Introduction
Polycythemia vera (PV) is a rare and relatively
poorly understood cause of chronic myeloproliferative disorder
characterized by an increased red cell mass, circulating white
blood cells (WBCs), and platelets; in this way, thrombosis and
bleeding are the major complications associated with this disease.
The most common sites of thrombosis and embolization are the
intracranial artery, coronary artery, and abdominal blood vessels
(1). The majority of patients with
PV have Janus kinase 2 (JAK2) mutations, of which ~96% occur in
JAK2V617F (exon 14) and ~2% occur in JAK2 exon 12 (2). A diagnosis of PV is currently made in
accordance with the 2016 World Health Organization criteria and is
based on the composite assessment of clinical and laboratory
features (http://www.bloodjournal.org/content/127/20/2391).
Ischemic colitis (IC) can be described as an ischemic disease of
the colon, which results from decreased blood flow due to various
causes that leads to intestinal wall ischemia, injury or necrosis
(3). The risk factors for IC mainly
include diabetes, hypertension, dyslipidemia, peripheral vascular
disease, aspirin administration, and digoxin or
constipation-inducing medications (4). The main clinical manifestations include
abdominal pain, diarrhea, and hematochezia (5). A reliable diagnosis of IC depends on
the comprehensive evaluation of clinical symptoms, biochemical
tests, radiological examinations, and endoscopic assessments
(6). In certain cases, PV may cause
mesenteric vascular thrombosis, which can lead to ischemic bowel
disease, although uncommon. Cryer reported a case of pathologically
confirmed ischemic bowel disease caused by PV in 1979 (7). In addition, Brada reported a case of IC
caused by acute erythroid leukemia-induced PV in 1998 (8). In the present report, the third known
case of PV-related ischemic bowel disease is described.
Case report
A 59-year-old Chinese male was admitted to The
Fourth Hospital of Hebei Medical University (Shijiazhuang, China)
on July 15, 2017 with complaints of abdominal pain for 2 weeks with
5 days of intermittent hematochezia. A review of the patient's
medical history indicated a PV diagnosis by transient ischemic
attack (TIA) accompanied by a significantly increased WBC count,
hemoglobin (HGB) level, and platelet (PLT) count 9 years prior.
Following treatment with regular aspirin enteric-coated tablets
(100 mg/day) and hydroxyurea (500 mg, three times per day), the
patient's WBC count, HGB level and PLT count were within normal
ranges. The cessation of aspirin and hydroxyurea administration
between early February and early March 2017 induced increases in
WBC count to 22.21×109/l, red blood cell (RBC) count to
4.65×1012/l, HGB level to 165 g/l, and the PLT count to
467×109/l. The reuse of aspirin enteric-coated tablets
and hydroxyurea corrected the blood cell abnormalities; however,
the patient complained of abdominal pain characterized by sustained
spasmodic pain in the middle abdomen, which worsened following
eating, 10 days prior to local hospitalization. These symptoms were
accompanied by small amounts of bloody stools with mucous 7–8 times
per day, 1 day prior to local hospitalization. Routine blood tests
revealed that the patient's WBC count was 15.94×109/l,
the RBC count was 4.27×1012/l, the HGB level was 151
g/l, the PLT count was 403×109/l, and the D-dimer level
was 1 mg/l. The subsequent treatment of hemostasis and antibiotics
did not improve the patient's symptoms of intermittent abdominal
pain or hematochezia following colonoscopy revealing colonic
lesions; therefore, the patient was transferred to The Fourth
Hospital of Hebei Medical University for further treatment with the
following clinical characteristics.
On physical examination, the patient's blood
pressure was 110/69 mmHg, pulse was 85 beats/min, respiration rate
was 21 times/min, and body temperature was 36.9°C. The abdomen was
soft and there was no tenderness with active bowel sounds.
The laboratory examination revealed a WBC count of
10.55×109/l, an RBC count of 3.35×1012/l, an
HGB level of 115.7 g/l, a PLT count of 442×109/l, and a
D-dimer level of 0.156 mg/l. Tumor markers, including
carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA19-9),
carbohydrate antigen 72-4 (CA72-4), and hepatorenal function, were
all within the normal ranges. The fecal occult blood test was
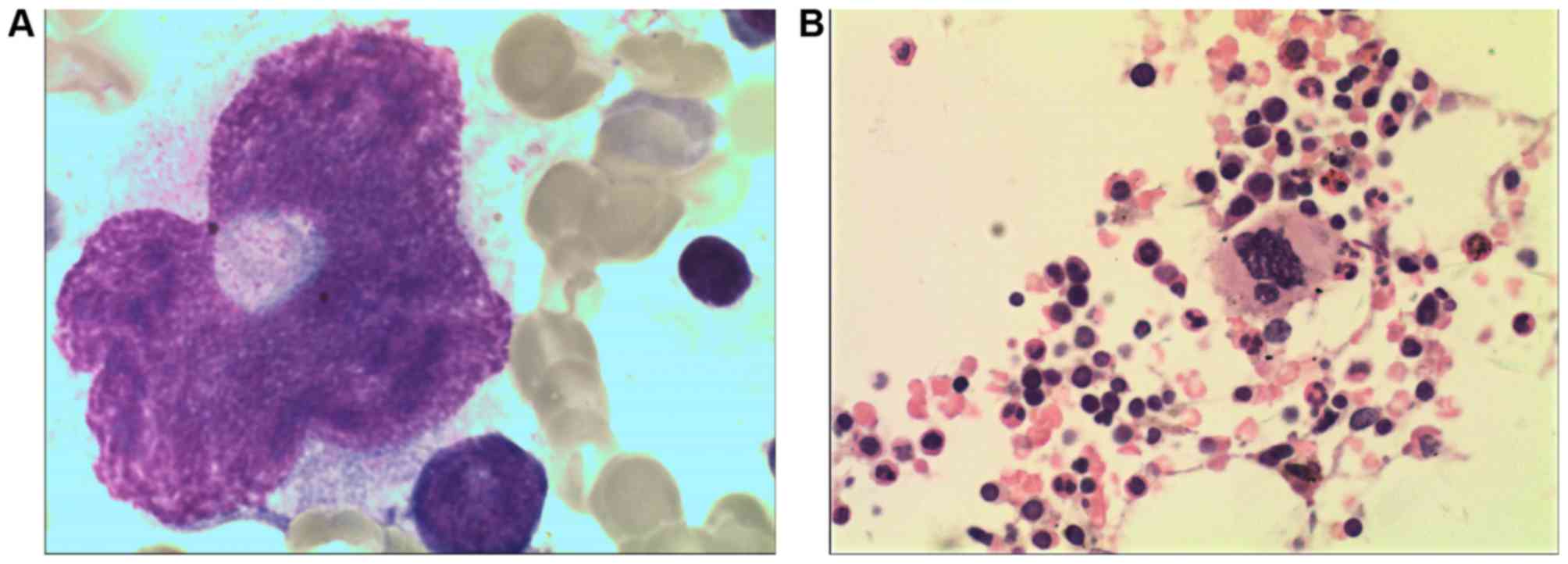
positive, and the bone marrow cytology and biopsy showed an
increased red ratio. The pathological changes were indicative of
myeloproliferative disease, and the patient was JAK2V617F-positive
(Fig. 1A and B).
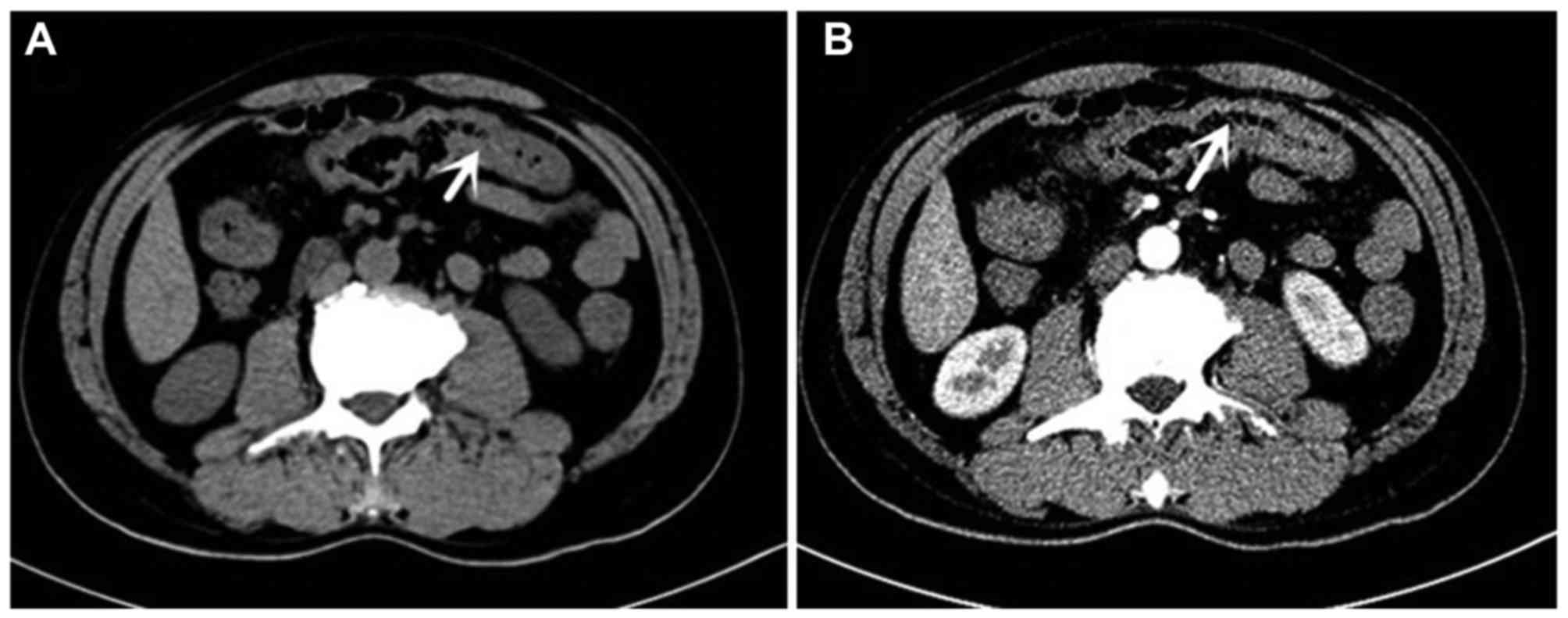
An enhanced abdominal computed tomography (CT) scan
revealed a thickened transverse colon wall, suspected to be due to
malignant lesions (Fig. 2A and B).
The colonoscopy examination revealed segmental and superficial
ulcers, mucosal hyperemia in the cecum, and hepatic flexure at the
transverse colon, which were involved either all around or on one
side of the intestinal wall. The boundary between the lesion and
the normal intestinal mucosa was clear and the remaining colon
mucosa was smooth (Fig. 3A-C). The
colonoscopy yielded a diagnosis of colonic lesions, either due to
Crohn's disease (CD) or IC, and the histopathological diagnosis
indicated mucosal chronic inflammation and inflammatory
granulation.
The patient was treated with mesalazine
enteric-coated tablets (1 g) four times per day for 2 days without
symptomatic relief. The subsequent subcutaneous injection of
low-molecular-weight heparin (100 IU/kg) once every 12 h was
performed for suspected IC. The patient's abdominal pain and
hematochezia were relieved 1 day later. In addition, the fecal
occult blood test was negative 2 days later. Superior and inferior
mesenteric artery CT angiography was performed, which indicated
arteriosclerosis in the superior and inferior mesenteric artery
(Fig. 4). It was recommended that
the patient undergo mesenteric angiography, however, the patient
refused the procedure for financial reasons. The patient was
discharged from hospital 7 days following anticoagulant therapy
with continued administration of aspirin enteric-coated tablets
(100 mg/day) and hydroxyurea (500 mg, three times per day), and
with a regular review of routine blood tests. A colonoscopy review
was performed 1 month later and the entire colon mucous membrane
had returned to normal (Fig.
5A-C).
Discussion
The enhanced abdominal CT scan performed in hospital
detected possible malignant lesions of the transverse colon,
however, the patient complained only of abdominal pain and
hematochezia with no alarming symptoms of weight loss, weakness, or
anorexia; the patient's intestinal tumor markers were normal. In
addition, the histopathology results did not support a diagnosis of
colon cancer. Therefore, the patient was treated with mesalazine
enteric-coated tablets first, based on the results of the
colonoscopy examination, which were indicative of either CD or
IC.
CD is an inflammatory immune-related disease, which
usually manifests between 15–30 years of age, and its clinical
features largely depend on disease location (9). The typical presentations include
abdominal pain, diarrhea, weight loss, and an abdominal mass, and
the complications include strictures, abscesses, and fistulas
(10). The stools are predominantly
loose without blood, with the exception that lesions are involved
in the lower colon and rectum (11).
Endoscopic features include discontinuous ulcerations (skip
lesions), a cobblestone pattern, deep ulcerations, and strictures
(9). The results of histopathology
typically reveal the presence of a non-caseating granuloma. It was
difficult to distinguish between CD and IC from the colonoscopy and
histopathology findings of the patient examined in the present
report.
Although IC mainly occurs in the left hemi-colon
(12), Cryer reported a case of
pathologically confirmed ischemic bowel disease caused by PV, where
the patient's lesion was located in the right hemi-colon (7); this is similar to the case reported
here. Therefore, experimental therapy of low-molecular-weight
heparin was performed following treatment with mesalazine
enteric-coated tablets, based on the risk factors of ischemic bowel
disease including a history of PV, the cessation of aspirin
enteric-coated tablets and hydroxyurea prior to onset of illness,
and the increased WBC count and PLT levels when hematochezia was
identified. In addition, the patient had a TIA 9 years previously
and the incidence of vascular events is approximately doubled in
patients who have a history of previous thrombosis (13). Furthermore, the following clinical
features supported IC: Disease had a sudden onsongside persistent
spasmodic abdominal pain followed by hematochezia; the patient's
abdominal pain was worse on eating and did not ease on defecation;
colonoscopy examination revealed segmental and superficial ulcers,
mucosal hyperemia in the cecum, and hepatic flexure at the
transverse colon, which were either involved all around or on one
side of the intestinal wall; the boundary between the lesion and
the normal intestinal mucosa was clear.
When D-dimer levels are >0.9 mg/l, the
specificity and sensitivity of a diagnosis of ischemic bowel
disease are 82 and 60%, respectively (14). The patient had high D-dimer levels of
1 mg/l when he had bloody stools, which also supports a diagnosis
of ischemic bowel disease. Although CT angiography has 94%
specificity and 96% sensitivity to the diagnosis of occlusive
mesenteric ischemia for the large mesenteric artery, the
observation of branches below the third level of the mesenteric
artery trunk with CT angiography is not reliable (15). Selective mesenteric angiography is
the gold standard for a diagnosis of ischemic bowel disease with a
sensitivity of 90–100% even for the small mesenteric artery
(16), however, the patient refused
mesenteric angiography for financial reasons following a negative
CT scan for thrombus. Following experimental anticoagulation
therapy, the patient no longer reported suffering from abdominal
pain or hematochezia, and the fecal occult blood test was negative.
The patient continued receiving aspirin enteric-coated tablets (100
mg/day) and hydroxyurea (500 mg, three times per day), and the
patient underwent regular review of routine blood tests following
discharge from hospital. The colonoscopy review showed no obvious
anomalies 1 month later, which enabled the exclusion of
nonsteroidal anti-inflammatory drug-related enteropathy caused by
aspirin.
This is the third reported case of IC caused by PV.
The previous two cases were characterized by increased leukocyte
and hematocrit counts, whereas the case described here was
characterized by elevated leukocyte counts and platelet levels. It
is reported that a JAK2 V617 mutation affects the number and
activation of WBCs (17). Landolfi
reported that the risk of thrombosis was significantly increased
when the WBC count was >10×109/l in patients with PV
(13), although the underlying
mechanism of thrombosis remains to be fully elucidated (18).
In conclusion, the present report describes a case
of a patient with IC caused by PV with elevated leukocyte counts
and platelet levels.
Acknowledgements
The authors would like to thank Professor Liu
Yueping (Department of Pathology) and Professor Wang Qi (Department
of Radiology) in The Fourth Hospital of Hebei Medical University
for their kind assistance with the pathological and radiographic
images.
Funding
The present study was supported by the Science and
Technology Project of Hebei (grant no. 162777114D).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SZ collected the data and wrote the manuscript. RL
collected the pathological data. XG collected the radiographic
data. YufZ contributed to the study design and manuscript review.
YueZ collected the endoscopic data. JW collected and revised the
figures. ZG contributed to project design, data collection and
manuscript writing. All authors read and approved the final
manuscript. The authors agreed to be accountable for all aspects of
the study, ensuring that questions related to the accuracy or
integrity of any part of the study are appropriately investigated
and resolved.
Ethics approval and consent to
participate
All procedures were supervised and approved by the
Ethics Committee of The Fourth Hospital of Hebei Medical
University. The patient provided written informed consent prior to
enrolment in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Finazzi G and Barbui T: Evidence and
expertise in the management of polycythemia vera and essential
thrombocythemia. Leukemia. 22:1494–1502. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tefferi A and Barbui T: Polycythemia vera
and essential thrombocythemia: 2017 update on diagnosis,
risk-stratification, and management. Am J Hematol. 92:95–108. 2017.
View Article : Google Scholar
|
|
3
|
Chen M, Remer EM, Liu X, Lopez R and Shen
B: Identification of the distinguishing features of Crohn's disease
and ischemic colitis using computed tomographic enterography.
Gastroenterol Rep (Oxf). 5:219–225. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
FitzGerald JF and Hernandez LO III:
Ischemic colitis. Clin Colon Rectal Surg. 28:93–98. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bradbury MS, Kavanagh PV, Bechtold RE,
Chen MY, Ott DF, Regan FD and Weber TM: Mesenteric venous
thrombosis: Diagnosis and noninvasive imaging. Radiographics.
22:527–541. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stamatakos M, Douzinas E, Stefanaki C,
Petropoulou C, Arampatzi H, Safioleas C, Giannopoulos G,
Chatziconstantinou C, Xiromeritis C and Safioleas M: Ischemic
colitis: Surging waves of update. Tohoku J Exp Med. 218:83–92.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Polycythemia and abdominal pain. Am J Med.
66:321–330. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brada SJ, de Wolf JT, Poppema S and
Vellenga E: Ischaemic colitis and lung infiltrates caused by
extramedullary haematopoiesis in a patient with an acute erythroid
leukaemia following polycythaemia vera. Neth J Med. 52:142–146.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Laass MW, Roggenbuck D and Conrad K:
Diagnosis and classification of Crohn's disease. Autoimmun Rev.
13:467–471. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baumgart DC and Sandborn WJ: Inflammatory
bowel disease: Clinical aspects and established and evolving
therapies. Lancet. 369:1641–1657. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mazal J: Crohn disease: Pathophysiology,
diagnosis, and treatment. Radiol Technol. 85:297–320.
2014.PubMed/NCBI
|
|
12
|
Flynn AD and Valentine JF: Update on the
diagnosis and management of colon ischemia. Curr Treat Options
Gastroenterol. 14:128–139. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Landolfi R, Di Gennaro L, Barbui T, De
Stefano V, Finazzi G, Marfisi R, Tognoni G and Marchioli R;
European Collaboration on Low-Dose Aspirin in Polycythemia Vera
(ECLAP), : Leukocytosis as a major thrombotic risk factor in
patients with polycythemia vera. Blood. 109:2446–2452. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Block T, Nilsson TK, Björck M and Acosta
S: Diagnostic accuracy of plasma biomarkers for intestinal
ischaemia. Scand J Clin Lab Invest. 68:242–248. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kirkpatrick ID, Kroeker MA and Greenberg
HM: Biphasic CT with mesenteric CT angiography in the evaluation of
acute mesenteric ischemia: Initial experience. Radiology.
229:91–98. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brandt LJ and Boley SJ: AGA technical
review on intestinal ischemia. American Gastrointestinal
Association. Gastroenterology. 118:954–968. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
De Stefano V, Za T, Rossi E, Vannucchi AM,
Ruggeri M, Elli E, Micò C, Tieghi A, Cacciola RR and Santoro C:
Leukocytosis is a risk factor for recurrent arterial thrombosis in
young patients with polycythemia vera and essential
thrombocythemia. Am J Hematol. 85:97–100. 2010.PubMed/NCBI
|
|
18
|
Falanga A, Marchetti M, Vignoli A,
Balducci D and Barbui T: Leukocyte-platelet interaction in patients
with essential thrombocythemia and polycythemia vera. Exp Hematol.
33:523–530. 2005. View Article : Google Scholar : PubMed/NCBI
|