Introduction
Chest trauma accounts for approximately 13.5% of all
traumas, and the death directly caused by chest trauma accounts for
20–25% of the death due to all traumas (1). As a chest trauma, multiple rib
fracture, especially fractures of multiple ribs, is easily
complicated with hemothorax or pneumothorax, greatly impacting the
patient's eupnea, or even causing asphyxiation and other extremely
dangerous conditions, so emergency thoracic surgical treatment is
needed (2) In recent years, open
reduction and internal fixation treatment for multiple rib
fracture, especially flail chest rib fracture, has achieved
satisfactory results, and there is also a consensus on some
surgical indications in the industry at the same time (3,4). Because
this operation involves multiple and multisegmental ribs,
satisfactory exposure can only be obtained by cutting a larger
incision in traditional open reduction and internal fixation
surgery for rib fracture. Although video-assisted thoracoscopic
surgery has been applied to intrathoracic exploration, hemostasis
and other treatment for chest trauma and becomes a necessary
technical means in the treatment of chest trauma (3,5–7), its specific application in open
reduction and internal fixation for rib fracture has not been
reported. This is because osseous thorax and chest wall soft
tissues are tightly bound to each other, and some dissociated chest
wall soft tissues currently have no conventional internal
supporting surgical instruments to provide operational space for
surgery. In this study, a self-developed internal support system of
chest wall (ISSW) capable of distracting the muscular chest wall
internally was developed, and the thoracoscope-assisted minimally
invasive open reduction and internal fixation for rib fracture was
successfully achieved. This surgical method can effectively reduce
incision length and damage to chest wall muscles, fully expose
surgical field, decrease surgical trauma, save surgical manpower,
and obtain satisfactory results. This study investigated the
application value of thoracoscope-guided minimally invasive open
reduction and internal fixation for rib fractures.
Patients and methods
Clinical data and grouping
A total of 84 patients undergoing open reduction and
internal fixation for rib fracture in Tianjin Hospital (Tianjin,
China) from January 2017 to December 2017 were selected into the
study, and retrospective analyses were performed. These patients
were divided into the minimally invasive internal fixation for rib
fracture group (n=34) and the traditional incision surgery group
(n=50) according to different surgical methods. Inclusion criteria:
patients diagnosed with rib fracture by the Imaging Department of
Tianjin Hospital before operation, patients with >4 fractures
(fractured ribs), patients not complicated with spinal, limb and
pelvic fractures and abdominal organ injury, patients treated in
the Hospital, patients willing to obey with the arrangements of
medical staff in the Hospital, and patients with complete medical
history. Exclusion criteria: patients with surgical contra
indications, patients complicated with other cardiovascular and
cerebrovascular diseases, patients complicated with other upper
respiratory diseases, patients complicated with other lower
gastrointestinal infections, long-term bedridden patients, patients
with physical disabilities, patients transferred to another
Hospital halfway, and patients receiving treatment from another
Hospital during treatment.
The study was approved by the Ethics Committee of
Tianjin Hospital. All patients or their guardians signed the
informed consent.
Methods
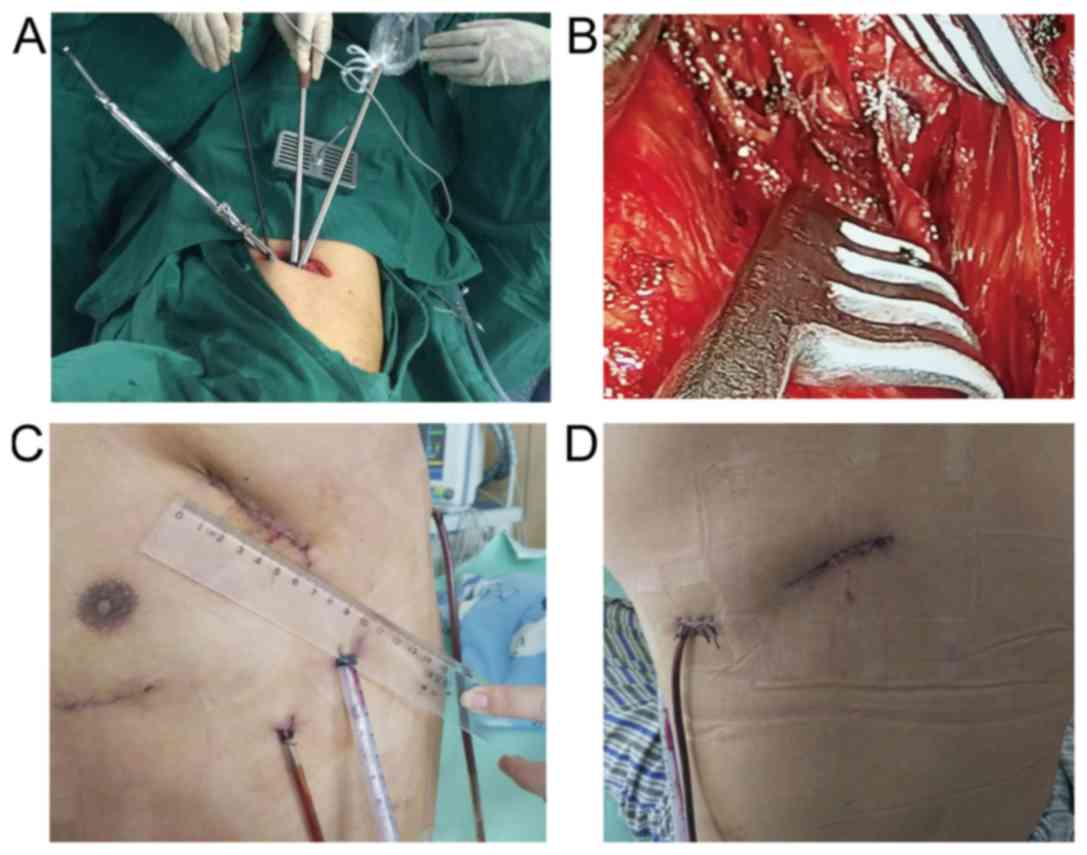
Patients in the minimally invasive group were
treated with minimally invasive internal fixation for rib fracture
using thoracoscope combined with ISSW. Single-lumen endotracheal
intubation was used for general anesthesia. Before operation,
fracture locations were marked on the body surface based on
apparent chest wall pressure pain point and bone friction feeling
in physical examination and presentations on rib three-dimensional
computed tomography (CT). Then, a vertical and incline incision was
cut in the appropriate midpoint of upper and lower broken ends of
rib fractures, closing to the space of chest wall superficial
muscles to the greatest extent. The length and number of incision
depended on the number and location of rib fractures. Usually,
incision length was 6–12 cm. Muscle space was fully used to
dissociate chest wall muscles and cut off partial attachment points
of chest wall muscles and osseous thoraxes, during which cutting
off muscles were avoided as far as possible. ISSW was used to strut
part of the dissociated osseous thoraxes and muscular thoraxes up
and down, and a space therefrom was a thoracoscopic observation
hole to insert into a thoracoscope. After that, space between
osseous and muscular thorax was further dissociated to expose the
fractured ends of a rib. The upper and lower intercostal muscles of
the rib were appropriately stripped off, periostea on both sides of
the broken ends of the rib were separated ~2.0 cm, intercostal
vascular nerves were anatomical separated and protected, and
anatomical reduction of the broken ends of the rib was carried out.
According to the width and shape of the rib where the fracture was
located, an appropriate type of memory alloy rib bone plate (ice
immersion) was selected, shaped, buckled and pressed on both sides
of the broken ends of anatomically reduced fractured rib along the
direction of the rib, and fixed using the special rib plate holding
clamp in ISSW. Next, sterile saline gauze at ~60°C was placed on
the surface of the rib plate, to adduct the jaw to hold the rib,
completing fracture fixation. After operation, a closed thoracic
drainage tube and a wound drainage tube were placed (Fig. 1). Patients in the control group were
treated with traditional large incision internal fixation for rib
fracture. The clinical data, pain score, operating time,
intraoperative blood loss, indwelling time of thoracic tube, total
drainage volume of thoracic tube in 3 days after operation,
indwelling time of wound drainage tube, total drainage volume of
wound drainage tube, length of stay, hospitalization costs,
postoperative complications, C-reactive protein (CRP) and pulmonary
function of patients in both groups were compared. All patients
were followed up for prognosis for 2–4 months via re-examination,
and chest numbness at 1 month after operation was recorded.
Observation indexes
i) General indicators included operating time,
intraoperative blood loss, indwelling time of thoracic tube, total
drainage volume of thoracic tube in 3 days after operation,
indwelling time of wound drainage tube, total drainage volume of
wound drainage tube, length of stay, hospitalization costs, wound
infection and numbness of the affected chest. ⅱ) Rehabilitation
indexes covered pain scores at 3 and 7 days before operation and
during treatment, and preoperative and postoperative CRP values and
pulmonary function in the two groups of patients.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
19.0 software (IBM Corp., Armonk, NY, USA) was used for statistical
analysis. Measurement data are expressed as (means ± SD), and
t-test was employed. Chi-square test was used for enumeration data.
P<0.05 indicates that the difference was statistically
significant.
Results
Clinical data
Comparisons of the clinical data of the two groups
of patients showed that there were no obvious differences in sex,
age, smoking, drinking, exercise habit, nationality, place of
residence, number of rib fracture, pneumothorax and location of rib
fracture of patients between them (p>0.05), suggesting that the
two groups of patients are comparable (Table I).
 | Table I.Clinical data of the two groups of
patients (n, %). |
Table I.
Clinical data of the two groups of
patients (n, %).
| Variables | Minimally invasive
group (n=34) | Traditional group
(n=50) | χ2 | P-value |
|---|
| Sex |
|
| 1.65 | 0.44 |
| Male | 22 (64.7) | 36 (72.0) |
|
|
|
Female | 12 (35.3) | 14 (28.0) |
|
|
| Age (years) |
|
| 2.36 | 0.32 |
|
<45 | 26 (76.5) | 35 (70.0) |
|
|
| ≥45 | 8 (23.5) | 15 (30.0) |
|
|
| Smoking |
|
| 3.17 | 0.28 |
| Yes | 24 (70.6) | 35 (70.0) |
|
|
| No | 10 (29.4) | 15 (30.0) |
|
|
| Drinking |
|
| 4.24 | 0.16 |
| Yes | 18 (52.9) | 29 (58.0) |
|
|
| No | 16 (47.1) | 21 (42.0) |
|
|
| Exercise habit |
|
| 3.67 | 0.28 |
| Yes | 14 (41.2) | 22 (44.0) |
|
|
| No | 20 (58.8) | 28 (56.0) |
|
|
| Nationality |
|
| 2.25 | 0.46 |
| Han | 31 (91.2) | 48 (96.0) |
|
|
|
Minority | 3 (8.8) | 2 (4.0) |
|
|
| Place of
residence |
|
| 2.95 | 0.36 |
| City | 18 (52.9) | 27 (54.0) |
|
|
|
Countryside | 16 (47.1) | 23 (46.0) |
|
|
| No. of rib
fractures |
|
| 2.36 | 0.41 |
|
<8 | 24 (70.6) | 37 (74.0) |
|
|
| ≥8 | 10 (29.4) | 13 (26.0) |
|
|
| Pneumothorax |
|
| 2.88 | 0.37 |
| Yes | 8 (23.5) | 10 (20.0) |
|
|
| No | 26 (76.5) | 40 (80.0) |
|
|
| Location of rib
fracture |
|
| 3.34 | 0.25 |
|
Unilateral | 28 (82.4) | 38 (76.0) |
|
|
|
Bilateral | 6 (17.6) | 12 (24.0) |
|
|
Comparison of efficacy
There were statistically significant differences in
operating time (145.27±18.80 vs. 112.20±21.40 min, p<0.001),
intraoperative blood loss (51.00±12.66 vs. 78.87±24.98 ml,
p<0.001), indwelling time of thoracic tube (3.48±0.87 vs.
4.23±1.14 days, p=0.003), total drainage volume of thoracic tube at
first 3 days (475.15±137.18 vs. 553.69±148.1 ml, p=0.019),
indwelling time of wound drainage tube (2.24±0.97 vs. 3.48±4.22
days, p<0.001), total drainage volume of wound drainage tube
(145.75±61.03 vs. 248.91±93.95 ml, p<0.001), postoperative
length of stay (5.64±1.11 vs. 7.58±1.15 days, p<0.001), total
hospitalization costs [7.52±0.88 vs. 8.99±1.15 (×10,000) yuan,
p<0.001], cases of wound infection [1 (2.94%) vs. 9 (18.00%),
p=0.044] and cases of chest numbness at 1 month after operation [4
(11.8%) vs. 17 (34.00%), p=0.023] between the minimally invasive
and traditional groups (Table
II).
 | Table II.Comparison of general indexes of
patients between the two groups. |
Table II.
Comparison of general indexes of
patients between the two groups.
| Variables | Minimally invasive
group (n=34) | Traditional group
(n=50) | χ2/t
value | P-value |
|---|
| Operating time
(min) | 145.27±18.80 | 112.20±21.40 | 7.222 | 0.001 |
| Intraoperative blood
loss (ml) | 51.00±12.66 | 51.00±12.66 | −5.882 | 0.001 |
| Indwelling time of
thoracic tube (days) | 3.48±0.87 | 4.23±1.14 | −3.122 | 0.003 |
| Total drainage volume
of thoracic tube at first 3 days (ml) | 475.15±137.18 | 553.69±148.10 | −2.397 | 0.019 |
| Postoperative length
of stay (days) | 5.64±1.11 | 7.58±1.15 | 7.549 | 0.001 |
| Total hospitalization
costs (×10,000 yuan) | 7.52±0.88 | 8.99±1.15 | −6.147 | 0.001 |
| Indwelling time of
wound drainage tube (days) | 2.24±0.97 | 3.48±4.22 | −5.62 | 0.001 |
| Total drainage volume
of wound drainage tube (ml) | 145.75±61.03 | 248.91±93.95 | −5.521 | 0.001 |
| Cases of wound
infection | 1 (2.94%) | 9 (18.00%) | 4.37 | 0.044 |
| Cases of chest
numbness at 1 month after operation | 4 (11.8%) | 17 (34.0%) | 5.336 | 0.023 |
Rehabilitation indicators
Pain scores at 3 and 7 days after operation in the
minimally invasive group were significantly better than those in
the traditional group (p<0.05). CRP at 3 and 7 days after
operation was clearly better in the minimally invasive group
compared with those in the traditional group (p<0.05). Pulmonary
function data at 3 and 7 days after operation in the minimally
invasive group were overtly superior to those in the traditional
group (p<0.05) (Table III).
 | Table III.Comparison of rehabilitation
indicators of patients between the two groups. |
Table III.
Comparison of rehabilitation
indicators of patients between the two groups.
| Variables | Minimally invasive
group (n=34) | Traditional group
(n=50) | χ2/t
value | P-value |
|---|
| Pain score |
| Before
operation | 6.32±1.43 | 6.62±1.07 | −1.088 | 0.280 |
| 3 days
after operation | 57.52±8.92 | 86.74±7.54 | 7.225 | 0.002 |
| 7 days
after operation | 36.75±7.33 | 58.53±6.78 | 7.448 | 0.002 |
| MV (l) |
| Before
operation | 64.56±5.27 | 62.77±4.89 | 0.135 | 0.893 |
| 3 days
after operation | 91.63±7.54 | 86.04±9.69 | 2.756 | 0.007 |
| 7 days
after operation | 116.12±17.39 | 107.68±5.40 | 3.062 | 0.003 |
| FEV1 (%) |
| Before
operation | 1.57±0.36 | 1.49±0.33 | 1.491 | 0.278 |
| 3 days
after operation | 57.90±6.19 | 49.68±5.67 | 6.083 | 0.001 |
| 7 days
after operation | 59.66±6.09 | 55.95±5.11 | −3.971 | 0.001 |
| CRP (mg/l) |
| Before
operation | 12.55±3.27 | 13.47±4.08 | 1.024 | 0.356 |
| 3 days
after operation | 43.51±8.28 | 58.22±6.07 | −9.054 | 0.001 |
| 7 days
after operation | 39.42±8.64 | 46.51±7.10 | −3.971 | 0.001 |
Discussion
Severe chest trauma complicated with multiple rib
fractures often leads to severe pain, softening chest wall and
paradoxical respiration, and it, coupled with hypoxemia caused by
lung contusion, leads to respiratory failure that needs
respirator-assisted respiration, and even threatens life.
Therefore, the fundamental purpose for the treatment of chest
trauma is to fix the chest wall, relieve pain and prevent and cure
chest complications (8). The greater
the number of rib fractures is, the worse the patient's quality of
life becomes (9–11). Currently, many scholars in China and
other countries advocate prompt open reduction and internal
fixation in the treatment of multiple rib fracture, especially
flail chest (12–14). Open reduction and internal fixation
for multiple rib fracture can relieve pain, restore thoracic
anatomy and respiratory function, reduce the incidence of pulmonary
complications, shorten Intensive Care Unit (ICU) mechanical
ventilation time and bed-ridden time, and decrease the use of
high-dose analgesics and antibiotics (15,16). In
addition, it can indirectly reduce gastrointestinal suppression,
decrease the incidence of pulmonary atelectasis and chest
infections, and lower death rate by reducing complications
(17). Internal fixation for rib
fracture can restore thoracic integrity and stability, and
eliminate paradoxical respiration and abnormal stimulation on the
broken ends of fractures, which is a stably optimal choice in the
treatment of rib fracture (18).
Moreover, minimally invasive surgery under ISSW
developed by Tianjin Hospital has been perfected in orthopedic
surgeries with the rapid development of modern medical science and
technology. Therefore, this study screened objects of study
strictly based on the inclusion and exclusion criteria, carried out
experiments and tests in strict accordance with operating
guidelines, seriously and rigorously recorded all data of patients,
and adopted advanced statistical software for processing, so as to
study the advantages of using laparoscope combined with ISSW in the
minimally invasive open reduction and internal fixation compared
with the traditional large incision surgery, providing a reference
and guidance for future clinical treatment of patients with
multiple rib fractures.
The results of this study showed that compared with
the traditional open reduction and internal fixation, the minimally
invasive open reduction and internal fixation for multiple rib
fracture using thoracoscope combined with ISSW not only had less
damage to patients, but also had a significantly better effect.
Based on analyses, this is because the traditional large incision
rib fracture open reduction and internal fixation needs to cut off
partial chest wall muscles and nerves (long thoracic and
thoracodorsal nerve) during operation, damaging some blood vessels
below incisions, thus resulting in a higher incision infection rate
and postoperative dysfunction: limited upper limb, shoulder and
back function, long-term numbness of affected chest. However, open
reduction and internal fixation for multiple rib fracture using
thoracoscope combined with ISSM is a surgical method based on ISSM,
which, compared to conventional surgery, can provide good lighting,
comprehensively probe the tissues and structures around the broken
ends of fractures in an intuitive and clear manner, determine the
specific location, number and severity of fractures, effectively
prevent the injury to intercostal vascular nerves, and reduce
postoperative intrathoracic bleeding and effusion. At the same
time, it does not cut off the chest wall muscles and nerves and can
significantly reduce postoperative complications. It can be used
for surgical opening on anterior, posterior and lateral ribs,
because ISSW is able to go deep into the wound and can be opened
internally. The width of the front of the lower supporting plate is
less than that of the back, so a better surgical incision shape can
be obtained. Moreover, ISSW can also support internally when there
is a small opening in an outside incision, which is convenient for
surgery and avoids contusion of outside muscles of the incision at
the same time, so as to realize the minimally invasive surgery.
There were still shortcomings in the comparison of
efficacy in the treatment of patients with rib fracture between
traditional incision surgery and minimally invasive surgery using
thoracoscope combined with ISSW. For example, all study
participants were of the same race due to limited experimental
conditions and small research object base, so there may be
differences in different ethnic groups. In addition, the subsequent
follow-up time for patients was short, so it was unable to evaluate
the long-term efficacy of the two surgical methods, which will be
constantly improved and perfected in future experiments.
In conclusion, application of thoracoscope combined
with ISSW in minimally invasive internal fixation for rib fracture
can effectively improve the prognosis of patients and reduce the
length of stay and adverse reactions, and has high economic
benefits, which is worthy of popularization and application in
clinical practice.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DW conceived and designed the study. JL, DZ, ZS, LD
and YZ were responsible for the collection and analysis of the
data. HX and PZ interpreted the data and drafted the manuscript.
DW, HX and PZ revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Tianjin Hospital (Tianjin, China). Signed informed consents were
obtained from the patients or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liu CP, Gao JM, Hu P, Li CH, He P, Wang
XL, Xiao X and Zhao XJ: Use of bronchofiberscopy in management of
severe thoracic trauma. Chin J Traumatol. 16:195–198.
2013.PubMed/NCBI
|
|
2
|
Brasel KJ, Moore EE, Albrecht RA, deMoya
M, Schreiber M, Karmy-Jones R, Rowell S, Namias N, Cohen M, Shatz
DV, et al: Western Trauma Association critical decisions in trauma:
Management of rib fractures. J Trauma Acute Care Surg. 82:200–203.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Leinicke JA, Elmore L, Freeman BD and
Colditz GA: Operative management of rib fractures in the setting of
flail chest: A systematic review and meta-analysis. Ann Surg.
258:914–921. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bemelman M, de Kruijf MW, van Baal M and
Leenen L: Rib fractures: To fix or not to fix? An evidence-based
algorithm. Korean J Thorac Cardiovasc Surg. 50:229–234. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang X, Wang L, Zhang H, Li K and Gong X:
Feasibility and application of single-hole video-assisted
thoracoscope in pulmonary peripheral tumors. Oncol Lett.
12:4957–4960. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ben-Nun A, Orlovsky M and Best LA:
Video-assisted thoracoscopic surgery in the treatment of chest
trauma: Long-term benefit. Ann Thorac Surg. 83:383–387. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Milanchi S, Makey I, McKenna R and
Margulies DR: Video-assisted thoracoscopic surgery in the
management of penetrating and blunt thoracic trauma. J Minim Access
Surg. 5:63–66. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pieracci FM, Majercik S, Ali-Osman F, Ang
D, Doben A, Edwards JG, French B, Gasparri M, Marasco S, Minshall
C, et al: Consensus statement: Surgical stabilization of rib
fractures rib fracture colloquium clinical practice guidelines.
Injury. 48:307–321. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Marasco S, Lee G, Summerhayes R,
Fitzgerald M and Bailey M: Quality of life after major trauma with
multiple rib fractures. Injury. 46:61–65. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gordy S, Fabricant L, Ham B, Mullins R and
Mayberry J: The contribution of rib fractures to chronic pain and
disability. Am J Surg. 207:659–663. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shulzhenko NO, Zens TJ, Beems MV, Jung HS,
O'Rourke AP, Liepert AE, Scarborough JE and Agarwal SK: Number of
rib fractures thresholds independently predict worse outcomes in
older patients with blunt trauma. Surgery. 161:1083–1089. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Slobogean GP, MacPherson CA, Sun T,
Pelletier ME and Hameed SM: Surgical fixation vs non-operative
management of flail chest: A meta-analysis. J Am Coll Surg.
216:302–311. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pieracci FM, Rodil M, Stovall RT, Johnson
JL, Biffl WL, Mauffrey C, Moore EE and Jurkovich GJ: Surgical
stabilization of severe rib fractures. J Trauma Acute Care Surg.
78:883–887. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marasco SF, Davies AR, Cooper J, Varma D,
Bennett V, Nevill R, Lee G, Bailey M and Fitzgerald M: Prospective
randomized controlled trial of operative rib fixation in traumatic
flail chest. J Am Coll Surg. 216:924–932. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wada T, Yasunaga H, Inokuchi R, Matsui H,
Matsubara T, Ueda Y, Gunshin M, Ishii T, Doi K, Kitsuta Y, et al:
Effectiveness of surgical rib fixation on prolonged mechanical
ventilation in patients with traumatic rib fractures: A propensity
score-matched analysis. J Crit Care. 30:1227–1231. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Doben AR, Eriksson EA, Denlinger CE, Leon
SM, Couillard DJ, Fakhry SM and Minshall CT: Surgical rib fixation
for flail chest deformity improves liberation from mechanical
ventilation. J Crit Care. 29:139–143. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fowler TT, Taylor BC, Bellino MJ and
Althausen PL: Surgical treatment of flail chest and rib fractures.
J Am Acad Orthop Surg. 22:751–760. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Caragounis EC, Fagevik Olsén M, Pazooki D
and Granhed H: Surgical treatment of multiple rib fractures and
flail chest in trauma: A one-year follow-up study. World J Emerg
Surg. 11:272016. View Article : Google Scholar : PubMed/NCBI
|