Introduction
It is difficult to rule out cholangiocarcinoma in
patients with dilated bile ducts. Therefore, clinicians must
consider primary sclerosing cholangitis (PSC) and immunoglobulin
(Ig)G4-related sclerosing cholangitis (IgG4-SC) as potential
diagnoses in such cases. The incidence of benign stricture of the
hilar bile duct was reported to be approximately 10% of surgically
resected cases involving a preoperative diagnosis of
cholangiocarcinoma (1). Most benign
hilar strictures detected in surgically resected cases involved
PSC, IgG4-SC, or secondary sclerosing cholangitis (SSC). Here, we
report a rare case of idiopathic sclerosing cholangitis, which was
preoperatively diagnosed as cholangiocarcinoma. This case had some
pathological features of SC, but it could not be classified into
either of the reported types of benign SCs. So it was diagnosed as
an idiopathic sclerosing cholangitis. We report this case including
the pathological features about SCs.
Case report
A 73-year-old female presented with high fever and
abdominal pain during follow-up after endoscopic mucosal resection
(EMR) for gastric cancer. On admission, her laboratory findings
were as follows: White blood cell count and C reactive protein
level were elevated to 14,960/µl (neutrophils=92.0%) and 23.55
mg/dl, respectively. In addition, her total bilirubin, aspartate
aminotransferase, and alanine aminotransferase levels were elevated
0.62 mg/dl, 48, and 39 U/l, respectively. Carcinoembryonic antigen
level was within the reference limits, whereas carbohydrate antigen
level was slightly elevated, 68 U/ml. Unfortunately, preoperative
serum IgG4 was not measured. Postoperative serum IgG4 was measured
periodically, but it was within normal range at 10 to 18 mg/dl.
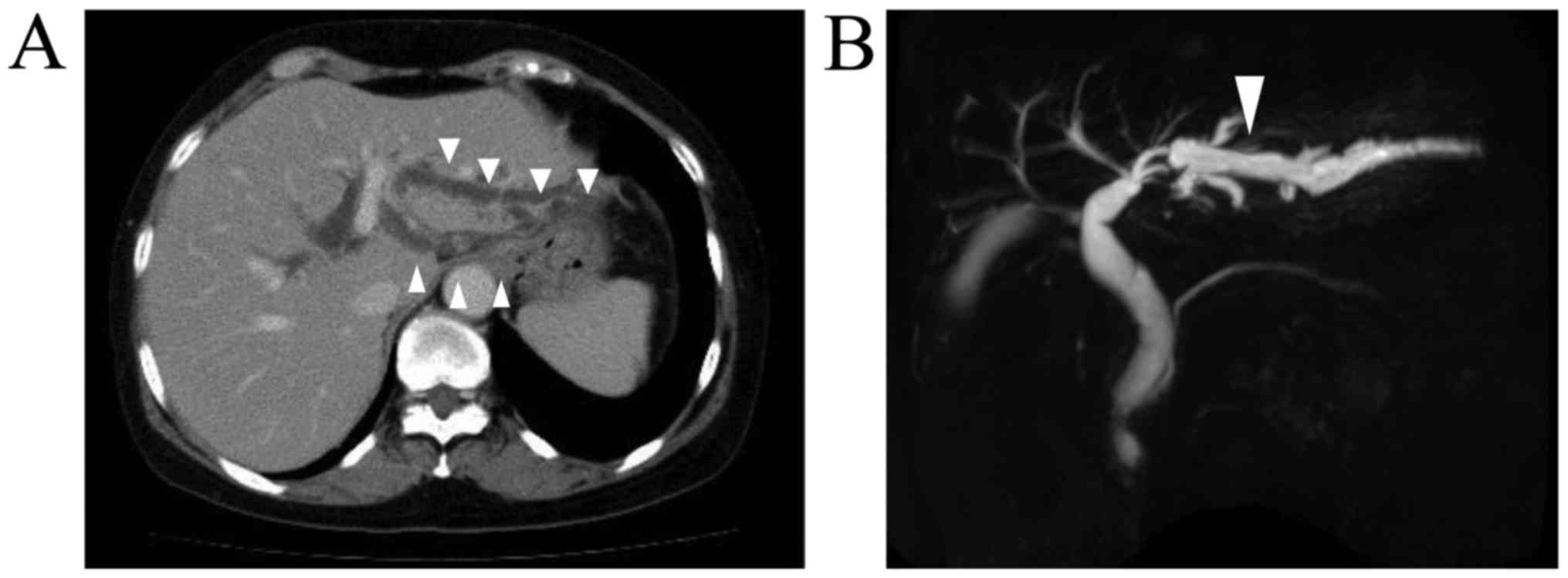
Contrast-enhanced computed tomography and magnetic resonance
cholangiopancreatography showed stenosis and dilation of the
intrahepatic bile duct, in the left hepatic lobe; i.e., within
segments 2 and 3 of the liver (Fig.
1). During percutaneous transhepatic biliary drainage, the
contrast medium that was injected into the drainage tube could not
pass into the center of the bile duct. Endoscopic retrograde
cholangiopancreatography revealed obstruction of the intrahepatic
bile duct. Scrape cytology of this narrow segment of the bile duct
revealed some atypical cells, which were suggestive of hilar
cholangiocarcinoma. In addition, follow-up upper endoscopy was
conducted, and a biopsy of a scar on the patient's stomach caused
by the previous EMR was carried out, which revealed tubular
adenocarcinoma. According to these results, we suspected
intrahepatic cholangiocarcinoma and diagnosed the patient with
locally recurrent gastric cancer. Surgical resection of the liver
and stomach were recommended. A lobectomy of the left side of the
liver, cholecystectomy, and a distal gastrectomy combined with a D2
lymph node dissection were performed. The operation time was 10 h
and 28 min, and 840 ml of intraoperative blood loss occurred. An
examination of the surgical specimens showed that the bile duct was
thickened and extended and the length of stenosis was 2 cm, but
there was no tumor. The patient did not suffer any complications
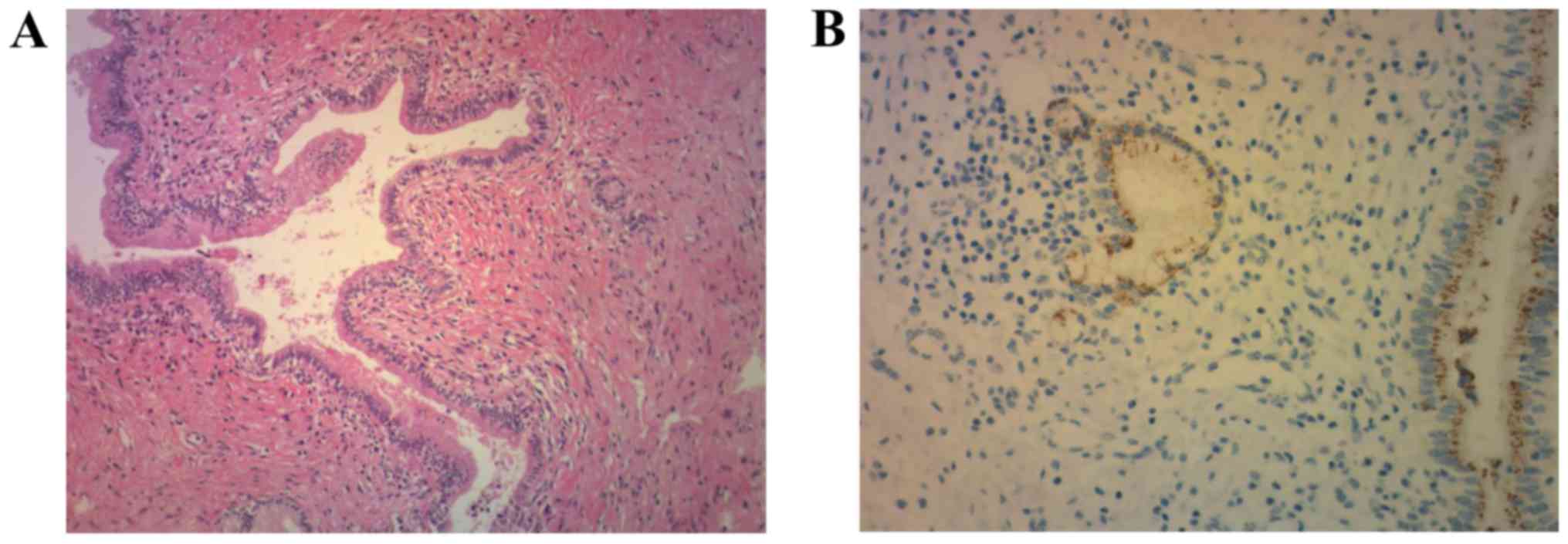
during the postoperative period. A pathological examination of her
liver showed marked fibrosis in the stroma and clusters of lymphoid
cells. The bile duct exhibited irregular dilation and stenotic
compression from the outside, but no thickening of the bile duct
wall was noted. No carcinoma or IgG4-positive plasma cells were
observed, and we did not detect the typical findings of PSC. The
patient had no history of SSC (Fig.
2). Based on these clinical and pathological results, we made a
diagnosis of idiopathic sclerosing cholangitis. Incidentally, the
pathological findings from the patient's stomach showed early
gastric carcinoma, but there was no evidence of a pathological
relationship between the bile duct stenosis and the gastric
cancer.
Discussion
It is difficult to differentiate between
cholangiocarcinoma and benign bile duct stenosis preoperatively. In
this case, we did not detect any obvious malignant findings;
however, based on the progression of the intrahepatic bile duct
stenosis and dilation, we suspected that the patient might have
cholangiocarcinoma and decided to perform a lobectomy of the left
side of the liver.
It remains difficult to distinguish bile duct
malignancy from PSC or IgG4-SC based on imaging features alone. The
presence of pancreatic abnormalities, including a peripancreatic
rind, atrophication, abnormal enhancement, or high T2 signal
intensity, strongly favors a diagnosis of IgG4-SC (2). However, benign bile duct stenosis is
detected at a relatively high frequency during liver surgery
(8–17%) (1). Thus, additional
diagnostic strategies are likely to be vital for distinguishing
between these conditions (3).
PSC, IgG4-SC, and SSC are the most common causes of
benign bile duct stenosis. PSC and IgG4-SC exhibit similar
pathological features, but do differ in some aspects. For example,
the pathological features of PSC include onion-skin fibrosis of the
bile duct, whereas those of IgG4-SC include infiltration by
IgG4-positive plasma cells, obliterative phlebitis, and storiform
fibrosis (4). SSC displays
suppurative inflammation and erosion of the bile duct mucosa during
infections and ischemia. Some representative diseases, such as PSC,
IgG4-SC, and SSC, cause benign bile duct stenosis and dilation.
This case did not display the typical findings of PSC or IgG4-SC,
and the patient did not have a history that was suggestive of
SSC.
Fujita et al reported the pathological
features of 5 cases of benign sclerosing cholangitis of unknown
origin (1). Pathologically,
fibroinflammatory changes and lymphoplasmacytic infiltration were
observed in all 5 cases. Furthermore, these cases were classified
into two types. One type exhibited a thickened bile duct wall and
dense fibrosis as well as the formation of numerous lymphoid
follicles with germinal centers under the mucosal layer. The other
type involved a single focal stricture of the bile duct and subtle
lymphoplasmacytic infiltration. The pathological features of our
case included fibrosis and lymphoplasmacytic infiltration, which
were seen in the previously reported cases, and lymphoid follicle
formation, whereas thickening of the bile duct wall was absent. So,
this case cannot be classified into either of the reported types of
benign sclerosing cholangitis.
Therefore, it cannot be classified into typical
benign bile duct stenosis, and as far as we know, no similar cases
have been reported. So, we consider that this case was a rare case
of idiopathic sclerosing cholangitis involving atypical
pathological findings, such as benign bile duct stenosis.
In conclusion a rare case of idiopathic sclerosing
cholangitis was determined. It is often difficult to differentiate
between cholangiocarcinoma and benign bile duct stenosis
preoperatively. Additional diagnostic strategies are likely to be
vital for distinguishing between these diseases.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SS, TE, MS, HM, RK, KS, TS, FM, TH and HA performed
the operation and perioperative medical treatment. KN performed
preoperative examination and diagnosis. NK performed the
histopathological examination of the liver. AT analyzed the
pathological findings, assisted with patient diagnosis and was a
major contributor in writing the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
participating patient.
Patient consent for publication
Written informed consent for publication was
obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fujita T, Kojima M, Gotohda N, Takahashi
S, Nakagohri T, Konishi M, Ochiai A and Kinoshita T: Incidence,
clinical presentation and pathological features of benign
sclerosing cholangitis of unknown origin masquerading as biliary
carcinoma. J Hepatobiliary Pancreat Sci. 17:139–146. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gardner CS, Bashir MR, Marin D, Nelson RC,
Choudhury KR and Ho LM: Diagnostic performance of imaging criteria
for distinguishing autoimmune cholangiopathy from primary
sclerosing cholangitis and bile duct malignancy. Abdom Imaging.
40:3052–3061. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kalaitzakis E, Levy M, Kamisawa T, Johnson
GJ, Baron TH, Topazian MD, Takahashi N, Kanno A, Okazaki K, Egawa
N, et al: Endoscopic retrograde cholangiography does not reliably
distinguish IgG4-associated cholangitis from primary sclerosing
cholangitis or cholangiocarcinoma. Clin Gastroenterol Hepatol.
9:800–803.e2. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakazawa T, Naitoh I, Hayashi K, Miyabe K,
Simizu S and Joh T: Diagnosis of IgG4-related sclerosing
cholangitis. World J Gastroenterol. 19:7661–7670. 2013. View Article : Google Scholar : PubMed/NCBI
|