Introduction
As a non-steroidal anti-inflammatory drug, aspirin
blocks the production of thromboxane A2 (TXA2) pathway by
arachidonic acid though inhibiting the production of platelet
cyclooxygenase-1 (COX-1), thereby inhibiting the function of
platelets and reducing the formation of thrombosis (1). However, increasing numer of studies
have shown that aspirin alone cannot effectively inhibit platelets
and reduce the incidence rate of cardiovascular-related diseases,
which is also known as aspirin tolerance (2,3). Its
mechanism is unclear and current research suggests that it may be
related to a variety of factors such as accelerated platelet
renewal, genetic factors, and the non-COX-1 activation pathway
(4). Cilostazol, as a quinoline
derivative, is used in combination with aspirin to reduce the
incidence of cardiovascular and cerebrovascular diseases. It has
been reported in most literature that cilostazol can inhibit cyclic
adenosine monophosphate (cAMP) degradation and increase cAMP in
platelets and vascular endothelial cells. Increased cAMP can reduce
the release of adenosine diphosphate (ADP), thereby inhibiting
platelet aggregation and preventing thrombosis (5). At the same time, cilostazol can well
dilate peripheral artery vessels and relieve vascular obstruction,
thereby reducing the incidence rate of atherosclerosis and
thromboangiitis obliterans (5).
Based on other literature, the clinical effects of cilostazol
combined with aspirin on diabetic patients with thromboangiitis
obliterans were explored in this study, so as to provide
preclinical research data for a more effective cure of
patients.
Patients and methods
General data
A total of 90 diabetic patients with thromboangiitis
obliterans admitted to Weifang People's Hospital (Weifang, China)
from August 2015 to June 2017 were selected and divided into the
control (n=45) and the combination group (n=45). The control group
included 28 males and 17 females, aged 48–79 years. The combination
group included 26 males and 19 females, aged 50–82 years. This
study was approved by the Ethics Committee of Weifang People's
Hospital. Signed informed consents were obtained from all
participants before the study. Inclusion criteria of diabetic
patients were in line with the World Health Organization (WHO)
standards in 1999. Thromboangiitis obliterans was diagnosed with
symptoms such as numbness of the limbs, redness and swelling, and
heat pain along the vessel shape and other inflammatory reaction,
and color Doppler ultrasound showed vascular lesions. The two
groups of patients were comparable in complications, age and sex
(P>0.05) (Table I).
 | Table I.Comparison of the basic data of the
two groups of patients. |
Table I.
Comparison of the basic data of the
two groups of patients.
|
| Groups |
|---|
|
|
|
|---|
| Items | Control (n=45) | Combination group
(n=45) |
|---|
| Sex |
| Male | 28 | 26 |
|
Female | 17 | 19 |
| Age (years) | 56.3±6.8 | 58.1±4.7 |
| Complication |
|
Hypertension | 14 | 16 |
|
Hyperlipidemia | 17 | 19 |
|
Myocardial infarction | 7 | 5 |
| Coronary
heart disease | 9 | 11 |
Research methods
The two groups of patients were treated with
corresponding drugs according to their own complications under the
basic treatment of diet and exercise. Patients with hyperglycemia
were given oral antidiabetic drugs or subcutaneous injection of
insulin. Patients with hypertension were given antihypertensive
drugs or intravenous drip diuretics to reduce blood pressure.
Patients with hyperlipidemia were given lipid-lowering drugs chosen
according to the patient's own condition. Based on the basic
treatment, the control group was treated with aspirin at 0.1 g/day,
the combination group was treated with 0.1 g aspirin and cilostazol
at 0.1 g/day at the same time. After 6 weeks of administration, the
clinical data collected from the two groups of patients were
analyzed and compared.
Clinical observation indexes
The clinical data of this study were mainly
collected by the research nurses who were in charge of this study.
Among them, clinical observation indexes included the subjective
symptoms of the patients before and after treatment and whether
there was pain, such as numbness, redness and swelling, heat pain
and other clinical symptoms in the affected limbs of patients with
thromboangiitis. Besides, symptom score criteria (6) were adopted for scoring according to the
degree of severity described by the patients. It was significantly
effective if it declined by >1 point at the end of treatment,
effective if it declined by 1 point at the end of treatment, and
ineffective if it increased by ≥1 point at the end of the treatment
(6). If the affected limbs were
lower, the patients were asked if they had intermittent
claudication and lame distance, and the results were recorded.
Symptom score criteria are shown in Table II. The arterial blood flow,
ankle-brachial index (ABI; contractile pressure ratio of ankle
artery to brachial artery) and 6 min walk test (6MWT) were detected
once a day before and after treatment.
 | Table II.Symptom score criteria. |
Table II.
Symptom score criteria.
| Items | 0 point | 1 point | 2 points | 3 points | 4 points |
|---|
| Intermittent
claudication (M) | >450 | 350–450 | 250–349 | 100–249 | <100 |
| Numbness | No or slight | Occasional | Tolerable | Intolerable | Intolerant |
| Keen feel | No | Occasional | Tolerable | Intolerable | Continuous pain |
| Sense of coldness or
red and swollen | No | Occasional | Often | With other
inflammatory reactions | Continuous,
unbearable |
Experimental test indicators
Before treatment and after 6 weeks of treatment, the
fasting venous blood was extracted from patients by the research
nurses in the early morning, and the specimens were then sent to
the Clinical Laboratory to be detected by a specialized laboratory
technician. Red blood cell lysate was added into the blood samples
to remove red blood cells, the serum was separated after
coagulation, the supernatant was taken by centrifugation at 2,500 ×
g at 4°C for 10 min, and then the concentrations of various
inflammatory factors, such as interleukin (IL)-6, IL-8, matrix
metalloprotease (MMP)-2 and MMP-9, were determined by
double-antibody sandwich enzyme-linked immunosorbent assay (ELISA).
The detection procedures were performed according to the
manufacturer's instructions.
Statistical analysis
The data in this study were statistically analyzed
by GraphPad Prism 6.0 (GraphPad Software, Inc., La Jolla, CA, USA).
The quantitative data were analyzed by t-test, and the data were
expressed as mean ± SD. P<0.05 indicates that the difference is
statistically significant.
Results
Comparison of clinical scores of the
two groups of patients before and after treatment
There was no statistical difference in clinical
scores between the two groups of patients before treatment, and the
scores were comparable. After treatment, the clinical symptoms such
as numbness, intermittent claudication, pain, and sense of coldness
or redness and swelling of patients in the combination group were
significantly improved compared with those in the control group,
and the differences were statistically significant (P=0.01, 0.02,
<0.001 and 0.02, respectively) (Table III), indicating that the effects of
cilostazol combined with aspirin in improving the clinical symptoms
of diabetic patients with thromboangiitis obliterans are better
than those of aspirin alone.
 | Table III.Comparison of clinical scores between
the two groups before and after treatment (mean ± SD). |
Table III.
Comparison of clinical scores between
the two groups before and after treatment (mean ± SD).
|
| Intermittent
claudication | Numbness | Keen feel | Sense of coldness or
red and swollen |
|---|
|
|
|
|
|
|
|---|
| Groups | Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment |
|---|
| Control (n=45) | 2.62±0.19 | 2.09±0.18 | 2.49±0.19 | 2.38±0.18 | 2.77±0.14 | 2.47±0.16 | 2.50±0.15 | 2.29±0.16 |
| Combination
(n=45) | 2.09±0.19 | 1.53±0.14 | 2.67±0.18 | 1.89±0.11 | 2.53±0.15 | 1.73±0.16 | 2.36±0.18 | 1.67±0.21 |
| t | 1.90 | 2.51 | 0.67 | 2.31 | 1.20 | 3.2 | 0.57 | 2.34 |
| P-value | 0.06 | 0.01 | 0.51 | 0.02 | 0.23 | <0.001 | 0.57 | 0.02 |
Comparison of the changes in ABI and
6MWT between the two groups
There were no significant differences in the ABI and
6MWT of the patients between the control and the combination group
before treatment (P>0.05). After treatment, the ABI and 6MWT of
the patients in the control and the combination group were
significantly improved. Among them, the ABI and 6MWT in the
combination were significantly higher than those in the control
group (P<0.001 and <0.001, respectively, P<0.05),
indicating that cilostazol combined with aspirin has a better
effect than aspirin alone (Table
IV).
 | Table IV.Comparison of the changes in ABI and
6MWT in the two groups of diabetic patients with thromboangiitis
obliterans. |
Table IV.
Comparison of the changes in ABI and
6MWT in the two groups of diabetic patients with thromboangiitis
obliterans.
|
| ABI | 6MWT (m) |
|---|
|
|
|
|
|---|
| Groups | Before treatment | After treatment | Before treatment | After treatment |
|---|
| Control |
|
(n=45) | 0.73±0.05 | 1.07±0.07 | 245.1±4.20 | 284.1±3.34 |
| Combination |
|
(n=45) | 0.73±0.05 | 0.91±0.01 | 244.5±5.51 | 316.6±5.70 |
| t | 0.84 | 12.62 | 0.08 | 4.89 |
| P-value | 0.40 | <0.001 | 0.93 | <0.001 |
Comparison of the changes in serum
inflammatory factors and vasoactive substances between the two
groups of patients
Before treatment, there were no significant
differences in the levels of serum inflammatory factors IL-8, IL-6,
C-reactive protein (CRP) and vasoactive substances nitric oxide
(NO) and endothelin-1 (ET-1) of patients between the control and
the combination group, and the levels were comparable. After
treatment, the levels of serum inflammatory factors IL-6, IL-8 and
CRP in the two groups were decreased, while that of vasoactive
substance ET-1 was increased, and the differences were
statistically significant (data not given). Among them, compared
with the control group after treatment, the levels of serum
inflammatory factors of the patients in the combination group were
decreased, and the differences were statistically significant
(P<0.05), indicating that cilostazol combined with aspirin has a
better clinical effect than aspirin alone in reducing serum
inflammatory factors. The levels of NO in the two groups were
increased after treatment, but the difference was not statistically
significant (P>0.05) (Table V).
The mechanism still needs to be further studied.
 | Table V.Comparison of the changes of serum
inflammatory factors IL-6, IL-8, CRP, NO and ET-1 between the two
groups (mean ± SD). |
Table V.
Comparison of the changes of serum
inflammatory factors IL-6, IL-8, CRP, NO and ET-1 between the two
groups (mean ± SD).
|
| IL-8 (µg/l) | IL-6 (pg/ml) | NO (µM/l) | ET-1 (µM/l) | CRP (mg/l) |
|---|
|
|
|
|
|
|
|
|---|
| Groups | Before
treatment | After
treatment | Before
treatment | After
treatment | Before
treatment | After
treatment | Before
treatment | After
treatment | Before
treatment | After
treatment |
|---|
| Control |
|
(n=45) | 114.1±2.76 | 106.5±2.12 | 14.2±0.32 | 11.6±0.36 | 102.6±1.06 | 107.6±1.28 | 196.7±2.93 | 177±2.99 | 7.01±0.17 | 6.26±0.14 |
| Combination |
|
(n=45) | 110.9±2.91 | 93.8±2.29 | 13.4±0.31 | 9.58±0.26 | 100.6±3.52 | 105.6±2.27 | 188.9±3.79 | 140.9±3.56 | 7.23±0.29 | 4.17±0.18 |
| t | 1.90 | 4.07 | 1.83 | 4.58 | 0.55 | 0.55 | 1.63 | 7.77 | 0.37 | 9.29 |
| P-value | 0.06 | <0.001 | 0.07 | <0.001 | 0.58 | 0.58 | 0.11 | <0.001 | 0.71 | <0.001 |
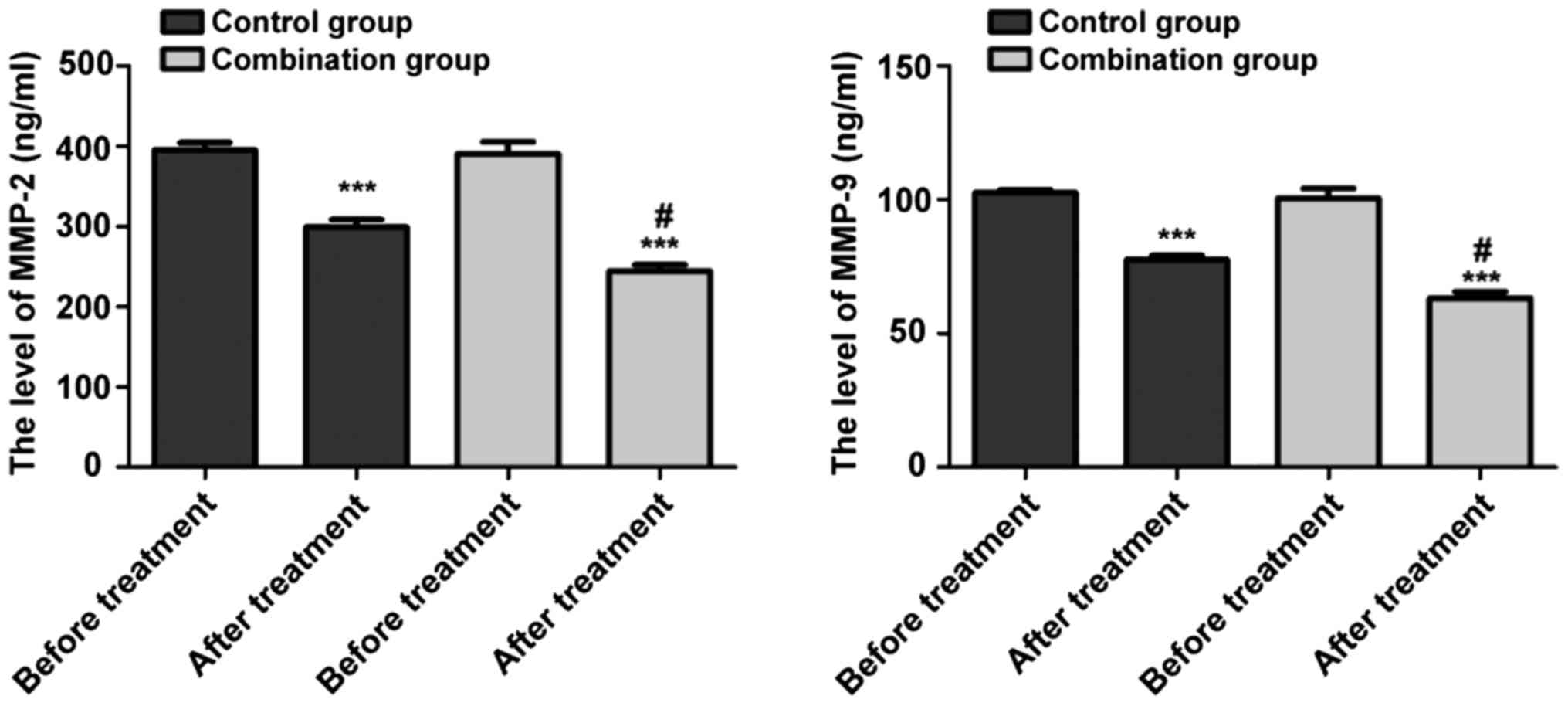
Comparison of the changes in MMP
levels between the two groups of patients
Compared with that before treatment, the levels of
MMP-2 and-9 in the two groups of patients were significantly
decreased (P<0.05), and the effects in the combination group
were better than those in the control group (Fig. 1).
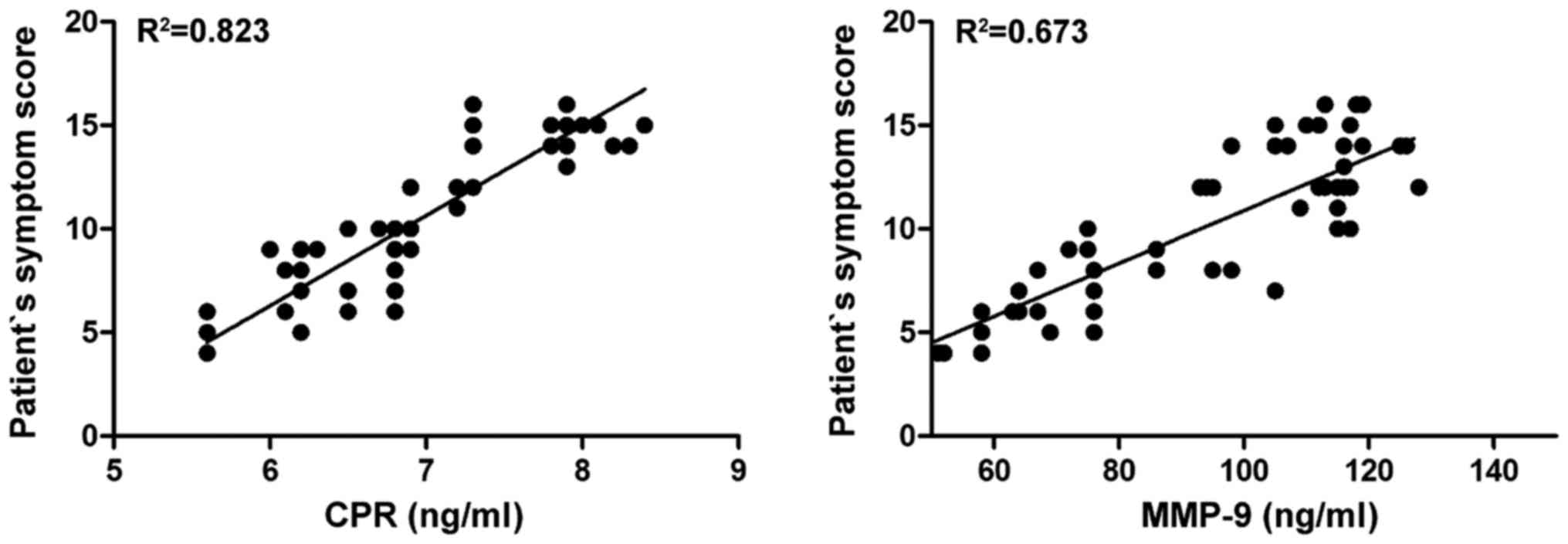
Pearson's correlation analyses of
serum inflammatory factors CRP and MMP-9 with patient's symptom
score
There were positive correlations of the patient's
symptom score with CRP and MMP-9 (P<0.05) (Fig. 2).
Discussion
Thromboangiitis obliterans often occur
independently, and the main manifestation is an occlusive disease
caused by arteriole thrombosis in the limbs (6). Its incidence is not related to age, sex
and vascular location, and the etiology is not clear at present. It
is considered to be an autoimmune disease, which is mainly related
to the overexpression of anti-endothelial cell antibodies and the
increased expressions of anti-neutrophil antibodies and leukocyte
compatible antigens in the body itself (5,7).
Immunological studies have suggested that thromboangiitis
obliterans is associated with the deposition of overactivated
cluster of differentiation 3 (CD3)+ T, CD20+
B cells, and immune proteins such as immunoglobulin A (IgA), IgG,
and IgM on the internal elastic lamina (8). Diabetes mellitus is mainly classified
into type 1 and 2. Type 2 often occurs in obese elderly patients
and often accompanied by other complications. Increased plasminogen
activator inhibitors and von Willebrand factors in the blood
circulation of diabetic patients lead to the increased activity of
fibrin protease and the decreased prostaglandin I2 (PGI2), and
consequently cause systolic/diastolic dysfunction in the vessel and
the increased platelet adhesion and aggregation, thus triggering
the occurrence of thrombus (9). In
addition, hyperglycemia in the blood circulation will lead to the
increase of terminal glycosylation products, which are easy to bind
to specific receptors on the vascular endothelium and further lead
to endothelial dysfunction (10). In
addition, vascular endothelial cells can synthesize and secrete
vasoactive substances such as ET-1 and NO to regulate the
systolic/diastolic function of vascular smooth muscle. The
combination of terminal glycosylation products and vascular
endothelial cells breaks the disorder of endothelial cell function
and causes secretion dysfunction of endothelial cells, and the
imbalance of NO and ET-1 secretion inhibits the active factors in
blood vessel wall and circulating blood to put the circulatory
system in a state of hypercoagulability (10), causing vascular occlusive embolism,
and myocardial infarction, which pose threats to the life of
patients (11,12). Patients with hyperglycemia are often
accompanied by increased stress, endothelial dysfunction and high
expression of IL, which are caused by insulin resistance (13–15).
Aspirin is often used as an antiplatelet agent in
clinical practice to treat acute myocardial infarction and vascular
embolism (16). However, aspirin
will also produce clinical resistance, and excessive consumption
will lead to gastrointestinal hemorrhage, so its application has
some limitations (17,18). Cilostazol, as a phosphodiesterase
inhibitor, can increase the level of adenosine monophosphate and
inhibit the activity of phosphodiesterase in platelets and smooth
muscle endothelial cells, which in turn can counteract platelet
aggregation (19,20). This study aimed to explore the
clinical advantages of cilostazol combined with aspirin and provide
a certain data support for clinical application. In this study,
compared with the control group, cilostazol combined with aspirin
could reduce the duration of intermittent claudication and the
patient's clinical symptoms such as redness and numbness. At the
same time, in laboratory data, cilostazol combined with aspirin can
decrease the serum levels of IL-8, IL-6 and MM-9 and other
inflammatory response factors in patients. These data revealed that
cilostazol combined with aspirin has a better clinical effect than
aspirin alone in the treatment of diabetic patients with
thromboangiitis obliterans, which is worth of further clinical
confirmation and promotion. However, cilostazol combined with
aspirin does not seem to have a significant effect on the
optimization of NO level, which remains to be further verified.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
JY and QZ designed the study and performed the
experiments, JY, SZ, YG and WG collected the data, SZ and PS
analyzed the data, JY and QZ prepared the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China). Signed informed
consents were obtained from all participants before the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
ISIS-2 (Second International Study of
Infarct Survival) Collaborative Group: Randomised trial of
intravenous streptokinase, oral aspirin, both, or neither among
17,187 cases of suspected acute myocardial infarction: ISIS-2.
Lancet. 2:349–360. 1988.PubMed/NCBI
|
|
2
|
Weber AA, Przytulski B, Schanz A, Hohlfeld
T and Schrör K: Towards a definition of aspirin resistance: A
typological approach. Platelets. 13:37–40. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ji AL, Chen WW and Huang WJ: Clinical
study on influences of enteric coated aspirin on blood pressure and
blood pressure variability. Eur Rev Med Pharmacol Sci.
20:5017–5020. 2016.PubMed/NCBI
|
|
4
|
Olszanecka A, Olszanecki R, Korbut R and
Kawecka-Jaszcz K: Aspirin resistance - pharmacological mechanisms
and clinical implications. Kardiol Pol. 62:87–92. 2005.(In Polish).
PubMed/NCBI
|
|
5
|
Eichhorn J, Sima D, Lindschau C, Turowski
A, Schmidt H, Schneider W, Haller H and Luft FC: Antiendothelial
cell antibodies in thromboangiitis obliterans. Am J Med Sci.
315:17–23. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
ATS Committee on Proficiency Standards for
Clinical Pulmonary Function Laboratories, . ATS statement:
Guidelines for the six-minute walk test. Am J Respir Crit Care Med.
166:111–117. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wan J, Yang Y, Ma ZH, Sun Y, Liu YQ, Li GJ
and Zhang GM: Autologous peripheral blood stem cell transplantation
to treat thromboangiitis obliterans: Preliminary results. Eur Rev
Med Pharmacol Sci. 20:509–513. 2016.PubMed/NCBI
|
|
8
|
Kobayashi M, Ito M, Nakagawa A, Nishikimi
N and Nimura Y: Immunohistochemical analysis of arterial wall
cellular infiltration in Buerger's disease (endarteritis
obliterans). J Vasc Surg. 29:451–458. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kimura A, Kobayashi Y, Takahashi M,
Ohbuchi N, Kitamura H, Nakamura T, Satoh M, Sasaoka T, Hiroi S,
Arimura T, et al: MICA gene polymorphism in Takayasu's arteritis
and Buerger's disease. Int J Cardiol. 66 Suppl 1:S107–S113;
discussion S115. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sadik NA, Mohamed WA and Ahmed MI: The
association of receptor of advanced glycated end products and
inflammatory mediators contributes to endothelial dysfunction in a
prospective study of acute kidney injury patients with sepsis. Mol
Cell Biochem. 359:73–81. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Laight DW, Carrier MJ and Anggård EE:
Endothelial cell dysfunction and the pathogenesis of diabetic
macroangiopathy. Diabetes Metab Res Rev. 15:274–282. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
O'Brien JR: Shear-induced platelet
aggregation. Lancet. 335:711–713. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shikano M, Sobajima H, Yoshikawa H, Toba
T, Kushimoto H, Katsumata H, Tomita M and Kawashima S: Usefulness
of a highly sensitive urinary and serum IL-6 assay in patients with
diabetic nephropathy. Nephron. 85:81–85. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Avogaro A, Piarulli F, Valerio A, Miola M,
Calveri M, Pavan P, Vicini P, Cobelli C, Tiengo A, Calò L, et al:
Forearm nitric oxide balance, vascular relaxation, and glucose
metabolism in NIDDM patients. Diabetes. 46:1040–1046. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Steinberg HO, Chaker H, Leaming R, Johnson
A, Brechtel G and Baron AD: Obesity/insulin resistance is
associated with endothelial dysfunction. Implications for the
syndrome of insulin resistance. J Clin Invest. 97:2601–2610. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shimoyama Y, Taki K, Mitsuda Y, Tsuruta Y,
Hamajima N and Niwa T: KLOTHO gene polymorphisms G-395A and C1818T
are associated with low-density lipoprotein cholesterol and uric
acid in Japanese hemodialysis patients. Am J Nephrol. 30:383–388.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zheng AS, Churilov L, Colley RE, Goh C,
Davis SM and Yan B: Association of aspirin resistance with
increased stroke severity and infarct size. JAMA Neurol.
70:208–213. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Paez Espinosa EV, Murad JP and Khasawneh
FT: Aspirin: Pharmacology and clinical applications. Thrombosis.
2012:1731242012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rydzewski A, Urano T, Hachiya T, Kaneko H,
Baba S, Takada Y and Takada A: The effect of a 5HT2 receptor
antagonist sarpogrelate (MCI-9042) treatment on platelet function
in Buerger's disease. Thromb Res. 84:445–452. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ishibashi H, Hayakawa N, Yamamoto H,
Nishikimi N, Yano T and Nimura Y: Thoracoscopic sympathectomy for
Buerger's disease: A report on the successful treatment of four
patients. Surg Today. 25:180–183. 1995. View Article : Google Scholar : PubMed/NCBI
|