Introduction
Fractures in the thoracic spine are a result of
thoracolumbar bone damage caused by external forces (1). These injuries frequently occur in young
patients with high-energy injuries caused by car accidents, falling
from a height and other accidents (2). Merging neural function damage is one of
the most common complications in patients with thoracolumbar
fractures, which frequently results in great difficulties and
challenges in treating these patients (3). Singh et al (4) have demonstrated that cervical and
lumbar spine injuries and rib fractures are significantly
associated with the causes of thoracic spine injury. Additionally,
traumatic thoracic spine fractures often lead to inter- and
intraobserver injury of vertebral, local and segmental kyphosis in
lateral X-rays, and appropriate studies should be performed prior
to providing general recommendations by surgeons (5,6).
Percutaneous minimally invasive surgery (PMIS) is a
small trauma surgery performed using an auxiliary laparoscope,
thoracoscope and other modern medical instruments to perform the
surgery (7,8). PMIS is the most common surgical
procedure used for patients with fractures in the thoracic spine
(9). A meta-analysis has indicated
minimally invasive direct coronary artery bypass graft surgery or
percutaneous coronary intervention for proximal left anterior
descending artery stenosis may decrease the risk for target vessel
interventions (10). Kwan et
al (11) have also demonstrated
that minimally invasive spinal stabilization combined with the use
of fluoroscopic-guided percutaneous screws can be regarded as a
type of palliative surgery in patients with spinal metastasis. In
addition, PMIS presents more advantages compared with open spine
surgery in the treatment of fractures of the thoracolumbar
junction, as suggested by a comparative effectiveness review
(12). Furthermore, PMIS combined
with all methods, including pedicle screw fixation and
vertebroplastry with grafting has been investigated in preventing
grafting for new thoracolumbar burst fractures in a previous study
(13).
In the present study, the benefits of PMIS and
conventional open surgery (COS) in the treatment of patients with
fractures in the thoracic spine were compared. The study observed
that PMIS decreased the postoperative infection rate and
inflammatory responses. It was also demonstrated that the kyphosis,
anterolisthesis, neurological state and hospitalization time were
significantly improved in patients with fractures in the thoracic
spine subsequent to PMIS.
Materials and methods
Patients
The current clinical trial (approval number,
CZHA2010M0430) was conducted in strict accordance with the
recommendations provided in the Guide for the Care and Use of
clinical study of Pharmaceutical Administration Measures for
Implementation (14). The current
study was approved by the ethics committee of Changzheng Hospital
Affiliated to the Second Military Medical University. All patients
were required to provide written informed consent prior to
participation in the current study. In total, 84 patients with
fractures in the thoracic spine (T4-10) who were surgically treated
at Changzheng Hospital Affiliated to the Second Military Medical
University (Shanghai, China) between May 2010 and June 2015 were
enrolled into the present study. Exclusion criteria for patients
with fractures in the thoracic spine were based on the diagnostic
outcomes of radiographs, computed tomography scan and magnetic
resonance imaging (15). The
sensitivity of PMIS and COS for fracture localization was
determined by the actual fracture to fracture diagnosed by PMIS or
COS as described previously (16).
ELISA
Blood samples (10 ml) were obtained from patients
with fractures in the thoracic spine on day 7 after PMIS or COS.
Serum was obtained from blood samples after centrifugation at 4,000
× g for 10 min at 4°C The serum levels of interleukin (IL)-1 (cat
no. 88-7261-22; Thermo Fisher Scientific, Inc., Waltham, MA, USA),
IL-17 ((cat no. BMS2037-2; Thermo Fisher Scientific, Inc.), tumor
necrosis factor α (TNF-α; KHC3014; Thermo Fisher Scientific, Inc.)
and IL-6 (KHC0062; Thermo Fisher Scientific, Inc.) were analyzed
using ELISA kits, according to the manufacturer's protocol.
Subsequently, the serum concentration levels of IL-1, IL-17, TNF-α
and IL-6 were measured by an enzyme microplate reader at 450
nm.
Analysis of physical activity
The physical activity of patients with fractures in
the thoracic spine on day 7 after PMIS or COS was measured as
described previously (17). Briefly,
following the PMIS or COS, the patients received a functional
training program initiated by the nurses in addition to the usual
physiotherapy. The functional training program included walking in
the corridor for 30 min each day, and was targeted to the level of
difficulty relevant for each participant.
Analysis of visual analog scale (VAS)
and Japanese Orthopedic Association (JOA) scores
The VAS and JOA scores for patients with fractures
in the thoracic spine were investigated 7 days following PMIS or
COS. The patients were requested to report their pain levels using
a 10-cm VAS scoring system (18).
All patients were able to self-rate their pain. Furthermore, the
JOA score was used to evaluate the clinical neurological symptoms
and neurological status of the patients as described in a previous
study (19).
Anterolisthesis and neurological
state
Anterolisthesis was observed in patients with
fractures in the thoracic spine on day 7 after PMIS or COS
(20). Briefly, the neurological
state of patients who had undergone PMIS or COS was determined
using the American Spinal Injury Association (ASIA) scale, as
described previously (21). Each
patient's neurologic status was classified between grade 1
(complete paraplegia) and grade 5 (normal neurologic status). The
presence of kyphosis and anterolisthesis was assessed according to
radiographic deformities (22). The
reduction and correction loss of patients with fractures after PMIS
or COS was analyzed as described previously (23).
Statistical analysis
The data are expressed as the mean ± standard error
in each experiment. Statistical differences between groups were
assessed using one-way analysis of variance in six replicate
experiments, along with the post-hoc Dunnett's test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Characteristics and inflammation of
patients with fractures in the thoracic spine subsequent to
receiving PMIS and COS
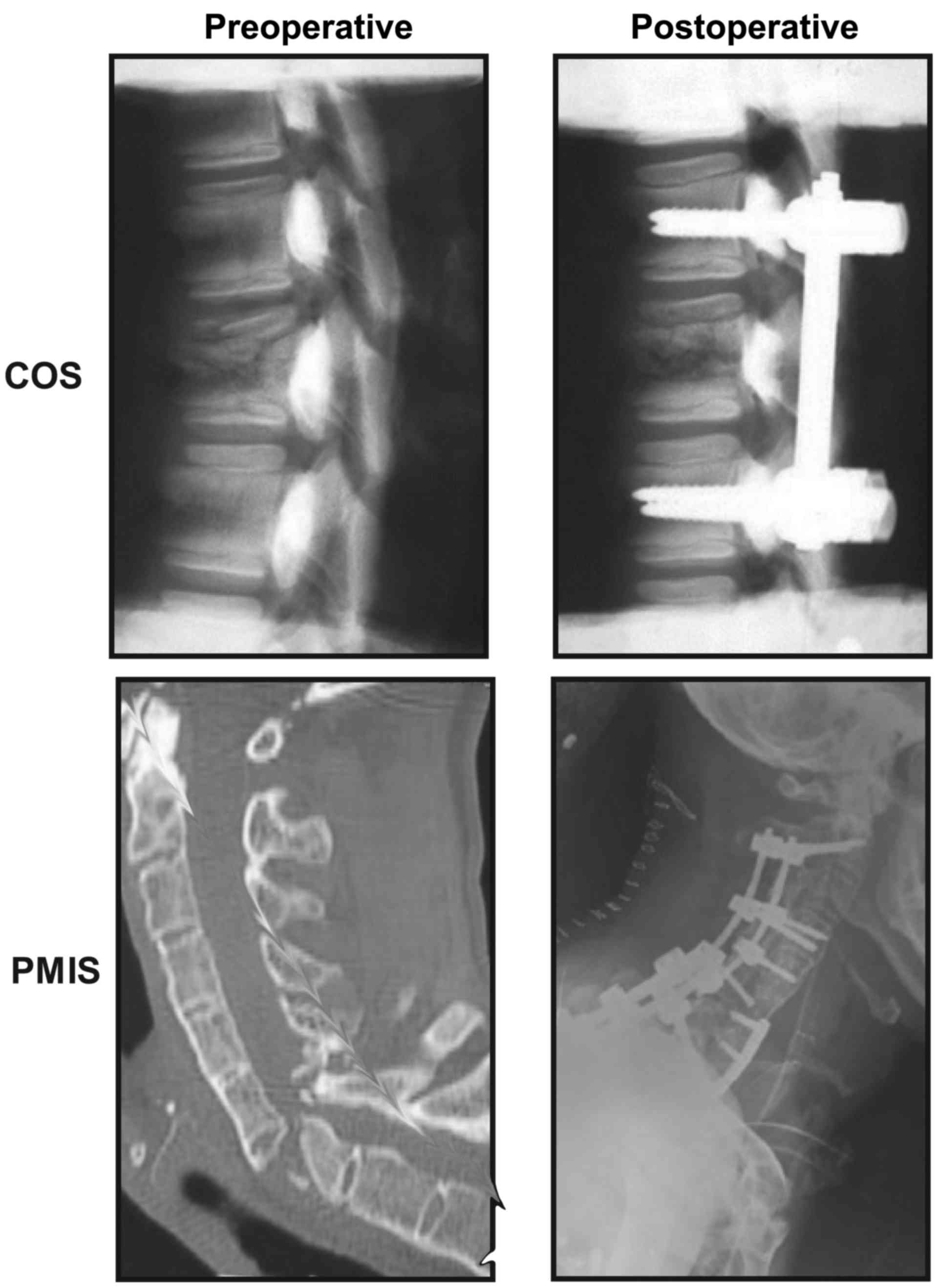
CT scanning confirmed the location of the fractures
in the thoracic spine of patients before and after surgery of PMIS
or COS (Fig. 1). In total, 48
patients (84%) were men and 36 (16%) were women, with a mean age of
32.60±10.28 years. A total of 42 patients received PMIS and 42
patients received COS. The characteristics of patients are listed
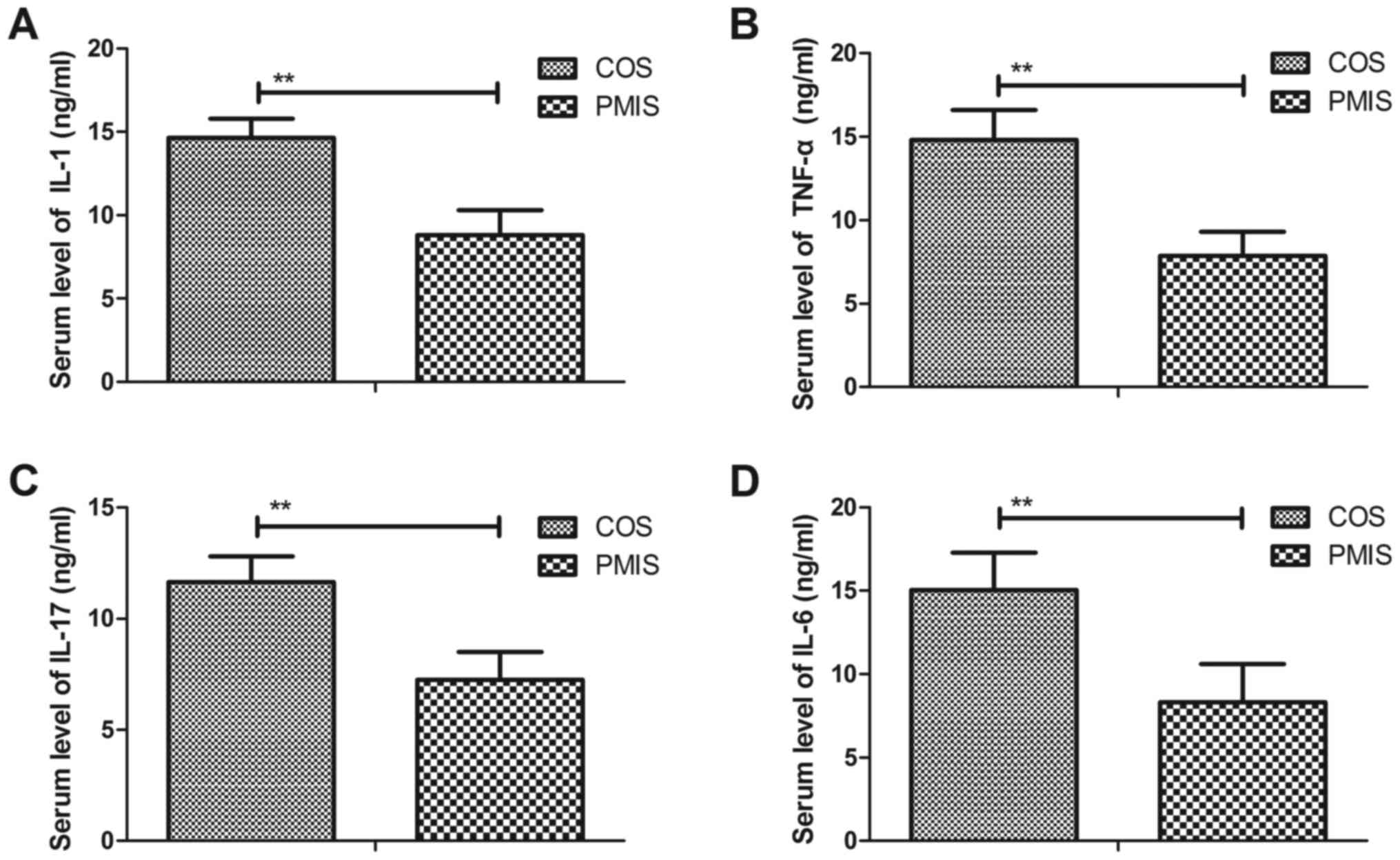
in Table I. On day 7 after PMIS or
COS, the serum levels of inflammatory cytokines in the patients
were analyzed by ELISA. As shown in Fig.
2A-D, the IL-1, TNF-α, IL-17 and IL-6 serum levels were
significantly lower in PMIS patients when compared with the COS
patients (P<0.01). These results indicate that the inflammatory
risk was reduced following PMIS compared with COS for patients with
fractures in the thoracic spine.
 | Table I.Characteristics of patients with
fractures in the thoracic spine (n=84). |
Table I.
Characteristics of patients with
fractures in the thoracic spine (n=84).
| Characteristics | Men | Women |
|---|
| Number | 48 | 36 |
| Age range, years | 22.3–54.8 | 24.6–58.2 |
| Cause of injury,
n |
|
|
| Car
accident | 32 | 21 |
| Fall from
height | 16 | 15 |
| Site of fracture,
n | – | – |
|
T4/T5 | 10 | 8 |
|
T6/T7 | 12 | 12 |
|
T8/T9 | 14 | 7 |
|
T9/T10 | 12 | 9 |
| COS | 24 | 18 |
| PMIS | 24 | 18 |
Comparison of hospitalization time for
fracture localization between patients with fractures in the
thoracic spine receiving PMIS and COS
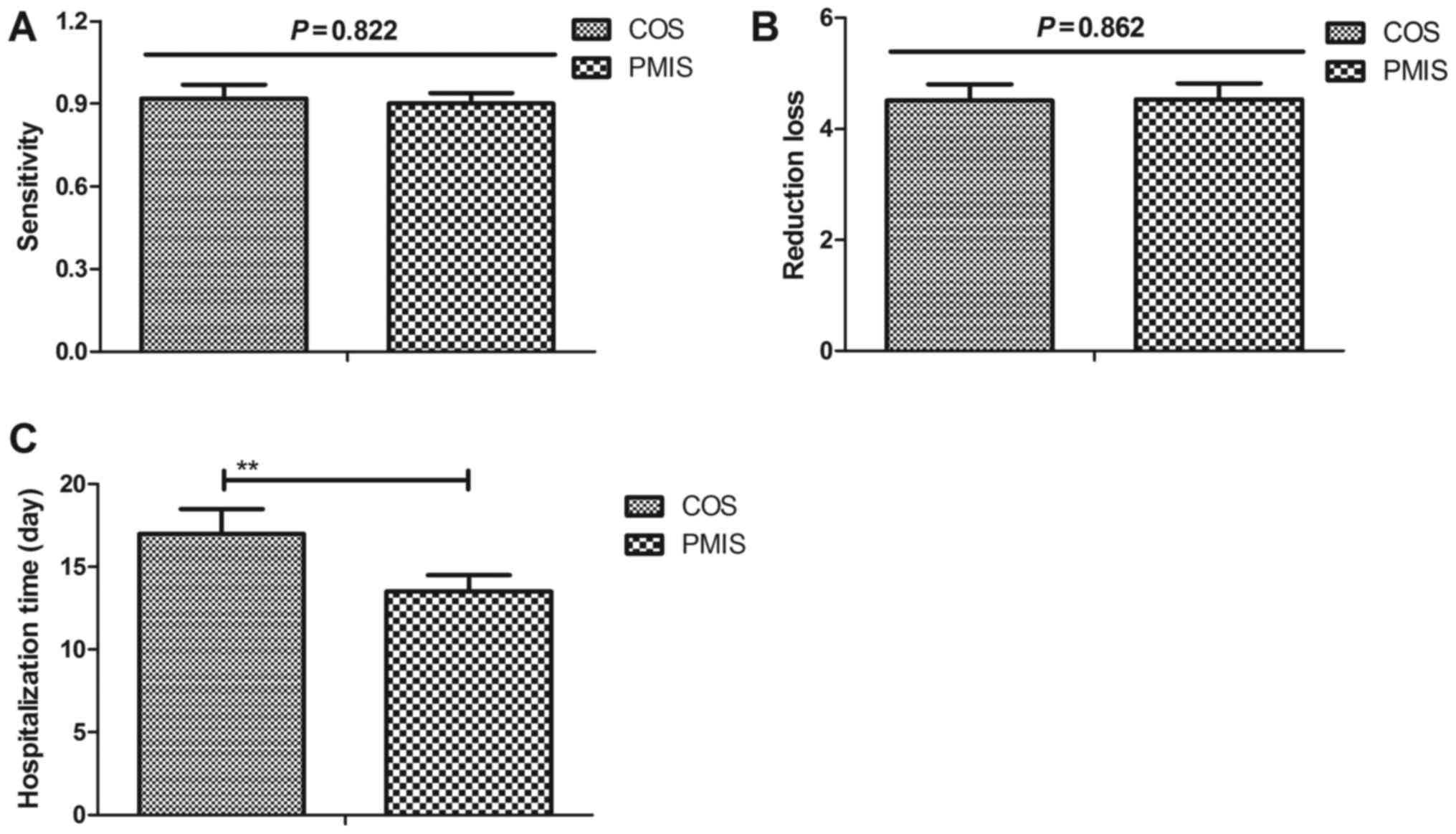
The results demonstrated that the sensitivity for
fracture localization to the correct vertebra was 0.90 in PMIS and
0.92 in COS, and was not significantly different between the two
groups (Fig. 3A; P>0.05). In
addition, the mean values of reduction and correction loss were
similar in the PMIS and COS groups (Fig.
3B; 4.5 degrees; P>0.05). It was also observed that patients
who underwent PMIS required a markedly reduced hospitalization time
compared with patients who underwent COS (Fig. 3C; P=0.026). These observations
indicate that PMIS is beneficial in reducing the hospitalization
time following surgery in patients with thoracic spine
fractures.
Comparison of kyphosis,
anterolisthesis, neurological state and physical activity following
PMIS or COS in patients with fractures in the thoracic spine
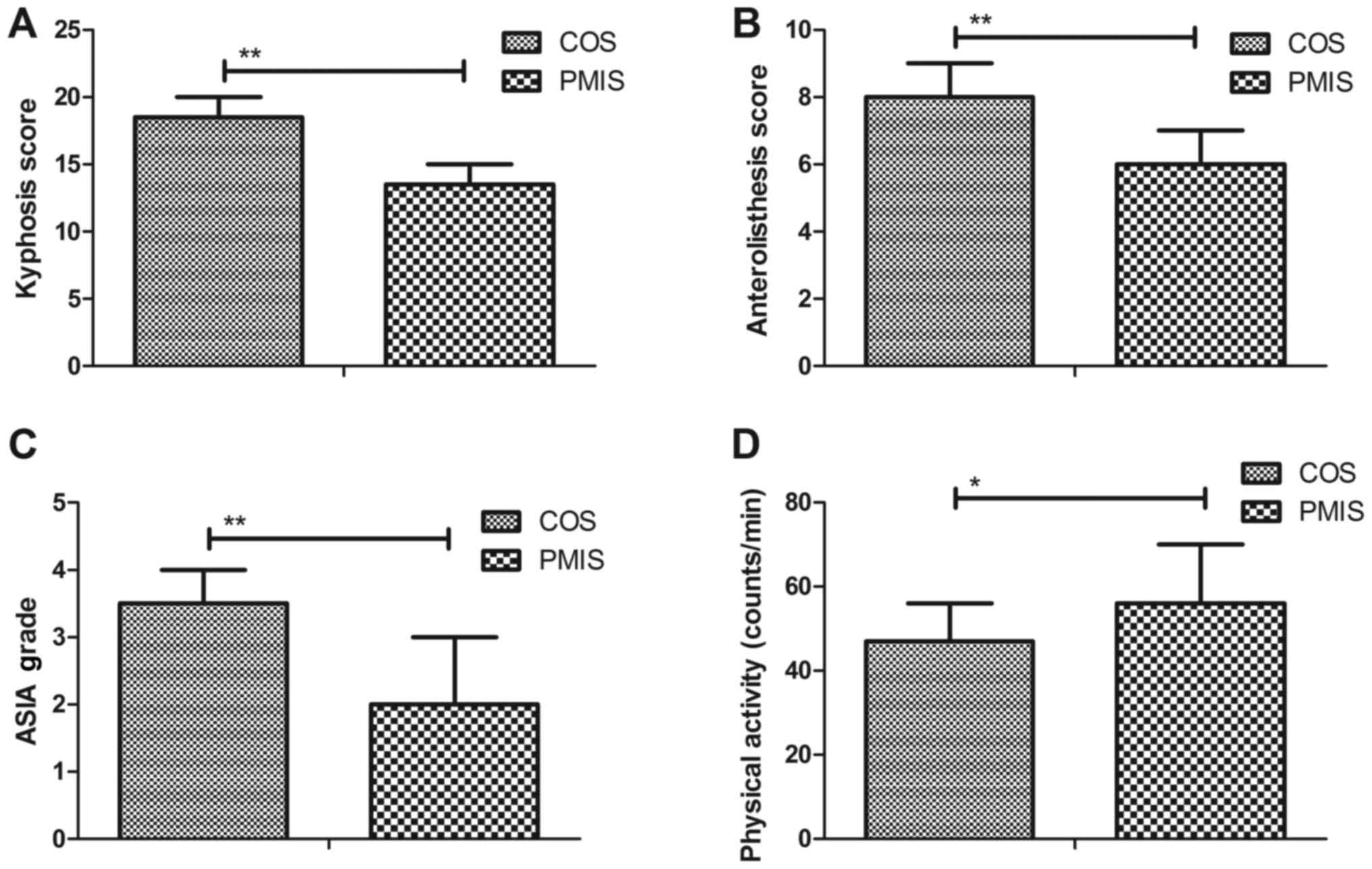
As shown in Fig. 4A,
the kyphosis score was significantly improved in patients
subsequent to PMIS as compared with patients who received COS
(Fig. 4A; P<0.05). It was also
observed that the anterolisthesis and neurological state were
significantly improved in patients receiving PMIS as compared with
patients receiving COS (Fig. 4B and
C; P<0.01). Notably, regarding the level of physical
activity, patients who had undergone PMIS were evidently more
active when compared with the COS patients (P<0.05; Fig. 4D). These findings indicate that PMIS
was able to increase the physical activity of patients with
fractures in the thoracic spine as compared with the COS
procedure.
Comparison of physical condition
following PMIS or COS in patients with fractures in the thoracic
spine
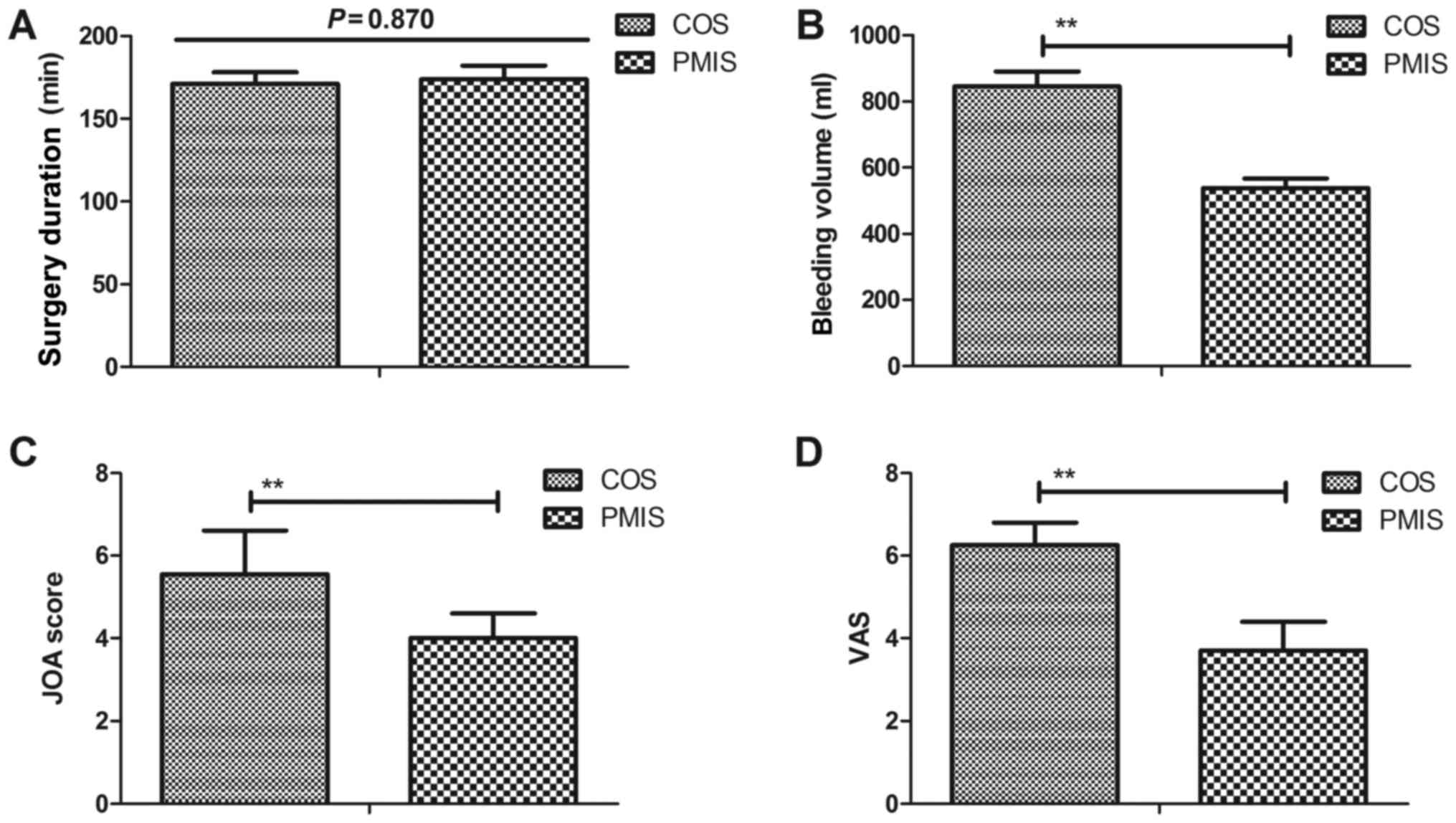
In the present study, the mean follow-up period of
patients was 6 months. The mean surgery duration was ~170 min
(range, 120–294 min) in the PMIS and COS groups, which was not
significantly different the two groups (P=0.870; Fig. 5A). It was observed that the mean
bleeding volume during surgery was 538 ml in the PMIS group and 845
ml in the COS group, with a significantly reduced blood loss
observed during PMIS (Fig. 5B;
P=0.023). Furthermore, the mean JOA and VAS scores in patients who
had undergone PMIS were significantly improved in comparison with
those in patients who had undergone COS (Fig. 5C and D; P < 0.01). Collectively,
these results suggest that PMIS presented a superior performance
when compared with COS in patients with fractures in the thoracic
spine.
Discussion
Traumatic fractures in the thoracic spine are common
worldwide, and are derived from a strong impact force damaging the
sternum (24,25). PMIS is a type of minimally invasive
surgery performed using a laparoscope, thoracoscope or endoscope,
which causes fewer injuries and surgery-associated defects as
compared with the COS procedure (8,26). It
has been suggested that PMIS presents certain advantages for the
treatment of patients with fractures in the thoracic spine
(13,27). Thus, the present study compared the
differences between PMIS and COS performed in patients with
fractures in the thoracic spine. The results indicated that the
inflammatory risk and hospitalization time were significantly
reduced subsequent to PMIS as compared with COS in patients with
fractures in the thoracic spine. It was also observed that the
physical activity, bleeding volume, as well as the mean JOA and VAS
scores, were markedly improved in patients undergoing PMIS compared
with those in patients undergoing COS.
A previous study has indicated the PMIS is a
reliable method in fracture management (28). Pan et al (29) have also indicated that treatment of
children with supracondylar fracture of the humerus using PMIS
decreased the recovery time, hospitalization days and blood
transfusion rate. In addition, minimally invasive posterior
decompression combined with percutaneous pedicle screw fixation has
been demonstrated to achieve a similar effect with COS for the
treatment of thoracolumbar fractures with neurological deficits
(27). Furthermore, the efficacy and
safety of simultaneous combined minimally invasive percutaneous
nephrolithotomy and flexible ureteroscopic lithotripsy was
investigated in the treatment of partial staghorn calculi, and was
observed to be more efficient compared with the conventional
minimally invasive percutaneous nephrolithotomy monotherapy,
without additional procedure-associated complications (30). In the current study, the results
indicated that PMIS presented a superior performance to COS for the
treatment of patients with fractures in the thoracic spine. It was
also demonstrated that the anterolisthesis and neurological state
were significantly improved in patients receiving PMIS as compared
with those receiving COS. Notably, the study findings further
suggested that there were significant differences between PMIS and
COS as determined by the VAS score, JOA score and ASIA grade of the
patient symptoms.
Although a previous review revealed that PMIS has a
comparative effectiveness and safety with COS in the treatment of
fractures of the thoracolumbar junction (12), further investigation on the
effectiveness of PMIS in the treatment of thoracic spine fractures
is required. In the current study, clinical analysis indicated that
PMIS presents more benefits for patients with fractures in the
thoracic spine, while the study also improved the understanding on
the management of thoracic spine injuries. In addition, previous
studies have demonstrated that posterior instruments of PMIS may
improve the therapeutic efficacy for patients with fractures
(31,32). However, additional studies with
larger samples and extended follow-ups are required to further
assess the efficacy of this minimally invasive surgical technique
for the treatment of thoracic spine fracture (33,34). In
the present study, a large number of clinical patients were
recruited to analyze the advantages of PMIS as compared with those
of COS. However, long-term differences (>1 year) between PMIS
and COS in patients with fractures in the thoracic spine were not
compared, which is a limitation of the current study. Additionally,
the study was only able to provide short-term inflammation and
neurologic data, and thus long-term results should be investigated
in future studies.
In conclusion, the present study suggested that PMIS
has a superior performance in patients with thoracic spine
fractures as compared with COS. It is indicated that PMIS is more
beneficial in decreasing inflammation and blood loss for the
treatment of patients with fractures in the thoracic spine.
However, further studies are required to verify these findings in
clinical patients with fractures in the thoracic spine.
References
|
1
|
Beisse R and Verdú-López F: Current status
of thoracoscopic surgery for thoracic and lumbar spine. Part
1General aspects and treatment of fractures. Neurocirugia (Astur).
25:8–19. 2014.
|
|
2
|
Božík M, Magala M, Heger T, Matejička D,
Baka J and Šimko P: Pedicle screw fixation of thoracic spine
fractures. Acta Chir Orthop Traumatol Cech. 81:140–151. 2014.(In
Slovak). PubMed/NCBI
|
|
3
|
van der Jagt-Willems HC, van Munster BC,
Tulner LR and Lems WF: Geriatricians should screen for vertebral
fractures in all individuals by performing X-rays of the thoracic
spine. J Am Geriatr Soc. 62:2027–2029. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Singh R, McD Taylor D, D'Souza D, Gorelik
A, Page P and Phal P: Injuries significantly associated with
thoracic spine fractures: A case-control study. Emerg Med
Australas. 21:419–423. 2009.PubMed/NCBI
|
|
5
|
Gross EA: Computed tomographic screening
for thoracic and lumbar fractures: Is spine reformatting necessary?
Am J Emerg Med. 28:73–75. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ulmar B, Gühring M, Stuby F, Brunner A,
Schmälzle T, Weise K and Badke A: Traumatic thoracic spine
fractures: Inter- and intraobserver reliability of vertebral, local
and segmental kyphosis in lateral X-rays. Z Orthop Unfall.
147:481–486. 2009.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rosengart TK, Feldman T, Borger MA,
Vassiliades TA Jr, Gillinov AM, Hoercher KJ, Vahanian A, Bonow RO
and O'Neill W; American Heart Association Council on Cardiovascular
Surgery and Anesthesia, ; et al Percutaneous and minimally invasive
valve procedures: A scientific statement from the American Heart
Association Council on Cardiovascular Surgery and Anesthesia,
council on clinical cardiology, functional genomics and
translational biology interdisciplinary working group, and quality
of care and outcomes research interdisciplinary working group.
Circulation. 117:1750–1767. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Raffa GM, Pellegrini C, Lentini S,
Perrotta S, Tancredi F, Gaeta R and Viganò M: Minimally invasive
video-assisted surgery for iatrogenic aortic root-to-right atrium
fistula after incomplete percutaneous occlusion of patent foramen
ovale: Case report and review of the literature. J Card Surg.
23:75–78. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ohuchi H, Kyo S, Asano H, Tanabe H, Yokote
Y and Omoto R: Development and clinical application of minimally
invasive cardiac surgery using percutaneous cardiopulmonary
support. Jpn J Thorac Cardiovasc Surg. 48:562–567. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Deo SV, Sharma V, Shah IK, Erwin PJ, Joyce
LD and Park SJ: Minimally invasive direct coronary artery bypass
graft surgery or percutaneous coronary intervention for proximal
left anterior descending artery stenosis: A meta-analysis. Ann
Thorac Surg. 97:2056–2065. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kwan MK, Lee CK and Chan CY: Minimally
invasive spinal stabilization using fluoroscopic-guided
percutaneous screws as a form of palliative surgery in patients
with spinal metastasis. Asian Spine J. 10:99–110. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Barbagallo GM, Yoder E, Dettori JR and
Albanese V: Percutaneous minimally invasive versus open spine
surgery in the treatment of fractures of the thoracolumbar
junction: A comparative effectiveness review. Evid Based Spine Care
J. 3:43–49. 2012.PubMed/NCBI
|
|
13
|
Takami M, Yamada H, Nohda K and Yoshida M:
A minimally invasive surgery combining temporary percutaneous
pedicle screw fixation without fusion and vertebroplasty with
transpedicular intracorporeal hydroxyapatite blocks grafting for
fresh thoracolumbar burst fractures: prospective study. Eur J
Orthop Surg Traumatol. 24 Suppl 1:S159–S165. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tu KK, Zhou XT, Tao ZS, Chen WK, Huang ZL,
Sun T, Zhou Q and Yang L: Minimally invasive surgical technique:
Percutaneous external fixation combined with titanium elastic nails
for selective treatment of tibial fractures. Injury. 46:2428–2432.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Napier RJ and Nolan PC: Diagnosis of
vertebral fractures in post-ictal patients. Emerg Med J.
28:169–170. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pavon JM, Sanders LL, Sloane R and
Colón-Emeric C: Sensitivity of osteoporosis screening guidelines
for eventual hip fracture in older male veterans. Bonekey Rep.
3:5302014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kataoka H, Ikemoto T, Yoshimura A, Shibuya
M, Goto K, Yamashita J, Morita K, Sakamoto J, Nakano J and Okita M:
Association of early physical activity time with pain, activities
of daily living, and progression of vertebral body collapse in
patients with vertebral compression fractures. Eur J Phys Rehabil
Med. 53:366–376. 2017.PubMed/NCBI
|
|
18
|
Rahbek O, Jensen SL, Lind M, Penny JØ,
Kallemose T, Jakobsen T and Troelsen A: Inferior reliability of VAS
scoring compared with International Society of the Knee reporting
system for abstract assessment. Dan Med J. 64(pii):
A53462017.PubMed/NCBI
|
|
19
|
Yonenobu K, Abumi K, Nagata K, Taketomi E
and Ueyama K: Interobserver and intraobserver reliability of the
japanese orthopaedic association scoring system for evaluation of
cervical compression myelopathy. Spine (Phila Pa 1976).
26:1890–1895. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Payer M, Smoll NR, Oezkan N and Tessitore
E: Dynamic transpedicular stabilisation and decompression in
single-level degenerative anterolisthesis and stenosis. Acta
Neurochir (Wien). 156:221–227. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van Middendorp JJ, Hosman AJ, Pouw MH;
EM-SCI Study Group, ; Van de Meent H: ASIA impairment scale
conversion in traumatic SCI: is it related with the ability to
walk? A descriptive comparison with functional ambulation outcome
measures in 273 patients. Spinal Cord. 47:555–560. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ippolito E, Farsetti P, Boyce AM, Corsi A,
De Maio F and Collins MT: Radiographic classification of coronal
plane femoral deformities in polyostotic fibrous dysplasia. Clin
Orthop Relat Res. 472:1558–1567. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bartley CE, Bastrom TP and Newton PO:
Blood loss reduction during surgical correction of adolescent
idiopathic scoliosis utilizing an ultrasonic bone scalpel. Spine
Deform. 2:285–290. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kreinest M, Schmahl D, Grützner PA and
Matschke S: Trisegmental fusion by vertebral body replacement:
Outcome following traumatic multisegmental fractures of the
thoracic and lumbar spine. Unfallchirurg. 121:300–305. 2018.(In
German). PubMed/NCBI
|
|
25
|
Linhares D, Neves N, Ribeiro da Silva M
and Almeida Fonseca J: Analysis of the cochrane review: Pedicle
screw fixation for traumatic fractures of the thoracic and lumbar
spine. Cochrane database syst rev. 2013;05:CD009073. Acta Med Port.
29:297–300. 2016.(In Portuguese).
|
|
26
|
Chiu KM, Lin TY, Chen JS and Chu SH:
Percutaneous cardioplegia delivery using the miniport in minimally
invasive mitral valve surgery. Interact Cardiovasc Thorac Surg.
7:342–343. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang W, Li H, Zhou Y, Wang J, Chu T,
Zheng W, Chen B and Li C: Minimally invasive posterior
decompression combined with percutaneous pedicle screw fixation for
the treatment of thoracolumbar fractures with neurological
deficits: A prospective randomized study versus traditional open
posterior surgery. Spine (Phila Pa 1976). 41 Suppl 19:B23–B29.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zeng BF: Minimally invasive surgery in
fracture management. Chin Med J (Engl). 121:1349–1351.
2008.PubMed/NCBI
|
|
29
|
Pan YW, Wang XM and Pei XQ: Treatment of
children supracondylar fracture of humerus with minimally invasive
surgery. Zhongguo Gu Shang. 22:3432009.(In Chinese). PubMed/NCBI
|
|
30
|
Wen J, Xu G, Du C and Wang B: Minimally
invasive percutaneous nephrolithotomy versus endoscopic combined
intrarenal surgery with flexible ureteroscope for partial staghorn
calculi: A randomised controlled trial. Int J Surg. 28:22–27. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wei FC: Minimally invasive surgery for
vertebral fracture and spinal infection. Biomed J. 36:1532013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jing ZF, Zhao YY, Wang RG, Wang GZ and
Teng LL: Minimally invasive surgery to treat severe
acromioclavicular dislocation combined with coracoid process
fracture. Zhongguo Gu Shang. 23:46–48. 2010.PubMed/NCBI
|
|
33
|
Hu YM and Pang QJ: Effectiveness of
manipulative reduction combined with minimally invasive surgery in
the treatment of osteoporotic vertebral compression fracture: A
meta-analysis. Zhongguo Gu Shang. 28:1042–1047. 2015.PubMed/NCBI
|
|
34
|
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ
and Huang B: Minimally invasive transforaminal interbody fusion
surgery for the old fracture of the thoracolumbar junction. J
Spinal Disord Tech. 27:E55–E60. 2014. View Article : Google Scholar : PubMed/NCBI
|