Introduction
Mild encephalitis/encephalopathy with a reversible
splenial lesion (MERS) is a type of acute encephalitic
encephalopathy as reported by Tada et al (1). The characteristic magnetic resonance
imaging (MRI) findings of MERS include reversible lesions of the
splenium of the corpus callosum that resolved spontaneously within
one week in most cases (2). In
recent years, diffusion weighted images (DWIs) of MRI have become
widespread, and reports have increased on incidences of MERS
related to various conditions. The clinical course of MERS is
generally mild, when compared to other types of acute
encephalopathy, and it depends on the severity of the subjacent
condition. The pathogenesis of MERS has been known to involve a
variety of different mechanisms and includes cases associated with
the use of anti-epileptic drugs (3,4), cases
accompanying acute mountain sickness (5), and others associated to microbial
infections (mycoplasma (6),
legionella (7), dengue fever
(8), rubella (9), rotavirus (10), HHV-6 (11), Influenza virus type A (12), and others). Thus, MERS is recognized
as a unique clinico-radiological encephalitis/encephalopathy
syndrome associated with diverse pathological conditions. However,
to the best of our knowledge, this is the first instance wherein
bacterial translocation has been implicated as a causative
mechanism. Herein, we report the case of a 9-year-old girl who had
complicated esophageal varices due to congenital portal vein
hypoplasia and developed a bacterial infection with abdominal pain
and neurological abnormalities that led to a diagnosis of MERS.
Case report
Our pediatric patient was born following a normal
delivery at 37 weeks of gestation. Her birth height was 43.3 cm and
her weight was 2,090 g. There were no delays in motor development
and the girl started walking at the age of 1. No family history of
major diseases was reported.
One year after her birth, the girl was reported to
suffer from frequent epistaxis episodes. Medical examinations
performed at the local hospital showed she had thrombocytopenia and
splenomegaly. She was referred to our university hospital at the
age of 1 year and 3 months; X-ray images showed evidence of an
expansion of the mediastinum, which led us to suspect the presence
of a mediastinal tumor. A chest computed tomography (CT) scan
revealed a low-density area in the hepatic portal section, and a
tentative diagnosis of portal hypertension was made. After that,
the patient underwent abdominal ultrasound and contrast CT
examinations, and abnormalities of the portal vein running through
the liver were recognized. Multiple esophageal varices were also
confirmed by upper gastrointestinal contrast radiographic images.
Overall, the patient was diagnosed as having idiopathic portal
hypertension caused by congenital portal hypoplasia.
At 3 years of age, contrast CT examination showed
exacerbation of the esophageal varices from the lower portion of
the esophagus to the cardia of the stomach. The portal vein was
undergoing a cavernous transformation from the splenoportal
junction. The images revealed a splenic vein aneurysm.
Additionally, the left kidney was atrophic due to the progressing
splenomegaly. Therefore, a pediatric surgeon performed an
endoscopic variceal ligation (EVL) surgery at multiple sites that
were deemed as prone to bleeding.
A second EVL surgery for recurrent esophageal
varices was performed under general anesthesia when the patient was
6 years and 8 months. The day after the EVL surgery, the girl
experienced a sudden high fever (>40°C). Paralysis of the
intestinal tract due to general anesthesia and the existing portal
vein hypoplasia were suspected as resulting in secondary bacterial
translocation and sepsis. The blood culture test collected from the
elbow vein produced a negative result. An attempt to obtain blood
directly from the portal vein proved impossible. Nevertheless, a
course of antibiotics and gamma globulin therapy were promptly
administered and the infectious symptoms subsided.
Later, at the age of 9 years and 6 months, the
patient underwent a third EVL surgery under general anesthesia once
again for esophageal varices. This time, cephem antibiotics
(ceftriaxone sodium hydrate; CTRX) were prescribed prophylactically
and immediately after the surgical procedure. Nevertheless, the
next day after the EVL surgery, the girl developed a 40°C fever.
She was hospitalized in the city hospital but her consciousness
level reduced by the evening of the same day. Thus, she was
transferred to our university hospital. Blood examinations showed
the following values: White blood cells 3,200×109/l,
hemoglobin 10.4 g/dl, Plt 2.3×104/µl, sodium 130 mEq/l,
CRP 7.39 mg/dl, and procalcitonin 26.34 ng/ml. Sepsis and acute
encephalopathy due to bacterial translocation after the EVL surgery
were suspected. The cell count of cerebral spinal fluid collection
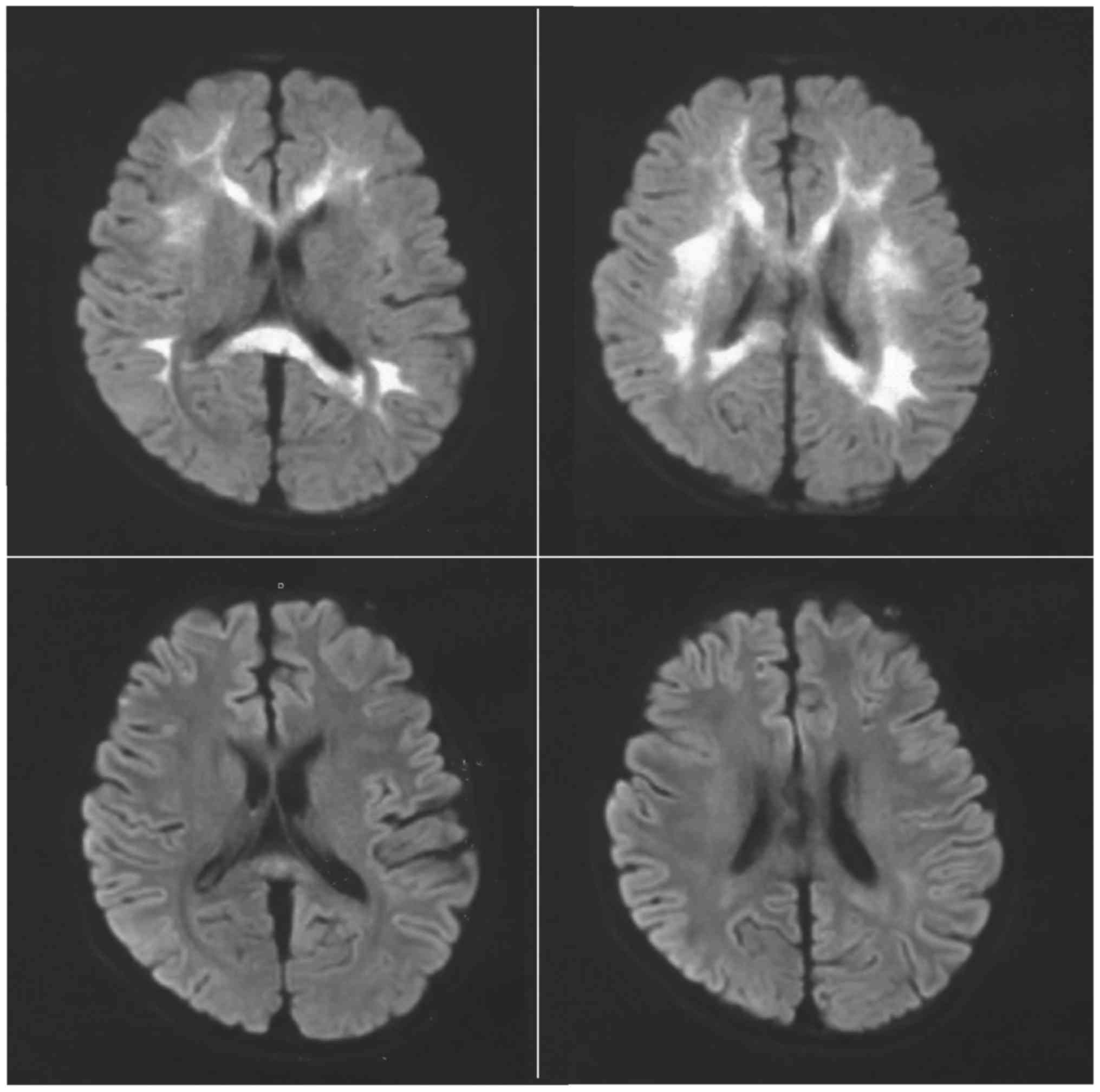
was 42/µl. A head CT showed no remarkable changes. Her MRI images,
nonetheless, revealed abnormal signal intensities mainly at the
splenium of the corpus callosum and both sides of white matter
using contrast (Fig. 1). So the
patient was diagnosed as having a MERS type 2, which was probably
precipitated by bacterial translocation. The antibiotic treatment
with CTRX was switched to penem (panipenem; PAPM/BP) and 5 days of
gamma globulin therapy with 3 days of steroid pulse treatment.
After 24 h of the last treatment dosage, the fever prevailed but at
a lower temperature. On the second day after the aforementioned
treatments, DWIs of MRI showed marked improvement (Fig. 1), a finding that was in agreement
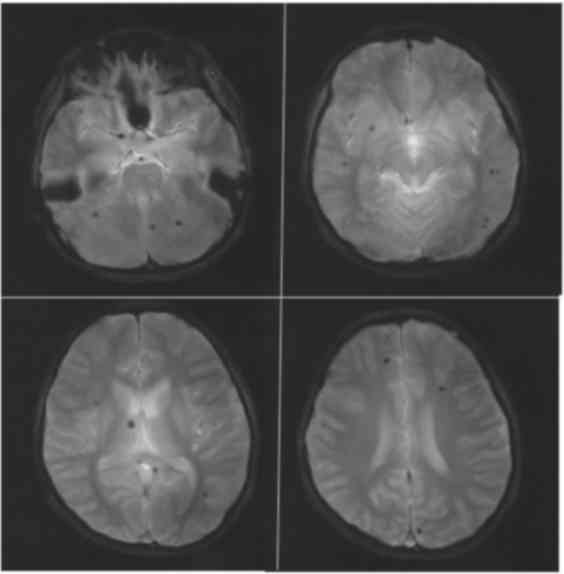
with the typical course of MERS. Nevertheless, many abnormal spots
suspected to be due to micro-bleeding were apparent (Fig. 2). On the third day after the
treatment, her neurological symptoms and fever had completely
disappeared. Regarding the publication of this case report, the
patient's parents consented in advance to the formal form prepared
by the Ethics Organization Committee of Dokkyo Medical University
Hospital (Tochigi, Japan).
Discussion
The clinical course of this pediatric case is very
interesting. Initially, the patient manifested symptoms of portal
hypertension due to congenital portal defects. Between infancy and
childhood, formation of a collateral circulation pathway to
compensate for portal vein deficits was observed, complicating the
situation with dangerous esophageal varices from the left gastric
vein. In addition, pancytopenia accompanied by marked reduction of
platelet cells was observed as a result of spleen hyperfunction.
Under such circumstances, any gastroenteritis is likely to bring
bacteria and toxic substances from the intestinal tract directly
into the general circulation system, which can lead to septicemia
and encephalopathy from the translocated bacteria. On the other
hand, in cases where bacterial translocation is suspected and in
cases where antibiotics are already being administered, the
causative bacteria are rarely detected.
In the course of our case, fever and abdominal pain,
seen as symptoms of gastroenteritis, evolved to develop
neurological speech disturbances with altered consciousness. An
emergency MRI then led to the diagnosis of MERS. The clinical
course of MERS has been previously reported to include a febrile
state with alterations of speech and consciousness (13). These symptoms are considered part of
febrile derilium (14). However, the
fever in our patient was more consistent, one having an infectious
origin due to its onset timing and the results of the initial blood
tests at hospitalization, which were consistent with a septicemia.
The possibility of disseminated intravascular coagulation (DIC)
syndrome was difficult to rule out in our patient due to the
impossibility of distinguishing it from the original low platelet
counts and pancytopenia from the underlying spleen hyperactivity.
The treatment chosen for the patient included antibiotics and gamma
globulin therapy and steroid pulses for MERS with sepsis and
possible DIC syndrome. The diagnosis of MERS was further confirmed
by the fast improvement of splenial abnormalities on the MRI
re-examination after 2 days of treatment. And the efficacy of the
administered treatment was clear with a complete resolution of the
patient's symptoms 3 days after treatment.
Bacterial translocation occurs when abnormal
proliferation of intestinal bacteria coupled with impairment of the
intestinal mucosa defense function leads to an extremely serious
systemic infection. In those instances, intestinal bacteria
penetrate the broken barrier of intestinal mucosal epithelium and
migrate to the whole body via blood and lymph flow. Such cases
generally ensue on fasting patients with acute gastroenteritis or
some kind of intestinal chronic disease that leads to abnormally
slow intestinal flow, accumulation of bacteria, and altered defense
function of the intestinal mucosa. In our patient, portal
hypertension and slowed intestinal tract movements due to
anesthesia probably led to edema of the intestinal mucosa and
deterioration of the lymphatic vessel flow, which together allowed
the translocation of intestinal bacteria that ultimately reached
the central nervous system. Recent advances in the pathogenesis
mechanisms of bacterial translocation point to the effects of
direct invasion of bacterial cells throughout the body as well as
severe inflammatory reactions caused by inflammatory cytokines
released during phagocytosis in the broken intestinal mucosa. As
such, there have been reports of MERS from bacteremia with toxic
shock syndrome (15), and MERS
associated with acute focal bacterial nephritis caused by
Enterococcus faecalis related to marked elevation of
interleukin 6 (16). Our case of
MERS is also related to bacterial infection triggered by bacterial
translocation, which caused symptoms of bacteremia or sepsis and
acute encephalopathy.
The clinical course of MERS varies among patients,
and a clear mechanism of onset has not yet been elucidated.
Nevertheless, it is interesting to note that severe bacterial
infections due to bacterial translocation may be at play in the
multiple cases of MERS in childhood associated with viral
infections that run a clinical course similar to the one described
here. We believe that our report represents a model case of
bacterial translocation leading to MERS.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GI, TY, JI, KOg, KOk and TT designed the study and
drafted the manuscript. GI, JI and SY collected the clinical and
imaging data and analyzed the serological data. TY, Kog, Kok and TT
operated and collected surgical and anatomical information of the
patient. SY collected information on the medical history of the
patient, interpreted blood test data and decided the fluid therapy
treatment. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Regarding the publication of this case report, the
patient's parents consented in advance to the formal form prepared
by the Ethics Organization Committee of Dokkyo Medical University
Hospital (Tochigi, Japan).
Patient consent for publication
Consent was obtained from the parents of the patient
for publication of data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tada H, Takanashi J, Barkovich AJ, Oba H,
Maeda M, Tsukahara H, Suzuki M, Yamamoto T, Shimono T, Ichiyama T,
et al: Clinically mild encephalitis/encephalopathy with a
reversible splenial lesion. Neurology. 63:1854–1858. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Takanashi J, Hirasawa K and Tada H:
Reversible restricted diffusion of entire corpus callosum. J Neurol
Sci. 247:101–104. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim SS, Chang KH, Kim ST, Suh DC, Cheon
JE, Jeong SW, Han MH and Lee SK: Focal lesion in the splenium of
the corpus callosum in epileptic patients: Antiepileptic drug
toxicity? AJNR Am J Neuroradiol. 20:125–129. 1999.PubMed/NCBI
|
|
4
|
Maeda M, Shiroyama T, Tsukahara H, Shimono
T, Aoki S and Takeda K: Transient splenial lesion of the corpus
callosum associated with antiepileptic drugs: Evaluation by
diffusion-weighted MR imaging. Eur Radiol. 13:1902–1906. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kallenberg K, Bailey DM, Christ S, Mohr A,
Roukens R, Menold E, Steiner T, Bärtsch P and Knauth M: Magnetic
resonance imaging evidence of cytotoxic cerebral edema in acute
mountain sickness. J Cereb Blood Flow Metab. 27:1064–1071. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yuan ZF, Shen J, Mao SS, Yu YL, Xu L,
Jiang PF, Gao F and Xia ZZ: Clinically mild
encephalitis/encephalopathy with a reversible splenial lesion
associated with Mycoplasma pneumoniae infection. BMC Infect Dis.
16:2302016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tomizawa Y, Hoshino Y, Sasaki F, Kurita N,
Kawajiri S, Noda K, Hattori N, Amemura-Maekawa J, Kura F and Okuma
Y: Diagnostic utility of splenial lesions in a case of
legionnaires' disease due to legionella pneumophila serogroup 2.
Intern Med. 54:3079–3082. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Saito N, Kitashouji E, Kojiro M, Furumoto
A, Morimoto K, Morita K and Ariyoshi K: A case of clinically mild
encephalitis/encephalopathy with a reversible splenial lesion due
to dengue fever. Kansenshogaku Zasshi. 89:465–469. 2015.(In
Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jinnai A, Kikuchi T, Ishikawa M, Nishimura
Y, Shibata K and Sakura H: A case of rubella encephalitis
presenting as clinically mild encephalitis/encephalopathy with a
reversible splenial lesion. Rinsho Shinkeigaku. 54:668–670.
2014.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kobata R, Tsukahara H, Nakai A, Tanizawa
A, Ishimori Y, Kawamura Y, Ushijima H and Mayumi M: Transient MR
signal changes in the splenium of the corpus callosum in rotavirus
encephalopathy: Value of diffusion-weighted imaging. J Comput
Assist Tomogr. 26:825–828. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hatanaka M, Kashiwagi M, Tanabe T,
Nakahara H, Ohta K and Tamai H: Overlapping MERS and mild AESD
caused by HHV-6 infection. Brain Dev. 37:334–338. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Takanashi J, Tada H, Kuroki H and
Barkovich AJ: Delirious behavior in influenza is associated with a
reversible splenial lesion. Brain Dev. 31:423–426. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hoshino A, Saitoh M, Oka A, Okumura A,
Kubota M, Saito Y, Takanashi J, Hirose S, Yamagata T, Yamanouchi H
and Mizuguchi M: Epidemiology of acute encephalopathy in Japan,
with emphasis on the association of viruses and syndromes. Brain
Dev. 34:337–343. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takanashi J, Takahashi Y, Imamura A,
Kodama K, Watanabe A, Tominaga K, Muramatsu K and Barkovich AJ:
Late delirious behavior with 2009 H1N1 influenza: Mild
autoimmune-mediated encephalitis? Pediatrics. 129:e1068–e1071.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kosami K, Kenzaka T, Sagara Y, Minami K
and Matsumura M: Clinically mild encephalitis/encephalopathy with a
reversible splenial lesion caused by methicillin-sensitive
Staphylococcus aureus bacteremia with toxic shock syndrome: A case
report. BMC Infect Dis. 16:1602016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kometani K, Kawatani M, Ohta G, Okazaki S,
Ogura K, Yasutomi M, Tanizawa A and Ohshima Y: Marked elevation of
interleukin 6 in mild encephalopathy with a reversible splenial
lesion (MERS) associated with acute forcal bacterial nephritis
caused by Enterococcus faecalis. Brain Dev. 36:551–553.
2014. View Article : Google Scholar : PubMed/NCBI
|