Introduction
Acute myocardial infarction (AMI) is a leading cause
of mortality and morbidity in the world, despite the rates having
significantly declined over the past decade (1). Numerous risk factors, including age,
sex, social deprivation, smoking, use of anti-hypertensives or
lipid-lowering drugs and diabetes mellitus, are associated with
myocardial infarction (2–4). In the clinic, the treatment of AMI
includes blood transfusion and a previous study has reviewed the
risks and benefits of thrombolytic, anti-platelet and
anti-coagulant therapies for myocardial infarction (5). In recent years, early diagnosis of
myocardial infarction has been widely applied for patients with
recent myocardial infarction or suspected or known coronary artery
disease (6).
At present, ultrasound, positron emission tomography
(PET) with fludeoxyglucose (FDG)/computed tomography and MRI are
widely used for the diagnosis and staging of human cardiovascular
diseases (7–9). Among these diagnostic methods, MRI
provides a higher sensitivity and accuracy in the diagnosis of
myocardial infarction in the clinic (10,11). The
clinical utility of cardiac MRI in patients with myocardial
infarction has a high reproducibility and accuracy, allowing for
detailed functional assessment and characterization of myocardial
tissue determined by infarct size (IS), transmural extent of
necrosis (TEN) and microvascular obstruction (MVO) (12). A previous study also reported that
simultaneous assessment of late gadolinium enhancement (LGE) and
FDG uptake using a hybrid PET/MRI system is feasible, which
accurately predicted the regional outcome of wall motion after AMI
(13). In addition, although
numerous studies have reported on the diagnosis of myocardial
infarction by using MRI (14,15), the
diagnostic accuracy of MRI in diagnosing patients with early-stage
myocardial infarction requires to be improved.
In the present study, a novel contrast agent,
chitosan/Fe3O4-enclosed albumin (CFEA), was
introduced and the efficacy of MRI with CFEA (MRI-CFEA) in the
diagnosis of patients with early-stage myocardial infarction was
assessed. The results indicated that MRI-CFEA not only improved the
signal intensity in the localized area of the myocardial
infarction, but also enhanced the diagnostic efficacy of MRI in the
diagnosis of clinical patients with suspected myocardial
infarction.
Materials and methods
Ethics statement
The present clinical trial was performed in strict
accordance with the recommendations for clinical study in China
(approval number, 20140521TJ) (16).
The present study was also approved by the Ethics Committee of
Tongji Medical College (Wuhan, China). Written informed consent was
obtained from all patients or their relatives prior to their
inclusion within the study.
Targeted contrast agent
The CFEA nano-size contrast agent was used for the
diagnosis of patients with suspected early-stage myocardial
infarction as previously described (17). Nano-size CFEA was produced using a
covalent bond with albumin as previously described (18). The CFEA was administrated by
intravenous injection. The nano-particle contrast agent to be
visualized by the MRI system was administered by intravenous
injection at 30 min prior to MRI.
Patients
A total of 68 patients (males, n=36; females, n=32)
with suspected myocardial infarction were enrolled in the present
study. In addition, 32 healthy individuals (males, n=15; females,
n=9) were enrolled in the present study. The mean age was 45.6 and
42.8 years in patients with suspected myocardial infarction and
healthy individuals, respectively. The present study included 68
patients consecutively registered between January 2015 and May 2016
at Tongji Medical College (Wuhan, China) with suspected myocardial
infarction who wished to be included in the study. A total of 32
healthy individuals were recruited between January 2015 and May
2016 following a routine health check. All patients with suspected
myocardial infarction were subjected to MRI scanning for the
detection of early-stage myocardial infarction using conventional
LGE-cardiovascular magnetic resonance (MRI) and MRI-CFEA. Patients
with chest pain (which was rated using the rapid emergency medical
scoring system (19)) and/or
abnormities in the electrocardiograph and heart color ultrasound
were included in the present study. Patients with a personal or
family history of heart disease and/or myocarditis were also
excluded from the study. All measurements were performed at the
diastole status for patients with myocardial infarction.
ELISA
The serum levels of marker proteins were analyzed by
commercialized ELISA kits [C-reactive protein (CRP; cat. no.
DY1707), tumor necrosis factor (TNF-α; cat. no. DTA00C),
interleukin (IL-1; cat. no. DLB50) and creatine phosphokinase (CPK;
cat. no. DYDTA02P); all from R&D Systems, Inc., Minneapolis,
MN, USA). The operational procedures were performed according to
the manufacturer's instructions. The results were performed by an
ELISA reader system (1775×Mark™, Bio-Rad Laboratories, Inc.,
Hercules, CA, USA).
MRI scanning
An MRI diagnosis system (Ingenia 1.5T CX; Philips
Medical Systems, Cleveland, OH, USA) was used to diagnose patients
with suspected myocardial infarction using pre-programmed settings.
These settings were optimized to reach the optimal image formation.
The whole heart in all of the patients was subjected to MRI
scanning according to the manufacturer's protocol. The details of
principles and settings of MRI were described in a previous study
(20). MRI processes included T1 and
T2 parametric mapping. Imaging parameters were set as follows: Flip
angle, 46°; repetition time, 3.2 msec; echo time, 1.40 msec;
typical field of view, 340×260 mm2; matrix, 250×210;
slice thickness, 6 mm; slice gap, 3 mm; receiver bandwidth, 977
Hz/pixel; and cardiac phases, n=25. The necessary dose of CFEA for
optimal signal intensity for MIR detection was determined by
analyzing MRI images following increasing doses of CFEA (0–0.5
mg/kg). Images were collected 10–15 min after the administration of
0.30 mg/kg CFEA or 0.1 mmol/kg contrast agent (Gadovist; Bayer,
Leverkusen, Germany).
Image analysis
The MRI image sets were analyzed using the software
included in the MRI system, based on which the presence and
location of myocardial infarction was determined. Signal
enhancement of MRI by CFEA was also measured with this preparatory
program. Planimetric analysis of the myocardial infarction size was
performed using the software included in the system (SyngoMR A30;
Philips Medical Systems) and ImageJ 1.38× software (National Health
Institute, Bethesda, MD, USA).
Statistical methods
Values are expressed as the mean ± standard
deviation. SPSS version 19.0 (IBM Corp., Armonk, NY, USA) was used
to perform all statistical analyses. All statistical analyses were
performed using one-way analysis of variance followed by Dunnett's
post hoc test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Characteristics of patients
A total of 68 patients with suspected myocardial
infarction were enrolled in the present study. Baseline
characteristics all patients are summarized in Table I. The median period between the index
events, including chest pain or abnormities in the
electrocardiograph and heart color ultrasound and MRI or MRI-CFEA
examination was 2 days with an interquartile range of 1–4 days
(21). The cohort included 36 male
patients and 32 female patients and the mean age was 50±17.8
(range, 32.2–67.8) years and 54.3±18.1 (range, 36.2–72.4) years in
male and female patients, respectively.
 | Table I.Characteristics of patients with
myocardial infarction. |
Table I.
Characteristics of patients with
myocardial infarction.
| Characteristic | Males (n=36) | Females (n=32) |
|---|
| Age (years) | 50±17.8 | 54.3±18.1 |
| Chest pain | 36 | 32 |
| Heart rate
(beats/min) | 122 | 130 |
| Diagnostic
method |
|
|
| MRI | 36 | 32 |
|
MRI-CFEA | 36 | 32 |
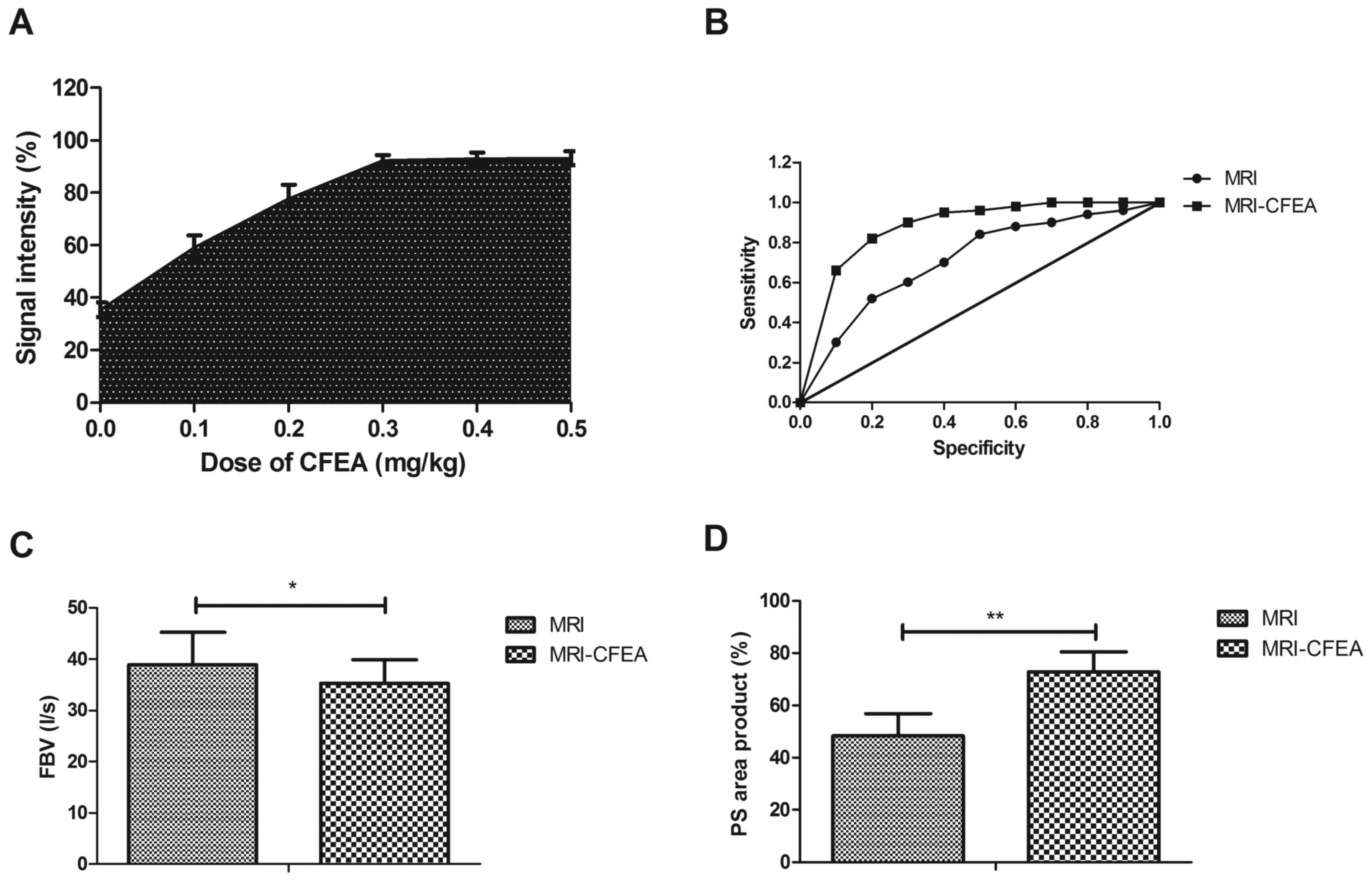
Specificity of MRI-CFEA in the early
clinical diagnosis of patients with suspected myocardial
infarction
The dose of CFEA to achieve the optimum signal
intensity for MIR detection was identified as 0.30 mg/kg (Fig. 1A). The diagnostic efficacy of
MRI-CFEA in patients with suspected myocardial infarction was then
further analyzed. It was demonstrated that MRI-CFEA is more
specific than MRI, as more patients were diagnosed with myocardial
infarction (P<0.05; Fig. 1B). By
MRI-CFEA, 50/68 myocardial infarction cases were diagnosed, which
is significantly higher than the 38/68 myocardial infarction
patients diagnosed by MRI (P<0.05; Table II). It was also indicated that
MRI-CFEA was able to discriminate the infarcted regions based on a
decreased fractional blood volume (FBV) and increased
permeability-surface (PS) area product in the infarcted myocardium
(Fig. 1C and D). A total of 42
patients were confirmed as having myocardial infarction and 20
patients were without myocardial infarction. These outcomes suggest
that MRI-CFEA is a reliable method for early clinical diagnosis of
patients with suspected myocardial infarction.
 | Table II.Diagnostic rates of myocardial
infarction by MRI and MRI-CFEA in suspicious patients. |
Table II.
Diagnostic rates of myocardial
infarction by MRI and MRI-CFEA in suspicious patients.
| Gender | MRI (%) | MRI-CFEA (%) | P-value |
|---|
| Male | 21 (58.33) | 26 (72.22) | 0.0404 |
| Female | 17 (53.13) | 24 (75.00) | 0.0362 |
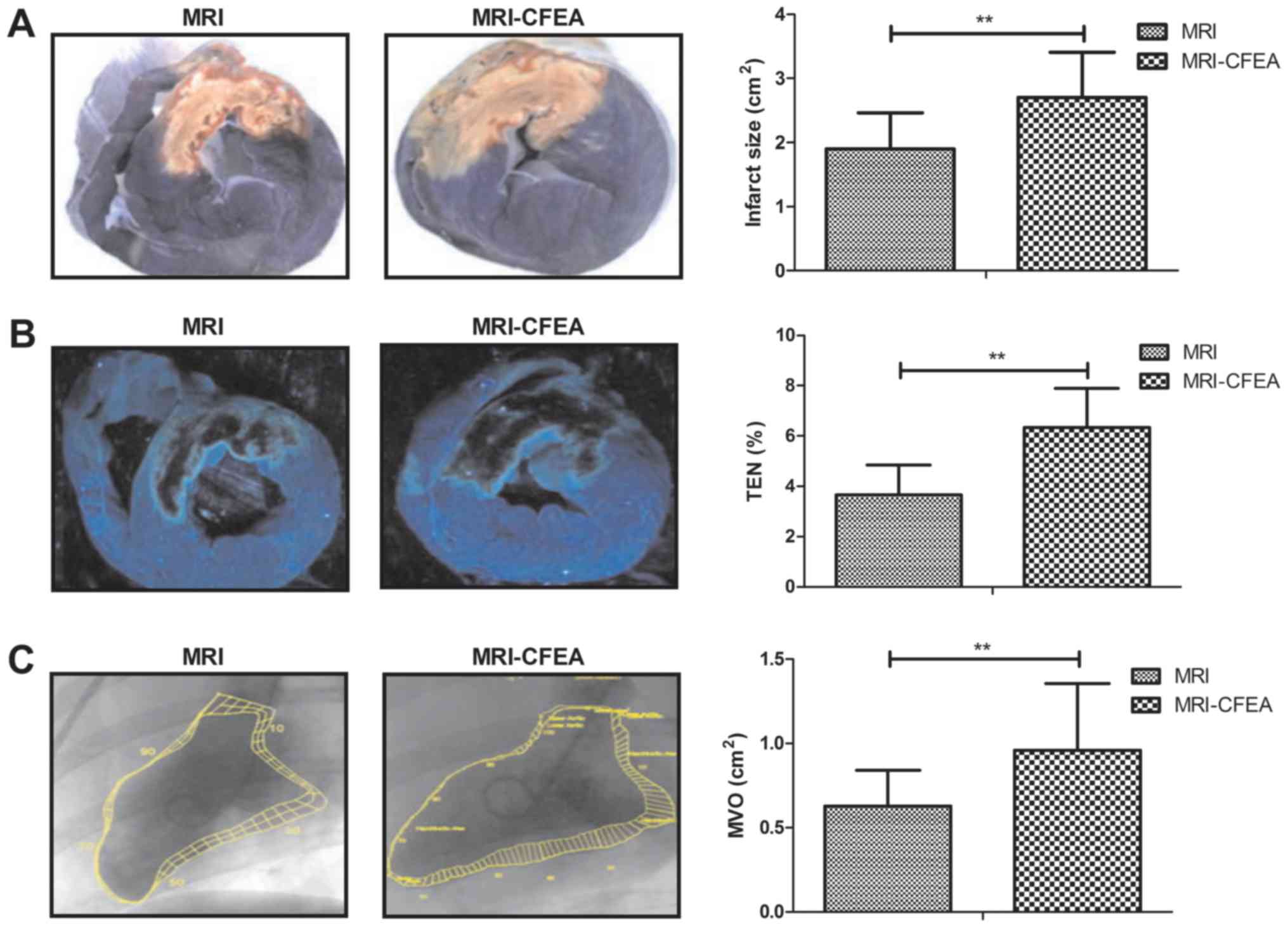
Morphological analysis of myocardial
infarction
Next, the efficacy of the clinical utilization of
cardiac MRI-CFEA in patients with myocardial infarction was
assessed. It was observed that MRI-CFEA displayed the IS and
transmural extent of necrosis more clearly than MRI for patients
with myocardial infarction (Fig. 2A and
B). It was also indicated that MRI-CFEA was able to detect the
MVO for patients with myocardial infarction (Fig. 2C). These results suggest that
MRI-CFEA is more accurate than MRI in detecting pathological
features of myocardial infarction in suspicious patients.
Serology confirms the diagnosis of
MRI-CFEA for patients with suspected myocardial infarction
Assessment of serological biomarkers of myocardial
infarction demonstrated that serum levels of CPK were increased in
patients with myocardial infarction compared with those in healthy
individuals (P<0.05; Table
III). Furthermore, it was demonstrated that the serum levels of
CRP, TNF-α and IL-1 were increased in patients with myocardial
infarction (P<0.05; Table III).
Of note, MRI-CFEA is efficient in diagnosing patients with
myocardial infarction along with high levels of CRP, CPK, TNF-α and
IL-1.
 | Table III.Serum levels of inflammatory factors
in patients with suspected myocardial infarction. |
Table III.
Serum levels of inflammatory factors
in patients with suspected myocardial infarction.
| Factor | Myocardial
infarction | No myocardial
infarction | Normal range | P-value |
|---|
| CPK (U/dl) | 6.130±2.300 | 2.752±1.248 | 4.240±1.240 | 0.0052 |
| CRP (mg/l) | 4.290±4.110 | 11.225±4.495 | 10.000±3.000 | 0.0088 |
| TNF-α (g/l) | 1.770±0.540 | 1.220±0.320 | 1.000±0.300 | 0.0072 |
| IL-1 (µg/l) | 26.100±10.700 | 14.200±6.200 | 15.000±5.000 | 0.0028 |
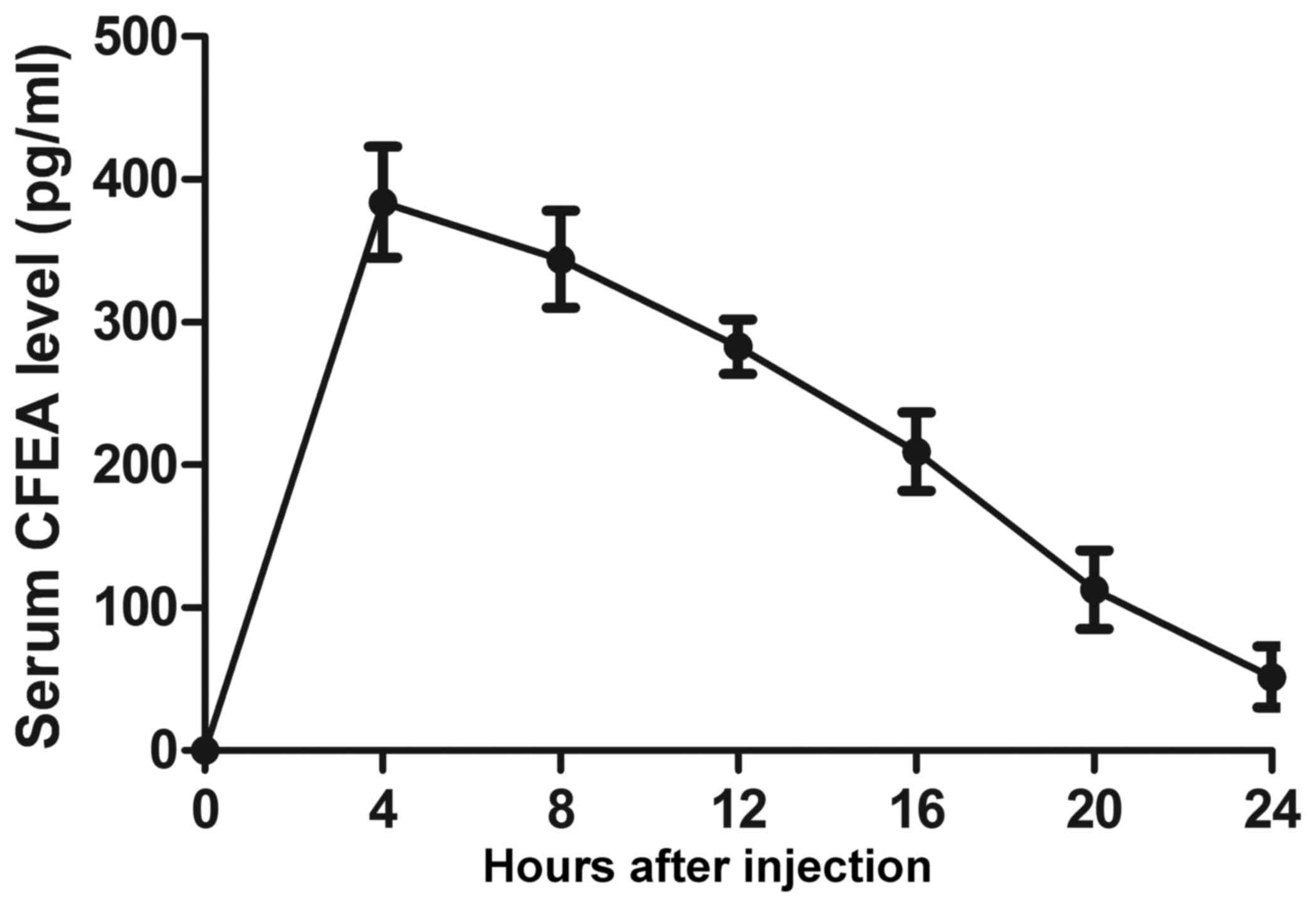
Pharmacodynamics of CFEA in patients
with myocardial infarction
Finally, the pharmacodynamics of CFEA were assessed
after administration to the patients with myocardial infarction. It
was demonstrated that CFEA was eliminated from the plasma within 24
h after intravenous injection (Fig.
3). This result indicates that CFEA may be easily eliminated
from patients with myocardial infarction. No adverse effects were
observed in the present study.
Discussion
Early diagnosis of myocardial infarction is an
efficient method to decrease the mortality and morbidity of
affected patients (22,23). At present, MRI is widely used for
diagnosing myocardial infarction (14,15).
Evidence has indicated that contrast agents increase the diagnostic
efficacy in patients with AMI undergoing coronary angiography
(24). In the present study, the
diagnostic efficacy of the nano-size contrast agent CFEA combined
with MRI was investigated to quantify the blood volume and
permeability in the infarcted myocardium in a total of 68 patients
with suspected myocardial infarction. It was indicated that
MRI-CFEA is an efficient method for diagnosing patients with
suspected myocardial infarction. Of note, a pharmacodynamics
analysis demonstrated that CFEA was easily eliminated from patients
with myocardial infarction within 24 h.
A previous study summarized the current knowledge of
the pharmacokinetic principles of gadolinium chelates for enhancing
the diagnostic value of cardiac MRI in the diagnosis of
complications of myocardial infarction (25). In addition, delayed-enhancement 3.0T
MRI with 0.15 mmol/kg of contrast agent superparamagnetic iron
oxide provides more accuracy in the assessment of chronic
myocardial infarction (26). The
present study identified that the optimal dose of CFEA was 0.30
mg/kg to achieve the maximum signal intensity for MIR detection,
which enhanced the diagnostic efficacy of MRI for patients with
suspected myocardial infarction. A previous study also revealed
that early assessment of myocardial contractility by
contrast-enhanced magnetic resonance imaging is inversely
associated with the contractility after revascularization in
patients after AMI (27). It was
demonstrated that the nano-size contrast agent CFEA improves the
signal intensity for the localization of the myocardial infarction
area and the accuracy of MRI in the diagnosis of clinical patients
with early-stage myocardial infarction.
The pathological characteristics of myocardial
infarction patients include IS, TEN and MVO (28). The present study reported that
MRI-CFEA clearly indicated the IS, TEN and MVO in patients with
early-stage myocardial infarction. It was also demonstrated that
MRI-CFEA was able to discriminate the infarcted regions based on a
decreased FBV and increased PS area product in the infarcted
region. Observation of these parameters facilitates the selection
of a targeted therapy for patients with myocardial infarction.
Inflammatory responses are included in the
pathogenesis of atherosclerosis and its clinical result, myocardial
infarction (29). CRP and CPK-MB may
act as mortality predictors in patients with AMI (30). The present study reported that the
serum levels of CRP and CPK were upregulated in clinical myocardial
infarction patients. According to previous studies, the serum
levels of TNF-α and IL-1 were increased in patients with previous
myocardial infarction (31,32). The present study demonstrated that
the serum levels of TNF-m and IL-1 were increased in patients with
myocardial infarction. The present results suggested that MRI-CFEA
is efficient in diagnosing patients with myocardial infarction who
also presented with elevated levels of CRP, CPK, TNF-α and
IL-1.
In conclusion, the present study reported that MRI
using CFEA as a contrast agent improved the sensitivity and
accuracy of MRI in diagnosing patients with early-stage myocardial
infarction. It was reported that MRI-CFEA was able to detect
pathological characteristics of myocardial infarction. The present
study may contribute to the development of methods for the early
diagnosis of myocardial infarction, and may be used for evaluating
the degree of myocardial infarction.
Acknowledgements
Not applicable.
Funding
The authors acknowledge financial support from the
National Natural Science Foundation of China (grant no. 81401388)
and the Health Administration of Hainan Province, China (grant nos.
14A210259 and 1601320114A2002).
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
JQ and SZ performed the experiments. TA designed the
experiments for the study and ZL, YC and QQ analyzed the
experimental data. The final version of the manuscript has been
read and approved by all authors.
Ethics approval and consent to
participate
The present study was also approved by the Ethics
Committee of Tongji Medical College and written informed consent
was obtained from all patients or their relatives prior to their
inclusion within the study.
Consent for publication
Written informed consent was obtained from all
patients for the publication of their data.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Nam J, Caners K, Bowen JM, Welsford M and
O'Reilly D: Systematic review and meta-analysis of the benefits of
out-of-hospital 12-lead ECG and advance notification in ST-segment
elevation myocardial infarction patients. Ann Emerg Med.
64:176–186.e9. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Barauskas M, Unikas R, Tamulenaite E and
Unikaite R: The impact of clinical and angiographic factors on
percutaneous coronary angioplasty outcomes in patients with acute
ST-elevation myocardial infarction. Arch Med Sci Atheroscler Dis.
1:e150–e157. 2016.PubMed/NCBI
|
|
3
|
Sarikamis C, Caglar NT, Biyik I, Ozturk D,
Uzun F, Akturk IF, Ayaz A, Tasbulak O, Celik O and Yalcin AA: Can
thrombectomy and catheters used increase angiographically visible
distal embolization in st elevation myocardial infarction? Arch Med
Sci Atheroscler Dis. 1:e139–e144. 2016.PubMed/NCBI
|
|
4
|
Woolf-May K and Meadows S: Appropriateness
of the metabolic equivalent (MET) as an estimate of exercise
intensity for post-myocardial infarction patients. BMJ Open Sport
Exerc Med. 2:e0001722016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nascimento BR, de Sousa MR, Demarqui FN
and Ribeiro AL: Risks and benefits of thrombolytic, antiplatelet,
and anticoagulant therapies for st segment elevation myocardial
infarction: Systematic review. ISRN Cardiol. 2014:4162532014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
El Aidi H, Adams A, Moons KG, Den Ruijter
HM, Mali WP, Doevendans PA, Nagel E, Schalla S, Bots ML and Leiner
T: Cardiac magnetic resonance imaging findings and the risk of
cardiovascular events in patients with recent myocardial infarction
or suspected or known coronary artery disease: A systematic review
of prognostic studies. J Am Coll Cardiol. 63:1031–1045. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Christensen AV, Koch MB, Davidsen M,
Jensen GB, Andersen LV and Juel K: Educational inequality in
cardiovascular disease depends on diagnosis: A nationwide register
based study from denmark. Eur J Prev Cardiol. 23:826–833. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Han W, Xie M, Cheng TO, Wang Y, Zhang L,
Hu Y, Cao H, Hong L, Yang Y, Sun Z and Yu L: The vital role the
ductus arteriosus plays in the fetal diagnosis of congenital heart
disease: Evaluation by fetal echocardiography in combination with
an innovative cardiovascular cast technology. Int J Cardiol.
202:90–96. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ahmad IG, Abdulla RK, Klem I, Margulis R,
Ivanov A, Mohamed A, Judd RM, Borges-Neto S, Kim RJ and Heitner JF:
Comparison of stress cardiovascular magnetic resonance imaging
(CMR) with stress nuclear perfusion for the diagnosis of coronary
artery disease. J Nucl Cardiol. 23:287–297. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nensa F, Mahabadi AA, Erbel R and
Schlosser TW: Myocardial edema during acute myocardial infarction
visualized by diffusion-weighted MRI. Herz. 38:509–510. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang Y, Graham JJ, Connelly K, Foltz WD,
Dick AJ and Wright GA: MRI manifestations of persistent
microvascular obstruction and acute left ventricular remodeling in
an experimental reperfused myocardial infarction. Quant Imaging Med
Surg. 2:12–20. 2012.PubMed/NCBI
|
|
12
|
Ahmed N, Carrick D, Layland J, Oldroyd KG
and Berry C: The role of cardiac magnetic resonance imaging (MRI)
in acute myocardial infarction (AMI). Heart Lung Circ. 22:243–255.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rischpler C, Langwieser N, Souvatzoglou M,
Batrice A, van Marwick S, Snajberk J, Ibrahim T, Laugwitz KL,
Nekolla SG and Schwaiger M: PET/MRI early after myocardial
infarction: Evaluation of viability with late gadolinium
enhancement transmurality vs. 18F-FDG uptake. Eur Heart J
Cardiovasc Imaging. 16:661–669. 2015.PubMed/NCBI
|
|
14
|
Pegg TJ, Maunsell Z, Karamitsos TD, Taylor
RP, James T, Francis JM, Taggart DP, White H, Neubauer S and
Selvanayagam JB: Utility of cardiac biomarkers for the diagnosis of
type V myocardial infarction after coronary artery bypass grafting:
Insights from serial cardiac MRI. Heart. 97:810–816. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Malbranque G, Serfaty JM, Himbert D, Steg
PG and Laissy JP: Myocardial infarction after blunt chest trauma:
Usefulness of cardiac ECG-gated CT and MRI for positive and
aetiologic diagnosis. Emerg Radiol. 18:271–274. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zeng ZQ, Chen DH, Tan WP, Qiu SY, Xu D,
Liang HX, Chen MX, Li X, Lin ZS, Liu WK and Zhou R: Epidemiology
and clinical characteristics of human coronaviruses OC43, 229E,
NL63, and HKU1: A study of hospitalized children with acute
respiratory tract infection in Guangzhou, China. Eur J Clin
Microbiol Infect Dis. 37:363–369. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kousi E, Smith J, Ledger AE, Scurr E,
Allen S, Wilson RM, O'Flynn E, Pope RJE, Leach MO and Schmidt MA:
Quantitative evaluation of contrast agent uptake in standard
fat-suppressed dynamic contrast-enhanced MRI examinations of the
breast. Med Phy. 45:287–296. 2018. View
Article : Google Scholar
|
|
18
|
Chen CL, Hu GY, Mei Q, Qiu H, Long GX and
Hu GQ: Epidermal growth factor receptor-targeted ultra-small
superparamagnetic iron oxide particles for magnetic resonance
molecular imaging of lung cancer cells in vitro. Chin Med J (Engl).
125:2322–2328. 2012.PubMed/NCBI
|
|
19
|
Mehmood T, Al Shehrani MS and Ahmad M:
Acute coronary syndrome risk prediction of rapid emergency medicine
scoring system in acute chest pain. An observational study of
patients presenting with chest pain in the emergency department in
Central Saudi Arabia. Saudi med J. 38:900–904. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sahibzada I, Batura D and Hellawell G:
Validating multiparametric MRI for diagnosis and monitoring of
prostate cancer in patients for active surveillance. Int Urol
Nephrol. 48:529–533. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Andrade JM, Gowdak LH, Giorgi MC, de Paula
FJ, Kalil-Filho R, de Lima JJ and Rochitte CE: Cardiac MRI for
detection of unrecognized myocardial infarction in patients with
end-stage renal disease: Comparison with ECG and scintigraphy. AJR.
Am J Roentgenol. 193:W25–W32. 2009. View Article : Google Scholar
|
|
22
|
Lee HY, Choi JS, Guruprasath P, Lee BH and
Cho YW: An electrochemical biosensor based on a myoglobin-specific
binding peptide for early diagnosis of acute myocardial infarction.
Anal Sci. 31:699–704. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Westwood M, van Asselt T, Ramaekers B,
Whiting P, Thokala P, Joore M, Armstrong N, Ross J, Severens J and
Kleijnen J: High-sensitivity troponin assays for the early rule-out
or diagnosis of acute myocardial infarction in people with acute
chest pain: A systematic review and cost-effectiveness analysis.
Health Technol Assess. 19:1–234. 2015. View
Article : Google Scholar
|
|
24
|
Gunebakmaz O, Duran M, Kaya Z and Kaya MG:
Contrast agent: A scapegoat for serum creatinine increase in
patients with acute myocardial infarction undergoing coronary
angiography. Angiology. 64:4002013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Flavian A, Carta F, Thuny F, Bernard M,
Kober F, Moulin G, Varoquaux A and Jacquier A: Cardiac MRI in the
diagnosis of complications of myocardial infarction. Diagn Interv
Imaging. 93:578–585. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yang J, Ma H, Liu J, Wang C, Shi Y, Xie H,
Huo F, Liu F and Lin K: Delayed-enhancement magnetic resonance
imaging at 3.0T using 0.15 mmol/kg of contrast agent for the
assessment of chronic myocardial infarction. Eur J Radio.
83:778–782. 2014. View Article : Google Scholar
|
|
27
|
Lim HE, Yong HS, Shin SH, Ahn JC, Seo HS,
Oh DJ, Ro YM and Park CG: Early assessment of myocardial
contractility by contrast-enhanced magnetic resonance (ceMRI)
imaging after revascularization in acute myocardial infarction
(AMI). Korean J Intern Med. 19:213–219. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nagata Y, Usuda K, Uchiyama A, Uchikoshi
M, Sekiguchi Y, Kato H, Miwa A and Ishikawa T: Characteristics of
the pathological images of coronary artery thrombi according to the
infarct-related coronary artery in acute myocardial infarction.
Circ J. 68:308–314. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Coker A, Arman A, Soylu O, Tezel T and
Yildirim A: Lack of association between IL-1 and IL-6 gene
polymorphisms and myocardial infarction in Turkish population. Int
J Immunogenet. 38:201–208. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Beg M, Singhal KC, Wadhwa J and Akhtar N:
ST-deviation, C-reactive protein and CPK-MB as mortality predictors
in acute myocardial infarction. Nepal Med Coll J. 8:149–152.
2006.PubMed/NCBI
|
|
31
|
Vörös K, Prohászka Z, Kaszás E,
Alliquander A, Terebesy A, Horváth F, Janik L, Sima A, Forrai J,
Cseh K and Kalabay L: Serum ghrelin level and TNF-α/ghrelin ratio
in patients with previous myocardial infarction. Arch Med Res.
43:548–554. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zeybek U, Toptas B, Karaali ZE, Kendir M
and Cakmakoglu B: Effect of TNF-alpha and IL-1β genetic variants on
the development of myocardial infarction in Turkish population. Mol
Biol Rep. 38:5453–5457. 2011. View Article : Google Scholar : PubMed/NCBI
|