Introduction
Gastric polyps (GPs) are defined as protuberant
mucosal lesions that are usually detected endoscopically. Most
patients are asymptomatic; however, depending on their size and
location, some large GPs may cause symptoms, including bleeding,
chest pain, abdominal pain, anemia and even gastric tract
obstruction (1–4).
The widespread use of gastroscopy in China
contributes to the improvement of the detection rate of GPs.
Previous studies have reported that the rate of GPs was between
1.0–6.4% and the prevalence of GPs has been gradually increasing
over the past decade (4–6). In addition, GPs were less common in
males than in females, with a ratio of 1:1.8 to 1:2.5 (4–6). Other
studies also indicated that the detection rate of GPs increases
with increasing age (7,8). The most common pathologic type of GPs
are gastric fundus gland polyp and hyperplastic polyp, which are
associated with an increased risk of gastric cancer (7,8). Thus,
it is important to further improve the detection rate of GPs.
Sedated gastroscopy, i.e., gastroscopy under
conscious sedation, improves the patients' tolerance of procedures
and in recent years, it has become increasingly popular in China.
The present study hypothesized that the GP detection rate on
gastroscopy may be improved with sedation. Thus, the aim of this
retrospective observational study was to assess the superiority of
sedated gastroscopy over unsedated gastroscopy in detecting
GPs.
Patients and methods
Patients
In the present retrospective study, patients who
underwent gastroscopy with gastrointestinal symptoms, including
abdominal distention, abdominal pain, belching and sour
regurgitation or without symptoms at the First Affiliated Hospital
of Wenzhou Medical University (Wenzhou, China) between January 1,
2014 and December 31, 2016 were included. Patients decided to
undergo gastroscopic examination with or without sedation by
themselves, after having been informed about the benefits, risks
and limitations of sedation, as well as those of unsedated
gastroscopy, according to the recommendations of the American
Society for Gastrointestinal Endoscopy (9). No additional procedures were performed
during the gastroscopic examination. Those patients with GPs
diagnosed under gastroscopy were recorded, and the pathologies were
confirmed as inflammatory polyp, hyperplastic polyp, gastric fundus
gland polyp adenomas, juvenile polyp, squamous hyperplasia and
adenocarcinoma, while pathologies confirmed as pathology-negative
polyp, xanthelasma, mesenchymoma, lymphoma, leiomyoma, ectopic
pancreas, carcinoid and hamartoma were excluded within 7 working
days by experienced pathologists. In addition, patients who had a
history of gastric cancer, colon cancer, stomach surgery or colon
surgery were excluded. Patients who met the exclusion criteria were
deleted when detection rate was calculated. A total of 165,142
patients were included in the current study. A total of 112,512
patients underwent unsedated gastroscopy, whereas 52,630 patients
underwent sedated gastroscopy (propofol, 2 mg/kg, intravenous) with
monitoring via electrocardiograms.
Data
The present study retrospectively analyzed the data
of 165,142 patients who underwent gastroscopy, and 6,195 patients
with GPs were diagnosed on gastroscopy. The patient data were
obtained from endoscopy and pathologic reports, with parameters
extracted including sex, age, inspection time and GP
characteristics (location, histological diagnosis, number and
size).
Statistical analysis
Data were analyzed using SPSS (version 17.0; SPSS,
Inc., Chicago, IL, USA). Patient age was expressed as the mean ±
standard deviation. The detection rate in the two groups was
standardized prior to the c2 test due to a
disproportionate age distribution. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patient characteristics and procedure
time are not different
A total of 165,142 gastroscopies were performed
within 3 years at the Digestive Endoscopy unit of the First
Affiliated Hospital of Wenzhou Medical University (Wenzhou, China).
No statistically significant difference in the sex distribution and
procedure time were identified between the two groups (Table I).
 | Table I.Sex distribution and procedure time in
the two groups. |
Table I.
Sex distribution and procedure time in
the two groups.
| Parameter | Unsedated gastroscopy
group (112,512) | Sedated gastroscopy
group (52,630) |
|---|
| Sex |
|
|
| Male | 60,880 (54.11%) | 28,108 (53.41%) |
|
Female | 51,632 (45.89%) | 24,522 (46.59%) |
| Age (years) | 51.90±13.73 | 49.67±12.23 |
| Procedure time
(sec) | 321.2±97.5 | 305.1±90.4 |
Comparison of GP detection rate
between sedated and unsedated gastroscopy group
A total of 6,195 GPs were diagnosed by gastroscopy
and pathologic examination. Patients were stratified into 5
different groups based on age. The detection rate significantly
differed between the unsedated and sedated gastroscopy groups of
patients aged 20–39, 40–59, 60–79 and ≥80 years, but not of those
aged <20 years (Table II).
Considering the age distribution, the GP detection rate of these
two groups was standardized prior to the statistical analysis, and
the result indicated a significantly higher detection rate in the
sedated gastroscopy group compared with that in the unsedated
gastroscopy group (Table III).
 | Table II.Clinicopathological characteristics of
GP patients. |
Table II.
Clinicopathological characteristics of
GP patients.
|
| GP detection rate, %
(n/m) |
|
|
|---|
|
|
|
|
|
|---|
| Feature | Unsedated gastroscopy
group | Sedated gastroscopy
group | χ2 | P-value |
|---|
| Age (years) |
|
|
|
|
|
<20a | 0.97 (5/515) | 1.32 (2/151) |
| 0.66 |
|
20–39 | 2.00
(410/20,482) | 3.54
(387/10,945) | 67.9 | 0.001 |
|
40–59 | 3.06
(1,754/57,301) | 5.19
(1,538/29,606) | 243.9 | 0.001 |
|
60–79 | 3.95
(1,247/31,536) | 6.41
(740/11,538) | 116.1 | 0.001 |
| ≥80 | 3.32 (89/2,678) | 5.90 (23/390) | 6.4 | 0.011 |
| Sex |
|
|
|
|
| Male | 2.11
(1,284/60,880) | 3.86
(1,086/28,108) | 228.4 | 0.001 |
|
Female | 4.30
(2,221/51,632) | 6.54
(1,604/24,522) | 174.8 | 0.001 |
| GP location |
|
|
|
|
|
Cardiac | 0.35
(398/112,512) | 0.46
(242/52,630) | 22.9 | 0.001 |
| Gastric
fundus | 0.49
(552/112,512) | 0.93
(487/52,630) | 222.1 | 0.001 |
| Gastric
body | 1.15
(1,297/11,2512) | 2.28
(1,201/52,630) | 623.3 | 0.001 |
| Gastric
angular | 0.81
(910/112,512) | 0.85
(445/52,630) | 1.4 | 0.230 |
| Gastric
antrum | 0.07
(79/112,512) | 0.08 (43/52,630) | 1.3 | 0.249 |
|
Multiple-sites | 0.24
(268/112,512) | 0.52
(272/52,630) | 170.5 | 0.001 |
| Diameter of GPs
(cm) |
|
|
|
|
| ≤0.5 | 2.75
(3,089/112,512) | 4.57
(2,405/52,630) | 779.5 | 0.001 |
|
>0.5 | 0.37
(416/112,512) | 0.54
(285/52,630) | 53.5 | 0.0001 |
 | Table III.Standardized calculation of GP
detection rate. |
Table III.
Standardized calculation of GP
detection rate.
|
|
| Unsedated gastroscopy
group | Sedated gastroscopy
group |
|---|
|
|
|
|
|
|---|
| Age group
(years) | Standard
populationa | Detection rate
(%) | Expected GPs (n) | Detection rate
(%) | Expected GPs (n) |
|---|
| <20 | 666 | 0.97 | 6 | 1.32 | 9 |
| 20–39 | 31,427 | 2.00 | 629 | 3.54 | 1,113 |
| 40–59 | 86,907 | 3.06 | 2,659 | 5.19 | 4,510 |
| 60–79 | 43,074 | 3.95 | 1,701 | 6.41 | 2,761 |
| ≥80 | 3,068 | 3.32 | 102 | 5.90 | 181 |
| Totalb | 165,142 |
| 5,097 (3.09%) |
| 8,574 (5.19%) |
The present analysis indicated that the rate of GP
detection in female patients was significantly higher than that in
male patients regardless of sedation (P=0.001). In addition, the GP
detection rates for male and female patients receiving sedated
gastroscopy were significantly higher than for those receiving
unsedated gastroscopy (Table
II).
The location of GPs between the unsedated and
sedated gastroscopy groups included cardiac, gastric fundus,
gastric body and multiple sites, which means that GPs were detected
in ≥2 anatomy sections of the stomach. The incidence of cardiac,
gastric fundus, gastric body and multiple-site GPs was
significantly different between the unsedated and sedated
gastroscopy groups, due to the different diagnostic performance of
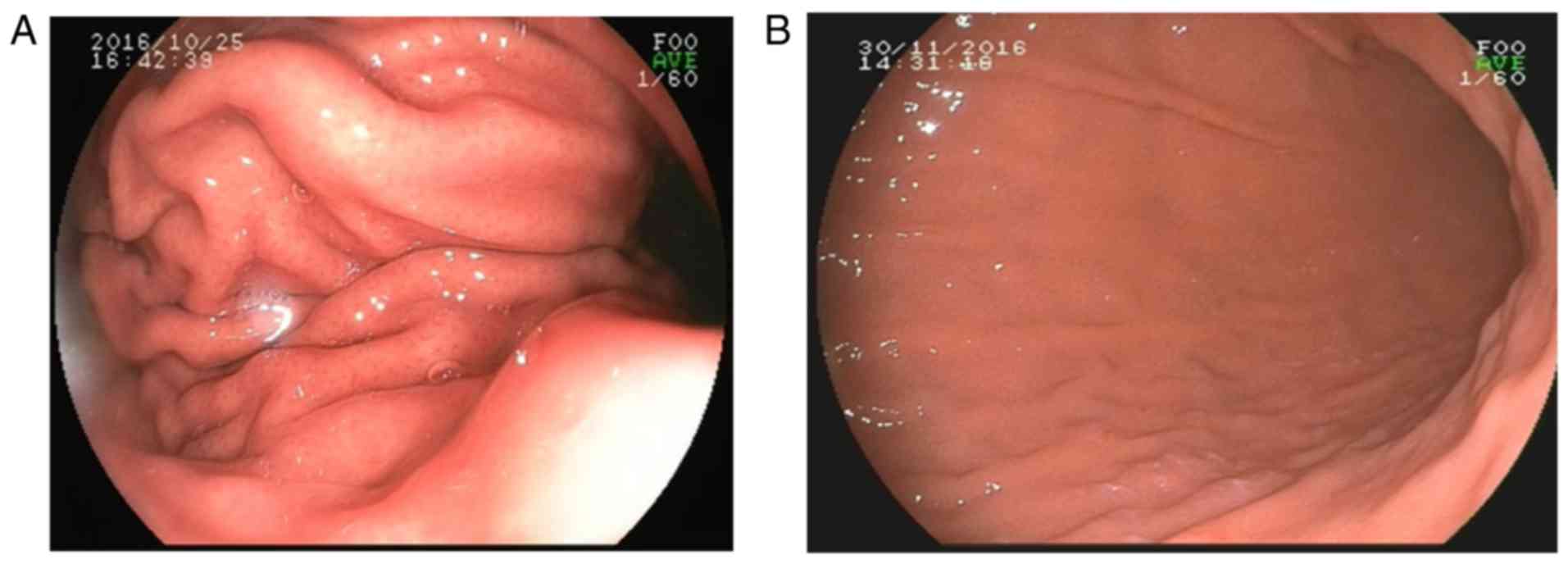
sedated and unsedated gastroscopy (Figs.
1 and 2). Whereas the incidence
of gastric angular and gastric antrum polyps was not significantly
different between these two groups (Table IV).
 | Table IV.Standardized calculation of GP
location and size. |
Table IV.
Standardized calculation of GP
location and size.
|
| Unsedated gastroscopy
group | Sedated gastroscopy
group |
|
|
|---|
|
|
|
|
|
|
|---|
| GP location | Detection rate
(%) | Expected GPs (n) | Detection rate
(%) | Expected GPs (n) | χ2 | P-value |
|---|
| Cardiac | 0.35 | 584 | 0.46 | 759 | 22.9 | 0.001 |
| Gastric fundus | 0.49 | 810 | 0.93 | 1,528 | 222.1 | 0.001 |
| Gastric body | 1.15 | 1,904 | 2.28 | 3,768 | 623.3 | 0.001 |
| Gastric antrum | 0.81 | 1,336 | 0.85 | 1,396 | 1.3 | 0.249 |
| Gastric
angular | 0.07 | 116 | 0.08 | 135 | 1.4 | 0.230 |
| Multiple-site | 0.24 | 393 | 0.52 | 853 | 170.5 | 0.001 |
| Size of GP
(cm) |
|
|
|
|
|
|
|
≤0.5 | 2.75 | 4,534 | 4.57 | 7,546 | 779.5 | 0.001 |
|
>0.5 | 0.37 | 611 | 0.54 | 894 | 53.5 | 0.001 |
Pathological characteristics of
GPs
As presented in Table
IV, the standardized GP detection rates in the sedated
gastroscopy group with lesion diameters of ≤0.5 and >0.5 cm were
significantly higher than those in the unsedated gastroscopy
group.
Pathologic examination of tissue samples of the
6,195 GPs identified them as gastric fundus gland polyp (n=3,238),
hyperplastic polyp (n=2,152), inflammatory polyp (n=531), squamous
hyperplasia (n=103), adenomatous polyp (n=116), adenocarcinoma
(n=35) and juvenile polyp (n=20) (Table
V).
 | Table V.Pathology type of GPs. |
Table V.
Pathology type of GPs.
| Pathological type
of GP | Unsedated
gastroscopy group, n (%) | Sedated gastroscopy
group, n (%) | Total, n (%) |
|---|
| Gastric fundus
gland polyp | 1,282 (20.69) | 1,956 (31.57) | 3,238 (52.27) |
| Hyperplastic
polyp | 1,020 (16.46) | 1,132 (18.27) | 2,152 (34.74) |
| Inflammatory
polyp | 253 (4.08) | 278 (4.49) | 531 (8.57) |
| Adenomatous
polyp | 52 (0.84) | 64 (1.03) | 116 (1.87) |
| Adenocarcinoma | 25 (0.40) | 10 (0.16) | 35 (0.56) |
| Juvenile polyp | 8 (0.13) | 12 (0.19) | 20 (0.32) |
| Squamous
hyperplasia | 50 (0.81) | 53 (0.86) | 103 (1.66) |
Discussion
GPs are usually detected endoscopically. It has been
reported that ~11% of gastric adenomatous polyps developed into
carcinoma in situ within 4 years of follow-up (10). After excision, the recurrence rate is
16% (6). At present, no precise and
relevant epidemiological data on GPs are available.
In the present study, the overall detection rate of
GPs was 3.75%, which is in accordance with the results of previous
studies (4–6). The patients were stratified into an
unsedated gastroscopy group and a sedated gastroscopy group. No
statistically significant difference in the procedure time was
present between these two groups, but a disproportion regarding
patient age was encountered. A lower proportion of patients aged
≥60 years underwent sedated gastroscopy, which may be attributed to
cautious anesthesia evaluation. Thus, the GP detection rate of
these two groups was standardized prior to statistical analysis.
The GP detection rate was higher in the sedated gastroscopy group
than that in the unsedated gastroscopy group, and the difference
was statistically significant, which implies that GPs may be more
easily detected under sedated gastroscopy. Furthermore, the present
study suggested that patients aged ≥20 years have a significantly
higher GP detection rate under sedated gastroscopy. In patients
aged <20 years, GPs were more often detected in the unsedated
gastroscopy group than in the sedated gastroscopy group, but the
difference was not statistically significant. This may be due to
the limited sample size.
The present study assessed and quantified the
location of the GPs, and the results indicated that the detection
rates of cardiac, gastric fundus, gastric body and multiple-site
GPs in the sedated gastroscopy group were statistically higher than
those in the unsedated gastroscopy group. The poorer diagnostic
performance of unsedated gastroscopy may be attributed to the
following: i) Patients always vomit when undergoing unsedated
gastroscopy, which causes shaking of the video screen; ii) vomiting
causes the gastric muscle to shrink, making it inconvenient for the
clinicians to observe each part of the gastral cavity, particularly
the side of the gastric body with the greater curvature, which has
numerous mucosal folds (Fig. 1);
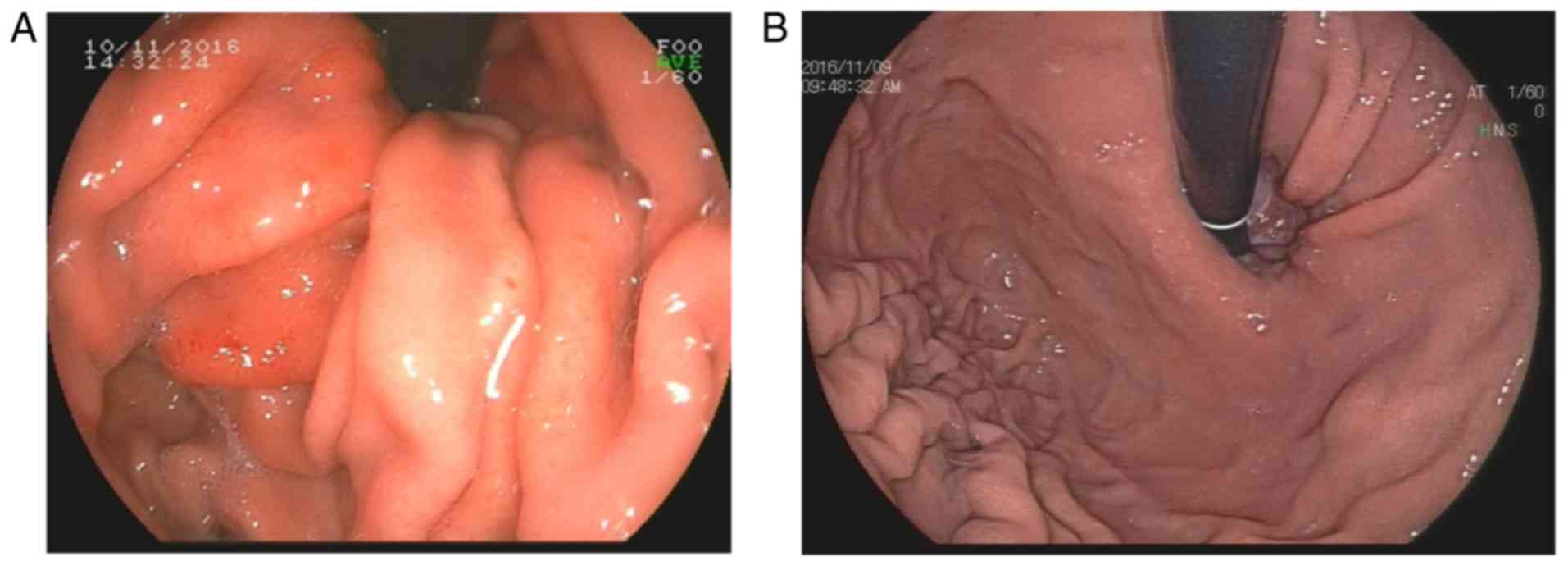
iii) drastic gastric muscle shrinking may cause mucosal hyperemia
and edema during unsedated gastroscopy within a short time, which
changes the base color of the gastric mucosa (Fig. 2). These factors may affect the
diagnosis of GPs.
In the present study, a slight difference in the
incidence of gastric angular polyps and gastric antrum polyps was
identified between the two groups, but with no statistically
significant difference. This is in accord with the actual
situation, as the gastric smooth muscles of the antrum do not
shrink as severely as those of the gastric body and are easier to
expand by gas injection. Furthermore, the limited sample size of
gastric angular polyps in the two groups may have affected the
statistical analysis. As the current study was a single-center
study, it was limited. Studies with larger samples sizes, may be
able to demonstrate that the GP detection rate can be improved by
sedated gastroscopy. More studies should be performed to further
confirm the diagnostic advantage of sedated gastroscopy.
A study has reported that the predilection site of
GPs was the gastric antrum (5). In
another study, the gastric body has been reported to be the most
common location (4). In the present
study, the most common predilection site of polyps in the two
groups was the gastric body. However, the second most common
predilection sites were the gastric antrum in the unsedated
gastroscopy group and the gastric fundus in the sedated gastroscopy
group. The third most common predilection sites were the gastric
fundus in the unsedated gastroscopy group and the gastric antrum in
the sedated gastroscopy group. Therefore, it is implied that
sedation not only makes patients comfortable during gastroscopy,
but it will also make it easier for doctors to observe the gastric
body and gastric fundus.
Various studies have reported on the common
pathologic types of GP. Evans et al (10) reported that the most common
pathologic type of GPs was the gastric fundus gland polyp, whereas
other studies reported inflammatory polyp or hyperplastic polyp to
be the most common pathologic types (5,11). The
present study indicated that the most common pathologic type of GPs
was gastric fundus gland polyp (52.27%), followed by hyperplastic
(34.74%) and inflammatory polyps (8.57%). Sections from biopsies of
the cardiac polyps were diagnosed as squamous epithelial
hyperplasia, which may be due to the proliferation and migration of
squamous epithelia to the cardiac site. Inaccurate positioning of
biopsy to contain parts of the esophageal mucosal epithelium maybe
another reason. Certain lesions were confirmed as adenomatous polyp
(1.87%), adenocarcinoma (0.56%), and juvenile polyp (0.32%), which
require polypectomy or surgical treatment as soon as possible.
In conclusion, the results of the present study
indicated that sedation enhances the diagnostic yield of GPs on
gastroscopy. Considering its low cost and convenient application in
South China, sedated gastroscopy is a better diagnostic option than
unsedated gastroscopy.
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
MJC and J-SW conceived and designed the study. WW,
SP, C-JL and L-MD were involved in the acquisition, analysis and
interpretation of data and drafting of the manuscript. Z-FC, J-SW
and Z-MH performed a critical revision of the manuscript and were
responsible for the intellectual content, statistical analysis,
supporting material and study supervision. The final version of the
manuscript has been read and approved by all authors, and each
author believes that the manuscript represents honest work.
Ethics approval and consent to
participate
Not required due to the retrospective nature of the
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nayudu SK, Niazi M, Balar B and Kumbum K:
A rare complication of hyperplastic gastric polyp. Case Rep
Gastrointest Med. 2013:6319752013.PubMed/NCBI
|
|
2
|
He HY, Shen ZB, Fang Y, Sun YH and Qin XY:
Bleeding and hyperpyrexia in an adult with gastric inflammatory
fibroid polyp. Chin Med J (Engl). 126:25942013.PubMed/NCBI
|
|
3
|
Vlacancich R, Sultan M and Al-Kawas F:
Gastric outlet obstruction caused by prolapsed gastric polyp into
the pyloric channel. Clin Gastroenterol Hepatol. 12:A27–A28. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fan NN, Yang J, Sun G, Lu ZS, Hu Ling EQ,
Wang XD and Yang YS: Changes in the spectrum of gastric polyps in
the Chinese population. World J Gastroenterol. 21:9758–9764. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cao H, Wang B, Zhang Z, Zhang H and Qu R:
Distribution trends of gastric polyps: An endoscopy database
analysis of 24 121 northern Chinese patients. J Gastroenterol
Hepatol. 27:1175–1180. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Carmack SW, Genta RM, Schuler CM and
Saboorian MH: The current spectrum of gastric polyps: A 1-year
national study of over 120,000 patients. Am J Gastroenterol.
104:1524–1532. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zheng E, Ni S, Yu Y, Wang Y, Weng X and
Zheng L: Impact of gender and age on the occurrence of gastric
polyps: Data analysis of 69575 southeastern Chinese patients. Turk
J Gastroenterol. 26:474–479. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Buyukasik K, Sevinc MM, Gunduz UR, Ari A,
Gurbulak B, Toros AB and Bektas H: Upper gastrointestinal tract
polyps: What do we know about them? Asian Pac J Cancer Prev.
16:2999–3001. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Standards of Practice Committee, .
Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S,
Dominitz JA, Fanelli RD, Gan SI, Harrison ME, et al: Sedation and
anesthesia in GI endoscopy. Gastrointest Endosc. 68:205–216. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
ASGE Standards of Practice Committee, .
Evans JA, Chandrasekhara V, Chathadi KV, Decker GA, Early DS,
Fisher DA, Foley K, Hwang JH, Jue TL, et al: The role of endoscopy
in the management of premalignant and malignant conditions of the
stomach. Gastrointest Endosc. 82:1–8. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin Y, Nie Y, Wang H, Li QQ and Li Y:
Analysis of clinical pathological characteristics and pattern
changes of 2643 gastric polyps in the past 15 years. Chin J Digest.
4:247–250. 2014.
|