Introduction
Patients with type 2 diabetes mellitus and coronary
heart disease usually have abnormal blood lipids, vascular
endothelial dysfunctions, insulin resistance and increased
inflammatory cells (1). For patients
with type 2 diabetes mellitus and coronary heart disease, the
comprehensive effect of multiple risk factors can lead to rapid
progression of the diseases, such as severe complications of the
heart, brain, liver, kidney and other important organs in the early
stage (2). Studies have confirmed
that increase in blood lipids, injury of vascular endothelial
cells, increase in inflammatory responses and insulin resistance
are the independent risk factors for the occurrence and development
of coronary heart disease and (or) type 2 diabetes mellitus
(3). Therefore, adjusting the level
of blood lipids effectively has significant value to alleviate the
severity, slow the progression and reduce the occurrence of
complications of type 2 diabetes mellitus and coronary heart
disease (4).
Statins can play a role in regulating the blood
lipids through selectively competitive inhibition of
3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase (5). As to treatment of coronary heart
disease, statins can effectively lower the levels of serum total
cholesterol (TC), triglyceride (TG) and other indexes related to
blood lipids; moreover, they can increase the level of high-density
lipoprotein cholesterol (HDL-C), slow the progression of
atherosclerosis, stabilize plaques and reduce the risk of
thromboembolism (6). For patients
with diabetes mellitus, statins have certain functions of lowering
inflammatory response factor level in the body, improving the
vascular endothelial functions, exerting anti-oxidation and
enhancing insulin sensitivity (7).
Rosuvastatin is a kind of water-soluble statin that is often used
at present; compared with lipid-soluble statins, it has shorter
onset time and better efficacy in clinic. Although there have been
studies on the treatment of diabetes mellitus, coronary heart
disease and hyperlipidemia with rosuvastatin in clinical practice
(8), after the treatment with
rosuvastatin of type 2 diabetes mellitus combined with coronary
heart disease, the blood lipid index and insulin resistance, the
correlation between the changes of inflammatory factors and the
function of endothelial cells is rarely reported. This research
focused on treatment with rosuvastatin on patients with diabetes
mellitus and coronary heart disease and investigated its effect on
vascular endothelial functions and inflammatory factors in the
body.
Materials and methods
General information
Eighty patients with type 2 diabetes mellitus and
coronary heart disease, who were admitted and treated in Center
hospital of Zibo (Zibo, China) from January 2016 to January 2017,
were selected; for all the enrolled patients, the coronary heart
disease was confirmed by coronary angiography, and type 2 diabetes
mellitus was confirmed by glucose tolerance test and glucose
determination. Before enrollment, the patients were advised, and
signed the informed consent; and, this study was approved by the
Ethics Committee of Center Hospital of Zibo (no. ZBCH2015-03).
Patients who were complicated with systemic infection, malignant
tumors, mental diseases, systemic immune system dysfunctions or
other endocrine system diseases, who had been treated with
glucocorticoid and (or) immunodepressant for 3 months before
enrollment, and who signed the informed consent but refused to be
enrolled, were excluded. All the patients were divided into
observation group (n=40) and control group (n=40) by the random
number table. In observation group, there were 26 men and 14 women
aged 50–75 years, with an average age of 67.1±1.2 years; the
duration of diabetes mellitus was 5–40 years, with an average
duration of 25.1±2.1 years, and the duration of coronary heart
disease was 5–30 years, with an average duration of 18.2±1.0 years.
In control group, there were 25 men and 15 women aged 50–75 years,
with an average age of 67.0±1.3 years; the duration of diabetes
mellitus was 5–40 years, with an average duration of 25.0±2.0
years, and the duration of coronary heart disease was 5–30 years,
with an average duration of 18.1±0.9 years. The differences in sex,
age as well as duration of diabetes mellitus and coronary heart
disease between the two groups were not statistically significant
(P>0.05).
Methods
Symptomatic and supporting therapy was used for
patients with type 2 diabetes mellitus and coronary heart disease
in control group, including oral administration of metformin (0.5
g, b.i.d. National Medicine Permission No. H11021518, Beijing
Jingfeng Pharmaceutical Co., Ltd., Beijing, China) for blood
glucose control, Captopril (12.5–25.0 mg 3 times a day, National
Medicine Permission No.: H44024904, Shantou Jinshi Pharmaceutical
General Factory, Shezhen, China) for blood pressure regulation,
anticoagulation, Enteric Aspirin Tablets (100 mg daily before
bedtime, National Medicine Permission No. H20065051 Shenyang Orge
Pharmaceutical Co., Ltd., Liaoning, China) for platelet inhibition,
oral administration of levocarnitine (3 g per day, three times a
day, National Medicine Permission No. H19990372, Northeastern
Pharmaceutical Group Shenyang First Pharmaceutical Co., Ltd.,
Liaoning, China) heart protection; in observation group,
rosuvastatin (Simcere Pharmaceutical Group, Nanjing, China;
National Medicine Permission No. H20113246) was adopted on the
basis of treatment for control group. The drug (10 mg) was orally
administered once at bedtime every day for a 3-month treatment
cycle. Outpatient follow-up was conducted for all the patients.
Observation indexes
Indexes related to blood lipids [such as TC, TG, low
density lipoprotein cholesterol (LDL-C) and HDL-C] (Cholesterol
determination kit, cat. no. YZB/Gui 0128-2013; Sichuan Mike
Biotechnology Co., Ltd., Chengdu, China), diabetes mellitus
[fasting insulin (FINS) and homeostasis model assessment of insulin
resistance (HOMA-IR)], inflammation-associated cytokines [including
variations in tumor necrosis factor-alpha (TNF-α) and
high-sensitivity C-reactive protein (hs-CRP)] and vascular
endothelial activity [changes in endothelin-1 (ET-1) and nitric
oxide (NO) levels] before and after intervention were compared; the
correlations of changes in TC with those in FINS, hs-CRP and ET-1
were analyzed.
Evaluation indexes
The enrolled patients underwent more than 8 h of
fasting, followed by collection of venous blood from the elbow in
the morning, which was taken as the specimen. The main detections
for the indexes related to blood lipids included TC (<5.20
mmol/l), TG (<1.70 mmol/l), LDL-C (<3.12 mmol/l) and HDL-C
(>1.04 mmol/l). All those detections were performed using
Aeroset automatic biochemistry analyzer (Abbott Pharmaceutical Co.
Ltd., Lake Bluff, IL, USA). HOMA-IR = [fasting blood glucose
(mmol/l) × FINS (mU/l)]/22.5, of which the normal range of FINS was
3.0–24.9 U/ml and the normal value of HOMA-IR was 1. Moreover,
Beckman Access DXI 800 Type analyzer (Beckman Coulter Inc., Brea,
CA, USA) as well as spectrophotometric method (Bio-Rad
Laboratories, Inc., Hercules, CA, USA) were applied to measure the
FINS. Detection of inflammatory cytokines: Double-antibody
single-step sandwich method was adopted to detect the TNF-α, of
which the normal reference value in adults was 5–100 ng/l; latex
particle-enhanced turbidimetric immunoassay was performed to
measure hs-CRP, and the level ≤10 mg/l was regarded as the normal
reference value in adults; radioimmunoassay was applied to examine
ET-1 and the normal reference value in adults was 43.50–58.38 ng/l;
enzyme-linked immunosorbent assay kit (Thermo Fisher Scientific,
Inc., Waltham, MA, USA) was used for NO measurement.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
21.0 (IBM Corp., Armonk, NY, USA) was applied for statistical
processing; the measurement data were presented as mean ± standard
deviation and were calculated as percent (%). The levels of indexes
related to blood lipid and HOMA-IR, ET-1, NO and inflammatory
cytokines were compared by Student's t-test. ANOVA was used for
comparison between multiple groups and the post hoc test was SNK
test, and scatterplot was utilized for Spearman's correlation
analysis. P<0.05 indicated that the difference was statistically
significant.
Results
Comparison of indexes related to blood
lipid before and after intervention
Among the blood lipid indexes of the patients, the
levels of TC, TG and LDL-C after intervention were significantly
lower than those before intervention (P<0.05), while the HDL-C
level after intervention was higher than that before intervention
(P<0.05) (Table I).
 | Table I.Comparison of indexes related to blood
lipid before and after intervention (mmol/l, mean ± SD). |
Table I.
Comparison of indexes related to blood
lipid before and after intervention (mmol/l, mean ± SD).
|
| TC | TG | LDL-C | HDL-C |
|---|
| Before
intervention | 6.24±0.02 | 2.41±0.02 | 3.54±0.02 | 1.13±0.01 |
| After
intervention | 5.41±0.01 | 1.86±0.01 | 2.55±0.02 | 1.42±0.02 |
| t value | 234.759 | 155.563 | 221.371 | 73.539 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 |
Comparison of FINS and HOMA-IR levels
before and after intervention
Compared with those before intervention, the level
of FINS after intervention was remarkably elevated (P<0.05),
while the HOMA-IR level after intervention was significantly
reduced (P<0.05) (Table II).
 | Table II.Comparison of FINS and HOMA-IR levels
before and after intervention (mean ± SD). |
Table II.
Comparison of FINS and HOMA-IR levels
before and after intervention (mean ± SD).
|
| FINS (mU/l) | HOMA-IR |
|---|
| Before
intervention | 4.6±0.1 | 1.4±0.2 |
| After
intervention | 8.5±0.3 | 1.0±0.1 |
| t value | 78.000 | 11.314 |
| P-value | <0.001 | <0.001 |
Comparison of levels of
inflammation-associated cytokines before and after
intervention
After intervention, the levels of hs-CRP and TNF-α
in the patients were obviously decreased compared with those before
intervention (P<0.05) (Table
III).
 | Table III.Comparison of levels of
inflammation-associated cytokines before and after intervention
(mean ± SD). |
Table III.
Comparison of levels of
inflammation-associated cytokines before and after intervention
(mean ± SD).
|
| hs-CRP (mg/l) | TNF-α (ng/l) |
|---|
| Before
intervention | 11.5±1.2 | 138.1±11.4 |
| After
intervention |
6.1±0.1 | 75.3±5.0 |
| t value | 28.362 | 31.907 |
| P-value | <0.001 | <0.001 |
Comparison of ET-1 and NO levels
before and after intervention
Compared with that before intervention, the ET-1
level was decreased (P<0.05), while the NO level was elevated
after intervention (P<0.05) (Table
IV).
 | Table IV.Comparison of ET-1 and NO levels
before and after intervention (mean ± SD). |
Table IV.
Comparison of ET-1 and NO levels
before and after intervention (mean ± SD).
|
| ET-1 (ng/l) | NO (µmol/l) |
|---|
| Before
intervention | 98.6±6.21 | 23.5±1.8 |
| After
intervention | 47.5±3.20 | 28.9±2.1 |
| t value | 46.262 | 12.348 |
| P-value | <0.001 | <0.001 |
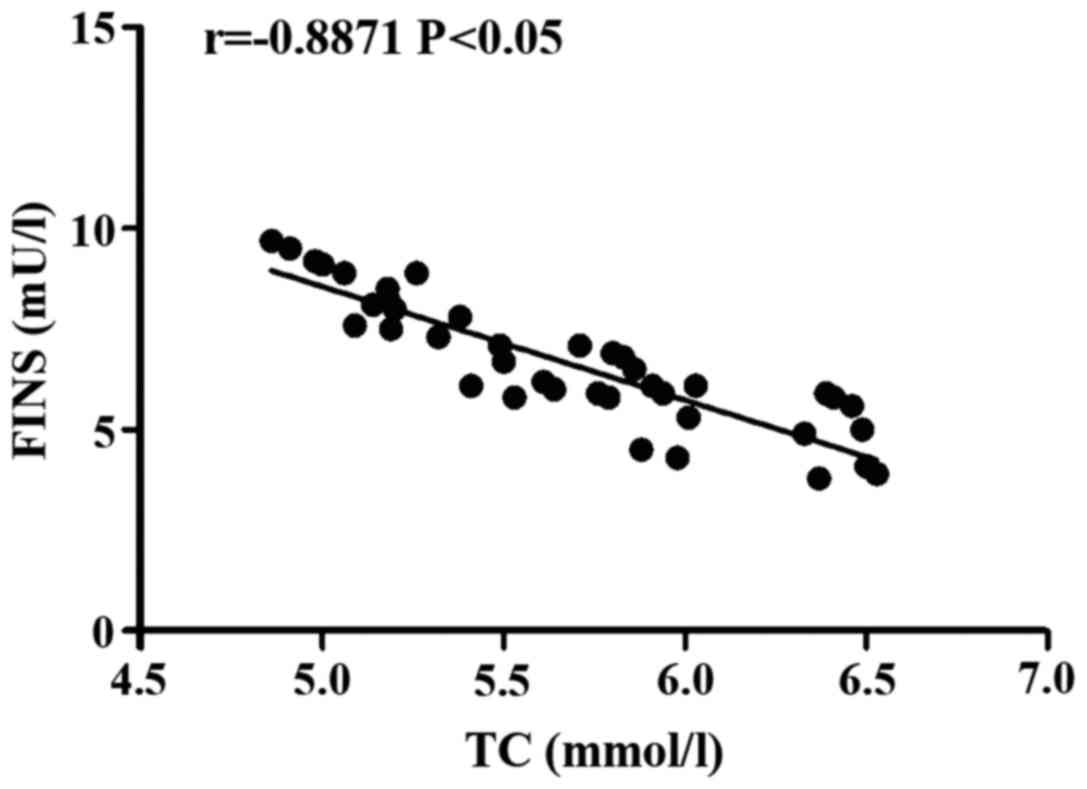
Correlation analysis of TC with FINS in the process
of treatment on patients with diabetes mellitus and coronary heart
disease using rosuvastatin. The TC level was negatively correlated
with FINS level (r= −0.8871, P<0.05) (Fig. 1).
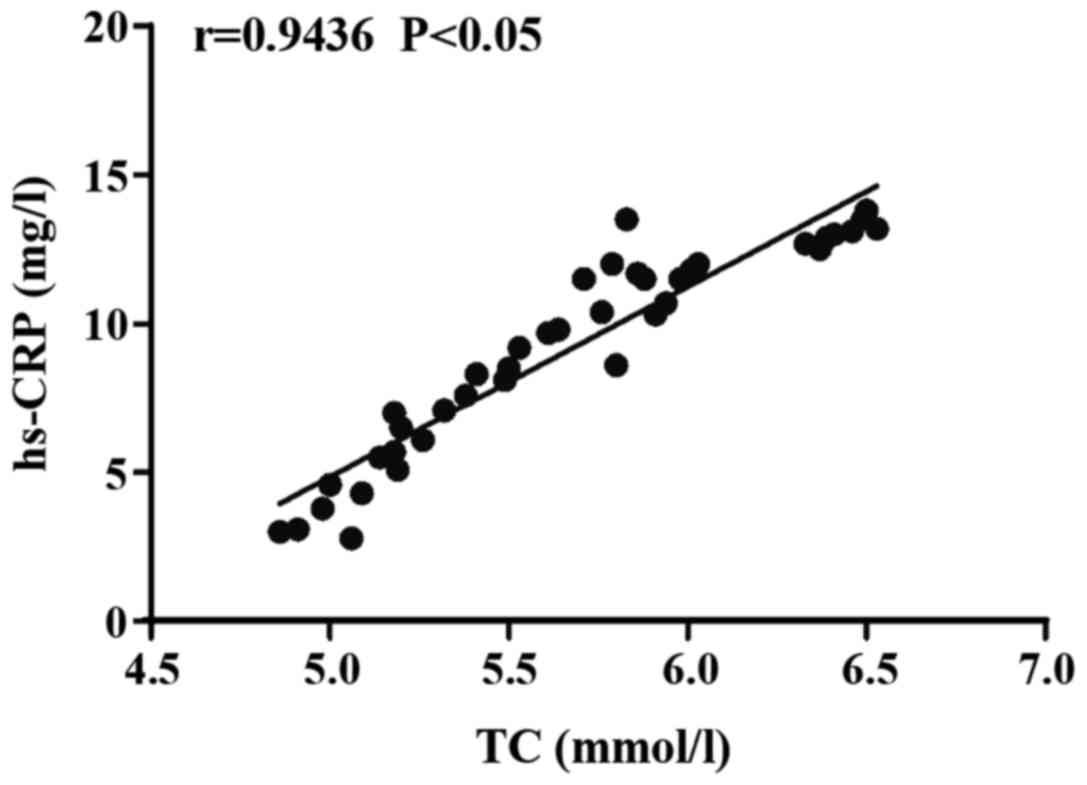
Correlation analysis of TC with hs-CRP
in the process of treatment on patients with diabetes mellitus and
coronary heart disease using rosuvastatin
The TC level was positively correlated with hs-CRP
level (r=0.9436, p=0.000<0.05) (Fig.
2).
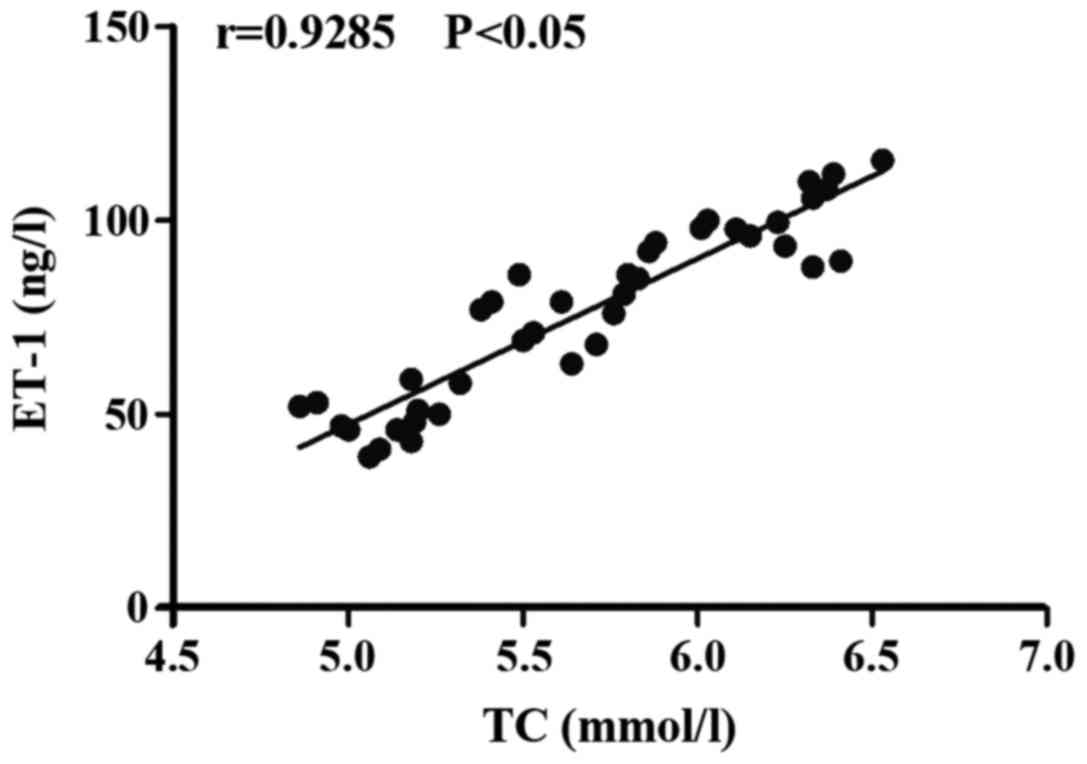
Correlation analysis of TC with ET-1
in the process of treatment on patients with diabetes mellitus and
coronary heart disease using rosuvastatin
The TC level was positively correlated with ET-1
level (r=0.9285, P<0.05) (Fig.
3).
Discussion
With the progression in aging of population,
improvement in living standards and changes in lifestyle and
dietary patterns in China, the proportion of type 2 diabetes
mellitus complicated with coronary heart disease has increased
significantly (9). Both type 2
diabetes mellitus and coronary heart disease are the most common
kinds of chronic and incurable internal diseases at present, which
have high disability rates and fatality rates (10). Type 2 diabetes mellitus can cause
metabolism disorders of carbohydrates and lipids which are energy
substances, thus accelerating the occurrence and development of
coronary atherosclerosis and leading to severely adverse prognosis
(11). So far, some studies have
confirmed that the metabolic disorder of blood lipid is an
independent risk factor for the onset of the above-mentioned
diseases (12); therefore, it is
very important for patients with type 2 diabetes mellitus and
coronary heart disease to effectively regulate their blood lipid
level. Rosuvastatin, a statin that is most commonly used to
regulate the metabolism of blood lipid in current clinical
practices, is mainly extracted by fermentation of Aspergillus
terreus, which can effectively suppress the synthesis of
endogenous cholesterol, thus lowering the blood lipid level
(13). As a result, the role of
rosuvastatin in regulating the blood lipid has been proved
clinically. The effect of rosuvastatin, however, on endothelial
functions and inflammatory response factors in patients with type 2
diabetes mellitus and coronary heart disease needs to be further
elucidated.
In this research, rosuvastatin was utilized for
treatment; by comparing the indexes related to blood lipid of the
patients before and after intervention, it was found that the
levels of TC, TG and LDL-C after intervention were significantly
lower than those before intervention, while the HDL-C level after
intervention was higher than that before intervention. It suggested
that treatment with rosuvastatin can effectively regulate the blood
lipid level of patients with type 2 diabetes mellitus and coronary
heart disease. In terms of testing indexes related to diabetes
mellitus, it was shown that compared with that before intervention,
the level of FINS after intervention was remarkably higher, while
the HOMA-IR level after intervention was significantly lower. It
indicated that applying rosuvastatin to type 2 diabetes mellitus
complicated with coronary heart disease has a significant value in
improving insulin function in the body and ameliorating insulin
resistance. Furthermore, the variations in levels of
inflammation-associated cytokines and vascular endothelial
functions before and after intervention were studied, and the
results revealed that the levels of hs-CRP and TNF-α in the
patients after intervention were obviously decreased compared with
those before intervention; compared with those before intervention,
the ET-1 level was decreased, while the NO level was elevated after
intervention. It suggested that for type 2 diabetes mellitus
complicated with coronary heart disease, treatment using
rosuvastatin can remarkably reduce inflammatory responses in the
body and improve the vascular endothelial functions. In addition,
the correlations of changes in TC with those in FINS, hs-CRP and
ET-1 in the process of treating patients with diabetes mellitus and
coronary heart disease using rosuvastatin were analyzed, and it was
discovered that the TC level was negatively correlated with FINS
level but positively correlated with the levels of hs-CRP and
ET-1.
As the most common kind of water-soluble drug
utilized to regulate lipid metabolism at present, rosuvastatin has
relatively strong cell membrane penetration ability, so that it can
exert its clinical efficacy by quickly entering the cytoplasm and
nucleus (14). As a selective
HMG-CoA reductase inhibitor (15),
the drug can effectively restrain the synthesis of precursor of
cholesterol in the body, elevate the level of LDL receptor on the
liver cell surface and promote its absorption, thus lowering the
levels of TG, TC and LDL-C and raising the HDL-C level (16). Moreover, rosuvastatin can inhibit the
signaling pathways in the process of cell signal transduction and
strengthen its binding to lymphocyte function-associated antigen l
(LFA-1), thus controlling the binding rate of lymphocytes to
intracellular adhesion molecule-1 (ICAM-1) and exerting the
immunosuppressive effects (17); as
a result, the levels of inflammation-associated cytokines in the
body are decreased. Therefore, after treatment with rosuvastatin,
the levels of hs-CRP and TNF-α in the body are decreased
significantly (18). At the same
time, rosuvastatin can lower the messenger RNA (mRNA) expression of
preproendothelin-1 (PPET-1), the precursor of ET-1, in the body and
then reduce the activity of ET-1 and its binding rate to receptors
(19); furthermore, it can increase
the expression level of endothelial nitric oxide synthase and
reduce the negative regulation of oxidized LDL on mRNA of
endothelial nitric oxide synthase, thus increasing the NO level in
the body (20).
In conclusion, for patients with type 2 diabetes
mellitus and coronary heart disease, treatment with rosuvastatin
can effectively lower the levels of blood lipids and regulate
insulin functions; moreover, potent decrease in blood lipid levels
has great significance in improving the vascular endothelial
functions and reducing inflammatory responses.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GM and SB were responsible for the observation
and the analysis of the indexes. GM collected and analyzed the
general data of the patients. Both authors read and approved the
final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Center Hospital of Zibo (Zibo, China) (no. ZBCH2015-03). The
patients were advised, and signed the informed consent
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Foley TR, Singh GD, Kokkinidis DG, Choy
HK, Pham T, Amsterdam EA, Rutledge JC, Waldo SW, Armstrong EJ and
Laird JR: High-intensity statin therapy is associated with improved
survival in patients with peripheral artery disease. J Am Heart
Assoc. 6:e0056992017.PubMed/NCBI
|
|
2
|
Liang M, Yang S and Fu N: Efficacy of
short-term moderate or high-dose rosuvastatin in preventing
contrast-induced nephropathy: A meta-analysis of 15 randomized
controlled trials. Medicine (Baltimore). 96:e73842017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kwon O, Kang SJ, Kang SH, Lee PH, Yun SC,
Ahn JM, Park DW, Lee SW, Kim YH, Lee CW, et al: Relationship
between serum inflammatory marker levels and the dynamic changes in
coronary plaque characteristics after statin therapy. Circ
Cardiovasc Imaging. 10:e0059342017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Roy S, Weinstock JL, Ishino AS, Benites
JF, Pop SR, Perez CD, Gumbs EA, Rosenbaum JA, Roccato MK, Shah H,
et al: Association of cognitive impairment in patients on
3-hydroxy-3-methyl-glutaryl-CoA reductase inhibitors. J Clin Med
Res. 9:638–649. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ovrakh T, Serik S and Kochubiei O: Impact
of atorvastatin and rosuvastatin on residual on-clopidogrel
treatment platelet reactivity in patients with ischemic heart
disease and type 2 diabetes mellitus after acute coronary syndrome.
Georgian Med News. 4:7–14. 2017.(In Russian).
|
|
6
|
Jellinger PS, Handelsman Y, Rosenblit PD,
Bloomgarden ZT, Fonseca VA, Garber AJ, Grunberger G, Guerin CK,
Bell DSH, Mechanick JI, et al: American Association of Clinical
Endocrinologists and American College of Endocrinology guidelines
for management of dyslipidemia and prevention of cardiovascular
disease. Endocr Pract. 23 Suppl 2:1–87. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang W, Yi L, Jin C, Xu S, Bi X, Zhao Y,
Qiu F, Fu G and Min W: The impact of rosuvastatin on the density
score of coronary artery calcification in coronary artery disease
patients with type 2 diabetes mellitus: Rationale and design of
RosCal Study. Clin Drug Investig. 36:1023–1029. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ullah F, Afridi AK, Rahim F, ur Rahman S
and Ashfaq M: Efficacy of 5 mg and 10 mg rosuvastatin in type-2
diabetes mellitus with hypercholesteroalemia. J Ayub Med Coll
Abbottabad. 27:564–568. 2015.PubMed/NCBI
|
|
9
|
Xiong X, Liu H, Hua L, Zhao H, Wang D and
Li Y: The association of HDL-apoCIII with coronary heart disease
and the effect of statin treatment on it. Lipids Health Dis.
14:1272015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gungoren F, Besli F, Caliskan S, Polat U,
Basar C and Serdar OA: Statin therapy may not effect NLR and MPV
levels in patients with hypercholesterolemia: A retrospective
study. Angiology. 67:536–540. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Koshelskaia OA, Vinnitskaia IV, Konko TI,
Kravchenko ES, Suslova TE and Karpov RS: Comparative randomized
study of the effects of long-term therapy with rosuvastatin and
combination of atorvastatin and ezetimibe on carbohydrate
metabolism and adipokines levels in patients with coronary artery
disease and diabetes mellitus. Kardiologiia. 55:67–74. 2015.
View Article : Google Scholar
|
|
12
|
Terao Y, Satomi-Kobayashi S, Hirata K and
Rikitake Y: Involvement of Rho-associated protein kinase (ROCK) and
bone morphogenetic protein-binding endothelial cell
precursor-derived regulator (BMPER) in high glucose-increased
alkaline phosphatase expression and activity in human coronary
artery smooth muscle cells. Cardiovasc Diabetol. 14:1042015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Suthar KS, Vanikar AV and Trivedi HL:
Acute kidney injury and quadriparesis due to rosuvastatin induced
rhabdomyolysis - a case report. J Clin Diagn Res. 9:OD08–OD09.
2015.PubMed/NCBI
|
|
14
|
Laires PA, Ejzykowicz F, Hsu TY,
Ambegaonkar B and Davies G: Cost-effectiveness of adding ezetimibe
to atorvastatin vs switching to rosuvastatin therapy in Portugal. J
Med Econ. 18:565–572. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Laufs U, Gertz K, Dirnagl U, Böhm M,
Nickenig G and Endres M: Rosuvastatin, a new HMG-CoA reductase
inhibitor, upregulates endothelial nitric oxide synthase and
protects from ischemic stroke in mice. Brain Res. 942:23–30. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Halcox JP, Tubach F, Lopez-Garcia E, De
Backer G, Borghi C, Dallongeville J, Guallar E, Medina J, Perk J,
Sazova O, et al: Low rates of both lipid-lowering therapy use and
achievement of low-density lipoprotein cholesterol targets in
individuals at high-risk for cardiovascular disease across Europe.
PLoS One. 10:e01152702015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ball T and McCullough PA: Statins for the
prevention of contrast-induced acute kidney injury. Nephron Clin
Pract. 127:165–171. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Puri R, Nissen SE, Shao M, Ballantyne CM,
Barter PJ, Chapman MJ, Erbel R, Libby P, Raichlen JS, Uno K, et al:
Sex-related differences of coronary atherosclerosis regression
following maximally intensive statin therapy: Insights from SATURN.
JACC Cardiovasc Imaging. 7:1013–1022. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu YH, Liu Y, Duan CY, Tan N, Chen JY,
Zhou YL, Li LW and He PC: statins for the prevention of
contrast-induced nephropathy after coronary
angiography/percutaneous interventions: A meta-analysis of
randomized controlled trials. J Cardiovasc Pharmacol Ther.
20:181–192. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stegman B, Puri R, Cho L, Shao M,
Ballantyne CM, Barter PJ, Chapman MJ, Erbel R, Libby P, Raichlen
JS, et al: High-intensity statin therapy alters the natural history
of diabetic coronary atherosclerosis: Insights from SATURN.
Diabetes Care. 37:3114–3120. 2014. View Article : Google Scholar : PubMed/NCBI
|