Introduction
Acute respiratory distress syndrome (ARDS) is
characterized by progressive hypoxemia caused by multiple factors.
The main clinical feature of ARDS is progressive hypoxemia. Its
early clinical features are increased capillary permeability and
coagulation dysfunction (1,2). Traumatic systemic inflammatory response
caused by lung injury is considered to be the main cause of ARDS.
In spite of the efforts made in the treatment of ARDS, mortality of
this disease is still as high as 30–60% (3–5).
Increased incidence of abdominal trauma caused by impact injuries,
crush injuries, and high-altitude crashes also increase the
incidence of ARDS. Excessive infusion is also one of the main
causes of ARDS. Therefore, abdominal surgery is a high risk of
ARDS, and ARDS is also one of the most serious complications after
abdominal injury. ARDS can cause serious disorder in the patient's
internal environment, resulting in the patient's whole body
sequential organ failure, which greatly increases the patient's
mortality rate (6–8). However, risk factors for patients with
ARDS after abdominal surgery still have not been well studied. In
this study, clinical data of patients with simple abdominal trauma
after surgery were retrospectively analyzed and compared between
patients with and without ARDS to explore the risk factors for ARDS
after abdominal surgery.
Patients and methods
Subjects
A total of 532 patients who underwent abdominal
surgery from February 2006 to May 2016 in Dongyang People's
Hospital (Dongyang, China) were selected. Among them, 113 patients
had ARDS after surgery and 45 patients died. Those patients were
included in observation group. The 419 patients who did not develop
ARDS were included in control group, and 11 patients in control
group died. All patients in observation group met the criteria for
ARDS diagnosis (9). All patients
were older than 18 years and had simple abdominal trauma. Patients
with allergies, pregnant women, and patients who gave up treatment
were excluded. This study was approved by the Medical Ethics
Committee of Dongyang People's Hospital, and patients or their
families signed informed consent.
ARDS diagnostic criteria
All 113 patients in observation group met the ARDS
Berlin definition of 2012. There are high risk factors for direct
lung injury or indirect injury. Acute onset, heart failure, and
fluid overload do not fully explain respiratory failure, and there
is no high hydrostatic pulmonary edema. Hypoxemia: PaO2/FiO2 ≤300
mmHg in acute lung injury and PaO2/FiO2 ≤200 mmHg in ARDS. Chest
imaging changes, chest X-ray or CT scan images show infiltrated
shadows in both lungs. Pulmonary arterial wedge pressure ≤18 mmHg
or left atrial hypertension was excluded.
Conventional treatment
Patients in control group received conventional
treatment including improvement of body's inflammatory response,
fluid management, nutritional and metabolic support, respiratory
support therapy, and other organ function support.
ARDS treatment plan
Patients in observation group received ARDS
treatment program on the basis of routine treatment to control the
causes, including drainage, debridement, anti-inflammation
treatment with aspirin purchased from Jiaxing Nanjian Biological
Materials Co., Ltd., (item no: 50-78-2; Jiaxing, China) and
hypoxemia correction. Under the premise of maintaining adequate
cardiac output, early diuresis and regulation of infusion volume
were performed. A lower preload of the heart was maintained so that
the incarceration pressure of the pulmonary artery does not exceed
1.6 kPa. Nutrition support was performed with the total calories
less than 30 kcal/kg.
Observation indicators
General information including sex, age, infection,
type of injury, number of damaged organs, trauma-to-operative time,
prognosis and body mass index (BMI) were collected. Pretreatment
heart rate, PaO2/FiO2, blood glucose, procalcitonin (PCT), albumin
(ALB), white blood cell count (WBC), acute disease physiology,
long-term health assessment (APACHE) II scores, perioperative
bleeding volume, blood transfusion volume and infusion volume were
also recorded.
Statistical analysis
SPSS 19.0 (SPSS, Inc., Chicago, IL, USA) was used.
Enumeration data were expressed as rate, and compared by using
χ2 test. Measurement data are expressed as mean ± SD and
distribution of data was analyzed by Kaplan-Meier method and the
log-rank test. Risk factor analysis and prognostic factor analysis
were performed by using logistic regression analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
General data
There were 419 patients in control group, including
316 male patients and 103 female patients, with an average age of
46.5±16.2 years. There were 113 patients in observation group,
including 84 male patients and 29 female patients, with an average
age of 55.8±16.9 years. There was no significant difference in sex
proportion, injury type and number of injured organs between the
two groups (P>0.05). There was a significant difference in age,
infection, trauma-to-surgery time, and prognosis between the two
groups (P<0.05) (Table I).
 | Table I.General data. |
Table I.
General data.
| Characteristics | Control (n=419) | Observation
(n=113) | Statistical
value | P-value |
|---|
| Sex [n (%)] |
|
|
0.013 | 0.807 |
| Male | 316 (75.4) | 84 (74.3) |
|
|
|
Female | 103 (24.6) | 29 (25.7) |
|
|
| Age | 46.5±16.2 | 55.8±16.9 |
5.336 | <0.001 |
| Infection [n
(%)] |
|
|
50.306 | <0.001 |
| Yes | 71
(16.9) | 56 (49.6) |
|
|
| No | 348 (83.1) | 57 (50.4) |
|
|
| Damage type [n
(%)] |
|
|
0.087 | 0.742 |
| Open | 262 (62.5) | 73 (64.6) |
|
|
|
Closed | 157 (37.5) | 40 (35.4) |
|
|
| Damaged organ number
[n (%)] |
|
|
0.000 | 1.000 |
| ≤2 | 291 (69.5) | 79 (69.9) |
|
|
|
>2 | 128 (30.5) | 34 (30.1) |
|
|
| Trauma-to-surgery
time [n (%)] |
|
|
23.411 | <0.001 |
| ≤12
h | 386 (92.1) | 85 (75.2) |
|
|
| >12
h | 33 (7.9) | 28 (24.8) |
|
|
| Prognosis [n(%)] |
|
| 126.830 | <0.001 |
|
Survive | 408 (97.4) | 68 (60.2) |
|
|
|
Death | 11 (2.6) | 45 (39.8) |
|
|
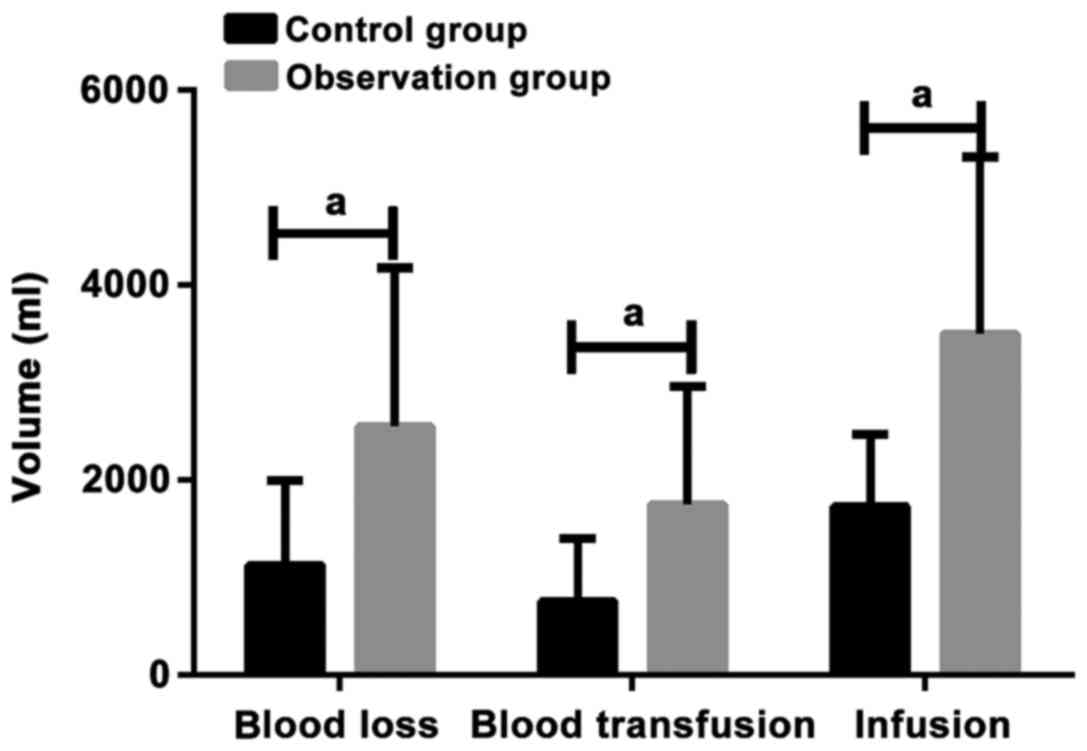
Perioperative conditions analysis
In control group, amount of blood loss was
1125.4±869.5 ml, blood transfusion volume was 756.4±642.1 ml, and
infusion volume was 1725.4±744.4 ml. In observation group, blood
loss volume was 2548.7±1,622.5 ml, blood transfusion volume was
1748.6±1,215.9 ml, and infusion volume was 3499.4±1819.6 ml. The
perioperative blood loss, blood transfusion, and infusion volume in
observation group were significantly higher than those in control
group (P<0.05) (Table II and
Fig. 1).
 | Table II.Analysis of perioperative conditions
(ml). |
Table II.
Analysis of perioperative conditions
(ml).
| Conditions | Control (n=419) | Observation
(n=113) | Statistical
value | P-value |
|---|
| Blood loss | 1,125.4±869.5 | 2,548.7±1,622.5 | 12.51 | <0.001 |
| Blood transfusion
volume |
756.4±642.1 | 1,748.6±1,215.9 | 11.72 | <0.001 |
| Infusion volume | 1,725.4±7,44.4 | 3,499.4±1,819.6 | 15.70 | <0.001 |
Analysis of vital signs of two groups
of patients
There was no significant difference in BMI and WBC
between two groups (P>0.05). There were differences in heart
rate, PaO2/FiO2, ratio of high (low) glucose, PCT, and ALB between
two groups. Heart rate and PCT were higher in observation group
than in control group (P<0.05). Percentage of hyperglycemic
patients, PaO2/FiO2, and ALB were lower in observation group than
those in control group (P<0.05, Table III).
 | Table III.Analysis of vital signs of two groups
of patients. |
Table III.
Analysis of vital signs of two groups
of patients.
| Vital signs | Control (n=419) | Observation
(n=113) | Statistical
value | P-value |
|---|
| BMI [n (%)] |
|
|
0.375 | 0.521 |
| <25
kg/m2 | 177 (42.2) | 52 (46.0) |
|
|
| ≥25
kg/m2 | 242 (57.8) | 61 (54.0) |
|
|
| Heart rate
(times/min) |
95.47±10.42 |
98.41±11.32 |
2.612 | 0.009 |
| PaO2/FiO2
(mmHg) | 136.75±56.45 | 121.44±49.26 |
2.626 | 0.009 |
| Blood glucose [n
(%)] |
|
| 14.475 | <0.001 |
| ≤150
mg/dl | 316 (75.4) | 64 (56.6) |
|
|
| >150
mg/dl | 103 (24.6) | 49 (43.4) |
|
|
| PCT (µg/l) |
4.2±1.7 |
4.6±1.5 |
2.274 | 0.023 |
| ALB (g/l) | 27.2±3.8 | 25.4±5.7 |
3.974 | <0.001 |
| WBC
(×109/l) | 11.9±6.8 | 12.2±7.1 |
0.412 | 0.680 |
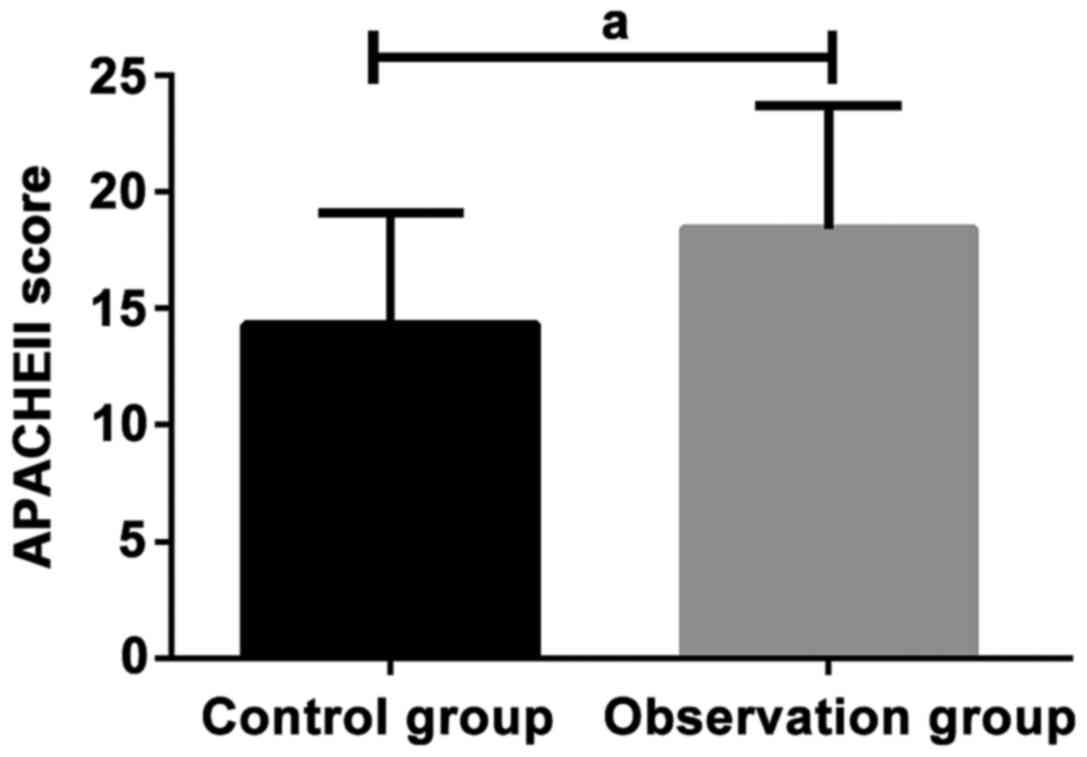
Comparison of APACHE II score between
two groups
APACHE II score in control group was 14.3±4.8, and
APACHE II score in observation group was 18.4±5.3. There was a
significant difference in APACHE II score between two groups.
APACHE II score in observation group was higher than that in the
control group (P<0.05) (Fig.
2).
Analysis of risk factors for ARDS
after abdominal surgery
Occurrence of ARDS (yes=1, no=0) was set as a
dependent variable, and factors with statistical significance were
set as independent variables for logistic regression analysis.
Results showed that occurrence of ARDS after abdominal surgery was
significantly correlated with age, infection, heart rate,
PaO2/FiO2, PCT levels, blood loss, blood transfusion volume, and
fluid volume (P<0.05), but was not correlated with blood glucose
and trauma-to-surgery time (P>0.05) (Table IV).
 | Table IV.Analysis of risk factors for ARDS
after abdominal surgery. |
Table IV.
Analysis of risk factors for ARDS
after abdominal surgery.
| Factors | OR | 95% CI | P-value |
|---|
| Age | 1.463 | 1.064–2.013 | 0.031 |
| Infection | 1.389 | 1.042–1.852 | 0.036 |
| Trauma-to-surgery
time | 0.871 | 0.672–1.130 | 0.152 |
| Heart rate | 0.457 | 0.261–0.801 | 0.019 |
|
PaO2/FiO2 | 0.192 | 0.056–0.661 | 0.024 |
| Blood glucose | 1.814 | 0.925–3.558 | 0.072 |
| PCT | 0.674 | 0.486–0.930 | 0.029 |
| ALB | 1.143 | 0.978–1.335 | 0.047 |
| Blood loss | 0.457 | 0.261–0.801 | 0.025 |
| Blood
transfusion | 13.228 | 1.883–92.936 | 0.001 |
| Infusion
volume | 1.483 | 1.096–1.975 | 0.016 |
Prognostic analysis results
Death of ARDS patients after abdominal surgery was
set as a dependent variable (yes=1, no=0), and factors associated
with ARDS after abdominal surgery and APACHE II score were used as
independent variables to carry out logistic regression analysis.
Results showed that age, infection, heart rate, PaO2/FiO2, ALB, and
APACHE II scores were related to the prognosis of ARDS patients
after abdominal surgery (P<0.05), while PCT levels were not
related to their prognosis (P>0.05, Table V).
 | Table V.Prognostic analysis results. |
Table V.
Prognostic analysis results.
| Factors | OR | 95% CI | P-value |
|---|
| Age | 1.210 | 1.020–1.436 | 0.040 |
| Infection | 0.702 | 0.499–0.986 | 0.048 |
| Heart rate | 1.281 | 1.031–1.591 | 0.036 |
|
PaO2/FiO2 | 0.529 | 0.306–0.916 | 0.035 |
| PCT | 0.789 | 0.625–0.996 | 0.053 |
| ALB | 1.385 | 0.987–1.683 | 0.023 |
| APACHE II
score | 2.380 | 1.341–4.222 | 0.011 |
Discussion
Pathogenesis of ARDS mainly includes direct and
indirect lung injury. Trauma is one of the main causes of indirect
lung injury-induced ARDS, and surgery is also a type of trauma. It
has been reported that approximately 25% of multiple trauma
patients and approximately 40% of emergency infusion patients are
complicated by ARDS. Although in recent years, due to the
application of mechanical ventilation in clinical treatment and the
improved cognition on ARDS, mortality rate of patients with ARDS
has declined, but is still high (10–12).
Therefore, our study aimed to identify risk factors and prognostic
factors of patients with postoperative ARDS, and provide references
for clinical treatment and prognosis of patients with ARDS.
In this study, clinical data of 532 patients
undergoing surgical treatment in Dongyang People's Hospital due to
simple abdominal trauma were retrospectively analyzed. Among them,
ARDS occurred in 113 patients and incidence was approximately
21.2%, which is consistent with previous studies (13,14).
Significant differences in age, infection, heart rate, PaO2/FiO2,
PCT levels, ALB levels, APACHE II scores, trauma-to-surgery time,
blood glucose, blood loss, blood transfusion volume, and infusion
volume were found between two groups. We first analyzed risk
factors for ARDS after abdominal surgery. Logistic regression
analysis showed age, infection, heart rate, PaO2/FiO2, PCT levels,
blood loss, blood transfusion, and infusion volume were closely
correlated with the occurrence of ARDS. Older patients have poor
organ storage function compared to younger patients, and have less
resistance to post-traumatic infections and stress responses, and
are more prone to organ damage (15). Results of this study also showed that
patients with ARDS after surgery are older and had higher infection
rates than patients without ARDS. PCT test results also showed that
patients with ARDS had higher PCT levels than patients without
ARDS. ALB is an acute phase protein. It has been reported that
hypoproteinemia is an independent risk factor for severe ARDS
patients complicated with ARDS, leading to a significant increase
in mortality (16,17).
Hypoproteinemia also affects the patient's colloidal
osmotic pressure, promotes pulmonary edema, and affects patient's
oxygenation capacity (18). Results
of this study also showed that ALB levels and PaO2/FiO2 in patients
with postoperative ARDS were significantly lower than those in
patients without ARDS. Amount of blood loss, blood transfusion, and
infusion volume in ARDS patients were significantly higher than
those in patients without ARDS. Excessive infusion during surgical
operation can dilute blood and decrease plasma colloid osmotic
pressure, further promoting the aggregation of pulmonary edema and
reducing oxygenation ability. Some denatured proteins may also
present in blood with longer storage time and affect patients'
coagulation function (19,20). Therefore, effectively shortening
operation time, effectively and quickly treating the wound, and
timely regulating liquid input during operation may be an effective
means for preventing postoperative ARDS.
We then analyzed the prognostic factors of ARDS. In
this study, among 113 patients, 45 patients died of ARDS after
surgery, and the mortality rate was 39.8%, which is consistent with
the findings in previous studies (21,22).
Prognostic factors of ARDS have long been a focus of clinical
concern. Some studies have reported that mortality of patients with
ARDS is closely related to age, oxygenation index, MODS score, and
APACHE II score (23,24). Consistently, we also found that the
patient's age, oxygenation index, MODS score, and APACHE II are
closely related to prognosis. APACHE II score is more comprehensive
than MODS score. Studies have reported that many patients with ARDS
have organ damage, and APACHE II score is also more sensitive to
the prognosis of patients with ARDS (25,26).
Therefore, MODS was not used in this study. Sensitivity of elderly
patients to drug treatment is poor, which may be a cause of poor
prognosis in elderly patients. Moreover, immune function of elderly
patients is relatively poor, and immunosuppressants can be used
during treatment to support systemic treatment. Tracheal intubation
and mechanical ventilation may also be performed to avoid the
occurrence of multiple infections. This study also has limitations.
Due to the limited experimental resources, some indicators, such as
status of infected bacteria, have not been included in the study.
We will include those factors in our future studies.
In summary, age, infection, heart rate, PaO2/FiO2,
PCT levels, blood loss, blood transfusion, and infusion volume may
be risk factors for ARDS after abdominal surgery. Age, infection,
heart rate, PaO2/FiO2, ALB and APACHE II scores may be related to
the prognosis of patients with ARDS after abdominal surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
BX wrote the manuscript. BX and YG treated patients
and collected the basic data of patients. YL worked on ARDS
treatment program for patients. QC and HZ were responsible for
prognostic analysis. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Dongyang People's Hospital (Dongyang, China). Signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Thompson BT, Chambers RC and Liu KD: Acute
respiratory distress syndrome. N Engl J Med. 377:562–572. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sweeney RM and McAuley DF: Acute
respiratory distress syndrome. Lancet. 388:2416–2430. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stevens JP, Law A and Giannakoulis J:
Acute respiratory distress syndrome. JAMA. 319:7322018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chang Y, Park SH, Huh J-W, Lim C-M, Koh Y
and Hong S-B: Intratracheal administration of umbilical cord
blood-derived mesenchymal stem cells in a patient with acute
respiratory distress syndrome. J Korean Med Sci. 29:438–440. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Grissom CK, Hirshberg EL, Dickerson JB,
Brown SM, Lanspa MJ, Liu KD, Schoenfeld D, Tidswell M, Hite RD,
Rock P, et al: National Heart Lung and Blood Institute Acute
Respiratory Distress Syndrome Clinical Trials Network: Fluid
management with a simplified conservative protocol for the acute
respiratory distress syndrome. Crit Care Med. 43:288–295. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bellani G, Laffey JG, Pham T, Fan E,
Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley
DF, et al: LUNG SAFE Investigators; ESICM Trials Group:
Epidemiology, patterns of care, and mortality for patients with
acute respiratory distress syndrome in intensive care units in 50
countries. JAMA. 315:788–800. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Amato MB, Meade MO, Slutsky AS, Brochard
L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat
A, et al: Driving pressure and survival in the acute respiratory
distress syndrome. N Engl J Med. 372:747–755. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pediatric Acute Lung Injury Consensus
Conference Group: Pediatric acute respiratory distress syndrome:
Consensus recommendations from the Pediatric Acute Lung Injury
Consensus Conference. Pediatr Crit Care Med. 16:428–439. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dizier S, Forel JM, Ayzac L, Richard JC,
Hraiech S, Lehingue S, Loundou A, Roch A, Guerin C and Papazian L:
ACURASYS study investigators; PROSEVA Study Group: Early hepatic
dysfunction is associated with a worse outcome in patients
presenting with acute respiratory distress syndrome: A post-hoc
analysis of the ACURASYS and PROSEVA Studies. PLoS One.
10:e01442782015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Patel BK, Wolfe KS, Pohlman AS, Hall JB
and Kress JP: Effect of noninvasive ventilation delivered by helmet
vs face mask on the rate of endotracheal intubation in patients
with acute respiratory distress syndrome: A randomized clinical
trial. JAMA. 315:2435–2441. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Needham DM, Yang T, Dinglas VD,
Mendez-Tellez PA, Shanholtz C, Sevransky JE, Brower RG, Pronovost
PJ and Colantuoni E: Timing of low tidal volume ventilation and
intensive care unit mortality in acute respiratory distress
syndrome. A prospective cohort study. Am J Respir Crit Care Med.
191:177–185. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Villar J, Blanco J and Kacmarek RM:
Current incidence and outcome of the acute respiratory distress
syndrome. Curr Opin Crit Care. 22:1–6. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Neto AS, Simonis FD, Barbas CS, Biehl M,
Determann RM, Elmer J, Friedman G, Gajic O, Goldstein JN, Linko R,
et al: PROtective Ventilation Network Investigators:
Lung-protective ventilation with low tidal volumes and the
occurrence of pulmonary complications in patients without acute
respiratory distress syndrome: A systematic review and individual
patient data analysis. Crit Care Med. 43:2155–2163. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dessap Mekontso A, Boissier F, Charron C,
Bégot E, Repessé X, Legras A, Brun-Buisson C, Vignon P and
Vieillard-Baron A: Acute cor pulmonale during protective
ventilation for acute respiratory distress syndrome: Prevalence,
predictors, and clinical impact. Intensive Care Med. 42:862–870.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cressoni M, Cadringher P, Chiurazzi C,
Amini M, Gallazzi E, Marino A, Brioni M, Carlesso E, Chiumello D,
Quintel M, et al: Lung inhomogeneity in patients with acute
respiratory distress syndrome. Am J Respir Crit Care Med.
189:149–158. 2014.PubMed/NCBI
|
|
16
|
Caironi P, Tognoni G, Masson S, Fumagalli
R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli
G, et al: ALBIOS Study Investigators: Albumin replacement in
patients with severe sepsis or septic shock. N Engl J Med.
370:1412–1421. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Masson S, Caironi P, Fanizza C, Carrer S,
Caricato A, Fassini P, Vago T, Romero M, Tognoni G, Gattinoni L, et
al: Albumin Italian Outcome Sepsis Study Investigators: Sequential
N-terminal pro-B-type natriuretic peptide and high-sensitivity
cardiac troponin measurements during albumin replacement in
patients with severe sepsis or septic shock. Crit Care Med.
44:707–716. 2016.PubMed/NCBI
|
|
18
|
Tokgöz Y, Erdur B and Öztürk Y: HLA
subtypes and Helicobacter pylori infection in an infant with
celiac crisis. Turk J Gastroenterol. 24:74–76. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Horowitz M, Neeman E, Sharon E and
Ben-Eliyahu S: Exploiting the critical perioperative period to
improve long-term cancer outcomes. Nat Rev Clin Oncol. 12:213–226.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ecker BL, Simmons KD, Zaheer S, Poe SL,
Bartlett EK, Drebin JA, Fraker DL, Kelz RR, Roses RE and Karakousis
GC: Blood transfusion in major abdominal surgery for malignant
tumors: A trend analysis using the National Surgical Quality
Improvement Program. JAMA Surg. 151:518–525. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Calfee CS, Delucchi K, Parsons PE,
Thompson BT, Ware LB and Matthay MA: NHLBI ARDS Network:
Subphenotypes in acute respiratory distress syndrome: Latent class
analysis of data from two randomised controlled trials. Lancet
Respir Med. 2:611–620. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schmidt M, Stewart C, Bailey M,
Nieszkowska A, Kelly J, Murphy L, Pilcher D, Cooper DJ,
Scheinkestel C, Pellegrino V, et al: Mechanical ventilation
management during extracorporeal membrane oxygenation for acute
respiratory distress syndrome: A retrospective international
multicenter study. Crit Care Med. 43:654–664. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang Z, Wei Y, Tejera P, Su L, Bajwa EK
and Christiani DC: A functional missense SNP in LRRC16A contributes
to an improved prognosis of ARDS patients mediated through
attenuated platelet count decline in ICU. Am J Respir Crit Care
Med. 193:A74892016.
|
|
24
|
Hendrickson CM and Matthay MA: Endothelial
biomarkers in human sepsis: Pathogenesis and prognosis for ARDS.
Pulm Circ. 8:20458940187698762018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Qi SY, Wang WT, Chu ZD, Chen CY, Zhou MK,
Ren YX and Liu XJ: The clinical analysis of extracorporeal membrane
oxygenation for adult severe acute respiratory distress syndrome.
Zhonghua Jie He He Hu Xi Za Zhi. 39:291–297. 2016.(In Chinese).
PubMed/NCBI
|
|
26
|
Zhu Q, Pan X, Cao Y, Wang H, Yu N, Liu F,
Yang S, Wang Y, Sun Y and Wang Z: Clinical evaluation of continuous
renal replacement therapy in combination with ultrasound-guided
percutaneous transhepatic gallbladder drainage for acute severe
biliary pancreatitis: A retrospective study. Kidney Blood Press
Res. 42:1023–1032. 2017. View Article : Google Scholar : PubMed/NCBI
|