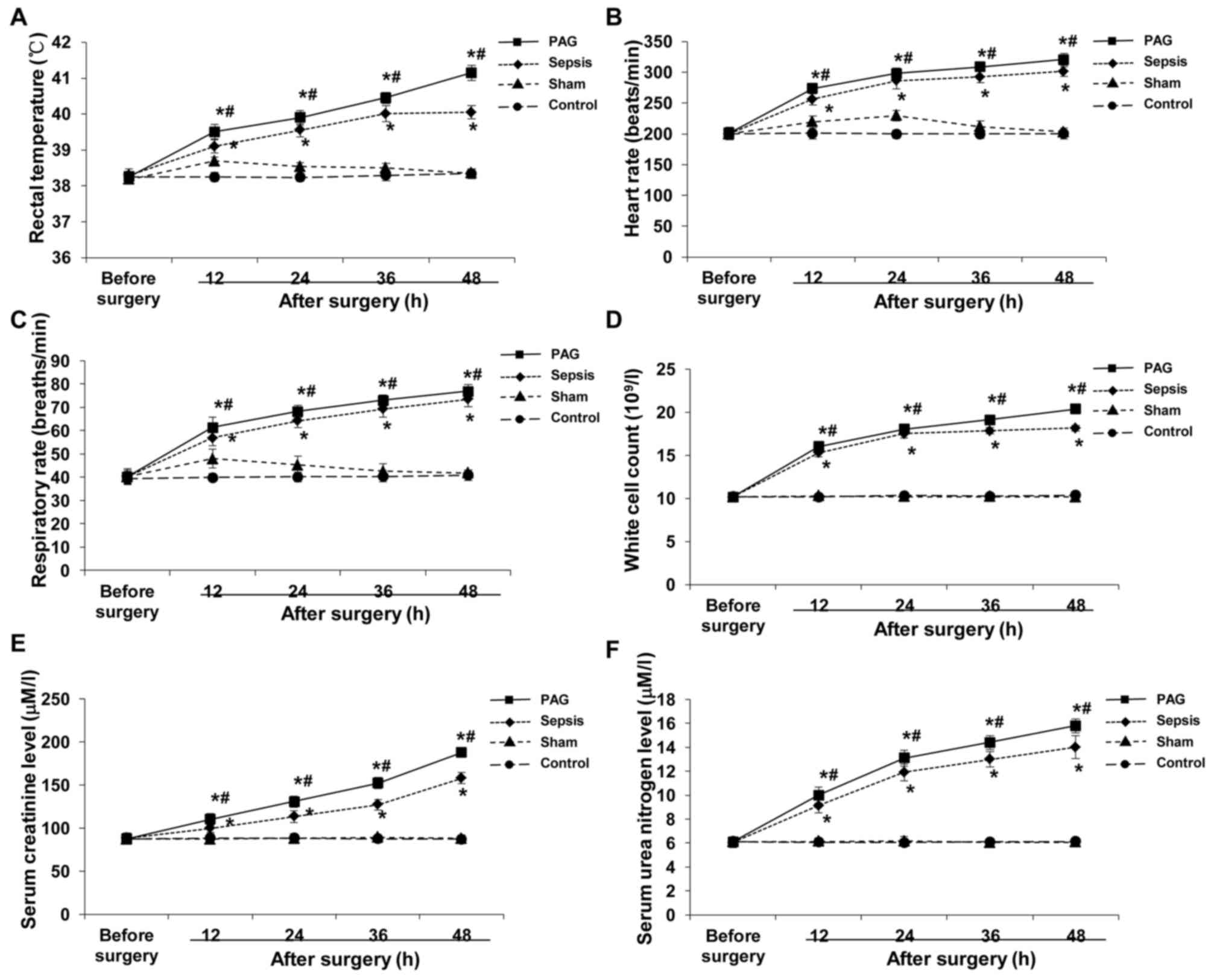
Monitoring of vital signs, routine blood
examinations and kidney function tests were performed in rabbits
from the control, sham, sepsis and PAG groups prior to surgery, and
at 12, 24, 36 and 48 h following surgery. Based on the monitoring
of vital signs, no significant differences in rectal temperature,
heart rate and respiratory rate among these four groups was
observed prior to surgery (Fig.
1A-C). By contrast, the rectal temperature, heart rate and
respiratory rate were significantly elevated at 12 h following
surgery in the sepsis and PAG groups compared with the sham group
(P<0.05); however, a gradual plateauing in the level of these
factors was observed at 48 h following surgery (Fig. 1A-C). In the sepsis group, the rectal
temperature, heart rate and respiratory rate of rabbits were
significantly elevated at 12 h following surgery compared with the
sham group (P<0.05), and continued to increase at 24, 36 and 48
h following surgery. In addition, the rectal temperature, heart
rate, and respiratory rate of rabbits in the PAG group were
significantly elevated following surgery when compared with the
sham group and the sepsis group (P<0.05; Fig. 1A-C). There was no significant
difference between the control group and the sham group.
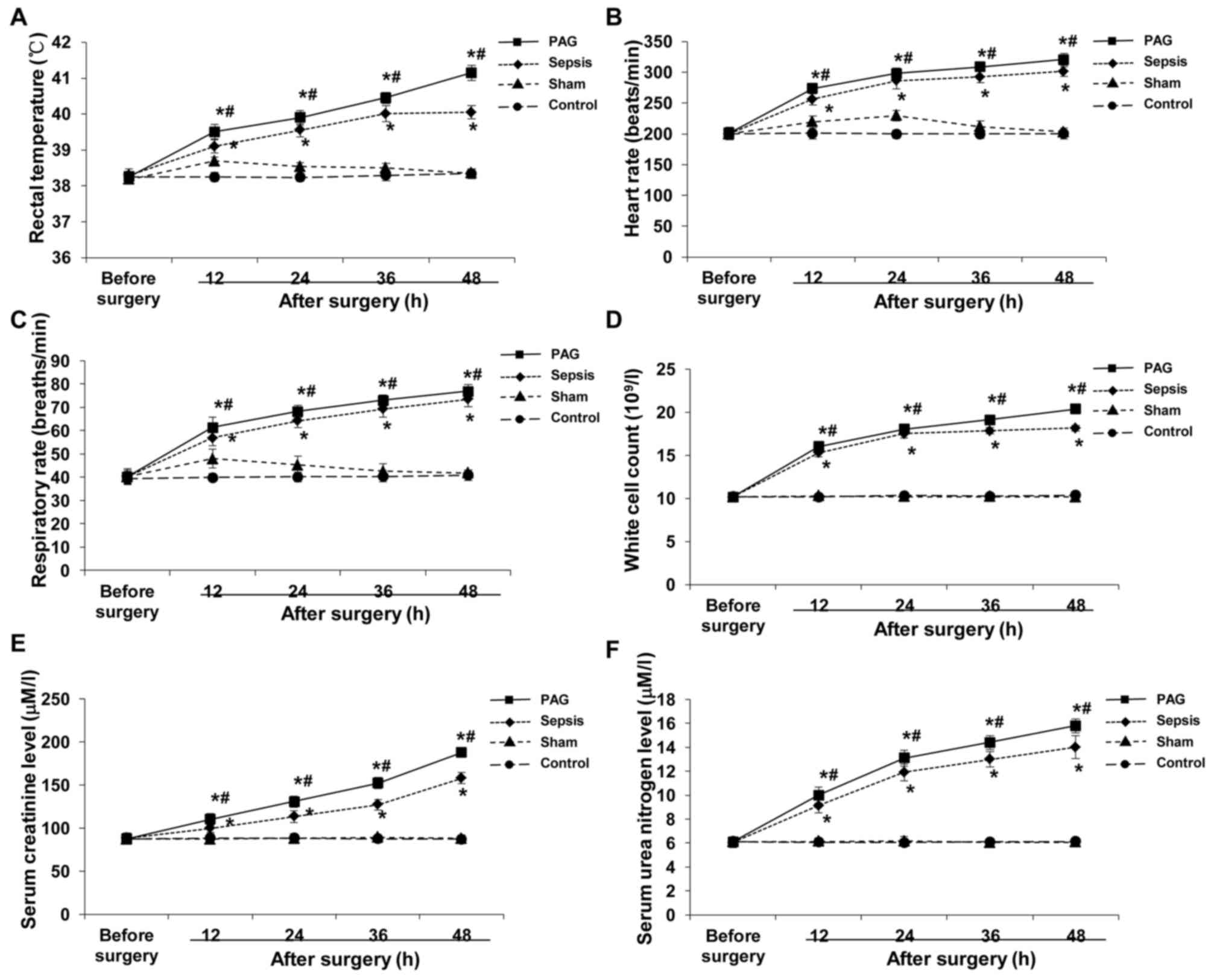 | Figure 1.Effect of PAG on pathophysiological
alterations in a rabbit model of urine-derived sepsis. Vital sign
monitoring, routine blood examinations and kidney function tests
were performed in rabbits from the control, sham, sepsis and PAG
groups prior to surgery, and at 12, 24, 36 and 48 h following
surgery. The (A) rectal temperature, (B) heart rate, (C)
respiratory rate, (D) white cell count, and serum levels of (E)
creatinine and (F) urea nitrogen were detected and analyzed.
*P<0.05 vs. sham group; #P<0.05 vs. sepsis group.
PAG, DL-propargylglycine. |
Similar results were observed for the routine blood
examinations and kidney function tests in the control, sham, sepsis
and PAG groups. Prior to surgery, no significant differences in the
white cell count and the levels of creatinine and urea nitrogen
among these four groups were observed (Fig. 1D-F). In the sepsis and PAG groups,
the white cell counts and the levels of creatinine and urea
nitrogen were significantly elevated following surgery when
compared with the sham group at the corresponding time points
(P<0.05), with increased levels of these factors observed in the
PAG group compared with the sepsis group at all time points
(Fig. 1D-F). No significant
differences were observed between the control group and the sham
group. These results indicated the successful establishment of a
rabbit model of urine-derived sepsis, which was considered to be
suitable for subsequent experiments. In addition, PAG treatment was
demonstrated to exacerbate sepsis-associated pathophysiological
alterations.
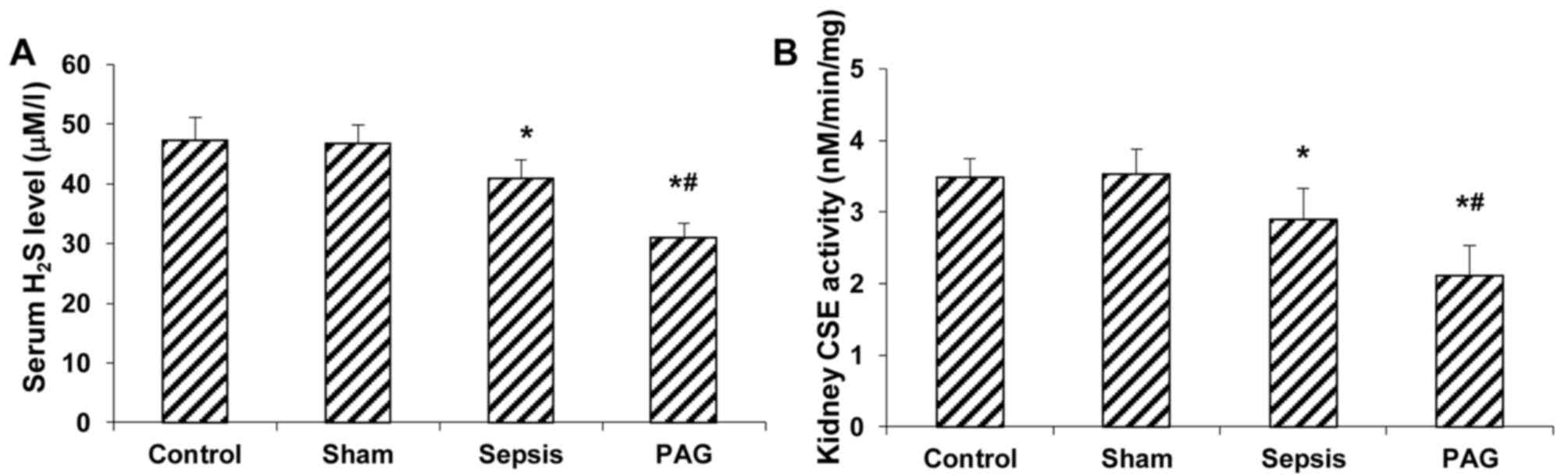
PAG reduces the serum H2S
concentration and kidney CSE activity in a rabbit model of
urine-derived sepsis
The effects of PAG on the concentration of serum
H2S and kidney CSE activity in a rabbit model of
urine-derived sepsis were subsequently investigated. As
demonstrated in Fig. 2A, no
significant difference in the serum H2S concentration
between the control and sham groups at 48 h following surgery was
observed. By contrast, the serum H2S concentration was
significantly reduced in the sepsis group at 48 h following surgery
when compared with the sham group (P<0.05; Fig. 2A). In addition, a significant
reduction the serum H2S concentration was observed in
the PAG group at 48 h after surgery when compared with the sham and
sepsis groups (P<0.05; Fig 2A).
Similar results were observed for the kidney CSE activity
detection. When compared with the sham group, CSE activity in
kidney tissues of rabbits in the sepsis group were significantly
decreased at 48 h following surgery (P<0.05), with a greater
reduction in kidney CSE activity in the PAG group compared with the
sham and sepsis groups (P<0.05; Fig.
2B). These results suggest that PAG treatment further decreased
the serum H2S concentration and kidney CSE activity in a
rabbit model of urine-derived sepsis, which suggests that PAG
exacerbates disease progression.
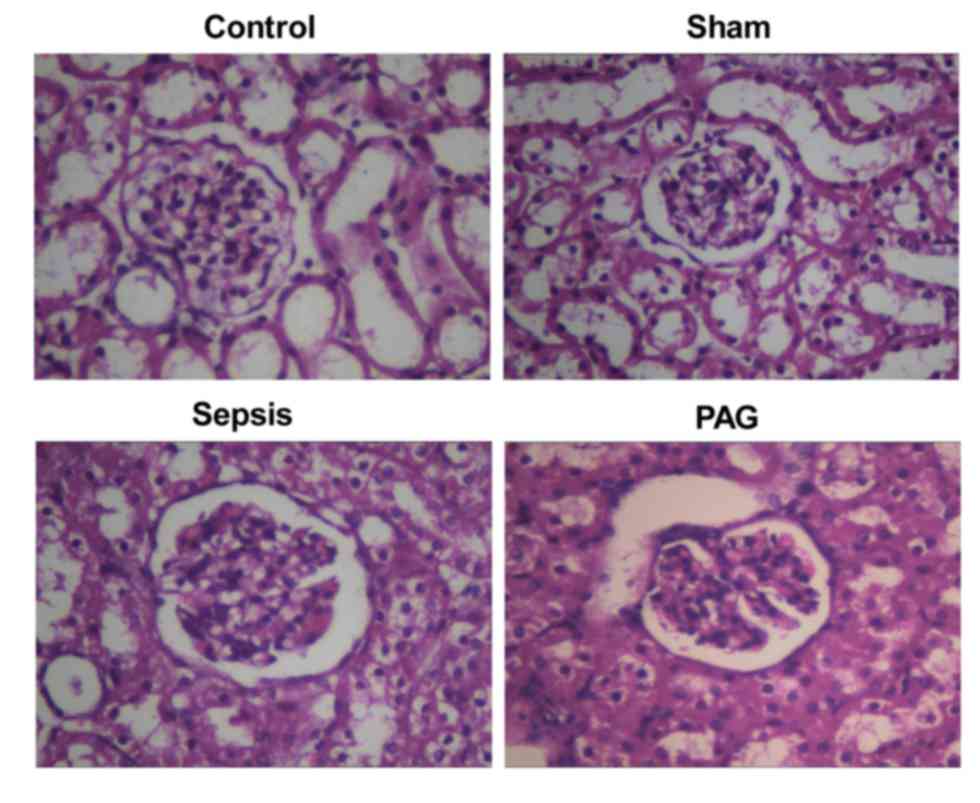
PAG exacerbates histopathological
kidney lesions in a rabbit model of urine-derived sepsis
In order to investigate the effects of PAG on the
formation of histopathological kidney lesions in a rabbit model of
urine-derived sepsis, H&E staining was performed. As indicated
in Fig. 3, no obvious
histopathological alterations in the kidney tissues of rabbits in
the control and sham groups were observed (Fig. 3). However, in the sepsis group,
H&E staining indicated obvious structural abnormalities in the
kidney tissues, including an abnormal glomerulus morphology, glomus
atrophy and deformation and kidney capsule expansion. In addition,
edema and necrosis were observed in the kidney tubular epithelial
cells, with detached necrotic cells blocking the lumen.
Furthermore, the size of the renal capsule and renal tubular lumen
were significantly expanded and significant kidney interstitium
hyperemia and edema, and abundant inflammatory cell infiltration
were observed in the kidney tissues of rabbits in the sepsis group
(Fig. 3). When compared with the
sepsis group, these histopathological alterations were
significantly exacerbated in the PAG group (Fig. 3). These results provide evidence to
suggest that treatment with PAG worsens the development of
histopathological kidney lesions in a rabbit model of urine-derived
sepsis.
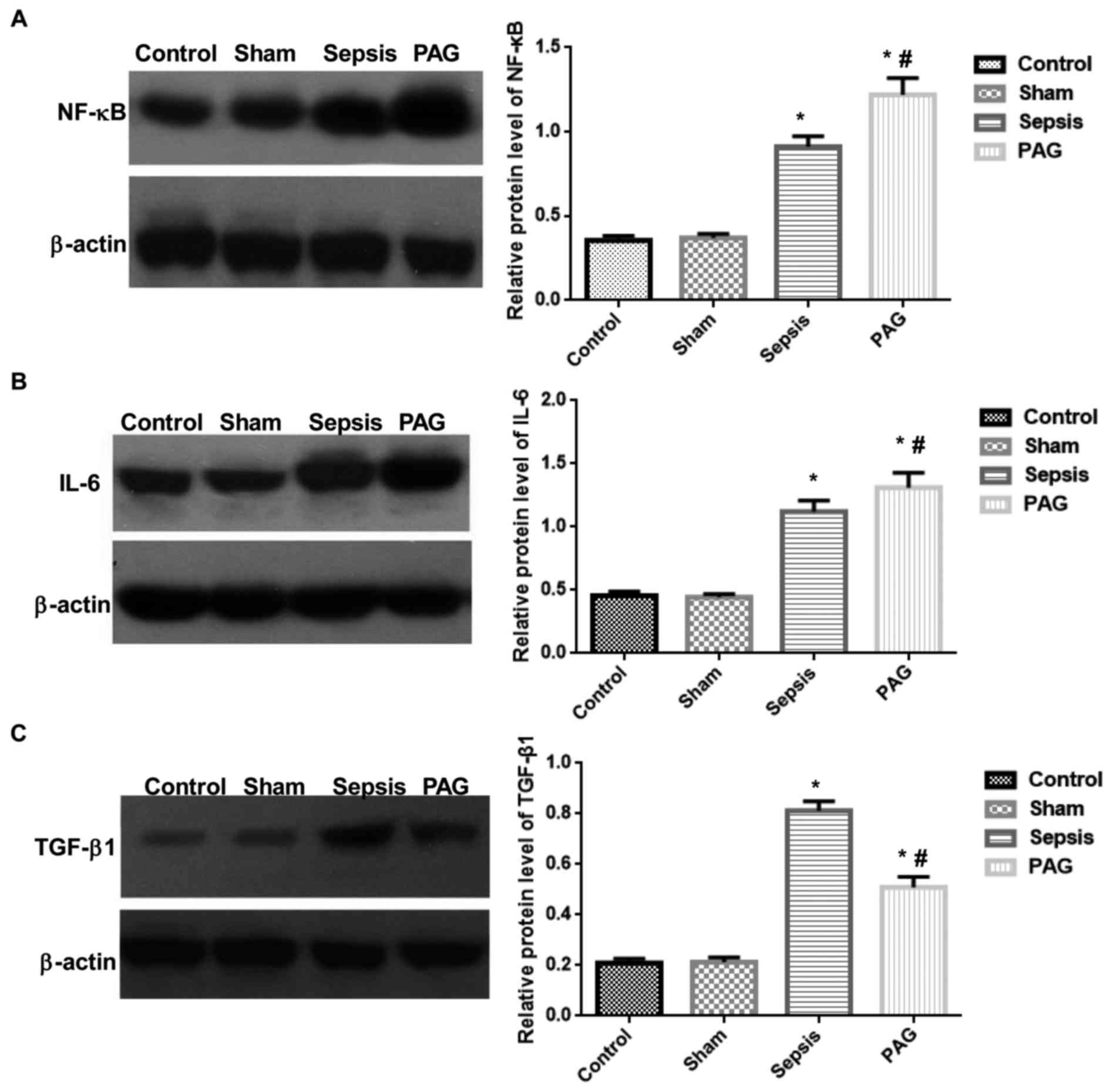
PAG alters the expression levels of
inflammation-associated cytokines in kidney tissues in a rabbit
model of urine-derived sepsis
To investigate the effects of PAG on the expression
levels of NF-κB, IL-6 and TGF-β1 in the kidney tissues of rabbits
with urine-derived sepsis, western blot analysis was performed. As
indicated in Fig. 4, no significant
difference in the protein expression levels of NF-κB, IL-6 and
TGF-β1 was observed between the control and sham groups at 48 h
following surgery. However, the expression levels of NF-κB and IL-6
in kidney tissues were significantly elevated in the sepsis group
when compared with the sham group (P<0.05). The expression of
NF-κB and IL-6 were significantly elevated in the PAG group when
compared with sham and sepsis groups (P<0.05; Fig. 4). In addition, TGF-β1 protein
expression was significantly elevated in the sepsis group compared
with the sham group (P<0.05). However, compared with the sepsis
group, the expression level of TGF-β1 was significantly reduced in
the PAG group (P<0.05); however, its expression remained
significantly higher than the sham group (P<0.05). No
significant differences were observed between the control group and
the sham group. These results suggest that PAG treatment may
significantly increase the expression levels of NF-κB and IL-6, and
decrease TGF-β1 expression in kidney tissues, in a rabbit model of
urine-derived sepsis.
Discussion
In the present study, a rabbit model of
urine-derived sepsis was established by injecting E. coli
into the ligated ureter (21).
Rabbits were subsequently treated with PAG, which is an inhibitor
of CSE. The effect of endogenous H2S on the inflammatory
response in kidneys following urine-derived sepsis was subsequently
investigated. The results demonstrated that the rectal temperature,
heart rate and respiratory rate of rabbits in the sham group were
elevated at 12 h following surgery; however these returned to
levels similar to that of the control group at 36–48 h following
surgery. Similar results were observed for the white cell counts,
and the serum levels of creatinine and urea nitrogen. However, a
significant and time-dependent increase in rectal temperature,
heart rate, respiratory rate and white cell count was observed in
the sepsis group when compared with the sham group. In addition,
pathological alterations were observed in the kidney tissues of
rabbits in the sepsis group. According to the diagnostic criteria
of urine-derived sepsis described in a previous study by Yao et
al (22), the model generated in
the present study was considered to have been successfully
established and suitable for subsequent investigations.
NF-κB activates the expression of a variety of
inflammatory factors, and is a key factor involved in the systemic
inflammatory response (23,24). During bacterial infection, endotoxins
enter the blood stream and form a complex with binding proteins in
the cytoplasm. It has been demonstrated that in sepsis, due to the
over-reaction of the host immune system against bacteria and
toxins, the pro-inflammatory cytokines (TNF-α, NF-κB and IL-6) were
initially produced, followed by the rapid release of
anti-inflammatory factors (including, TGF-β and IL-10), which
induced alternating peaks of pro-inflammatory and anti-inflammatory
cytokines in the blood circulation (23,25). In
addition, endotoxin may enter the blood circulation and form a
complex with binding proteins in the plasma, specifically binding
to molecular receptors (such as CD14) on the surface of the cell
membranes (26). The complex then
specifically binds to receptors, such as cluster of differentiation
14, on the cellular membrane (27),
which leads to transduction of signaling pathways into the
cytoplasm via Toll-like receptors. The TNF or tyrosine protein
kinase signaling pathways are then activated, thus leading to the
activation of NF-κB in the cytoplasm and its translocation to the
nucleus, which initiates the transcription of target genes
(28). In addition, endotoxins are
able to activate NF-κB in the cytoplasm via plant disease
resistance-like proteins (29).
Activated NF-κB induces the expression and release of specific
pro-inflammatory cytokines, including TNF-α, IL-6 and IL-8
(30), which subsequently enhances
the activation of NF-κB and amplifies the inflammatory response.
Anti-inflammatory cytokines, such as TGF-β and IL-10, are
simultaneously synthesized and released, thereby reducing the
expression of pro-inflammatory mediators and preventing the
development of inflammatory response-associated syndromes. Sepsis
occurs a result of an excessive inflammatory response (31).
IL-6 exhibits pro- and anti-inflammatory effects.
IL-6 induces the phosphorylation of signal transducer and activator
of transcription 3 to prevent T-cell apoptosis. This leads to the
accumulation of circulating T-cells and the development of chronic
inflammation, which is inhibited by the anti-IL-6 receptor antibody
(32). A previous study demonstrated
that alterations in the level of IL-6 may be a useful early
indicator of inflammation and sepsis (33). TGF-β has been demonstrated to exert
immunosuppressive functions, which serve important roles in
congenital and acquired immunity (34). TGF-β downregulates the expression of
pro-inflammatory cytokines and antagonizes the development of an
excessive inflammatory response. A previous study demonstrated that
endotoxins significantly increase the expression of
pro-inflammatory cytokines, such as TNF-α and IL-1β, as well as
their receptors in mice with a defect in TGF-β, which leads to an
excessive inflammatory response (35).
H2S is widely involved in a number of
biological processes in various tissues and/or organs (36). Treatment with PAG, an inhibitor of
CSE, may inhibit the endogenous production of H2S
(22). Previous studies have
demonstrated that, H2S inhibits the excessive activation
of NF-κB, reduces the production of pro-inflammatory cytokines and
increases the expression of anti-inflammatory factors, thereby
reducing sepsis-induced injuries (21,37). In
addition, H2S may reduce the production and release of a
variety of pro-inflammatory cytokines by inhibiting the
NF-κB/cyclooxygenase-2 signaling pathway, thus preventing an
excessive inflammatory response (37). The results of the present study
demonstrated that the expression levels of NF-κB, IL-6 and TGF-β1
in kidney tissues were significantly upregulated in the sepsis
group when compared with the sham group at 48 h following surgery.
Following treatment with PAG, endogenous H2S generation
and kidney CSE activity were significantly reduced when compared
with the untreated sepsis group, which is consistent with the
results presented by Ma et al (38). In addition, PAG treatment
significantly upregulated the expression of NF-κB and IL-6, and
downregulated the expression of TGF-β1 in kidney tissues at 48 h
following surgery when compared with the sepsis group. Furthermore,
histopathological alterations in the kidney tissues were
exacerbated, and white cell counts were further elevated by PAG
treatment in the rabbit model of urine-derived sepsis, thus
indicating decreased kidney function. The effects of PAG in the
rabbit model of urine-derived sepsis may be associated with the
altered expression levels of NF-κB, IL-6 and TGF-β1 in kidney
tissues. Future comprehensive studies are required to investigate
this hypothesis further.
In conclusion, the results of the current study
indicated that PAG treatment decreased H2S production
and CSE activity in a rabbit model of urine-derived sepsis. In
addition, treatment with PAG significantly exacerbated
urine-derived sepsis-induced pathological alterations in kidney
tissues, which may have been associated with the altered expression
levels of inflammation-associated cytokines. These results provide
novel information that may facilitate the development of clinical
strategies for the prevention and treatment of urine-derived sepsis
and associated kidney injury.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Hunan
Provincial Natural Science Foundation (grant no. 13JJ9009).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HLQ and XC established the rabbit model of
urine-derived sepsis, monitored the vital signs, performed HE
staining and western blot analysis and drafted the manuscript. ZGL
counted the white blood cells. LWZ performed the kidney function
test. TZ and NY measured the serum H2S concentration. XYL, HX and
JL conducted the CSE activity test. HLQ and XC performed the
statistical analysis. WJX conceived and designed the study and
revised the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Second Affiliated Hospital of Nanhua University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Stevenson EK, Rubenstein AR, Radin GT,
Wiener RS and Walkey AJ: Two decades of mortality trends among
patients with severe sepsis: A comparative meta-analysis. Crit Care
Med. 42:625–631. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Levy MM, Dellinger RP, Townsend SR,
Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay
G, Beale R, et al: The Surviving Sepsis Campaign: Results of an
international guideline-based performance improvement program
targeting severe sepsis. Crit Care Med. 38:367–374. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Martin GS, Mannino DM, Eaton S and Moss M:
The epidemiology of sepsis in the United States from 1979 through
2000. N Engl J Med. 348:1546–1554. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cawcutt KA and Peters SG: Severe sepsis
and septic shock: Clinical overview and update on management. Mayo
Clin Proc. 89:1572–1578. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Grabe M, Bjerklund-Johansen TE, Botto H,
Çek M, Naber KG, Pickard RS, Tenke P, Wagenlehner F and Wullt B:
Guidelines on urological infectionsEuropean Association of Urology.
Arnhem: 2013, https://uroweb.org/wp-content/uploads/18_Urological-infections_LR.pdfLimited
Update March 2013. PubMed/NCBI
|
|
6
|
Fry DE: Sepsis, systemic inflammatory
response, and multiple organ dysfunction: The mystery continues. Am
Surg. 78:1–8. 2012.PubMed/NCBI
|
|
7
|
Makkonen J, Pietilainen KH, Rissanen A,
Kaprio J and Yki-Jarvinen H: Genetic factors contribute to
variation in serum alanine aminotransferase activity independent of
obesity and alcohol: A study in monozygotic and dizygotic twins. J
Hepatol. 50:1035–1042. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou CF and Tang XQ: Hydrogen sulfide and
nervous system regulation. Chin Med J (Engl). 124:3576–3582.
2011.PubMed/NCBI
|
|
9
|
Wang R: Hydrogen sulfide: The third
gasotransmitter in biology and medicine. Antioxid Redox Signal.
12:1061–1064. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kimura H: Hydrogen sulfide: Its
production, release and functions. Amino Acids. 41:113–121. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Whiteman M and Winyard PG: Hydrogen
sulfide and inflammation: The good, the bad, the ugly and the
promising. Expert Rev Clin Pharmacol. 4:13–32. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Calvert JW, Coetzee WA and Lefer DJ: Novel
insights into hydrogen sulfide-mediated cytoprotection. Antioxid
Redox Signal. 12:1203–1217. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lobb I, Sonke E, Aboalsamh G and Sener A:
Hydrogen sulphide and the kidney: Important roles in renal
physiology and pathogenesis and treatment of kidney injury and
disease. Nitric Oxide. 46:55–65. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Koning AM, Frenay AR, Leuvenink HG and van
Goor H: Hydrogen sulfide in renal physiology, disease and
transplantation-the smell of renal protection. Nitric Oxide.
46:37–49. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tokuda K, Kida K, Marutani E, Crimi E,
Bougaki M, Khatri A, Kimura H and Ichinose F: Inhaled hydrogen
sulfide prevents endotoxin-induced systemic inflammation and
improves survival by altering sulfide metabolism in mice. Antioxid
Redox Signal. 17:11–21. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang P, Li F, Wiegman CH, Zhang M, Hong
Y, Gong J, Chang Y, Zhang JJ, Adcock I, Chung KF and Zhou X:
Inhibitory effect of hydrogen sulfide on ozone-induced airway
inflammation, oxidative stress, and bronchial hyperresponsiveness.
Am J Respir Cell Mol Biol. 52:129–137. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pan LL, Liu XH, Gong QH, Wu D and Zhu YZ:
Hydrogen sulfide attenuated tumor necrosis factor-alpha-induced
inflammatory signaling and dysfunction in vascular endothelial
cells. PLoS One. 6:e197662011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zuidema MY, Peyton KJ, Fay WP, Durante W
and Korthuis RJ: Antecedent hydrogen sulfide elicits an
anti-inflammatory phenotype in postischemic murine small intestine:
Role of heme oxygenase-1. Am J Physiol Heart Circ Physiol.
301:H888–894. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Spiller F, Orrico MI, Nascimento DC,
Czaikoski PG, Souto FO, Alves-Filho JC, Freitas A, Carlos D,
Montenegro MF, Neto AF, et al: Hydrogen sulfide improves neutrophil
migration and survival in sepsis via K+ATP channel activation. Am J
Respir Crit Care Med. 182:360–368. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ang SF, Sio SW, Moochhala SM, MacAry PA
and Bhatia M: Hydrogen sulfide upregulates cyclooxygenase-2 and
prostaglandin E metabolite in sepsis-evoked acute lung injury via
transient receptor potential vanilloid type 1 channel activation. J
Immunol. 187:4778–4787. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen X, Xu W, Wang Y, Luo H, Quan S, Zhou
J, Yang N, Zhang T, Wu L, Liu J, et al: Hydrogen sulfide reduces
kidney injury due to urinary-derived sepsis by inhibiting NF-kappaB
expression, decreasing TNF-alpha levels and increasing IL-10
levels. Exp Ther Med. 8:464–470. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yao Y, Sheng Z and Lin H: New
understanding of the definition and diagnosis of sepsis. Zhongguo
Wei Zhong Bing Ji Jiu Yi Xue. 16:321–324. 2004.PubMed/NCBI
|
|
23
|
Souza AC, Volpini RA, Shimizu MH, Sanches
TR, Camara NO, Semedo P, Rodrigues CE, Seguro AC and Andrade L:
Erythropoietin prevents sepsis-related acute kidney injury in rats
by inhibiting nuclear-factor kappa B and upregulating endothelial
nitric oxide synthase. Am J Physiol Renal Physiol. 302:1045–1054.
2012. View Article : Google Scholar
|
|
24
|
Xu H, Ye X, Steinberg H and Liu SF:
Selective blockade of endothelial NF-kappaB pathway differentially
affects systemic inflammation and multiple organ dysfunction and
injury in septic mice. J Pathol. 220:490–498. 2010.PubMed/NCBI
|
|
25
|
Sadik NA, Mohamed WA and Ahmed MI: The
association of receptor of advanced glycated end products and
inflammatory mediators contributes to endothelial dysfunction in a
prospective study of acute kidney injury patients with sepsis. Mol
Cell Biochem. 359:73–81. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Peri F, Piazza M, Calabrese V, Damore G
and Cighetti R: Exploring the LPS/TLR4 signal pathway with small
molecules. Biochem Soc Tran. 38:1390–1395. 2010. View Article : Google Scholar
|
|
27
|
Peri F, Piazza M, Calabrese V, Damore G
and Cighetti R: Exploring the LPS/TLR4 signal pathway with small
molecules. Biochem Soc Trans. 38:1390–1395. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kim TH, Yoon SJ and Lee SM: Genipin
attenuates sepsis by inhibiting toll-like receptor signaling. Mol
Med. 18:455–465. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Thome M, Hofmann K, Burns K, Martinon F,
Bodmer JL, Mattmann C and Tschopp J: Identification of CARDIAK, a
RIP-like kinase that associates with caspase-1. Curr Biol.
8:885–888. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Liu Z, Guan Y, Sun X, Shi L, Liang R, Lv X
and Xin W: HSV-1 activates NF-kappaB in mouse astrocytes and
increases TNF-alpha and IL-6 expression via Toll-like receptor 3.
Neurol Res. 35:755–762. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sagy M, Al-Qaqaa Y and Kim P: Definitions
and pathophysiology of sepsis. Curr Probl Pediatr Adolesc Health
Care. 43:260–263. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mudter J and Neurath MF: Il-6 signaling in
inflammatory bowel disease: pathophysiological role and clinical
relevance. Inflamm Bowel Dis. 13:1016–1023. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tambuyzer T, De Waele T, Chiers K,
Berckmans D, Goddeeris BM and Aerts JM: Interleukin-6 dynamics as a
basis for an early-warning monitor for sepsis and inflammation in
individual pigs. Res Vet Sci. 96:460–463. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hiraki S, Ono S, Tsujimoto H, Kinoshita M,
Takahata R, Miyazaki H, Saitoh D and Hase K: Neutralization of
interleukin-10 or transforming growth factor-beta decreases the
percentages of CD4+ CD25+ Foxp3+ regulatory T cells in septic mice,
thereby leading to an improved survival. Surgery. 151:313–322.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
McCartney-Francis N, Jin W and Wahl SM:
Aberrant toll receptor expression and endotoxin hypersensitivity in
mice lacking a functional TGF-beta 1 signaling pathway. J Immunol.
172:3814–3821. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kimura H, Shibuya N and Kimura Y: Hydrogen
sulfide is a signaling molecule and a cytoprotectant. Antioxid
Redox Signal. 17:45–57. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yang C, Yang Z, Zhang M, Dong Q, Wang X,
Lan A, Zeng F, Chen P, Wang C and Feng J: Hydrogen sulfide protects
against chemical hypoxia-induced cytotoxicity and inflammation in
HaCaT cells through inhibition of ROS/NF-κB/COX-2 pathway. Plos
One. 6:e219712011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ma B, Liang G, Zhang F, Chen Y and Zhang
H: Effect of hydrogen sulfide on restenosis of peripheral arteries
after angioplasty. Mol Med Rep. 5:1497–1502. 2012.PubMed/NCBI
|