Introduction
Diabetes mellitus (DM) is a common disorder of
glucose metabolism and a non-communicable chronic disease. DM is a
serious threat to human health after cardiovascular disease
(1). DM is currently one of the
global public health problems and shows an increasing trend year by
year. It is estimated that the number of diabetic patients in the
world will reach 500 million by 2030 (2). DM has a lot of complications, and
diabetic foot (DF) is one of the most serious ones. DF patients
suffer from inflammation and foot tissue damages caused by the
invasion of pathogenic microorganisms. Approximately 70% of DF
patients will have diabetic foot infection (DFI) (3). Many kinds of bacterial can infect DFI
patients, and Gram staining differentiate them into Gram-positive
(G+) and Gram-negative (G−) bacteria
(4). The clinical manifestations of
DFI are complex and the treatment cycle is long. In addition, the
unreasonable use of antimicrobial drugs, and the changes of
pathogens and drug resistance in recent years have complicated the
treatments and finally led to gangrene and increased amputation
rate (5). The distribution of
bacteria in DFI patients, the changes of their susceptibility to
antimicrobial drugs, and the clinical characteristics of DFI should
be studied to achieve better use of antimicrobial drugs, and to
provide a scientific basis for the prevention and rapid control of
DFI.
Materials and methods
General information
A retrospective analysis of 216 cases of DFI treated
at Xinxiang Central Hospital (Xinxiang, China) from 2013 to 2016
was conducted. The inclusion criteria included: i) Meeting the
diagnostic criteria of DF (6) and
ii) confirmation of bacterial infection by tissue culture of
specimen from the foot wound. The exclusion criteria included: i)
Liver and renal failure and ii) malignant tumor. All patients had a
history of drug use of the drugs covered by this study. The general
information of the patients was listed in Table I. The study was approved by the
Ethics Committee of Xinxiang Central Hospital and informed consents
were signed by the patients.
 | Table I.General patient data. |
Table I.
General patient data.
| Characteristics | Patients (n=216) |
|---|
| Sex, n (%) |
|
| Male | 101 (46.76) |
|
Female | 115 (53.24) |
| Age, years,
range | 30–78 |
| Mean age, years | 52.36±7.47 |
| BMI,
kg/m2 | 23.54±3.73 |
| Course of disease,
years, range | 1–25 |
| Average course of
disease, years | 11.48±5.36 |
| Fasting blood glucose
(mmol/l) (8 h) | 10.23±4.37 |
| Ulcer duration,
days | 51.73±8.75 |
| Diabetic Foot Wagner
Grading, n (%) |
|
| Level
0–2 | 31
(14.35) |
| Level 3
or higher | 185 (85.65) |
Methods
Sample collection and strain
identification
Patients' foot wound was cleaned with 0.9% sodium
chloride solution. A sterile cotton swab was used to collect
specimen from the base of the wound. Specimens from patients with
deep abscesses were collected by using a sterile syringe to get the
pus. The specimens were cultured in growth media (Oxoid
Corporation, Basingstoke, UK) and the bacterial strains were
identified using a VITEK 32 automated microbial analyzer
(BioMérieux, Craponne, France).
Susceptibility analysis
The cultured bacteria were classified and tested for
susceptibility by MH agar KB according to the National Committee
for Clinical Laboratory Standards (NCCLS). Bacteria were
immediately inoculated on blood agar plates and placed in a 37°C
incubator for 24 h. Bacterial identification was carried out using
a VITEK2 automatic bacterial analyzer (BioMérieux). Kirby-Bauer
disc diffusion method was used for drug susceptibility testing.
Escherichia coli ATCC35218A, TCC25922, Enterobacter
cloacae ATCC700323 and Klebsiella pneumoniae ATCC700603
were used as the quality controls for G− bacteria, while
Staphylococcus aureus ATCC29213 was the quality control for
G+ bacteria. All control strains were provided by
Nanjing Clinical Biotechnology Co., Ltd. Results between
sensitivity and drug resistance that emerged in this study were not
subjected to statistical analysis.
Observation indicators
Local clinical features of the patient, including
edema, defined as swelling of the lateral limbs and skin thickening
starting at the foot and ankle involving the entire lower
extremity, purulent secretions, defined as a thin pus overflow of
the affected foot, lower extremity pus and blood, defined as
pus-like material and blood from lower extremities, bone exposure
is defined as the presence of varying degrees of bone tissue
exposure in the foot, necrosis, defined as necrosis of skin of the
affected foot and the surrounding skin, malodorous smell, defined
as bad smell of secretion of the affected foot.
Statistical analysis
Epidata3.1 was used to do the data entry, and SPSS
19.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical
analysis. Count data were expressed as number or composition ratio.
Logistic regression analysis was conducted to study the impact of
different factors. P<0.05 was considered statistically
significant.
Results
Distribution of pathogens
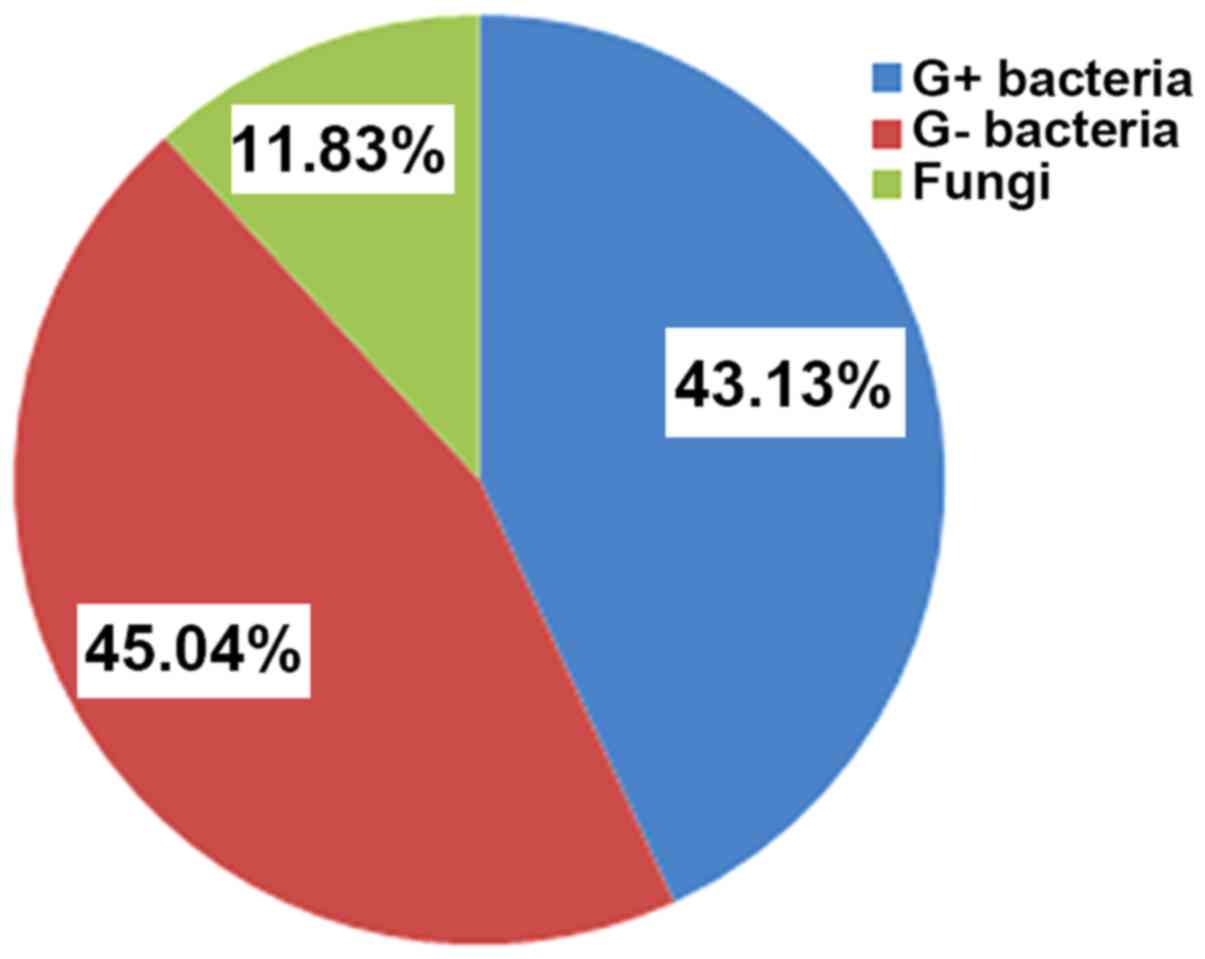
262 strains of pathogens were isolated from 216
patients with DFI, including 113 strains of G+ bacteria
(43.13%), 118 strains of G− bacteria (45.04%), and 31
strains of fungi (11.83%). The results were shown in Fig. 1.
Changes in drug susceptibility of
pathogenic bacteria
During 2013 to 2016, there was a gradual declining
trend about pathogenic bacteria susceptibility to conventional
antibacterial drug, but there was no statistically significant
difference among the different time points (P>0.05) (Table II).
 | Table II.Changes in drug susceptibilities of
pathogenic bacteria during 2013–2016. |
Table II.
Changes in drug susceptibilities of
pathogenic bacteria during 2013–2016.
|
| G+ bacteria, n
(%) | G−
bacteria, n (%) | Fungi, n (%) |
|---|
|
|
|
|
|
|---|
| Years | No. of identified
strains | Susceptibility | No. of identified
strains | Susceptibility | No. of identified
strains | Susceptibility |
|---|
| 2013 | 28 | 24 (85.71) | 29 | 25 (86.21) | 7 | 6 (85.71) |
| 2014 | 26 | 21 (80.77) | 27 | 21 (77.78) | 8 | 6 (75.00) |
| 2015 | 27 | 20 (74.07) | 28 | 20 (71.43) | 7 | 5 (71.43) |
| 2016 | 32 | 22 (68.75) | 34 | 23 (67.65) | 9 | 4 (44.44) |
Susceptibility of G+
bacteria to antibacterial drugs
G+ bacteria showed the highest
susceptibility to vancomycin and acetazolamide, while they had low
susceptibility to erythromycin, amoxicillin, norfloxacin and
penicillin (Table III).
 | Table III.Susceptibilities of G+ bacteria to
antibacterial drugs. |
Table III.
Susceptibilities of G+ bacteria to
antibacterial drugs.
|
|
Staphylococcus, n (%) (n=43) | Streptococcus,
n (%) (n=39) | Enterococcus,
n (%) (n=31) |
|---|
|
|
|
|
|
|---|
| Antibacterial
drugs | Resistance | Susceptibility | Resistance | Susceptibility | Resistance | Susceptibility |
|---|
| Erythromycin | 41 (95.35) | 2 (4.65) | 36 (92.31) | 1 (2.56) | 29 (93.55) | 1 (3.23) |
| Amoxicillin | 40 (93.02) | 3 (6.98) | 35 (89.74) | 2 (5.13) | 27 (87.10) | 2 (6.45) |
| Vancomycin | 6 (13.95) | 36 (83.72) | 3 (7.69) | 35 (89.74) | 3 (9.68) | 28 (90.32) |
| Acetazolamide | 5 (11.63) | 37 (86.05) | 2 (5.13) | 36 (92.31) | 2 (6.45) | 26 (83.87) |
| Norfloxacin | 37 (86.05) | 6 (13.95) | 34 (87.18) | 4 (10.26) | 28 (90.32) | 3 (9.68) |
| Penicillin | 35 (81.40) | 5 (11.63) | 31 (79.49) | 3 (7.69) | 26 (83.87) | 2 (6.45) |
Susceptibility of G−
bacteria to antibacterial drugs
G− bacteria showed high susceptibility to
dibekacin, panipenem and biapenem, and low susceptibility to
cefaclor, norfloxacin and erythromycin (Table IV).
 | Table IV.Susceptibilities of G−
bacteria to antibacterial drugs. |
Table IV.
Susceptibilities of G−
bacteria to antibacterial drugs.
|
| Proteus, n
(%) (n=45) | Escherichia
coli, n (%) (n=41) | Klebsiella
pneumoniae n (%) (n=32) |
|---|
|
|
|
|
|
|---|
| Antibacterial
drugs | Resistance | Susceptibility | Resistance | Susceptibility | Resistance | Susceptibility |
|---|
| Cefaclor | 41 (91.11) | 3 (6.67) | 40 (97.56) | 1 (2.44) | 29 (90.63) | 1 (3.13) |
| Dibekacin | 7 (15.56) | 35 (77.78) | 5 (12.20) | 32 (78.05) | 2 (6.25) | 29 (90.63) |
| Biapenem | 6 (13.33) | 37 (82.22) | 3 (7.32) | 37 (90.24) | 3 (9.38) | 28 (87.50) |
| Panipenem | 5 (11.11) | 38 (84.44) | 4 (9.76) | 36 (87.80) | 2 (6.25) | 26 (81.25) |
| Norfloxacin | 40 (88.89) | 5 (11.11) | 37 (90.24) | 2 (4.88) | 28 (87.50) | 2 (6.25) |
| Erythromycin | 38 (84.44) | 7 (15.56) | 35 (85.37) | 3 (7.32) | 29 (90.63) | 1 (3.13) |
Clinical symptoms of patients
The top three local clinical symptoms of the 216
patients were edema (98.61%), purulent secretions (62.96%), and
lower extremity sepsis (58.80%) (Table
V).
 | Table V.Clinical symptoms of patients. |
Table V.
Clinical symptoms of patients.
| Clinical
symptoms | No. of
patients | % |
|---|
| Edema | 213 | 98.61 |
| Purulent
secretions | 136 | 62.96 |
| Lower extremity
sepsis | 127 | 58.80 |
| Exposure of
bones | 76 | 35.19 |
| Necrosis | 61 | 28.24 |
| Stinky smell | 54 | 25.00 |
Complications of the patients
The top three complications were: Lower extremity
vascular disease (58.80%), peripheral neuropathy (39.81%), and
kidney disease (17.13%) (Table
VI).
 | Table VI.Complications in patients. |
Table VI.
Complications in patients.
| Complications | No. of
patients | % |
|---|
| Lower extremity
vascular disease | 127 | 58.80 |
| Peripheral
neuropathy | 86 | 39.81 |
| Kidney disease | 37 | 17.13 |
| Hyperlipidemia | 36 | 16.67 |
| Retinopathy | 29 | 13.43 |
Analysis of factors affecting drug
resistance in patients with DFI
For the analysis, the presence of drug resistance
was used as the dependent variable, and patient age,
hospitalization frequency, previous use of antibacterial drugs,
combination with osteomyelitis, application of third-generation
cephalosporins and the presence of more than three ulcers, were
used as the independent variables. The results showed that age
(OR=2.708, P=0.005), previous use of antibacterial drugs (OR=3.816,
P=0.007), application of the third-generation cephalosporins
(OR=3.014, P=0.008) were the independent risk factors for the
resistance in patients with DFI (P<0.05) (Table VII).
 | Table VII.Logistic regression analysis of the
factors affecting the drug resistance in DFI patients. |
Table VII.
Logistic regression analysis of the
factors affecting the drug resistance in DFI patients.
| Factors | β | SE | Wald | OR | 95% CI | P-value |
|---|
| Age | 0.618 | 0.673 | 6.424 | 2.708 | 1.106–3.854 | 0.005 |
| Hospitalization
frequency | 0.362 | 0.435 | 4.126 | 0.619 | 0.493–0.874 | 0.316 |
| Combination with
osteomyelitis | 0.615 | 0.314 | 3.427 | 0.716 | 0.496–0.862 | 0.218 |
| Previous use of
antibacterial drugs | 0.563 | 0.606 | 7.703 | 3.816 | 1.075–4.712 | 0.007 |
| Application of the
third-generation cephalosporins | 0.617 | 0.518 | 5.568 | 3.014 | 1.103–4.046 | 0.008 |
| More than three
ulcers | 0.456 | 0.412 | 3.713 | 0.753 | 0.275–0.916 | 0.356 |
Discussion
DM usually occurs in elderly patients. These
patients have other diseases and low immunities. In addition, they
suffer long-term inadequate local blood supply because of blood
glucose control and vascular diseases such as atherosclerosis.
Thus, DFI has a high incidence in elderly DM patients (7). Under the influence of long-term
hyperglycemia, patients have metabolic disorders and impaired
immune systems. Weak immune system results in reduced chemotaxis,
adhesion and phagocytosis of monocytes and neutrophils, which
cannot resist the invasion of pathogens. In addition, the high
levels of sugar and proteins in the exudates from foot wounds
create a good environment for the survival and reproduction of
bacteria, and thus can easily lead to the occurrence of infections
(8). Wound repair in DFI patients is
a complex physiological process. Patients usually have serious
tissue damage and long courses of disease. Their wounds are
difficult to heal and prone to drug resistance, and the prognosis
is poor (9).
DFI is caused by a lot of pathogens. According to a
relevant statistics (10),
G+ bacteria and G− bacteria can be detected
in DFI. The results of this study showed that G+
bacteria accounted for 43.13%, G− bacteria accounted for
45.04%, while others accounted for 11.83% of the pathogens. The
majority was G+ and G− bacteria. Among the
detected G+ bacteria were Staphylococcus,
Streptococcus and Enterococcus. Staphylococci is
named after the fact that they look like clusters of grapes.
Staphylococcus epidermidis, Staphylococcus aureus, and
Staphylococcus saprophyticus can cause suppurative
inflammation in DFI patients (11).
Streptococcus are usually <2 µm in diameter, ovoid or
spheroidal in appearance and has a chain-like appearance. They have
a strong invasiveness and can produce a variety of exotoxins, which
can aggravate the degree of infection in patients (12). Enterococcus are a group of
intestine-dwelling bacteria in the shape of oval or spherical. They
appear in short chains or pairs in liquid media and they do not
produce spores. They are a group of important infectious pathogens
(13). The G− bacteria
detected in this experiment mainly included Proteus, Escherichia
coli and Klebsiella pneumoniae. Proteus are also
called Bacillus. They are secondary infectious bacteria and
are usually detected in the late phase of DFI. They cause corrosive
tissue damage (14). Escherichia
coli is a single-cell bacterium that lives in human intestine
and is essential for human body (15). Klebsiella pneumoniae is one of
the important infectious pathogens, especially in the
immunocompromised population. It can lead to infections such as
urinary tract infection, pneumonia and bacteremia with high
mortality rate (16).
Clinically, DFI patients are often given
broad-spectrum antibacterial drugs to kill bacteria and control
infections (17). In clinical
practice, antibacterial drugs need to be changed and patients
usually need long-term use of a variety of drugs, especially those
high-level antimicrobial drugs, resulting in increased drug
resistance in patients. When bacteria invade into host cells,
antibacterial drugs cannot effectively enter the cells. The
compromised anti-infection effects result in delayed wound healing
and cause great suffering in patients (18). The results of this study showed that
the susceptibility of pathogens to conventional antibacterial drugs
have declined year by year from 2013 to 2016, which was closely
related to the unreasonable use of antibacterial drugs. In this
study, we found that G+ bacteria had high susceptibility
to vancomycin and acetazolamide, while G− bacteria were
sensitive to dibekacin, panipenem and biapenem. These results
indicated that drugs with low susceptibility should be avoided in
the clinical treatment for G+ bacteria-infected DFI
patients, while vancomycin and acetazolamide should be chosen.
Similarly, the third-generation cephalosporins should not be
prescribed for G− bacteria-infected DFI patients. The
fourth-generation cephalosporins, dibekacin, panipenem and biapenem
should be recommended. The use of drugs with high bacteria
susceptibility can effectively control infections and avoid
gangrene wounds.
DFI patients generally have low anti-infection
abilities. Their clinical syndromes are obvious and mainly
manifested as edema, purulent discharge, and lower extremity
sepsis. Some patients also suffer bone exposure and necrosis
(19). The long-term high blood
sugar can easily lead to various complications, including lower
extremity vascular disease (58.80%), peripheral neuropathy (39.81%)
and kidney disease (26.39%). Lower extremity vascular disease is
mainly because patients have low resistance to infections and
persistent hyperglycemia can lead to metabolic disorders. Patients'
limbs are vulnerable to bacterial invasion, resulting in damage to
the endothelial cells on the arterial wall of the lower
extremities, causing vascular endothelial dysfunction (20). In addition, the long-term
dyslipidemia and other metabolic disorders impair the sympathetic
and parasympathetic systems, triggering peripheral neuropathy
(21). Continued inflammation in DFI
patients also causes increased blood pressure, which in turn can
impair renal function (22).
This study showed that age, previous use of
antibacterial drugs and use of third-generation cephalosporins were
independent risk factors for drug resistance in DFI patients
(P<0.05). This is because autoimmune ability decreases as
patients' age increases. Their high glucose toxicity and oxidative
stress can lead to changes in the expression of autophagy genes.
The weakened autophagic function of the host cells makes it easier
for bacteria but harder for antibacterial drugs to enter the cells,
thereby increasing drug resistance (23). Because of lack of proper knowledge,
the inappropriate use of third-generation cephalosporins and heavy
use of antibacterial drugs in the past have led to a significant
increase in drug-resistant pathogens.
In conclusion, DFI patients with bacterial infection
mainly have G+ and G− bacteria. Their
susceptibility to commonly used antibacterial drugs declines year
by year. Proper clinical treatment of DFI needs to standardize the
use of antibacterial drugs with drug susceptibility testing, so as
to improve clinical symptoms and control of DFI.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and material
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LL wrote the manuscript. LL and ZL were responsible
for patient susceptibility analysis. XiL and SG recorded and
analyzed results. LG and XuL performed statistical analysis. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Xinxiang Central Hospital (Xinxiang, China) and informed consents
were signed by the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ismail H, Omar MA, Hisham AAN, Aris T,
Ambak R, Yusoff MFM and Lim KK: Undiagnosed type 2 diabetes
mellitus and its risk factors among malaysians: Findings of a
nationwide study. Int J Public Health. 6:677–684. 2016.
|
|
2
|
D'Emden MC, Shaw JE, Jones GR and Cheung
NW: Guidance concerning the use of glycated haemoglobin (HbA1c) for
the diagnosis of diabetes mellitus. Med J Aust. 203:89–90. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Al-Rubeaan K, Al Derwish M, Ouizi S,
Youssef AM, Subhani SN, Ibrahim HM and Alamri BN: Diabetic foot
complications and their risk factors from a large retrospective
cohort study. PLoS One. 10:e01244462015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yusuf N, Omar MI, Zakaria A, Masnan MJ,
Abdullah AA, Kamarudin LM, Shakaff AYM, Thriumani R, Yeap EJ,
Othman A and Yasin MS: Rapid bacteria identification using
multivariate classifier on diabetic foot infection. J Med Imag
Health In. 5:1251–1254. 2015.
|
|
5
|
Dorresteijn JA, Kriegsman DM and Valk GD:
Complex interventions for preventing diabetic foot ulceration.
Cochrane Database Syst Rev. Jan 19–2010.(Epub ahead of print). doi:
10.1002/14651858.CD007610.pub2. View Article : Google Scholar
|
|
6
|
Klenerman L, McCabe C, Cogley D, Crerand
S, Laing P and White M: Screening for patients at risk of diabetic
foot ulceration in a general diabetic outpatient clinic. Diabet
Med. 13:561–563. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lavigne JP, Sotto A, Dunyach-Remy C and
Lipsky BA: New molecular techniques to study the skin microbiota of
diabetic foot ulcers. Adv Wound Care (New Rochelle). 4:38–49. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hingorani A, Lamuraglia GM, Henke P,
Meissner MH, Loretz L, Zinszer KM, Driver VR, Frykberg R, Carman
TL, Marston W, et al: The management of diabetic foot: A clinical
practice guideline by the Society for Vascular Surgery in
collaboration with the American Podiatric Medical Association and
the Society for Vascular Medicine. J Vasc Surg. 63 Suppl 2:3S–21S.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pickwell K, Siersma V, Kars M, Apelqvist
J, Bakker K, Edmonds M, Holstein P, Jirkovská A, Jude E, Mauricio
D, et al: Predictors of lower-extremity amputation in patients with
an infected diabetic foot ulcer. Diabetes Care. 38:852–857. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stappers MHT, Hagen F, Reimnitz P, Mouton
JW, Meis JF and Gyssens IC: Direct molecular versus culture-based
assessment of Gram-positive cocci in biopsies of patients with
major abscesses and diabetic foot infections. Eur J Clin Microbiol
Infect Dis. 34:1885–1892. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Messad N, Prajsnar TK, Lina G, O'Callaghan
D, Foster SJ, Renshaw SA, Skaar EP, Bes M, Dunyach-Remy C,
Vandenesch F, et al: Existence of a colonizing staphylococcus
aureus strain isolated in diabetic foot ulcers. Diabetes.
64:2991–2995. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Katz DE, Friedman ND, Ostrovski E, Ravid
D, Amrami N, Avivi D, Mengesha B, Zaidenstein R, Lazarovitch T,
Dadon M and Marchaim D: Diabetic foot infection in hospitalized
adults. J Infect Chemother. 22:167–173. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Reghu R, Padma UD, Sasankan V, Puthur S
and Jose J: A microbiological study of diabetic foot ulcer in a
south Indian tertiary care hospital. Int J Pharm Sci. 37:167–170.
2016.
|
|
14
|
Shin NR, Whon TW and Bae JW:
Proteobacteria: Microbial signature of dysbiosis in gut microbiota.
Trends Biotechnol. 33:496–503. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Otsuji N, Sekiguchi M, Iijima T and Takagi
Y: Induction of phage formation in the lysogenic Escherichia coli
K-12 by mitomycin C. Nature. 184:1079–1080. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pitout JD, Nordmann P and Poirel L:
Carbapenemase-producing klebsiella pneumoniae, a key pathogen set
for global nosocomial dominance. Antimicrob Agents Chemother.
59:5873–5884. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alexandrescu VA, Hubermont G, Philips Y,
Guillaumie B, Ngongang C, Vandenbossche P, Azdad K, Ledent G and
Horion J: Selective primary angioplasty following an angiosome
model of reperfusion in the treatment of Wagner 1–4 diabetic foot
lesions: Practice in a multidisciplinary diabetic limb service. J
Endovasc Ther. 15:580–593. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Serra R, Grande R, Scarcello E, Buffone G
and de Franciscis S: Angiosome-targeted revascularisation in
diabetic foot ulcers. Int Wound J. 12:555–558. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sutton M, McGrath C, Brady L and Ward J:
Diabetic foot care: Assessing the impact of care on the whole
patient. Prac Diabetes. 17:147–151. 2000. View Article : Google Scholar
|
|
20
|
Sun P, Guo J and Xu N: Correlation between
diabetic lower-extremity arterial disease and diabetic neuropathy
in patients with type II diabetes: An exploratory study. Int J Clin
Exp Med. 8:1396–1400. 2015.PubMed/NCBI
|
|
21
|
Selvarajah D, Cash T, Davies J, Sankar A,
Rao G, Grieg M, Pallai S, Gandhi R, Wilkinson ID and Tesfaye S:
SUDOSCAN: A simple, rapid, and objective method with potential for
screening for diabetic peripheral neuropathy. PLoS One.
10:e01382242015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Muthuppalaniappan VM, Sheaff M and Yaqoob
MM: Diabetic nephropathy. Medicine. 43:520–525. 2015. View Article : Google Scholar
|
|
23
|
Amin N and Doupis J: Diabetic foot
disease: From the evaluation of the ‘foot at risk’ to the novel
diabetic ulcer treatment modalities. World J Diabetes. 7:153–164.
2016. View Article : Google Scholar : PubMed/NCBI
|