Introduction
Lower back pain is a common complication of
postoperative epidural analgesia, and the incidence is 2–31%
(1), especially in women with
cesarean section, whose incidence of lower back pain is as high as
35% (2). Mild pain can cause
insomnia and anxiety. In severe cases, it can even cause tearing
pain in the waist, which brings about tremendous physical and
psychological trauma to the mother. It is also possible that lower
back pain turns into chronic pain, disturbing parturient for a long
time and having a negative effect on quality of their lives
(3). In general, the treatment of
postoperative lower back pain is patient-controlled epidural
analgesia and intravenous controlled analgesia (4). Although the two treatment methods can
relieve pain after maternal, they have no preventive effect on
postoperative lower back pain. Therefore, it is considered that
whether there is a way that can effectively prevent the occurrence
of lower back pain, or can effectively reduce the degree of pain.
In the study of Salem et al (5), dexamethasone (DXMS) was shown to be
effective in reducing adverse anesthesia during cesarean delivery.
Thus whether DXMS also reduces back pain following epidural
delivery analgesia is considered. DXMS is a kind of steroid
hormones, and its role is similar to glucocorticoid, commonly used
in the local treatment of chronic pain. DXM also has significant
preventive effect on postpartum hemorrhage in cesarean section
(6). There are also studies showing
that DXMS is conducive for combined spinal-epidural analgesia
cesarean section (7), which
indicates that DXMS has been widely used in pregnant women and its
safety has been guaranteed. DXMS has a variety of therapeutic
effects, but there are few researches about its effect on
postoperative epidural analgesia lower back pain. To determine the
effect of DXMS local pretreatment on epidural puncture point on the
prevention of postoperative lower back pain after epidural
analgesia, the following statistical analysis was performed.
Materials and methods
General information
A total of 368 parturient women admitted into
People's Hospital of Rizhao (Rizhao, China) from January 2014 to
December 2016 undergoing epidural labor analgesia were included for
the study. A total of 188 patients treated with DXMS and lidocaine
mixture around the epidural puncture point were enrolled into the
observation group, with a mean age of (27.2±4.7) years; a total of
180 patients treated with 0.9% sodium chloride injection and
lidocaine mixture around the epidural puncture point were enrolled
in the control group, with a mean age of (28.3±4.9) years.
Epidural analgesia for labor was applied on
parturients who were primipara with full term single live fetus,
aged 22 to 35 years old, in full compliance with epidural
anesthesia contraindications and indications, and in line with
American Society of Anesthesiologists ASA grading (8) I–II level. Exclusion for the following
cases: patients allergic or resistant to DXMS, patients with
digestive diseases and in active phases; patients with
abnormalities in adrenocortical function; patients with
abnormalities in liver and kidney function; patients with a history
of pre-eclampsia, diabetes, gestational hypertension; patients with
mental disorders or abnormal brain judgments; patients failed for
epidural analgesics. The postoperative lower back pain condition at
48 and 72 h after operation and the general conditions such as
gender, height, weight were recorded. The study obtained the
medical Ethics Committee's approval of People's Hospital of Rizhao,
and all patients and their relatives signed the informed consent
form.
Treatment
Parturient was given oxygen immediately after
entering the delivery room. Routine monitoring of vital signs was
performed. When the cervix was open to 3–5 cm, epidural
catheterization anesthesia was immediately performed. Routine
disinfection and towels were placed, patients were right arm
reclining and received anesthesia at L3 and L4. Pretreatment for
patients in the observation group was the injection of lidocaine (4
ml) and DXMS (1 ml) mixture around the puncture point, patients in
the control group were given the injection of lidocaine (4 ml) and
0.9% sodium chloride mixture as the pretreatment. Then anesthesia
and puncture were performed, an epidural catheter was placed,
patients were injected with 0.2% ropivacaine (10 ml) and maintained
at 10 ml/h with 0.1% ropivacaine + 2 µg/ml fentanyl. The drug was
immediately stopped when the cervix was fully opened.
During the delivery, if prolonged labor or
stagnation occurred, the parturient was moved to the operation room
immediately for cesarean section. Narcotic drug was lidocaine
hydrochloride injection (SFDA approval no. H37022147; Shandong
Hualu Pharmaceutical Co., Ltd., Liaocheng, China), specifications:
5 ml: 0.1 g; DXMS sodium phosphate injection (SFDA approval no.
H41021255; Suicheng Pharmaceutical Co., Ltd., Zhengzhou, China),
specifications: 1 ml: 5 mg; Ropivacaine (SFDA approval no.
H20100126; Jiangsu Hengrui Pharmaceutical Co., Ltd., Nanjing,
China), specifications: 20 mg/10 ml/U, fentanyl (Zhunzi H20030199;
Yifan Renfu Pharmaceutical Co., Ltd., Shanghai, China),
specifications: 2 ml: 0.1 mg. The implementation standard was
Chinese Pharmacopoeia 2015 edition two (9).
Observation index
Postoperative lower back pain was assessed by using
the Visual Analogue Scale/Score (VAS) (10), defined as mild pain at 1–3 scores
moderate pain at 4–6 scores, severe pain at 7–10 scores.
Statistical analysis
SPSS 19.0 (IBM, Armonk, NY, USA) was used for
statistical analysis. The enumeration data was expressed as
percentage. The measurement data were expressed as mean ± SD. The
comparison between measurement data was performed by t-test. The
rate was compared by Chi-square test. p<0.05 represented the
difference was statistically significant.
Results
Clinical data
A total of 368 patients with labor analgesia were
enrolled, 188 cases were in the observation group and 180 cases in
the control group. There was no significant difference in the basic
data of maternal age, height, weight, education, residence,
exercise habits, ethnicity, mode of delivery, puncture times and
ASA grade between the two groups (p>0.05). The factors between
the two group were comparable. The clinical data of two groups can
be seen from Table I.
 | Table I.Clinical data of two groups of
patients. |
Table I.
Clinical data of two groups of
patients.
| Item | Observation group [n
(%)] | Control group [n
(%)] | t/χ2 | p-value |
|---|
| Age (year) |
|
| 0.876 | 0.411 |
|
<28 | 112 (59.57) | 109 (60.56) |
|
|
| ≥28 | 76
(40.43) | 71
(39.44) |
|
|
| Height (cm) |
|
| 0.175 | 0.969 |
|
<160 | 120 (63.83) | 126 (70.00) |
|
|
| ≥160 | 68
(36.17) | 54
(30.00) |
|
|
| Weight (kg) |
|
| 0.956 | 0.396 |
|
<55 | 96
(51.06) | 93
(51.67) |
|
|
| ≥55 | 92
(48.94) | 87
(48.33) |
|
|
| Cultural level |
|
| 1.363 | 0.517 |
| ≤High
school | 95
(50.53) | 88
(48.89) |
|
|
| >High
school | 93
(49.47) | 92
(51.11) |
|
|
| Residence |
|
| 1.336 | 0.522 |
| City | 99
(52.66) | 88
(48.89) |
|
|
|
Countryside | 89
(47.34) | 92
(51.11) |
|
|
| Exercise habits |
|
| 0.933 | 0.393 |
| Yes | 73
(38.83) | 66
(36.67) |
|
|
| No | 115 (61.17) | 114 (63.33) |
|
|
| Puncture times
(time) |
|
| 0.976 | 0.381 |
| 1 | 160 (85.11) | 153 (85.00) |
|
|
|
>1 | 28
(14.89) | 27
(15.00) |
|
|
| ASA
classification |
|
| 1.147 | 0.311 |
| I | 153 (81.38) | 150 (83.33) |
|
|
| II | 35
(18.62) | 30
(16.67) |
|
|
| Mode of delivery |
|
| 0.912 | 0.419 |
| Natural
production | 135 (71.81) | 131 (72.78) |
|
|
| Cesarean
section | 53
(28.19) | 49
(27.22) |
|
|
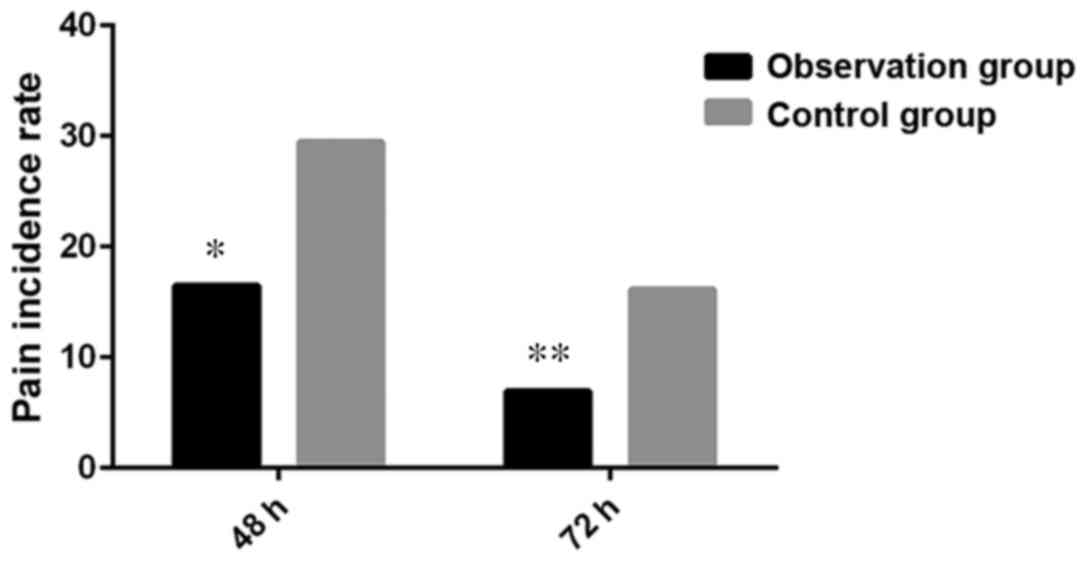
Comparison of postoperative lower back
pain incidence
There were 36 (19.15%) cases of lower back pain in
the observation group and 67 (37.22%) cases of the lower back pain
in the control group at 48 hours after operation. There were 18
(9.57%) cases of lower back pain in the observation group and 43
(23.89%) cases of the lower back pain in the control group at 72 h
after operation. There was a significant difference in the
incidence of lower back pain between the two groups (p=0.032) at 48
h after operation. The incidence of lower back pain at 72 h after
operation between the two groups was significantly different
(p=0.036). DXMS pretreatment can reduce the incidence of
post-partum back pain in patients with epidural analgesia (Fig. 1).
Effect of DXMS anesthesia on
parturient with different puncture times
In the observation group, the number of patients
undergoing one puncture was 160, of which 28 patients had
postoperative lower back pain; there were 28 patients undergoing
more than 1 punctures, of which 8 patients had postoperative lower
back pain. In the control group, the number of patients undergoing
one puncture was 153, of which 51 patients had postoperative lower
back pain; there were 27 patients undergoing more than 1 punctures,
of which 16 patients had postoperative lower back pain. Among the
patients undergoing one puncture, the incidence of postoperative
lower back pain in the observation group (17.50%) was significantly
lower than that in the control group (33.33%), and the difference
was statistically significant (p=0.018); among the patients
undergoing more than one punctures, the incidence of postoperative
lower back pain in the observation group (28.57%) was significantly
lower than that in the control group (59.26%), and the difference
was statistically significant (p=0.006) (Table II).
 | Table II.Comparison of the incidence of
postoperative lower back pain between the two groups of
parturient. |
Table II.
Comparison of the incidence of
postoperative lower back pain between the two groups of
parturient.
|
| One puncture | More than one
puncture |
|---|
|
|
|
|
|---|
| Group | n | Without pain [(n
%)] | Pain [(n %)] | n | Without pain [(n
%)] | Pain [(n %)] |
|---|
| Observation
group | 160 | 132 (82.50) | 28 (17.50) | 28 | 20 (71.43) | 8
(28.57) |
| Control group | 153 | 102 (66.67) | 51 (33.33) | 27 | 11 (40.74) | 16 (59.26) |
| χ2 |
| 4.232 | 6.438 |
| 4.697 | 7.626 |
| p-value |
| 0.033 | 0.018 |
| 0.030 | 0.006 |
Effect of DXMS in different modes of
delivery
In the observation group, the number of spontaneous
births was 135, of which 26 patients occurred postoperative lower
back pain; the number of cesarean section was 53, among them 10
patients occurred postoperative lower back pain. In the control
group, the number of births was 131, of which 48 patients occurred
postoperative lower back pain; the number of cesarean section was
49, postoperative lower back pain occurred in 19 patients. Among
the spontaneous birth patients, the incidence of postoperative
lower back pain in the observation group (19.26%) was significantly
lower than that in the control group (36.64%), and the difference
was statistically significant (p=0.028). Among the cesarean section
patients, the incidence of lower back pain in observation group
(18.87%) was significantly lower than that in control group
(38.78%), the difference was statistically significant (p=0.019)
(Table III).
 | Table III.Comparison of postoperative lower back
pain incidence between different modes of delivery. |
Table III.
Comparison of postoperative lower back
pain incidence between different modes of delivery.
|
| Spontaneous
birth | Cesarean section |
|---|
|
|
|
|
|---|
| Group | n | No pain [(n
%)] | Pain [(n %)] | n | No pain [(n
%)] | Pain [(n %)] |
|---|
| Observation | 135 | 109 (80.74) | 26 (19.26) | 53 | 43 (81.13) | 10 (18.87) |
| Control | 131 | 83
(63.36) | 48 (36.64) | 49 | 30 (61.22) | 19 (38.78) |
| χ2 |
| 4.667 | 4.213 |
| 4.888 | 6.434 |
| p-value |
| 0.031 | 0.028 |
| 0.021 | 0.019 |
Comparison of VAS score
At 48 h after operation, there were 36 cases of
postoperative lower back pain in the observation group, including
20 cases of mild pain, 13 cases of moderate pain and 3 cases of
severe pain. In the control group, there were 67 cases of
postoperative lower back pain, including 19 cases of mild pain, 33
cases of moderate pain and 15 cases of severe pain. At 72 h after
operation, 18 maternal postoperative lower back pain patients were
observed in the observation group, including 14 mild pains, 3
moderate pains and 1 severe pain. In the control group, 43 cases of
maternal postoperative lower back pain were observed, including 5
cases of mild, 25 cases of moderate, 13 cases of severe pain. There
was significant difference between the two groups in terms of
different degrees of lower back pain at 48 h, 72 h after operation
(p<0.05). At 48 h after operation, the number of severe pain
cases in the observation group was significantly lower than that in
the control group (p=0.021); at 72 h after operation, the number of
severe pain cases in the observation group was significantly lower
than that in the control group (p=0.014) (Table IV).
 | Table IV.Comparison of VAS scores at 48 h and
72 h. |
Table IV.
Comparison of VAS scores at 48 h and
72 h.
|
|
| 48 h |
| 72 h |
|---|
|
|
|
|
|
|
|---|
|
| n | Mild [(n %)] | Moderate [(n
%)] | Severe [(n %)] | n | Mild [(n %)] | Moderate [(n
%)] | Severe [(n %)] |
|---|
| Observation | 36 | 20 (55.56) | 13 (36.11) | 3
(8.33) | 18 | 14 (77.78) | 3
(16.67) | 1
(5.56) |
| Control | 67 | 19 (28.36) | 33 (49.25) | 15 (22.39) | 43 | 5
(11.63) | 25 (58.14) | 13 (30.23) |
| χ2 |
| 6.435 | 4.232 | 4.886 |
| 7.624 | 6.756 | 6.331 |
| p-value |
| 0.012 | 0.026 | 0.021 |
| 0.007 | 0.009 | 0.014 |
Discussion
Epidural analgesia has a variety of advantages
including rapid onset, small dosage, the exact effect, good
controllability, and it has become the preferred method of
obstetric surgical anesthesia in China (11). However, there are many adverse
reactions of epidural anesthesia, and lower back pain is one of the
major. Currently it is considered that postoperative lower back
pain is due to the lower back soft tissue injury caused by the
puncture during epidural anesthesia in the back. Soft tissue injury
can cause local aseptic inflammation, such as periostitis,
tendonitis, or cause traumatic edema of the supraspinal ligament
and the interspinal ligament (12).
DXMS is widely used in the treatment of pain. Epidural
postoperative lower back pain is its indications. The side effects
DXMS brings to the body is minimal, so it will not bring adverse
effect on the quality of patients' lives (13). Therefore, the medical records of 368
cases were retrospectively analyzed, and the effects of DXMS on the
prevention of lower back pain in pregnant women after epidural
analgesia were summarized.
In this study, the inclusion criteria was strictly
enforced and the relevant variables were strictly controlled so as
to ensure the validity of the research results. At the same time,
repeated examinations on the data processing part of the experiment
were conducted to minimize the error of the research results. In
this study, the incidence of lower back pain at 48 and 72 h
postoperatively in the observation group was significantly lower
than that in the control group, and the incidence of lower back
pain in both groups was significantly different at different
time-points (p<0.05). Therefore, it can be thought that
preoperative DXMS can effectively reduce the incidence of
postoperative lower back pain in patients with epidural analgesia.
In the study of Abd et al (14), they demonstrated that DXMS is
absorbed intramuscularly in human tissues and absorbed by tissue
vessels. DXMS binds to extracellular receptors and alters the
arrangement of cell surface molecules, resulting in decreased
permeability of the capillary wall to achieve the role of
vasoconstriction and analgesia. In a related study by Rathmell
et al (15), they concluded
that in epidural surgery, DXMS can inhibit the activation and
release of the inflammatory mediators around the injured tissue by
inhibiting the synthesis of prostaglandins and inhibiting the
oxidase activity around the wound site, thereby achieving the
analgesic effect of inhibiting spinal nerve root conduction. This
corroborates the results in this study that DXMS pretreatment is
effective in reducing the incidence of postoperative lower back
pain in epidural labor analgesia. In the study of Chau et al
(16) and Wilson et al
(17), it was shown that the number
of punctures is a direct factor affecting postoperative lower back
pain. Therefore, the effect of DXMS on patients with different
times of punctures was investigated and it was found that either
with one puncture or many times of puncture, the incidence of
postoperative lower back pain in the observation group was
significantly lower than that in the control group. In the study of
Chou et al (18), they found
that cesarean section led to a variety of complications such as
postoperative lower back pain. Therefore, the effect of DXMS on
different modes of delivery was also compared, and it was found
that both the incidence of postoperative lower back pain in the
observation group was significantly lower than that in the control
group, either in the case of spontaneous or in the case of cesarean
delivery. The result showed that DXMA can reduce the incidence rate
of postoperative lower back pain in different delivery mode. In
addition, the degree of maternal lower back pain at different
time-points after operation was also compared, and it was found
that DXMS pretreatment can significantly reduce the degree of lower
back pain after postoperative epidural analgesia. In the study by
Sharma et al (19), they
concluded that the long-term analgesic effect that DXMS exerts was
due to long half-life of DXMS and the slower absorption of DXMS in
the body, making DXMS perform a long time analgesic effect on the
puncture site.
Labor analgesia originated in foreign countries, and
it has a history of only more than 100 years. It is a simple, safe
and mature technology with a high penetration rate in foreign
countries. The analgesia rate in the United States is more than
85%, and more than 90% in the United Kingdom (20). In China, there are still few
hospitals that can perform labor analgesia, and the popularity in
China is still very low. Therefore, there are still few studies on
labor analgesia. The lack of sample size is also a problem in this
study. This study can play an auxiliary role in labor analgesia.
With the increase of painless childbirth in China, this study will
certainly provide guidance for labor analgesia in the future.
In conclusion, DXMS local pretreatment can reduce
the incidence of lower back pain after labor analgesia, and it can
reduce the degree of lower back pain. DXMS is beneficial for the
prevention of postoperative lower back pain after epidural delivery
and deserved to be widely used in clinical treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
ZY and LL designed the study. JM, WG and SL
collected the patient data. YJ and YL analyzed the patient data. ZY
prepared the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study obtained the medical Ethics Committee's
approval of People's Hospital of Rizhao (Rizhao, China), and all
patients and their relatives signed the informed consent form.
Patient consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to
declare.
References
|
1
|
Bateman BT, Mhyre JM, Ehrenfeld J,
Kheterpal S, Abbey KR, Argalious M, Berman MF, Jacques PS, Levy W,
Loeb RG, et al: The risk and outcomes of epidural hematomas after
perioperative and obstetric epidural catheterization: A report from
the Multicenter Perioperative Outcomes Group Research Consortium.
Anesth Analg. 116:1380–1385. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kazdal H, Kanat A, Batcik OE, Ozdemir B,
Senturk S, Yildirim M, Kazancioglu L, Sen A, Batcik S and Balik MS:
Central sagittal angle of the sacrum as a new risk factor for
patients with persistent low back pain after caesarean section.
Asian Spine J. 11:726–732. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Daly B, Young S, Marla R, Riddell L,
Junkin R, Weidenhammer N, Dolan J, Kinsella J and Zhang R:
Persistent pain after caesarean section and its association with
maternal anxiety and socioeconomic background. Int J Obstet Anesth.
29:57–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cho YH, Kim CK, Heo KH, Lee MS, Ha IH, Son
DW, Choi BK, Song GS and Shin BC: Acupuncture for acute
postoperative pain after back surgery: A systematic review and
meta-analysis of randomized controlled trials. Pain Pract.
15:279–291. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Salem MN, Abbas AM and Ashry M:
Dexamethasone for the prevention of neonatal respiratory morbidity
before elective cesarean section at term. Proc Obstet Gynecol.
6:pp. 1–10. 2016; View Article : Google Scholar
|
|
6
|
Nado H, Singh N, Laithangbam P, Devi RS,
Alemwapang O and Gangmei FL: A comparative study between propofol
and propofol plus dexamethasone as antiemetic during cesarean
section under spinal anesthesia. JMS. 31:174–183. 2017.
|
|
7
|
Wahdan AS, El-Sakka AI and Gaafar HMI: The
effect of addition of dexamethasone to levobupivacaine in
parturients receiving combined spinal-epidural for analgesia for
vaginal delivery. Indian J Anaesth. 61:556–561. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Djaladat H, Bruins HM, Miranda G, Cai J,
Skinner EC and Daneshmand S: The association of preoperative serum
albumin level and American Society of Anesthesiologists (ASA) score
on early complications and survival of patients undergoing radical
cystectomy for urothelial bladder cancer. BJU Int. 113:887–893.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li R, Wang C, Lei P, Huang L and Yuan S:
Chemical constituents in Flos Sophorae Carbonisatus. Zhongguo Zhong
Yao Za Zhi. 35:607–609. 2010.(In Chinese). PubMed/NCBI
|
|
10
|
Ciprandi G, Tosca MA and Silvestri M:
Measuring the perception of symptom, drug use and allergen
immunotherapy efficacy using the Visual Analogue Scale. Expert Rev
Clin Immunol. 10:179–182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang F, Cao YX, Ke SG, Zhu TH and Zhang M:
Effect of combined spinal-epidural analgesia in labor on frequency
of emergency cesarean delivery among nulliparous Chinese women. Int
J Gynaecol Obstet. 135:259–263. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rosero EB and Joshi GP: Nationwide
incidence of serious complications of epidural analgesia in the
United States. Acta Anaesthesiol Scand. 60:810–820. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mathiesen O, Dahl B, Thomsen BA, Kitter B,
Sonne N, Dahl JB and Kehlet H: A comprehensive multimodal pain
treatment reduces opioid consumption after multilevel spine
surgery. Eur Spine J. 22:2089–2096. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Abd OE, Amadera J, Gomba LA and Pimentel
DC: Poster 400 immediate and acute complications following
transforaminal epidural steroid injections with dexamethasone. Pain
Physician. 4:277–286. 2012.
|
|
15
|
Rathmell JP, Benzon HT, Dreyfuss P,
Huntoon M, Wallace M, Baker R, Riew KD, Rosenquist RW, Aprill C,
Rost NS, et al: Safeguards to prevent neurologic complications
after epidural steroid injections: Consensus opinions from a
multidisciplinary working group and national organizations.
Anesthesiology. 122:974–984. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chau A, Bibbo C, Huang CC, Elterman KG,
Cappiello EC, Robinson JN and Tsen LC: Dural puncture epidural
technique improves labor analgesia quality with fewer side effects
compared with epidural and combined spinal epidural techniques: A
randomized clinical trial. Anesth Analg. 124:560–569. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wilson SH, Wolf BJ, Bingham K, Scotland
QS, Fox JM, Woltz EM and Hebbar L: Labor analgesia onset with dural
puncture epidural versus traditional epidural using a 26-gauge
whitacre needle and 0.125% bupivacaine bolus: A randomized clinical
trial. Anesth Analg. 126:545–551. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chou R, Gordon DB, de Leon-Casasola OA,
Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL,
Chittenden EH, Degenhardt E, et al: Management of postoperative
pain: A clinical practice guideline from the American Pain Society,
the American Society of Regional Anesthesia and Pain Medicine, and
the American Society of Anesthesiologists' Committee on Regional
Anesthesia, Executive Committee, and Administrative Council. J
Pain. 17:131–157. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sharma SK, Rogers BB, Alexander JM,
McIntire DD and Leveno KJ: A randomized trial of the effects of
antibiotic prophylaxis on epidural-related fever in labor. Anesth
Analg. 118:604–610. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gupta N, Gupta S, Agrawal A, Agrawal S,
Diwedi S and Singh J: To study the acceptance of epidural analgesia
for painless labor at a tertiary care centre. Int J Reprod
Contracept Obstet Gynecol. 3:1087–1089. 2014. View Article : Google Scholar
|