|
1
|
Dal Maso L, Augustin LS, Karalis A,
Talamini R, Franceschi S, Trichopoulos D, Mantzoros CS and La
Vecchia C: Circulating adiponectin and endometrial cancer risk. J
Clin Endocrinol Metab. 89:1160–1163. 2014. View Article : Google Scholar
|
|
2
|
Wright JD, Barrena Medel NI, Sehouli J,
Fujiwara K and Herzog TJ: Contemporary management of endometrial
cancer. Lancet. 379:1352–1360. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Boer SM, Nout RA, Jürgenliemk-Schulz
IM, Jobsen JJ, Lutgens LC, van der Steen-Banasik EM, Mens JW, Slot
A, Stenfert Kroese MC, Oerlemans S, et al: Long-term impact of
endometrial cancer diagnosis and treatment on health-related
quality of life and cancer survivorship: Results from the
randomized PORTEC-2 trial. Int J Radiat Oncol Biol Phys.
93:797–809. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kurosawa H, Ito K, Nikura H, Takano T,
Nagase S, Utsunomiya H, Otsuki T, Toyoshima M, Nagai T, Tanaka S,
et al: Hysteroscopic inspection and total curettage are
insufficient for discriminating endometrial cancer from atypical
endometrial hyperplasia. Tohoku J Exp Med. 228:365–70. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Crispi CP, Vanin CM, Dibi RP, Kato SK and
Pesssini SA: Postmenopausal bleeding: Findings and accuracy of
hysteroscopy and histopathologic in the diagnosis of endometrial
cancer. J Minimal Invasive Gynecol. 18:S832011. View Article : Google Scholar
|
|
7
|
Bakir B, Sanli S, Bakir VL, Ayas S, Yildiz
SO, Iyibozkurt AC, Kartal MG and Yavuz E: Role of diffusion
weighted MRI in the differential diagnosis of endometrial cancer,
polyp, hyperplasia, and physiological thickening. Clin Imaging.
41:86–94. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bollineni VR, Ytrehauge S,
Bollinenibalabay O, Salvesen HB and Haldorsen IS: High diagnostic
value of FDG-PET/CT in endometrial cancer: Systematic review and
meta-analysis of the literature. J Nucl Med. 57:879–885. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jacobs I, Gentry-Maharaj A, Burnell M,
Manchanda R, Singh N, Sharma A, Ryan A, Seif MW, Amso NN, Turner G,
et al: Sensitivity of transvaginal ultrasound screening for
endometrial cancer in postmenopausal women: A case-control study
within the UKCTOCS cohort. Lancet Oncol. 12:38–48. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Palmieri VO, Santovito D, Marano G,
Minerva F, Ricci L, D'Alitto F, Angelelli G and Palasciano G:
Contrast-enhanced ultrasound in the diagnosis of hepatocellular
carcinoma. Radiol Med. 120:627–633. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dietrich CF, Averkiou MA, Correas JM,
Lassau N, Leen E and Piscaglia F: An EFSUMB introduction into
dynamic contrast-enhanced ultrasound (DCE-US) for quantification of
tumour perfusion. Ultraschall Med. 33:344–351. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang J, Lv F, Fei X, Cui Q, Wang L, Gao X,
Yuan Z, Lin Q, Lv Y and Liu A: Study on the characteristics of
contrast-enhanced ultrasound and its utility in assessing the
microvessel density in ovarian tumors or tumor-like lesions. Int J
Biol Sci. 7:600–606. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
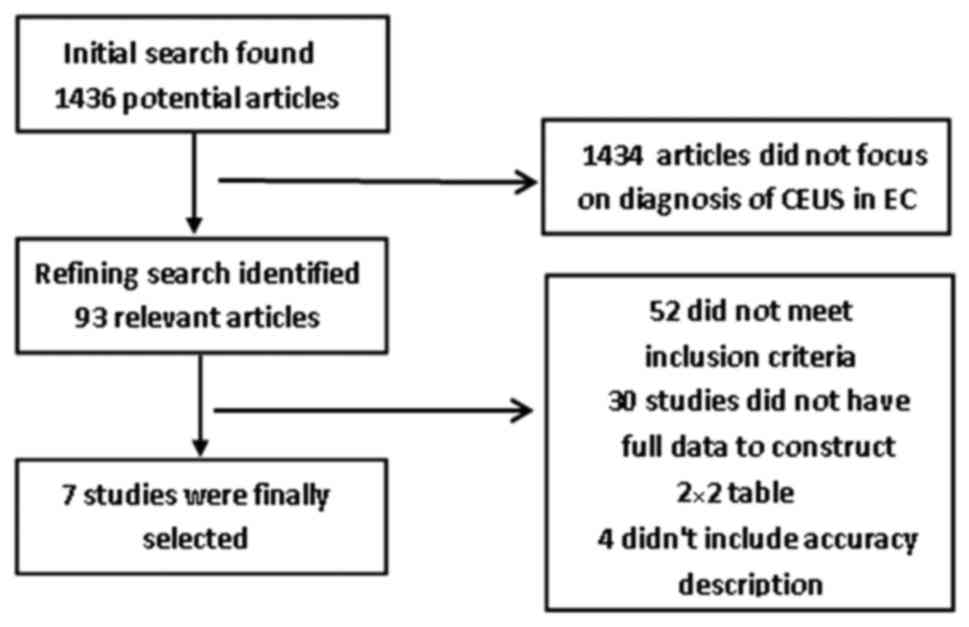
Moher D, Liberati A, Tetzlaff J, Altman DG
and PRISMA Group: Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. Ann Intern Med.
151:264–269. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
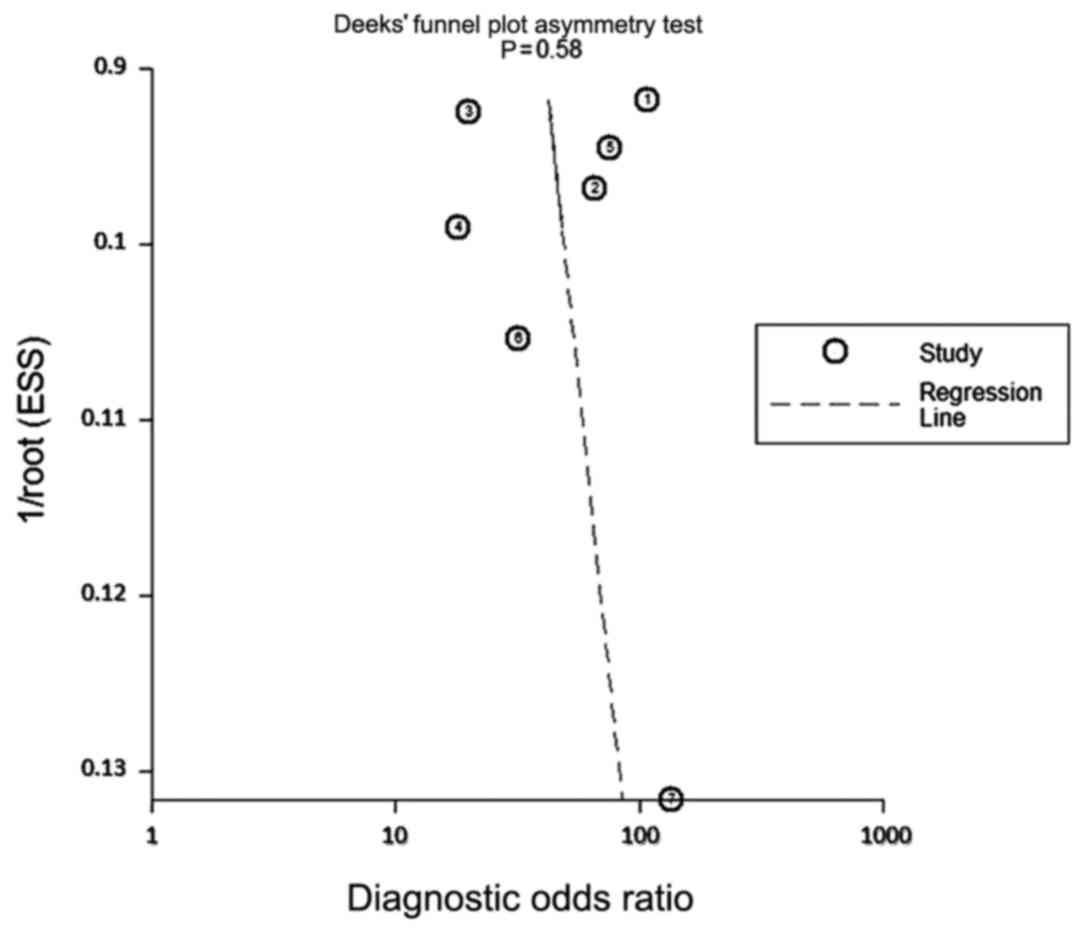
Puli SR, Kalva N, Bechtold ML,
Pamulaparthy SR, Cashman MD, Estes NC, Pearl RH, Volmar FH, Dillon
S, Shekleton MF and Forcione D: Diagnostic accuracy of endoscopic
ultrasound in pancreatic neuroendocrine tumors: A systematic review
and meta-analysis. World J Gastroenterol. 19:3678–3684. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
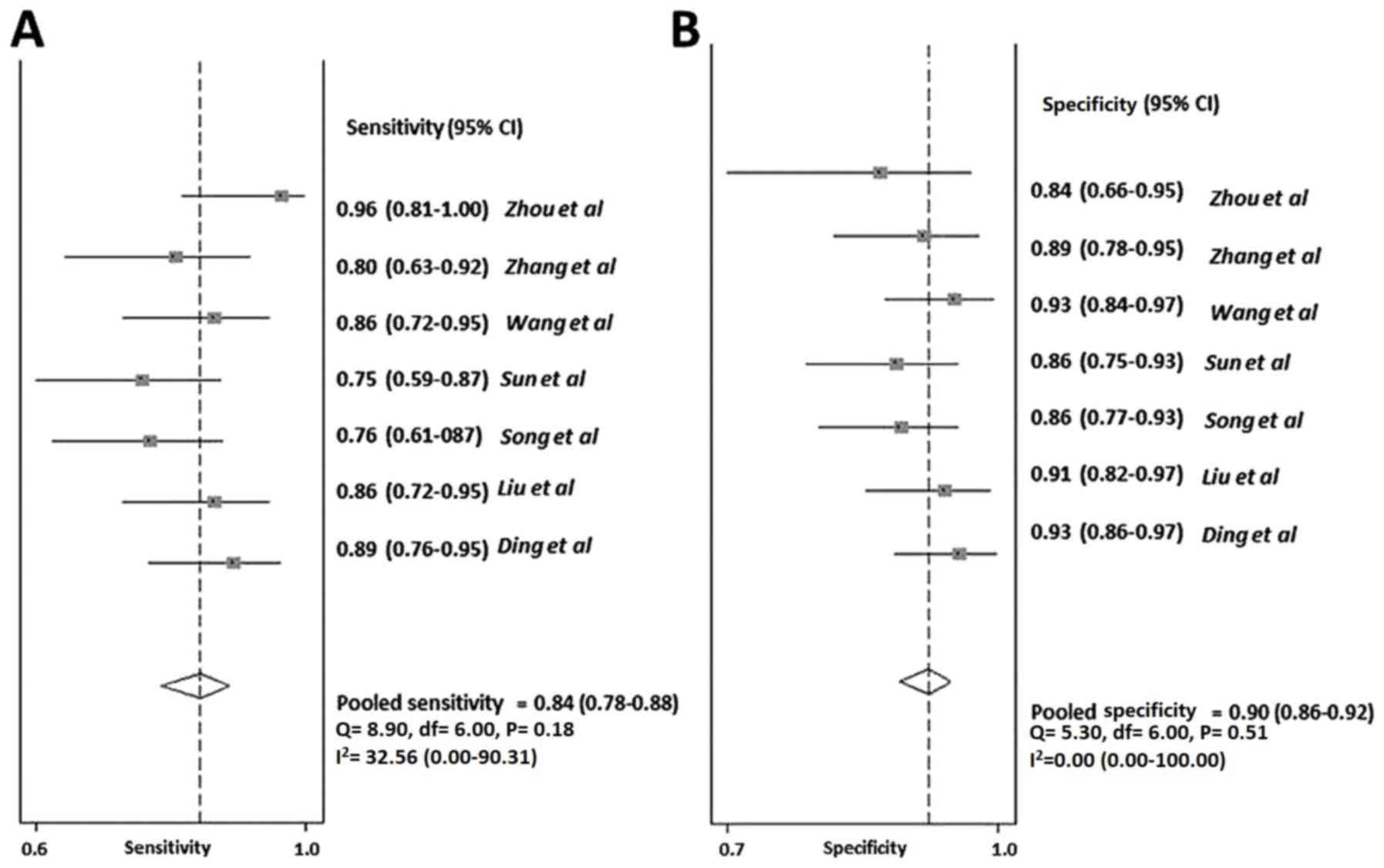
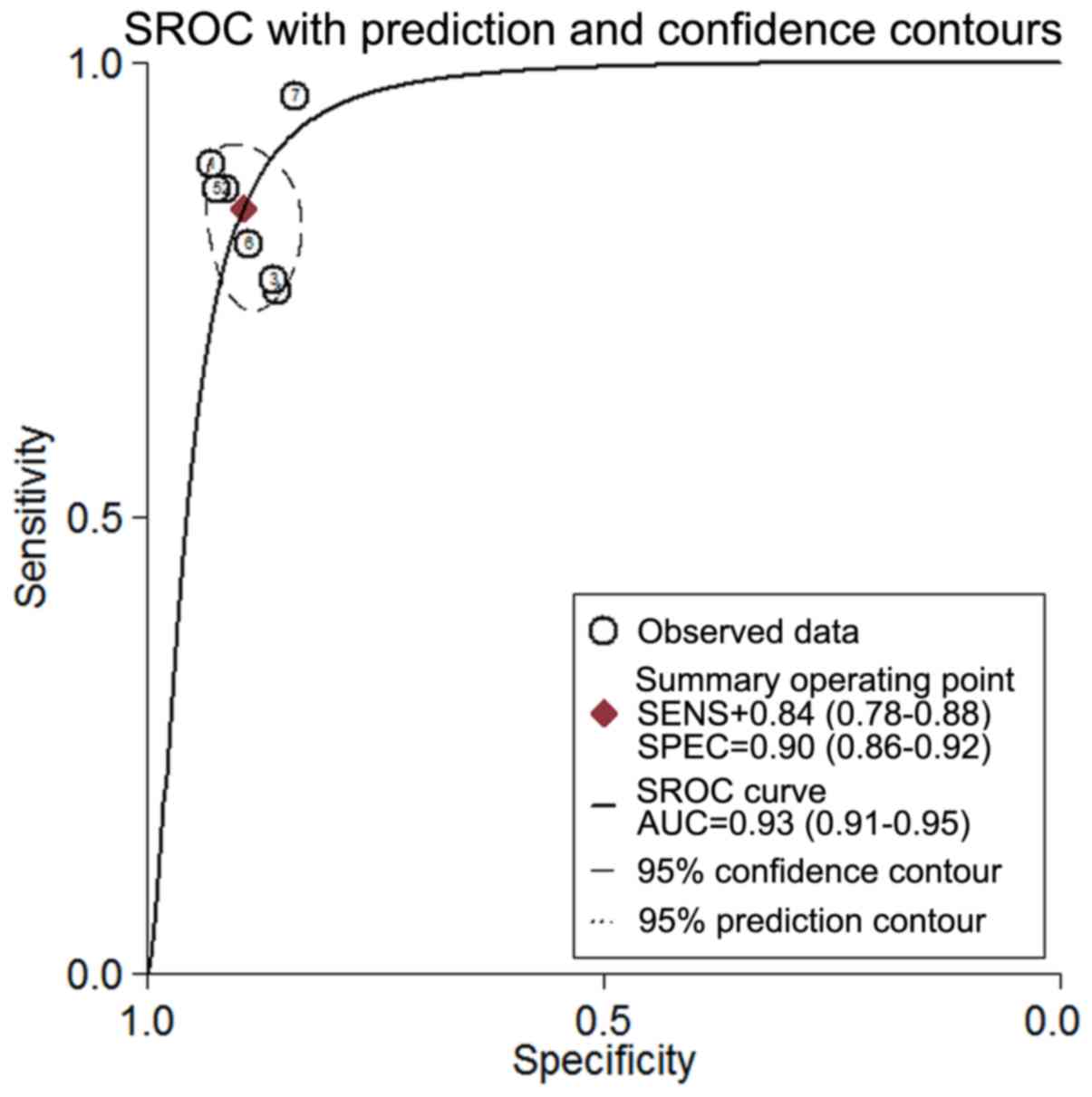
Wang AZ, Liu CY, Xie Q and Wu XP:
Contrast-enhanced ultrasound and magnetic resonance imaging
diagnosis value and differential diagnosis for myometrial invasion
of stage I endometrial carcinoma. Shaanxi Yi Xue Za Zhi. 41:80–83.
2012.(In Chinese).
|
|
16
|
Zhou HL, Xiang H, Duan L, Shahai G, Liu H,
Li XH and Mou RX: Application of combined two-dimensional and
three-dimensional transvaginal contrast enhanced ultrasound in the
diagnosis of endometrial carcinoma. Biomed Res Int.
2015:2927432015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Song Y, Yang J, Liu Z and Shen K:
Preoperative evaluation of endometrial carcinoma by
contrast-enhanced ultrasonography. BJOG. 116:298–299. 2009.
View Article : Google Scholar
|
|
18
|
Ding Y, Guo Y, Guan L, Wang H, Zhang D and
Wang Y: Application value of contrast-enhanced ultrasound for stage
of endometrial carcinoma. Chongqing Med J. 42:2103–2106. 2013.
|
|
19
|
Liu CY, Wang XF, Xie Q, Wan BB, Sheng X,
Wang M and Zhao LH: Diagnostic value of contrast-enhanced
ultrasound for myometrial invasion of stage I endometrial
carcinoma. Chinese J Med Image Technol. 27:1443–1446. 2011.
|
|
20
|
Sun ZJ, Yang JX, Shen K, et al:
Contrast-enhanced ultrasound in the evaluation of myometrial
invasion in endometrial carcinoma. J Reproduct Med. 2008.
|
|
21
|
Zhang XZ, Zhao HY, Peng M and Wei WB:
Application of contrast-enhanced ultrasound in the myometrial
invasion of endometrial carcinoma. J Bengbu Med Col. 36((3)):
285–287. 2011.
|
|
22
|
Lencioni R, Piscaglia F and Bolondi L:
Contrast-enhanced ultrasound in the diagnosis of hepatocellular
carcinoma. J Hepatol. 48:848–857. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhou XD, Ren XL, Zhang J, He GB, Zheng MJ,
Tian X, Li L, Zhu T, Zhang M, Wang L and Luo W: Therapeutic
response assessment of high intensity focused ultrasound therapy
for uterine fibroid: Utility of contrast-enhanced ultrasonography.
Eur J Radiol. 62:289–294. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sconfienza LM, Lacelli F, Gazzo P,
Gandolfo N, Gravano M and Serafini G: Is contrast-enhanced
ultrasound (CEUS) effective in the assessment of outcomes and in
the follow up of uterine fibroids after superselective uterine
fibroids embolization (SUFE) when compared to dynamic magnetic
resonance (MR)? Ultraschall in Der Medizin. 29((S1))2008.
|
|
25
|
Seitz K and Strobel D: A Milestone:
Approval of CEUS for diagnostic liver imaging in adults and
children in the USA. Ultraschall Med. 37:229–232. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
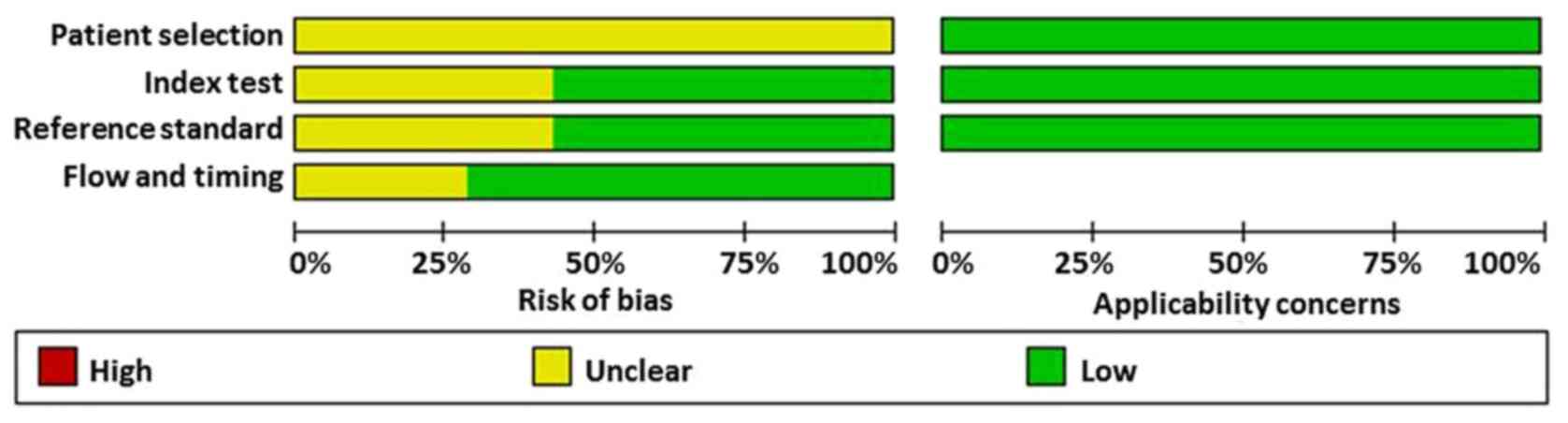
Whiting P, Rutjes AW, Reitsma JB, Bossuyt
PM and Kleijnen J: The development of QUADAS: A tool for the
quality assessment of studies of diagnostic accuracy included in
systematic reviews. BMC Med Res Methodol. 3:252003. View Article : Google Scholar : PubMed/NCBI
|