Introduction
It is known that systemic alpha-blockers determine
relaxation of the smooth muscle situated in the bladder and
prostate, this class of drugs being used in the treatment of benign
prostatic hypertrophy (BPH) (1).
Most of the patients with prostate adenoma use tamsulosin
hydrochloride, a sympathetic α-1a antagonist drug, because it
causes less postural hypotension (1). Alpha-blockers improve symptoms
correlated to BPH, but also complicate cataract surgery by changing
iris behaviour (1). The close
relationship between intraoperative floppy iris syndrome (IFIS) and
α-blockers, especially tamsulosin, were reported thirteen years ago
for the first time (1). IFIS has a
frequency of 2% in cataract surgeries, being mostly caused by
tamsulosin (2).
The reasons for causing IFIS and for its means of
action in the treatment for BPH are the same: Tamsulosin causes
relaxation of the smooth muscles in the bladder (the neck part of
the bladder) and of the iris dilator muscle, alpha1A
receptors being their targets (3).
In some cases two weeks of treatment with tamsulosin were
sufficient to cause IFIS (3).
Tamsulosin is the most common drug implicated in IFIS, although it
is not the only one which can determine this syndrome (3).
The iris is innervated by parasympathetic and
sympathetic nerves and controls the size of the pupil and adjusts
the amount of light received (4).
The sympathetic regulates the contraction of iris dilator muscle
through α1-adrenoceptors and the parasympathetic
controls the contraction of sphincter muscle through muscarinic
pathway in many species (4). Reverse
transcription-polymerase chain reaction (RT-PCR) was used in
studying the expression of mRNAs, structure that encodes proteins
of α1a, α1b and α1d-adrenoceptors (4). The α1a-adrenoceptor had the
strongest expression, the α1b-adrenoceptor had a weak expression
and α1d-adrenoceptor had an undetectable expression (4). In the human prostate, 70% of the
a1-receptors are α1a subtype (5).
Tamsulosin has a 20 times greater affinity for α1a than α1b
receptors according to in vitro data and animal studies (α1a
being the dominant adrenoreceptor in the iris) (5).
The irony comes from the fact that while tamsulosin
is treating BPH, it multiplies the risk of preoperative,
intraoperative and postoperative complications associated with
another condition, cataracts (3).
IFIS triad is composed of: Progressive and intraoperative miosis,
iris prolapse and billowing of the iris (3). Some authors declare the incidence of
IFIS among alpha-blocker treatment users between 33 and 78%, the
most common complication being iris trauma, followed by vitreous
loss posterior and capsular tears (3).
This syndrome has a wide scale of severity described
by other authors. Mild cases cause some iris billowing but dilate
well, which can permit successful use of recommended techniques for
controlling the unwanted intraoperative iris behavior (1). Severe cases can produce marked
billowing of the iris, wild iris prolapse, marked miosis during
surgery (1). Those require the use
of iris hooks, expander or iris retractors in order to complete the
surgery in safety conditions (1).
In this regard, our goal was to study albino Wistar
rats, if there were the same changes in the rat iris dilator muscle
as in rabbits, and if these changes were strictly related to the
tamsulosin treatment time, but also to its preoperative
discontinuation. We also chose the albino type to highlight the α1A
receptor expression and quantify the importance of the iris
dilatator muscle layer in IFIS manifestations.
Materials and methods
An experimental study was conducted on 20 Wistar
male rats aged 1.5–2 years, body mean weight 357±26.63 g, lasting 2
months, divided into four groups: Group 1, 5 rats under tamsulosin
hydrochloride 0.4 mg/day for 2 months; group 2, 5 rats without any
treatment in the first month, followed by tamsulosin hydrochloride
0,4 mg/day for 1 month; group 3, 5 rats under tamsulosin
hydrochloride 0,4 mg/day for 1 month, followed by 1 month without
any treatment; group 4, 5 rats (control group), without any
treatment. The calculation of the dose was performed according to
the body surface area ratio man/rats; the median lethal dose LD50
and the accelerated rat metabolism were taken into account.
Adult male wistar rats were supplied by ‘Iuliu
Haţieganu’ University of Medicine and Pharmacy (Cluj-Napoca,
Romania), and accommodated into ‘Establishment for breeding and use
of laboratory animals’ of University of Medicine and Pharmacy
(UMF), Cluj-Napoca, Romania. Rats were housed in standard
polypropylene cages, at optimum density and in standard laboratory
conditions (temperature 25±1°C, relative humidity 55±5%, and 12 h
light/dark cycle). The rats were allowed free access to standard
granular diet and water ad libitum.
All the procedures performed on laboratory animals,
comply with the European Directive 22.09.2010/63/EU, and Romanian
national low 43/2014 for protection of animals used for scientific
purposes. This project was legally approved by the Comity for
Bioethics of UMF (accord no. 336/31.08.2017) and the Veterinary
Sanitary Direction and Food Safety.
Tamsulosin hydrochloride was administrated to each
rat daily according to its group affiliation, before the first
meal, as 0.4 mg tamsulosin hydrochloride powder mixed in its food.
The tamsulosin dose that we used was the one calculated by the
anesthesiologist according to the accelerated metabolism of the
rat: 1 mg per kilogram body weight per day.
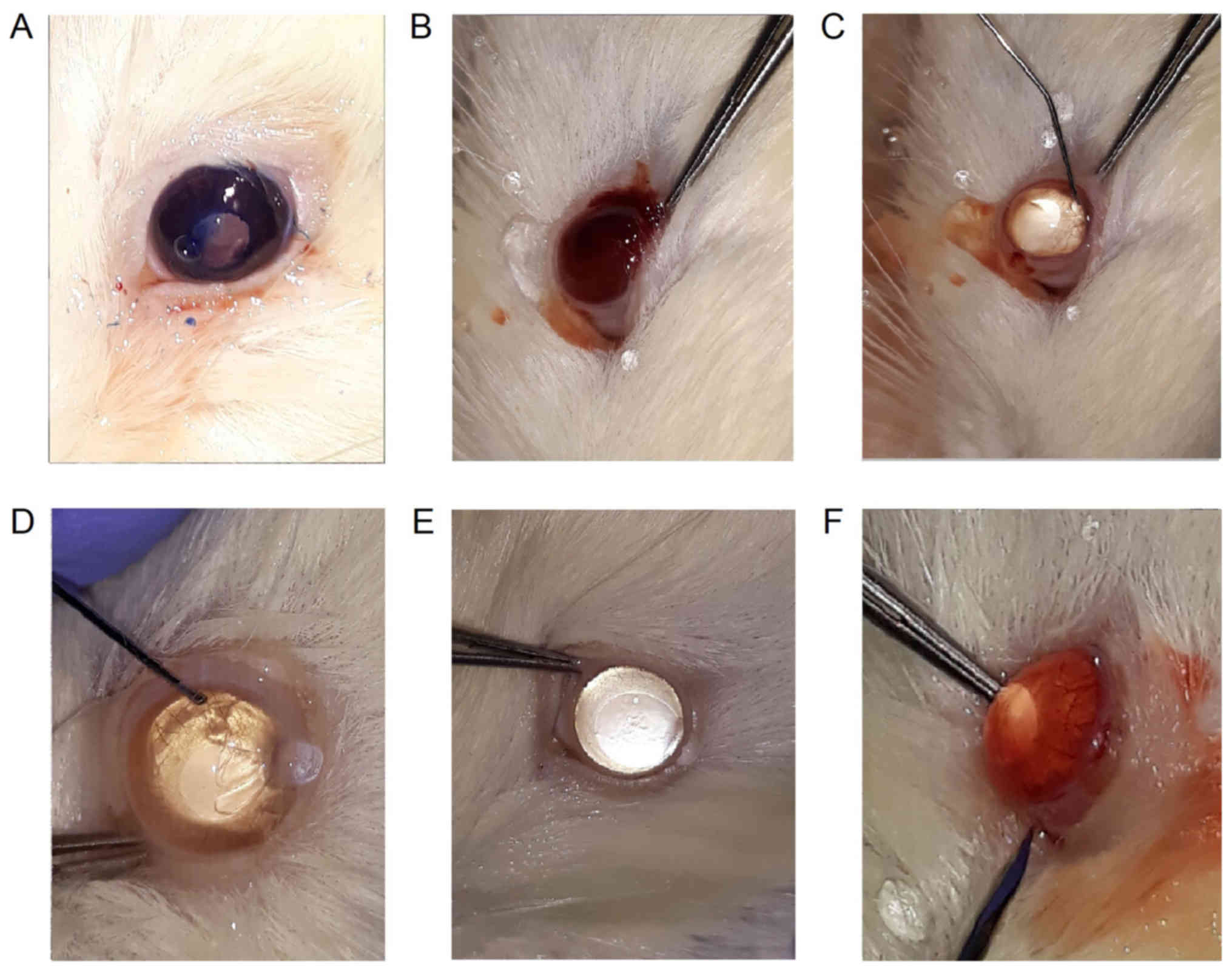
Surgery study in rats was done by the same
specialist over two days using an adapted protocol for cataracts.
The surgeon was not informed which group the animal belonged to
before or during surgeries, the order being random and with a
uniform distribution.
The anesthesia was performed with the combination of
xylazine and ketamine. The doses administered were 5.8 mg ketamine
and 0.8 mg xylazine per 100 g body weight, intraperitoneally.
Except for the first rat, everyone responded to this dose. The
animals did not wake up intraoperative. Euthanasia was induced by
the single intraperitoneal administration of pentobarbital 40
mg/100 g body weight immediately after surgery. Successful
euthanasia was confirmed after achieving a lack of heartbeat and
respiratory movements, lack of reactivity to painful stimuli and
rigor mortis.
The chosen protocol was the extraction of the lens
by the phacoemulsification technique, but adapted to the given
conditions. Most of the operator steps were followed, but without
using ultrasound to remove the lens. Because of the small
dimensions of the rat's lens, it was not possible to use the
ultrasound probe used in the human patients. Thus, we performed the
following steps in the operative protocol: Local anesthesia with
oxybuprocaine hydrochloride, side-ports at 10 and 14 h with the
15-degree V Lance knife, cannula introduction of physiological
serum in the anterior chamber, corneo-scleral incision at the
limbus level at 11–12 or temporal, coloration of the anterior
capsule of the lens in some cases for better visualization, the
capsulorhexis with 26-gauge twisted needle, hydrodissection and
hydrodelineation of the nucleus by injecting the lens with serum,
irrigation and aspiration of the remaining cortex, insertion of the
serum and side-port sealing by injecting serum in the edges of the
incisions.
Identification of the syndrome requires the presence
of a triad of three clinical signs: i) Intraoperative progressive
pupil constriction, ii) an iris that shows floppy as it billows
while irrigation and aspiration is being performed in the anterior
chamber, and iii) a clear tendency of the iris to prolapse first
into the phacoemulsification and anter in the side-port incisions
during surgery. This may or not be accompanied by a poorly dilated
pupil before surgery.
Valid results for a modified iris behavior were
obtained preoperative, intraoperative and postoperative. We noted
the pupillary diameter at 9 a.m. the day of surgery (before
instillation of 0,5% tropicamide-mydriatic and cycloplegic agent),
after 1 h from instillation of tropicamide and after 2 h of
instillation of tropicamide; the presence or absence of pupil
constriction during surgery, floppy iris, the prolapse into the
main incision or in side-ports, prolapse of the iris during serum
injection, iris rupture, posterior capsule tear, vitreous loss,
lens fragments in the vitreous, suprachoroidal bleeding, corneal
haze. Postoperative we measured the pupil diameter and we
calculated the total surgery time.
We noted cases of floppy iris as those situations
where the iris was shaking and billowing. The prolapse in the main
incision or in the sideport refers to the fact that the iris slides
into the incisions during or even in the absence of surgical
maneuvers. Prolapse of the iris during the injection of serum
indicates slippage during injection through side ports. The iris
rupture it's due to the iris atrophy under tamsulosin treatment and
translates its friability. The posterior capsule can break more
easily in the low visibility situation, stronger ultrasound
intraoperative parameters, and intense surgical maneuvers when
tamsulosin is used as a treatment. The posterior capsule of the
lens can be easy broken in low visibility and high surgery
parameters, intensive maneuvers, aggravating the operatory steps.
Lens fragments may also appear in the vitreous by breaking the
posterior capsule, complicating the surgery process. Due to
excessive manipulation in these cases, suprachoroidal haemorrhage
may occur, complication with small chances of recovery of
postoperative vision. Corneal haze means a cloudy cornea, also
being a result of high intraoperative parameters and a long total
operative time.
We enucleated one eye for each group, including the
control group, to perform histopathological examination of the
iris.
Light microscopy
The eyes of rats from the experimental groups (G-I,
G-II, G-III) and the control group were collected immediately after
euthanasia, fixed in 10% phosphate-buffered formalin with pH 7.0
(24 h), processed through a tissue-specific protocol and embedded
in paraffin wax. The 4 micrometer (µm) sections were cut
horizontally through the visual axis and routinely stained with
hematoxylin and eosin (H&E). The photomicrographs were taken
using an Olympus SP 350 digital camera and Stream Basic imaging
software (Olympus Corporation, Tokyo, Japan).
The thickness of the iris dilator muscle and the
posterior epithelium was evaluated. The animals used in this study
were albino Wistar rats; thus an assessment regarding the pigment
granules in the posterior epithelium cells could not be
performed.
Statistical analysis
All data are reported as the mean ± SEM. The
Gaussian distribution was checked by D'Agustino & Person
normality test. One-way analysis of variance ANOVA and followed by
post hoc Bonferoni range test procedure was performed for pair-wise
comparisons between the normally distributed data, while data with
non-Gaussian distribution were analyzed by analysis (one-way) of
variance Kruskal-Walis, followed by post test Dunns. Spearman's
correlation was chosen, to assess the correlation between non
normally distributed variables; the interpretation was made
according to the Colton scale. Logistic regression model for the
potential association between tamsulosin hydrochloride
administration and various associated ocular pathology was analyzed
by Fishers exact test followed by odds ratio. Statistical
significance was at 95% confidence interval, P<0.05. Statistical
values and figures were obtained using GraphPad Prism version 5.0
for Windows, GraphPad Software (San Diego, CA, USA).
Results
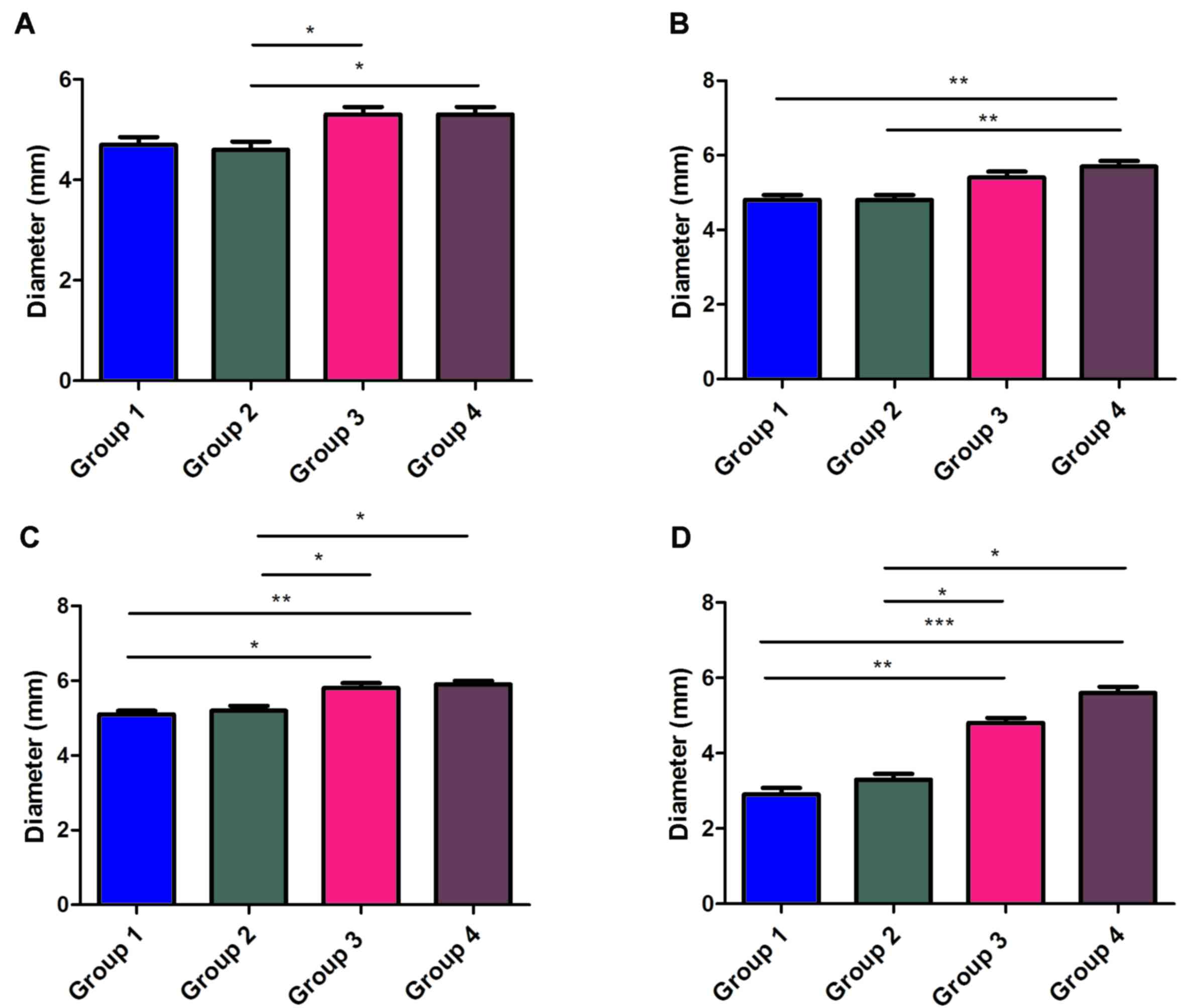
We measured the pupillary diameters on the day of
the surgery as follows: Before using tropicamide, one and two hours
after instillation of tropicamide and finally at the end of the
surgery. We also noted the moment when intraoperative miosis
occurred (miosis was considered when the pupillary diameter was ≤4
mm). The largest pupillary diameters were found in the control
group (mean value 5.3 mm), and in group 1 (mean value 4.7 mm) with
continuous treatment, the smallest pupil diameters. Statistically
significant differences occurred when comparing group 2/group 3
(P<0.05) and group 2/control group (P<0.05) before using
tropicamide and before the surgery (Fig.
1A). One hour after the tropicamide infiltration, statistically
significant P-values were found for the following comparative
situations: Group 2/group 4 and group 1/group 4. In both cases
P<0.01. (Fig. 1B). After 2 h of
tropicamide administration, the P-value was <0.05 when comparing
group 2 with group 4 and group 2 with group 3 or group 1 with group
3. The P-value was <0.01 when comparing groups 1 with 4.
(Fig. 1C). At the end of the surgery
there were statistically significant differences between the four
groups as follows: P<0.5 in case of comparison of group 2 with
group 3, group 2 with group 4; P<0.01 while comparing group 1 to
group 3 and P<0.001 while comparing group 1 (mean value 2.9 mm)
to group 4 (mean value 5.6 mm) (Fig.
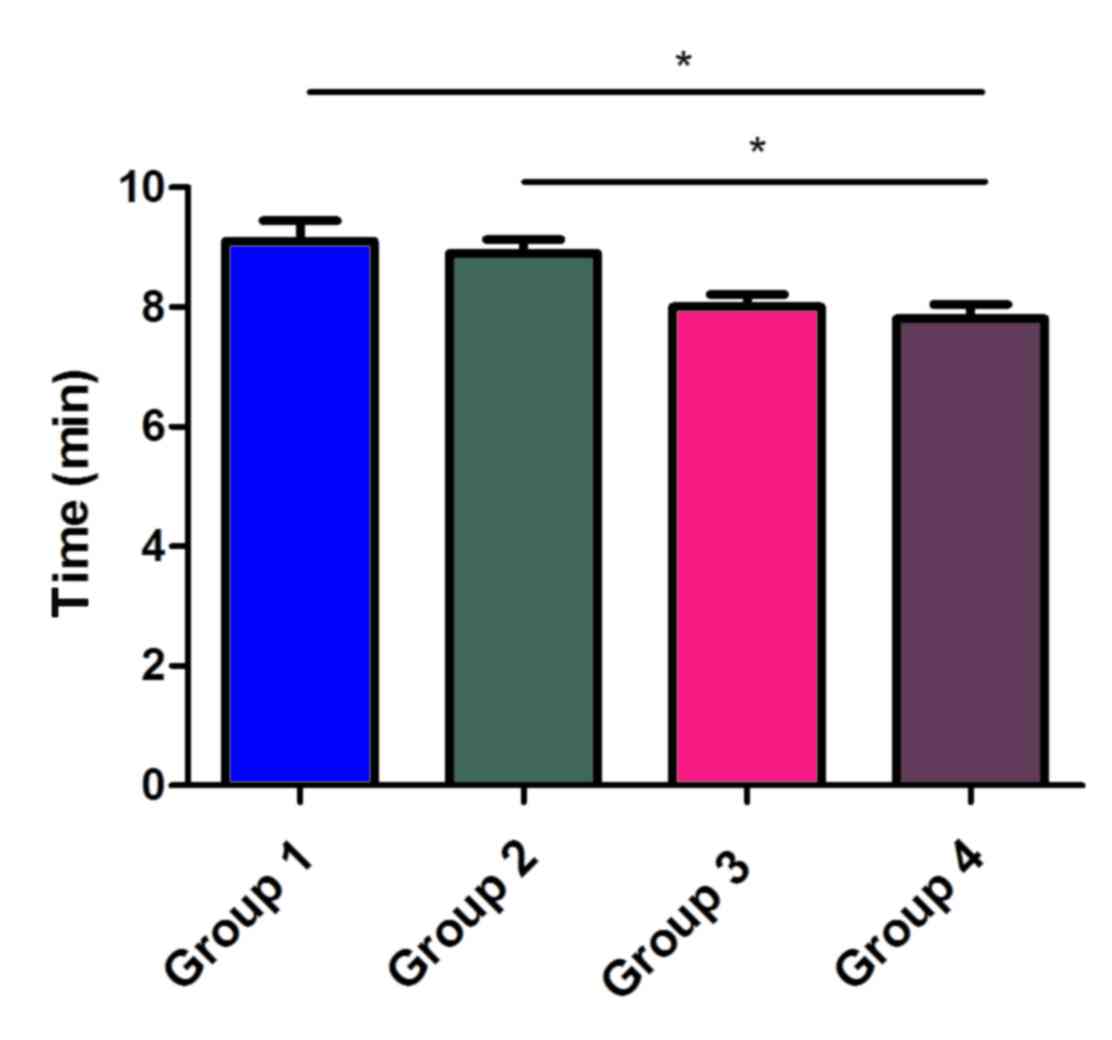
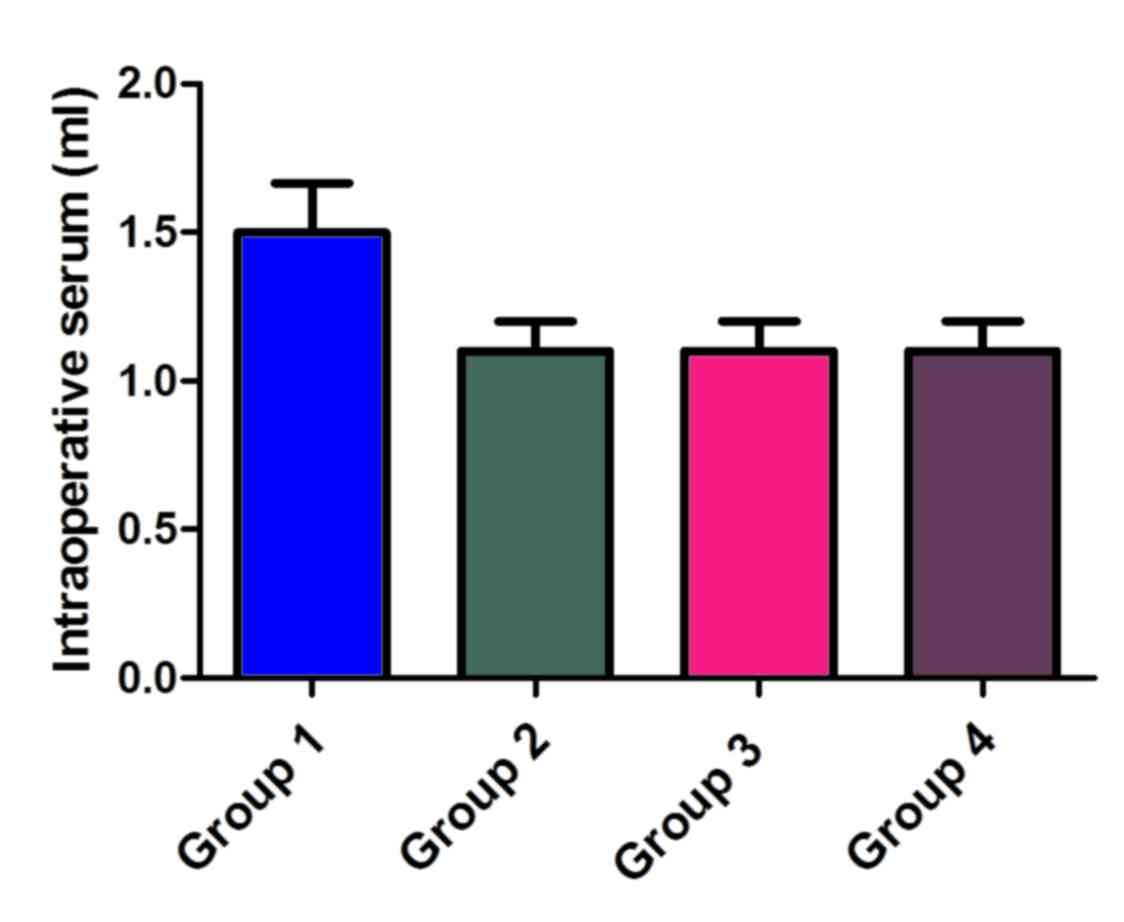
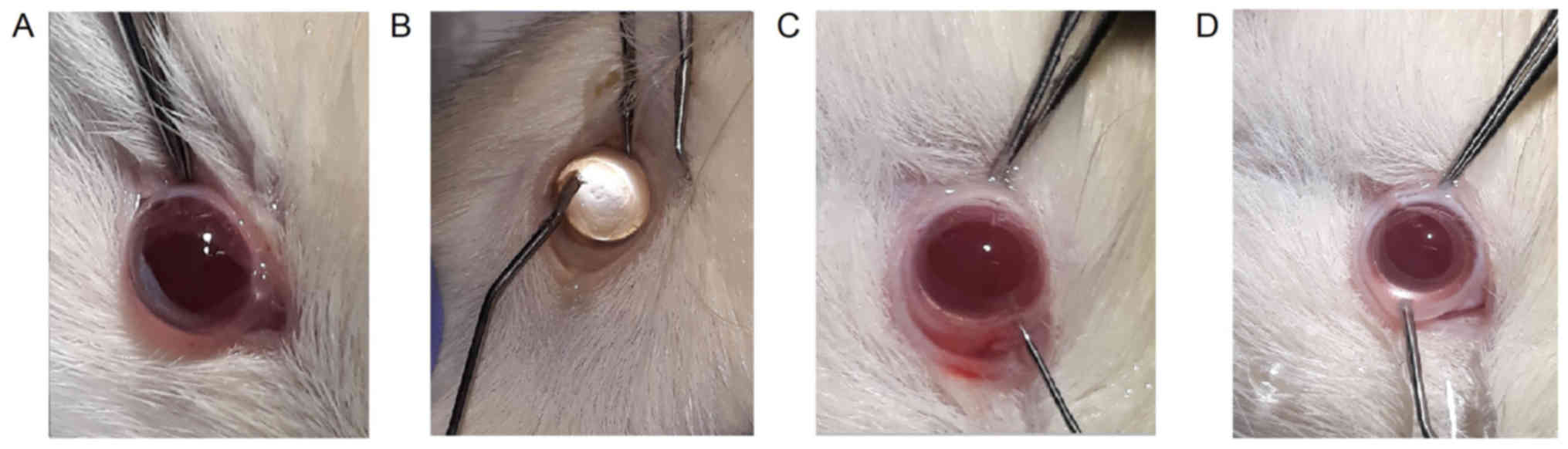
1D and Fig. 2A-D). The total
duration of the intervention post-anesthesia (measured in min) was
longer for group 1 and 2 compared to control group 4 (P<0.05;
Fig. 3). The total amount of
intraoperative serum (measured in ml) was not statistically
significantly higher in group 1 with continuous treatment (Fig. 4).
Floppy iris occurred at peak frequency for group 1
with continuous treatment (Fig. 5A and
B) and with zero frequency in the control group. Group 2 (odds
ratio, 30.33; confidence interval 95%, 3.002–1698; P=0.01), treated
with tamsulosin in the last part of the study followed group 1
regarding the presence of floppy iris (odds ratio, 71.4;
confidentiality interval 95%, 1.391–661.3; P<0.001); group 3
(odds ratio, 6.176; confidentiality interval 95%, 0.2597–146.9;
P>0.05) was next, followed by the control group with zero cases
(Table I).
 | Table I.Logistic regression model for the
potential association between tamsulosin hydrochloride
administration and various associated ocular pathology (Fishers
exact test followed by odds ratio). |
Table I.
Logistic regression model for the
potential association between tamsulosin hydrochloride
administration and various associated ocular pathology (Fishers
exact test followed by odds ratio).
| Variable | Odds ratio | 95% Confidence
interval | P-value |
|---|
| Floppy iris |
|
|
|
| Group
1 | 71.40 | 3.002–1698 | 0.0007 |
| Group
2 | 30.33 | 1.391–661.3 | 0.0108 |
| Group
3 | 6.176 | 0.2597–146.9 | 0.4737 |
| Group
4 | 1.00 | Reference
category |
|
| Iris prolapse in
main incision |
|
|
|
| Group
1 | 133.0 | 4.810–3677 | 0.0001 |
| Group
2 | 81.00 | 4.358–1506 | 0.0011 |
| Group
3 | 3.857 | 0.3263–45.60 | 0.5820 |
| Group
4 | 1.00 | Reference
category |
|
| Iris prolapse while
serum injection |
|
|
|
| Group
1 | 81.00 | 4.358–1506 | 0.0011 |
| Group
2 | 36.00 | 2.719–476.6 | 0.0055 |
| Group
3 | 9.000 | 0.8084–100.2 | 0.1409 |
| Group
4 | 1.00 | Reference
category |
|
| Lens fragments in
vitreous |
|
|
|
| Group
1 | 9.000 | 0.8084–100.2 | 0.1409 |
| Group
2 | 3.857 | 0.3263–45.60 | 0.5820 |
| Group
3 | 1.000 | 0.05380–18.59 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Posterior capsule
tear |
|
|
|
| Group
1 | 14.54 | 0.6669–316.9 | 0.0867 |
| Group
2 | 6.176 | 0.2597–146.9 | 0.4737 |
| Group
3 | 3.316 | 0.1199–91.68 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Suprachoroidal
haemorrhage |
|
|
|
| Group
1 | 6.176 | 0.2597–146.9 | 0.4737 |
| Group
2 | 3.316 | 0.1199–91.68 | 0.9999 |
| Group
3 | 1.000 | 0.05459–18.32 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Corneal haze |
|
|
|
| Group
1 | 9.000 | 0.8084–100.2 | 0.1409 |
| Group
2 | 3.857 | 0.3263–45.60 | 0.5820 |
| Group
3 | 1.000 | 0.05380–18.59 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Iris rupture |
|
|
|
| Group
1 | 9.000 | 0.8084–100.2 | 0.1409 |
| Group
2 | 3.857 | 0.3263–45.60 | 0.5820 |
| Group
3 | 3.316 | 0.1199–91.68 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Loss of
vitreous |
|
|
|
| Group
1 | 6.000 | 0.5318–67.69 | 0.3034 |
| Group
2 | 2.250 | 0.1700–29.79 | 0.9999 |
| Group
3 | 0.3016 | 0.01091–8.338 | 0.9999 |
| Group
4 | 1.00 | Reference
category |
|
| Intraoperative
miosis |
|
|
|
| Group
1 | 441.0 | 7.972–24400 | P<0.0001 |
| Group
2 | 441.0 | 7.972–24400 | P<0.0001 |
| Group
3 | 6.176 | 0.2597–146.9 | 0.4737 |
| Group
4 | 1.00 | Reference
category |
|
Iris prolapse in the main incision appeared with
maximum frequency for group 1 with continuous treatment (Fig. 5B) and low frequency (1 case) for the
control group. Group 2 (odds ratio, 81; confidentiality interval
95, 4.358–1506; P=0.001), undergoing treatment in the last part of
the study, followed group 1 (odds ratio, 133; confidence interval
95%, 4.810–3677; P<0.001). Group 3 recorded as follows: Odds
ratio, 3.857; confidence interval 95%, 0.3263–45.60; P=0.5
(Table I).
Iris prolapse during serum injection occurred with
the highest frequency for group 1, the one with continuous
treatment (Fig. 5B-D) and low
frequency (1 case) in the control group. Group 2 (odds ratio, 36;
confidence interval 95%, 2,719–476.6; P=0.005), followed group 1
(odds ratio, 81; confidence interval 95%, 4.358–1506; P<0.01);
in group 3 (odds ratio, 9; confidence interval 95%, 0.8084–100.2;
P>0.05) few cases were reported (Table I).
The rupture of the posterior capsule (posterior
capsule tear) had a null intraoperative presence in the control
group 4 but met among the other three groups as an intraoperative
complication: Group 3 (odds ratio 1, confidence interval 95%,
0.1199–91.68; P=1) group 2 (odds ratio, 6.17, confidence interval
95%, 0.2597–146.9’; P=0.47) group 1 (odds ratio, 14.54;
confidentiality interval 95%. 0.6669–316.9; P=0.08) (Table I).
Lens fragments in the vitreous were present in the
first three groups (Fig. 6A) and in
the 4th group no such intraoperative complication was recorded. The
complication had the following distribution: Group 3 (odds ratio 1,
confidence interval 95%, 0.05380–18.59; P=1), group 2 (odds ratio,
3.8; confidence interval 95%, 0.3263–45.60; P=0.58) group 1 (odds
ratio, 9; confidence interval 95%, 0.8084–100.2; P=0.1409 (Table I).
Suprachoroidal bleeding (haemorrhage) was installed
in the following cases: Group 1 (odds ratio, 6.176; confidence
interval 95%, 0.2597–146.9), group 2 (odds ratio, 3.31; confidence
interval 95%, 0.1199–91.68), group 3 (odds ratio, 1; confidence
interval 95%, 0.05459–18.32) (Fig. 6B
and F); group 4 not installed at all. The P-values were
>0.05, not statistically significant (Table I).
The corneal haze complicated the cataract surgery as
follows: Group 1 (odds ratio, 9,000; confidence interval 95%,
0.8084–100.2), group 2 (odds ratio, 3.857; confidence interval 95%,
0.3263–45.60), group 3 (odds ratio, 1,000; confidence interval 95%,
0.05380–18.59’) and group 4 with only one case (Table I).
The iris rupture was not present in the control
group, but it appeared with decreasing frequency in the following
groups: Group 1 (odds ratio, 9.000; confidence interval 95%,
0.8084–100.2), group 2 (odds ratio, 3.857; confidence interval 95%,
0.3263–45.60), group 3 (odds ratio, 3.316; confidence interval 95%,
0.1199–91.68) (Fig. 6C). The
P-values were all >0.05, not statistically significant (Table I).
Loss of vitreous was recorded as follows: Group 1
(odds ratio, 6.000; confidence interval 95%, 0.5318–67.69), group 2
(odds ratio, 2.250; confidence interval 95%, 0.1700–29.79), group 3
(odds ratio, 0.3016; confidence interval 95%, 0.01091–8.338)
(Fig. 6D). The P-values were all
>0.05, not statistically significant (Table I).
Intraoperative miosis had statistical relevance in
group 1 and group 2. Group 1 had a odds ratio of 441.0 (confidence
interval 95%, 7.972–24400; P<0.0001), group 2 had a odds ratio
of 441.0 (confidence interval 95%, 7.972–24400; P<0.0001) and
group 3 odds ratio, 6.176 (confidence interval 95%, 0.2597–146.9;
P>0.05) (Fig. 6C-F) (Table I).
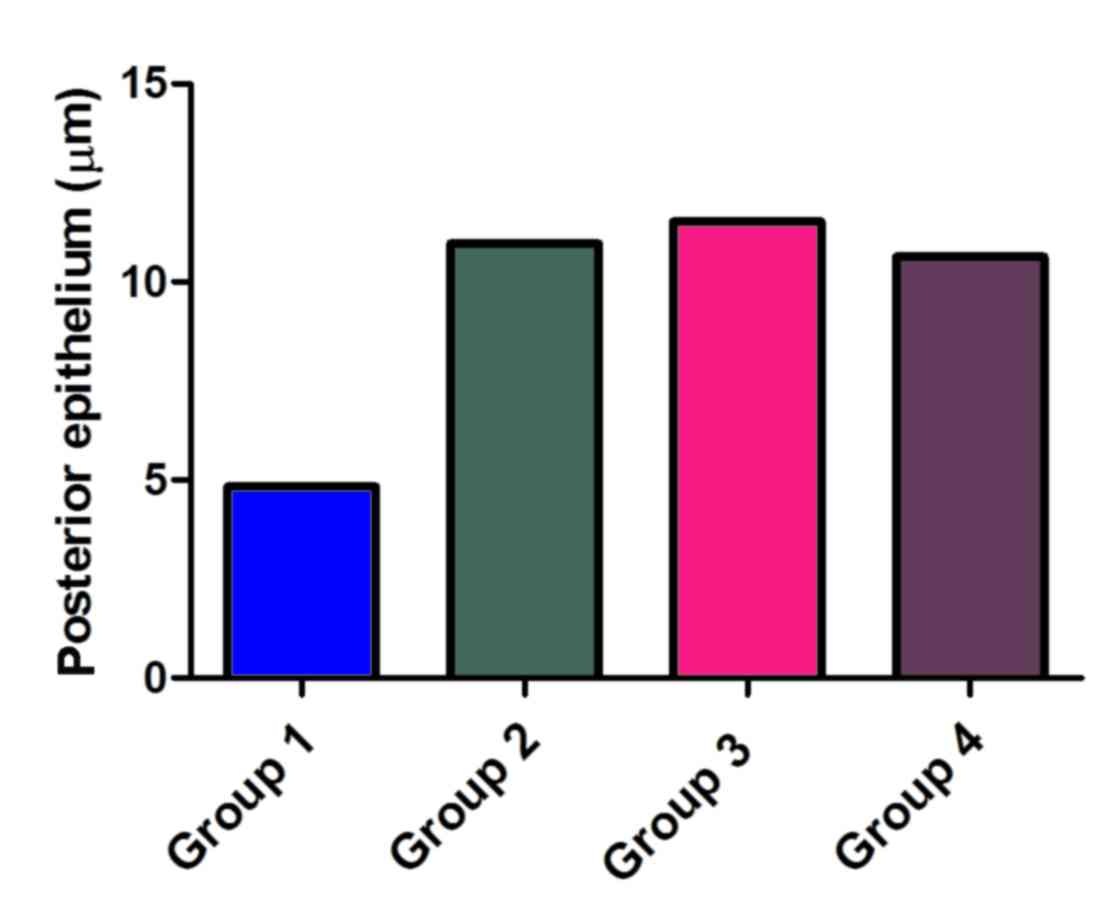
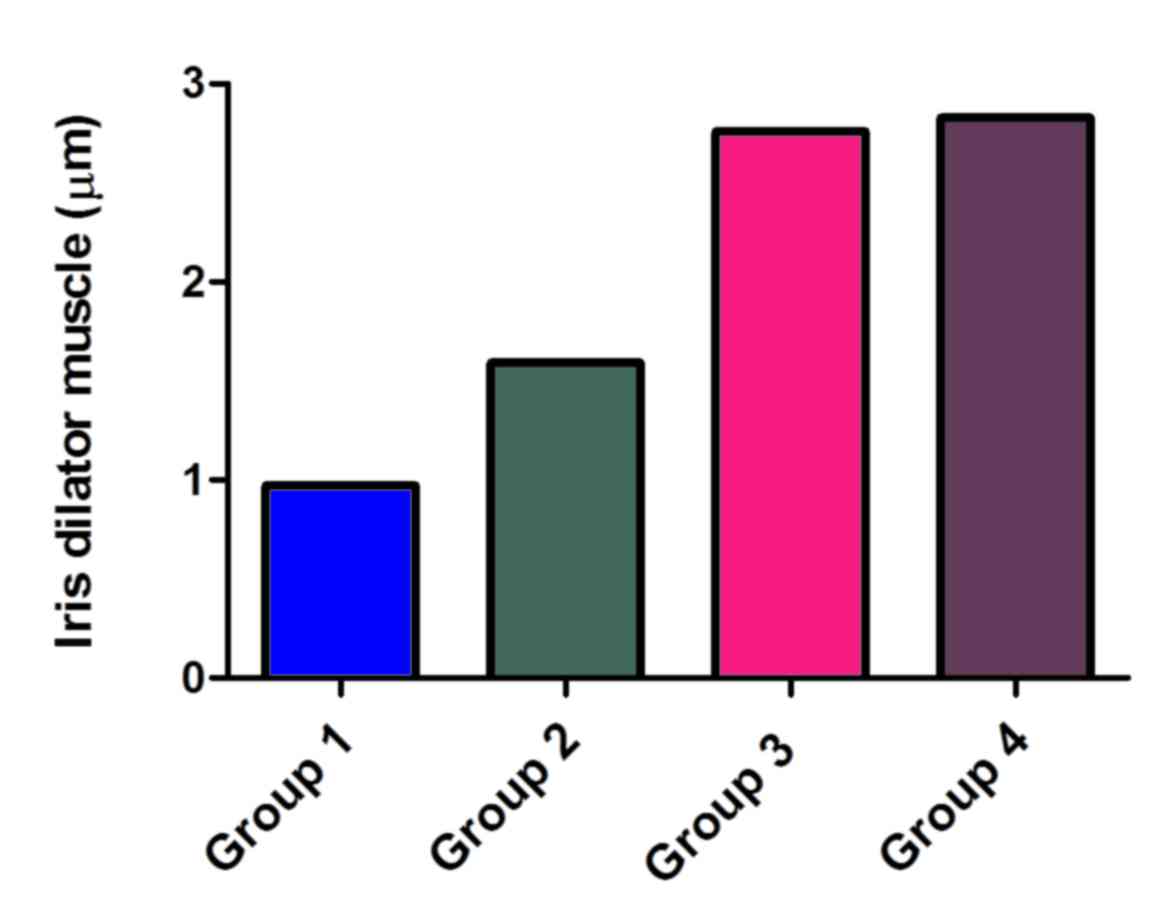
The thickness of the iris dilator muscle and the
posterior epithelium were evaluated (Table II). The measurements of the
thickness of the iris dilator muscle changed depending on the
duration of the alfa-blocker treatment. In other words, the 4th
control group recorded a thickness of 2.85 µm, the group 3 had a
smaller thickness (2.76 µm), followed by group 2 with 1.59 µm and
group 1 which had the smallest thickness of 0.97 µm. A significant
difference can be seen between the control group 4 and the group 1,
both in terms of the size of the iridium dilator muscle layer and
in terms of the thickness of the posterior epithelium (group 1
having a thickness of 4.83 µm, while group 4 of 10.63 µm) (Figs. 7 and 8).
 | Table II.The thickness of the iris dilator
muscle and the posterior epithelium (µm). |
Table II.
The thickness of the iris dilator
muscle and the posterior epithelium (µm).
| Component
evaluated | Length (µm) |
|---|
| Posterior
epithelium group 1 | 4.83 |
| Iris dilator muscle
group 1 | 0.97 |
| Posterior
epithelium group 2 | 10.97 |
| Iris dilator muscle
group 2 | 1.59 |
| Posterior
epithelium group 3 | 11.52 |
| Iris dilator muscle
group 3 | 2.76 |
| Posterior
epithelium control group 4 | 10.63 |
| Iris dilator muscle
control group 4 | 2.83 |
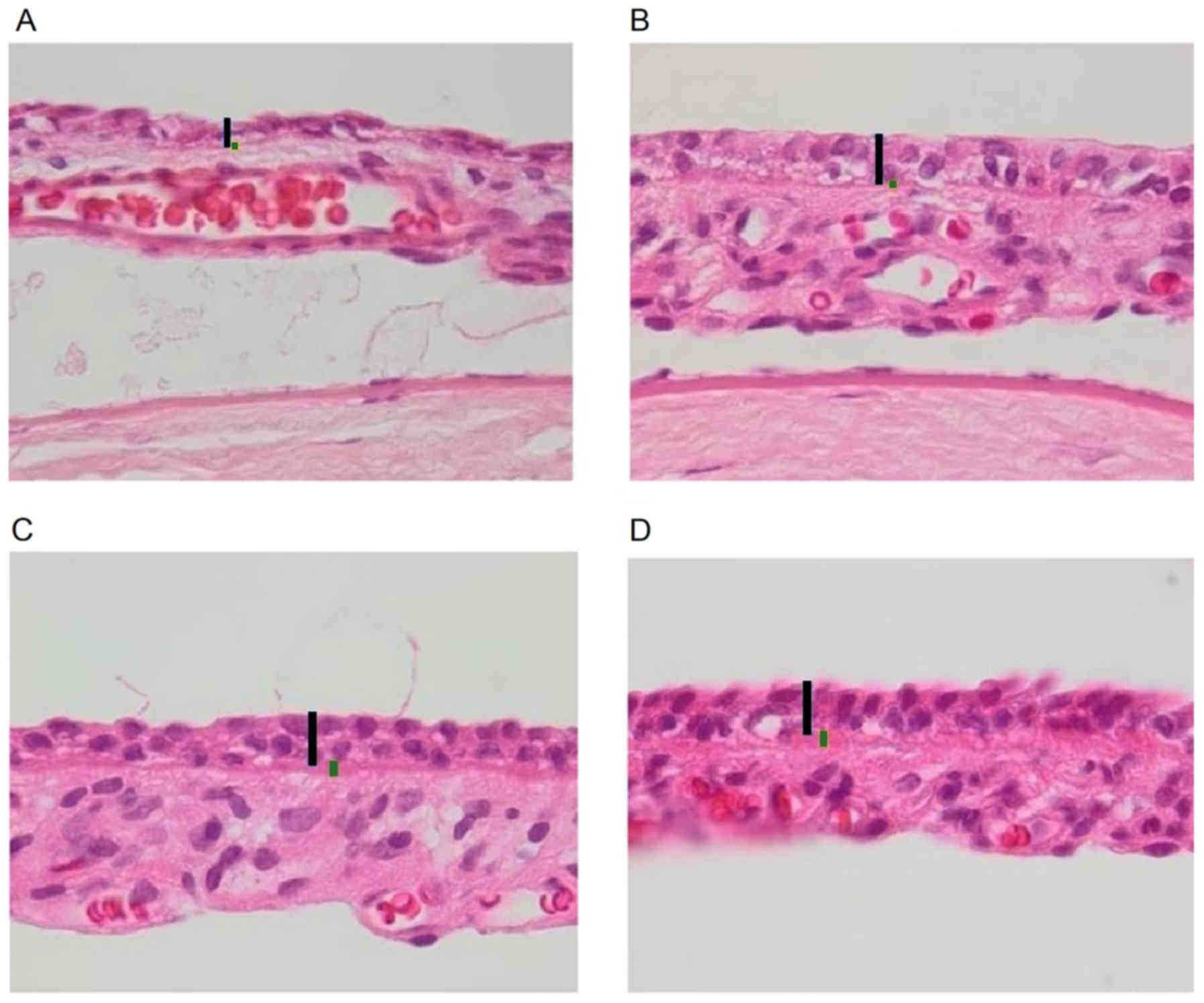
In the microscopic images below, we can see the
thinning of the iris dilator muscle layer, as the duration of
treatment with tamsulosin increases. The atrophy of the iris
dilator muscle is evident in the picture bellow, where the iris
section of an eyeball belonging to group 1, with continuous
treatment, is illustrated (Fig. 9A).
The muscle atrophy is also seen in group 2 (Fig. 9B) with treatment over the last month
but is not as obvious as in the previous case. Groups 3 and 4
(control) do not show any major changes to each other, group 4
being the reference in our case (Fig. 9C
and D).
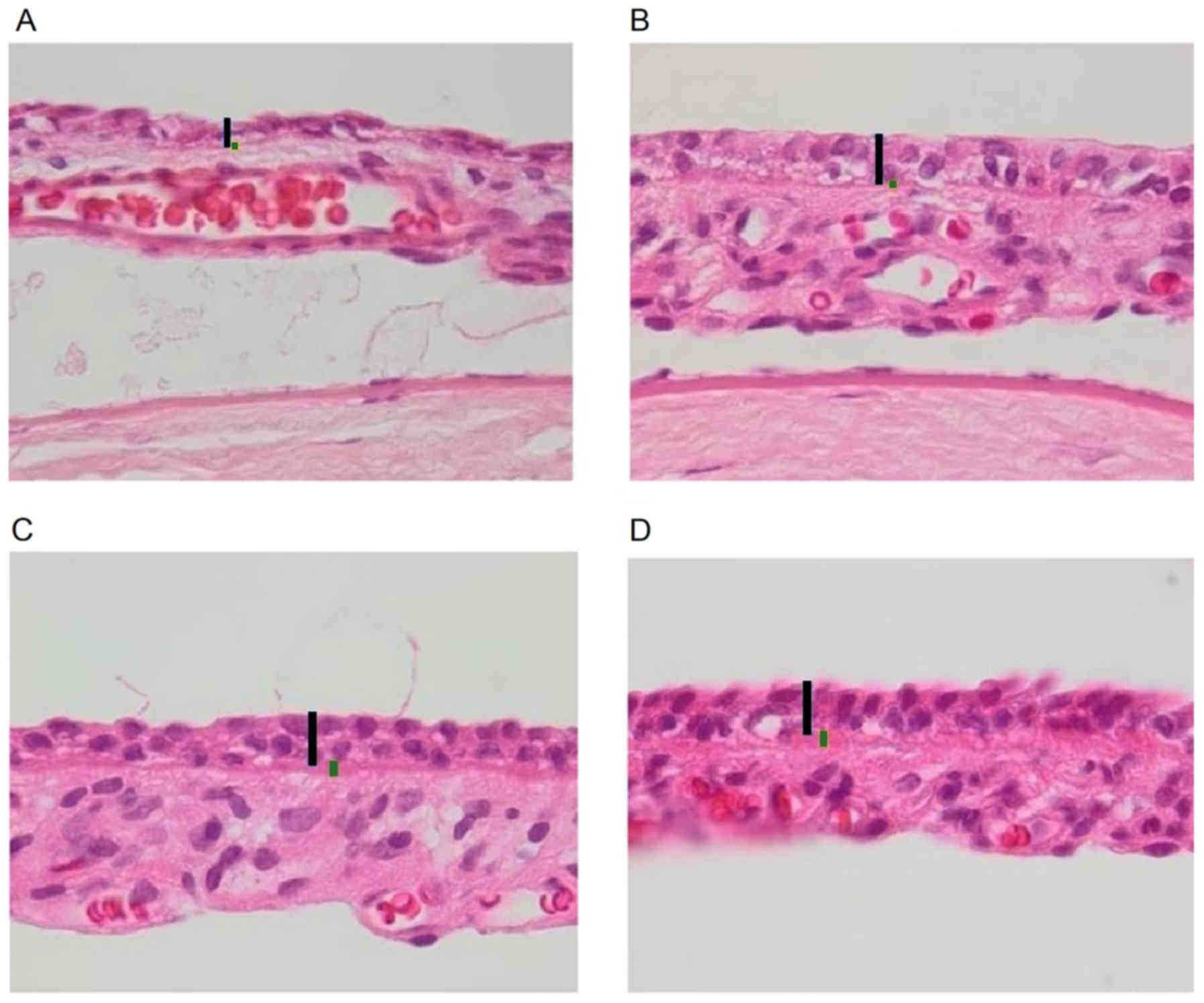 | Figure 9.Histological images representing the
posterior epithelium and the iris dilator muscle layer. (A) Iris:
Black bar, posterior epithelium; green bar, iris dilator muscle
(group 1). (B) Iris: Black bar, posterior epithelium; green bar,
iris dilator muscle (group 2). (C) Iris: Black bar, posterior
epithelium; green bar, iris dilator muscle (group 3). (D) Iris:
Black bar, posterior epithelium; green bar, iris dilator muscle
(control group 4). Histological analysis, hematoxylin and eosin
stain; scale bar, 10 µm. |
Discussion
The distribution on the four groups helped us to
highlighting the effects of tamsulosin hydrochloride, which is a
prostate adenoma medication, at the iris level. In other words,
group 1, with continuous medication in the two months, had the most
preoperative, intraoperative and postoperative complications,
followed by group 2, receiving medication only in the last month,
which was followed by group 3 with medication in the first month
and a month break after; group 1 did not have any specific
manifestation, being the control one. One can see a similarity
between groups 1 and 2 (those with continuous treatment,
respectively with treatment in the last one) and between groups 3
and 4 (treatment group in the first month followed by one month
break and the control group).
In terms of pupil diameter in the control group
(group 4), we found the highest pupillary diameters, and in the
case of group 1, with continuous treatment, the smallest pupil
diameters, as we expected. The greater statistically significant
difference was between the continuous treatment group and the
control group. In other words, we found in all the situations the
lowest pupillary diameter values in the groups 1 and 2, while
groups 3 and 4 showed elevated values.
Intraoperatory floppy iris syndrome was
characterized by Chang et al for the first time as a flaccid
iris (5). Flutter moves were
recorded during the procedure of phacoemulsification, running at
normal current levels concerning the circulating fluid, iris
prolapse in the main incision and through the side-ports, but also
intraoperative miosis (6,7). We discovered floppy iris in 80% in the
first group, the one with continous treatment. Group 2 (P=0.1), the
one with treatment in the last part of the study, followed group 1
(P<0.001) as frequency, and in group 3 there were the fewest
cases. We found iris prolapse through the main incision in 100%
cases during surgery and 90% during serum introduction in the
control group. In order to minimize this effect, authors recommend
using viscoelastic substance, meaning substance with big molecular
weight and a correctly performed incision (6,7).
Predisposing factors regarding the iris prolapse were revealed:
Improper iris configuration, low anterior chamber depth, and
unnormal architecture or position made by the surgeon of the
corneal tunnel (8).
In one study on men operated for cataracts
undergoing treatment for BPH, 23% showed IFIS, but only the ones
treated with tamsulosin (8). The
severity and of course the incidence of IFIS was highly reduced
after introducing a protocol, including iris retractors, minimal
phaco parameters, intracamerular phenylephrine and high quantity of
vascoelastic material (8). Bimanual
phacoemulsification can be somethimes sufficient, without any need
to use something else (6). Chang's
suggestion of using a mantainer and a chopper helps keeping this
way the circulatory irrigation in another position, anterior to the
iris, consequently reducing the behavior of the iris (5). Storr-Paulsen finds in other words the
same manifestations: significant inraoperative miosis, less
preoperative dilatation and greater endothelial cell loss in
comparision with patients without treatment for BPH, despite the
recommended precautions taken (9).
Other studies reccomends sub-Tenon lidocaine injection, which may
reduce the incidence of floppy iris in comparison with
intra-cameral lidocaine (10).
Intracameral phenylephrine can reverse IFIS, causing iris rigidity,
the pupil returning this way to its preoperative size (11). Tamsulosin performs its long action by
a constant blockade at the level of the iris receptors, leading to
an diffuse dilator muscle atrophy (1,8). This
may explain the poor preoperative dilation and the floppy iris
phenomenon (6,7).
The posterior capsule tear had a null intraoperative
presence in control group 4 but met among the other 3 groups as an
intraoperative complication, but with no statistical significance.
We had five cases of posterior capsule rupture (50%) with vitreous
loss in the first group, which would had required anterior
vitrectomy. Other authors have had a 12% frequency of this
complication in cases with IFIS (7).
Lens fragments in the vitreous were present in the first 3 groups,
but in the 4th group, no such intraoperative complication was
recorded. The iris rupture was not present in the control group,
but it appeared with descending frequency in the following groups:
1, 2, 3 in this order. The P-values were not statistically
significant. The loss of vitreous was recorded at high frequency in
group 1 as we expected. Intraoperative miosis was installed with
statistical relevance in group 1 and 2, P<0.0001.
Our goal was to study Wistar albino rats, more
exactly if these changes are strictly related to tamsulosin
treatment time and also to its preoperative discontinuation.
Nakamura was the one who revealed, at the level of iris dilator
smooth muscle, the existence of the alpha1 receptor in rabbits
(4). We found out from our study
that there is a clear connection between the time of administration
of the alpha-blocker medication and most of the operative
complications, especially in the case of intraoperative miosis,
floppy iris and iris prolapse. There was a close similarity between
the two groups (1-with continuous treatment and 2-with treatment in
the last month) with minimal statistical differences and also a
similarity between the other two groups (3-with treatment one month
and last month pause and 4-the control one). From the last
statement, we can emphasize the importance of stopping treatment
with tamsulosin prior to cataract surgery in Wistar rats, with one
month being optimal for good surgical outcomes.
The reason why we chose the albino type was to
highlight the α1A receptor expression and to strictly quantify the
importance of the iris dilatator muscle layer in the IFIS
manifestations, considering that this type has no pigmentary
granules in the posterior epithelial layer. We demonstrated the
thinning of the posterior epithelium, but especially the thinning
of the iridium dilator muscle, even its evident atrophy in group 1
and 2. All of these histological changes had echoes in the
intraoperative iris floppy syndrome, as the literature had
revealed: Melanin at the level of the posterior epithelial layer
influence IFIS manifestations (12).
We have expanded our research on the Wistar rats, as experiments
have so far been carried out only on albino rabbits. Researchers
also analyzed using electron microscopy (EM) on pigmented rabbit
the structure of the iris that received tamsulosin vs. groups
without treatment (12). They noted
clumping of pigment granules, irregularities in the size and also
thinning (atrophy) of the dilator muscle (12). There was a more lobular and irregular
nuclei of the pigment epithelium and dilator muscle, quite similar
to the human specimens (12). In
this study, the authors suggests, as presented before, that the α1a
antagonist high affinity for melanin, which was found in the
epithelial cells, may contribute to dilator muscle atrophy
(12). For stronger evidence
regarding their hypothesis, EM analyses of albino and pigmented
rabbit eyes (under α1a antagonists treatment) could be recommended
(12). There was no association
between IFIS and the iris color in a prospective clinical study,
suggesting that brown-eyed patients are not more susceptible to the
α1 antagonist than blue-eyed men. Maybe a prospective study using
individuals and correlating administration of tamsulosin, iris
color and severity of IFIS can help to demonstrate the quantity of
contribution regarding treatment-melanin interactions in IFIS
(12).
A study used iris dilator muscles from rabbits and
measured the tension at the iris level in response to a substance
named phenylephrine with and without an α1 agonist (13). They analyzed the concentration curve
as a response to phenylephrine in albino Japanese rabbits and Dutch
pigmented rabbits (13). Compared to
albino iris, phenylephrine had a much higher binding affinity for
pigmented iris to the α1 receptor (13). That may suggest that the melanin
pigment allows increased binding concerning the α1 receptor
(13). In these sense, they
concluded that the albino and pigmented rabbit iris are in other
words identical except for the melanin presence (13). It could be interesting, in our case,
the comparison on this matter of pigmented rats with Wistar rats,
to see if there is more obvious effects of tamsulosin in cataract
surgery in pigmented rats.
The incidence of IFIS according to Graefe (1,9%) was
significantly higher amongst tamsulosin and doxazosin users and
suggested that all men under α1antagonists treatment should be
identified before surgery and have alternative treatment and
surgery techniques made by an experimented surgeon (14). Clinical and laboratory evidence
suggest that there is a long-term anatomic and structural changes
after the use of these drugs, which explain the IFIS persistence
months after stopping the α-blockers treatment (15).
In our study, in contrast to what we discussed
before regarding the long-term effects of tamsulosin upon the iris,
we have shown that discontinuation of tamsulosin for one month
(group 3) largely cancels the manifestations of IFIS in rats. This
may suggest a closer collaboration between the urologist and the
ophthalmologist, with the urologist's suggestion to change
treatment for BPH with another class of drugs that do not interact
with the iris receptors. We are waiting for a definitive study
which may delineate IFIS pathogenesis and its connection to drugs
and diseases (15). Discontinuing
α-blockers prior to the patient's cataract surgery without drug
replacement may not be in the favor of the patient (15).
The other major group of drugs used to treat BPH
seems that does not cause IFIS (16). Finasteride, a member of the 5-alpha
reductase inhibitors, is a drug typically used for BPH as first
line treatment and androgenic alopecia, but is also associated
sometimes with cataracts (17).
Several studies have been reported, suggesting the existence of a
link between IFIS and some other drugs, like: Finasteride,
mianserin, antipsychotics (18–20).
Likewise, another relationship between IFIS and other drugs was
reported; for example, between IFIS and these drugs:
chlorpromazine, aspirin, losartan, metformin (21,22);
donepezil and quetiapine, imipramine, risperidone (23–26).
Duloxetine and warfarin were also reported (27,28).
There have been situations in which men with BPH
have interrupted tamsulosin for several months, years and still
have the classic triad of the syndrome and severe IFIS (29,30). In
other words, we cannot rely on stopping the treatment to cancel the
IFIS symptoms (30). The duration of
tamsulosin intake is not linked to the severity of the condition
(15).
As a conclusion, the fact that the symptoms of
intraoperative syndrome disappeared after stopping treatment with
alpha-blockers a month before surgery in rats (on the contrary in
humans stopping treatment more time before does not prevent the
appearance of IFIS signs) leads us to the importance of the
melalnin granules (the lack of melanin granules in albino rats,
respectively their presence in humans) and the accelerated
metabolism of rats. As we said above, there is clear evidence that
there is a statistically significant difference between pigmented
and albino rabbits, demonstrated by others, in terms of
histological changes in the iris after alfa-blocker treatment, as
well as between control group and group undergoing continuous
treatment, demonstrated in our study on albino rats.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RMP designed the study, wrote the article, analyzed
and interpreted the data, performed surgery on rats and was
involved in drug administration. CO contributed in analysis of the
data and was involved in drafting the manuscript. BS performed the
statistical analysis and made the charts. MN and MT performed the
histological examination of the enucleated eyes. IM performed the
anesthesia and drug dose calculation. SB was responsible for the
accommodation, feeding and drug administration for the animals and
captured the intraoperative images. CN assisted in analyzing and
interpreting the data, contributed to the study design and gave
final approval of the version to be published. IC assisted in
analyzing and interpreting the data, revised the manuscript
critically for important intellectual content and gave final
approval of the version to be published. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
All the procedures performed on laboratory animals
comply with the European Directive 22.09.2010/63/EU and Romanian
national law 43/2014 for protection of animals used for scientific
purposes. The project was approved by the Comity for Bioethics of
UMF (accord. no. 336/31.08.2017) and the Veterinary Sanitary
Direction and Food Safety.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Flach AJ: Intraoperative floppy iris
syndrome: Pathophysiology, prevention, and treatment. Trans Am
Ophthalmol Soc. 107:234–239. 2009.PubMed/NCBI
|
|
2
|
Chang DF and Campbell JR: Intraoperative
floppy iris syndrome associated with tamsulosin. J Cataract Refract
Surg. 31:664–673. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janjua S and Cremers S: Managing
intraoperative floppy iris syndrome. Cataract removal surgery and
intraocular lens implantation: HS-100. 3–5. 2016.
|
|
4
|
Nakamura S, Tanigukhit T, Suzuki F, Akagi
Y and Muramatsu I: Evaluation of alfa1 adrenoreceptors in the
rabbit iris: Pharamcological caracterisation and expression of m
RNA. Br J Pharmacol. 127:1367–1374. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang DF, Braga-Mele R, Mamalis N, Masket
S, Miller MK, Nichamin LD, Packard RB and Packer M; ASCRS Cataract
Clinical Committee, . ASCRS white paper: Clinical review of
intraoperative floppy-iris syndrome. J Cataract Refract Surg.
34:2153–2162. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nicula C, Nicula D and Popescu R:
Intraoperative floppy iris syndrome-a prospective study.
Oftalmologia. 57:38–44. 2013.(In Romanian). PubMed/NCBI
|
|
7
|
Mamalis N: Importance of pupil dilation
for cataract surgery. J Cataract Refract Surg. 43:583–584. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chiseliţă D, Cantemir A, Epifanov L,
Huţuleac A and Irod A: Management of intraoperative floppy iris
syndrome. Oftalmologia. 56:69–76. 2012.(In Romanian).
|
|
9
|
Storr-Paulsen A, Jørgensen JS, Norregaard
JC and Thulesen J: Corneal endothelial cell changes after cataract
surgery in patients on systemicsympathetic α-1a antagonist
medication (tamsulosin). Acta Ophthalmol. 92:359–363. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Klysik A and Korzycka D: Sub-tenon
injection of 2% lidocaine prevents intra-operative floppy iris
syndrome (IFIS) in male patients taking oral α-adrenergic
antagonists. Acta Ophthalmol. 92:535–540. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lorente R, de Rojas V, Vázquez de Parga P,
Moreno C, Varela J, Landaluce ML, Méndez J and Lorente B:
Intracameral phenylephrine 1.5% for prophylaxis against
intraoperative floppy iris syndrome: Prospective, randomized fellow
eye study. Ophthalmology. 119:2053–2058. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chao DL, Modi YS, Lee B, Sridhar J,
Kuriyan AE and Gedde SJ: Review of effects of tamsulosin and
silodosin on isolated albino and pigmented rabbit iris dilators:
Possible mechanism of intraoperative floppy-iris syndrome. Eye
World ASCRS Publication. 2012.
|
|
13
|
Masket S and Chang DF: Intraoperative
Floppy Iris Syndrome A systemic approach. J Cataract Refract Surg
Today. 10:68–73. 2010.
|
|
14
|
Haridas A, Syrimi M, Al-Ahmar B and
Hingorani M: Intraoperative floppy iris syndrome (IFIS) in patients
receiving tamsulosin or doxazosin-a UK-based comparison of
incidence and complication rates. Graefes Arch Clin Exp Ophthalmol.
251:1541–1555. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cheung CM, Awan MA and Sandramouli S:
Prevalence and clinical findings of tamsulosin-associated
intraoperative floppy-iris syndrome. J Cataract Refract Surg.
32:1336–1339. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schwinn DA and Afshari NA: Alpha
(1)-Adrenergic receptor antagonists and the iris: New mechanistic
insights into floppy iris syndrome. Surv Ophthalmol. 51:501–512.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wong AC and Mak ST: Finasteride-associated
cataract and intraoperative floppy-iris syndrome. J Cataract
Refract Surg. 37:1351–1354. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chatziralli IP, Sergentanis TN, Papazisis
L and Moschos MM: Risk factors for intraoperative floppy iris
syndrome: A retrospective study. Acta Ophthalmol. 90:e152–e153.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pringle E and Packard R: Antipsychotic
agent as an etiologic agent of IFIS. J Cataract Refract Surg.
31:2240–2241. 2015. View Article : Google Scholar
|
|
20
|
Unal M, Yücel I and Tenlik A:
Intraoperative floppy-iris syndrome associated with chronic use of
chloropromazine. Eye (Lond). 21:1241–1242. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Altiaylik Ozer P, Altiparmak UE, Unlu N,
Hazirolan DO, Kasim R and Duman S: Intraoperative floppy-iris
syndrome: Comparison of tamsulosin and drugs other than alpha
antagonists. Curr Eye Res. 38:480–486. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Papadopoulos R and Bachariou A:
Intraoperative floppy-iris syndrome associated with chronic intake
of donepezil. J Cataract Refract Surg. 33:1997–1998. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bilgin B, Ilhan D, Çetinkaya A and Ünal M:
Intraoperative floppy iris syndrome associated with quetiapine. Eye
(Lond). 27:6732013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ford RL, Sallam A and Towler HM:
Intraoperative floppy iris syndrome associated with risperidone
intake. Eur J Ophthalmol. 21:210–211. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gupta A and Srinivasan R: Floppy iris
syndrome with oral imipramine: A case series. Indian J Ophthalmol.
60:136–138. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
González-Martín-Moro J, González-López JJ,
Zarallo-Gallardo J and Fernández-Miguel Y: Intraoperative floppy
iris syndrome after treatment with duloxetine: Coincidence,
association, or causality? Arch Soc Esp Oftalmol. 90:94–96.
2015.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Asensio-Sánchez VM: Intraoperative floppy
iris syndrome and warfarin: Coincidence or side effect? Arch Soc
Esp Oftalmol. 88:1602013.(In English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Neff KD, Sandoval HP, Fernández de Castro
LE, Nowacki AS, Vroman DT and Solomon KD: Factors associated with
intraoperative floppy iris syndrome. Ophthalmology. 116:658–663.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yu Y and Koss MC: Studies of alfa
adrenoreceptor antagonists on simpathetic in rabbits. J Ocul
Pharmacol Ther. 19:255–263. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hovanesian JA and Chang DF: State of the
art: Intraoperative floppy iris syndrome. Ocular Surg News U.S.
Edition. March 10–2008.
|