Introduction
According to the statistics of the World Health
Organization in 2012, 4.9 million individuals suffered from
bilateral corneal blindness worldwide, which accounted for ~12% of
all cases of blindness (1–3). It has been well established that
penetrating keratoplasty (PK) may significantly improve
post-surgical visual acuity of patients with corneal blindness;
however, the long-term graft survival rates have been estimated to
be 28–55% over 5 years and 11% at 10 years post-graft implantation
in patients treated with repeated keratoplasty (4–7).
Furthermore, PK has been reported to be associated with poor
post-surgical visual outcomes, as well as surgical complications
and/or failure in high-risk patients, including those suffering
from aniridia, herpetic keratitis, severe chemical burns and
cicatrising diseases (8–11). Therefore, a novel strategy for the
treatment of patients with PK and poor prognoses was required,
which led to the development of the keratoprosthesis (Kpro)
implantation strategy (12).
Boston type 1 Kpro (Kpro-1) is considered to
represent an alternative therapeutic strategy for patients
suffering from late-stage corneal blindness, which is not specified
in standard keratoplasty. Several previous studies have
investigated the symptoms, complications and post-surgical outcomes
associated with Kpro-1 implantation (13–21);
however, the majority of these studies were performed in the USA.
Thus far, there has been limited research regarding the evaluation
of Kpro implantation outside North America. To the best of our
knowledge, only one study investigating the clinical outcomes
associated with Kpro-1 implantation in Southern China has been
published (22). Therefore, it is
important that symptoms, clinical outcomes and complications
associated with Kpro-1 implantation in patients in Northeast China
are further investigated in future studies.
Materials and methods
Patients
Clinical data of patients with corneal blindness who
had undergone implantation with Kpro-1 between July 2010 and
November 2014 were collected in a retrospective manner. Patients
were qualified for inclusion if they: i) had a history of PK
surgical failure; ii) were not amenable to standard keratoplasty;
iii) had no optic neuropathy or retinal neuropathy; and iv) had a
good eyelid contour with normal eye blink. Cases with autoimmune
diseases, including ocular cicatricial pemphigoid or
Stevens-Johnson syndrome, were excluded from the present study.
Written informed consent was obtained from each patient prior to
surgery. The clinical and personal data of the patients were
recorded, including age, sex, pre-operative diagnoses, symptoms,
prior history of ocular surgeries, ocular and medical comorbidities
and visual outcomes.
Surgical technique
A pre-operative assessment of the complete personal
medical and family ocular history for each patient was performed.
Each patient was subjected to ophthalmological examination to
determine whether they were suitable for keratoplasty. The KPro-1
threadless design was purchased from the Massachusetts Eye and Ear
Infirmary (Boston, MA, USA). Implantation with Kpro-1 was performed
using a standard technique that has been previously described
(23,24). Surgical procedures were performed by
the same experienced surgeon. A contact lens was placed on the
cornea of all patients following KPro implantation. During the
post-operative follow-up period, contact lenses were adjusted,
replaced and cleaned if required.
Patients' bandages were removed a total of 24 h
post-surgery. Topical tropicamide eye drops (twice per day),
levofloxacin eye drops (four times per day), prednisolone eye drops
(four times per day) and tobramycin dexamethasone eye ointment
(once per night) were administered over a 1-month time period.
Following this, the frequency of topical eye drops administered to
patients was reduced by half over a 6-month period. For patients
that exhibited elevated intraocular pressure (IOP) post-surgery,
loteprednol and anti-glaucoma eye drops, e.g. brimonidine tartrate,
were administered twice per day. Following this, patients were
subjected to systemic administration of numerous drugs for 6
months, including oral administration of minocycline (twice per
day) and a liver-preserving drug as antifungal drugs may result in
liver damage.
Outcome measures
Patients were subjected to follow-up examination at
the following time intervals post-surgery: 3 days, 1 month, 6
months and every 1 to 3 months thereafter. At each follow-up
examination, slit-lamp examination was performed, the logarithm of
the minimum angle of resolution (LogMAR), IOP, optic disc and
fundus were evaluated, and any possible complications were screened
for. The post-operative characteristics were subsequently observed,
including best spectacle-corrected visual acuity, device retention
and post-operative medications. The incidence of post-operative
complications, the timing of such complications and therapeutic
regimens administered were also recorded.
Statistical analysis
Quantitative data are expressed as the mean ±
standard deviation and differences between groups were analyzed
using one-way analysis of variance followed by Tukey's post-hoc
test. Data analysis was performed using SPSS 19.0 software (IBM
Corp., Armonk, NY, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline characteristics
A total of 20 patients were included in the present
study (14 males and 6 females; mean age, 47.15±14.79 years; age
range, 21–79 years). Of these patients, 17 cases had a history of
failed PK, one had experienced three failed PK surgeries and only
two patients had no history of failed PK. All patients were
followed up at 3 days, 1 month, 6 months, 1 year and 2 years
post-surgery. Details on the patients who received a KPro-1 implant
are presented in Table I.
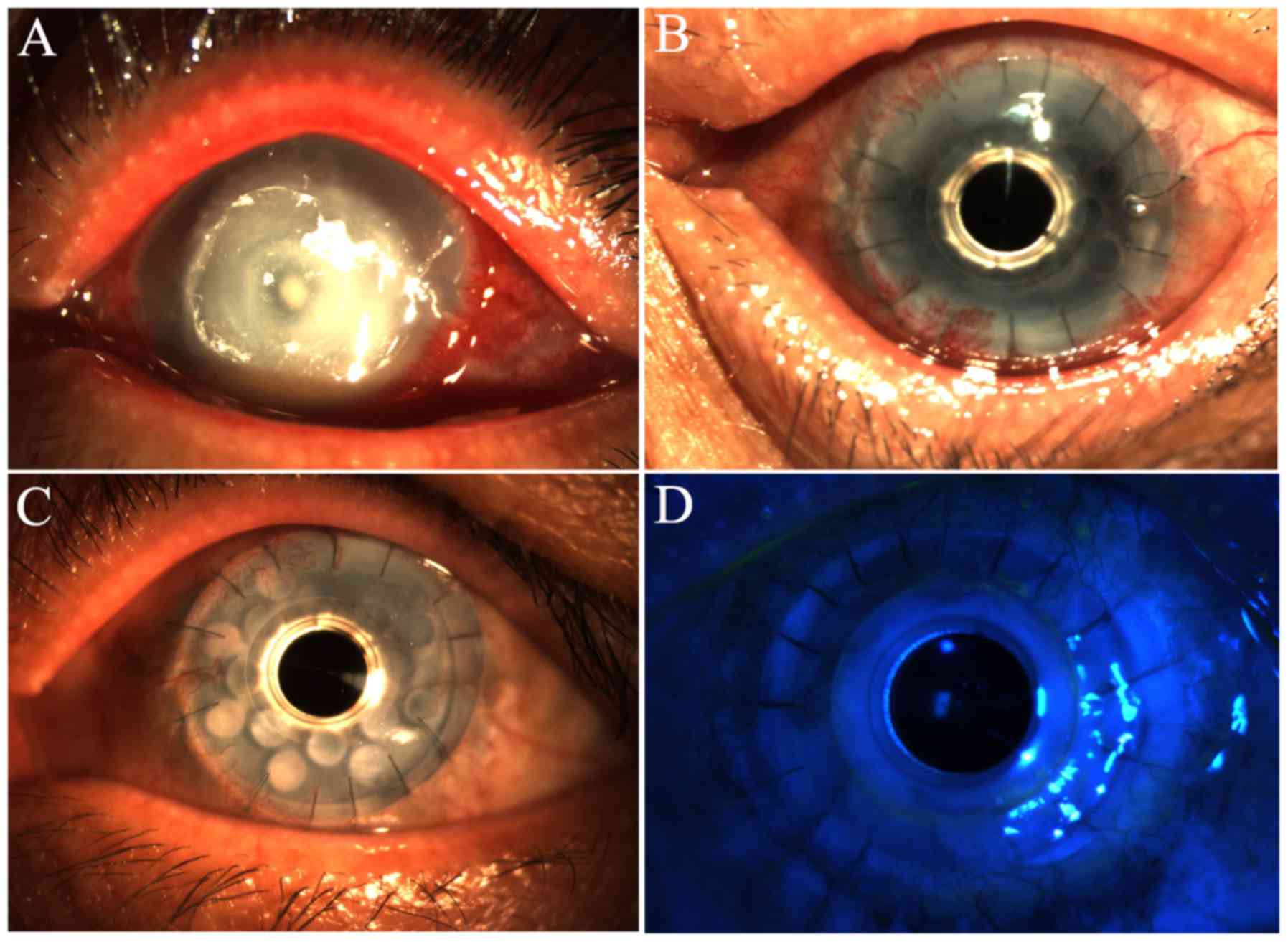
Representative mages of the patients' corneas prior to and
post-implantation with Kpro-1 are presented in Fig. 1.
 | Table I.Details of patients implanted with a
KPro-1. |
Table I.
Details of patients implanted with a
KPro-1.
| Age (years)/sex | Ocular diagnosis | Number of previous
failed PK | Technique |
|---|
| 49/F | Mycotic corneal
ulcer | 1 | KPro-1 + iridectomy +
AV |
| 36/M | Leukoma | 1 | KPro-1 + ECCE |
| 23/M | Mycotic corneal
ulcer | 1 | KPro-1 + cataract
removal + ILI |
| 21/M | Alkali burn | 1 | KPro-1 + AV |
| 49/M | Mycotic corneal
ulcer | 1 | KPro-1 + AV |
| 27/M | Bacterial corneal
ulcer | 1 | KPro-1 |
| 40/M | Acid burn | 3 | KPro-1 |
| 79/F | Herpes simplex
corneal ulcer | 1 | KPro-1 + AV |
| 54/M | Leukoma +
glaucoma | 1 | KPro-1 + CT +
cyclocryotherapy |
| 37/M | Mycotic corneal
ulcer | 1 | KPro-1 |
| 42/M | Mycotic corneal
ulcer | 1 | KPro-1 + ECCE +
ILI |
| 51/M | Leukoma |
| KPro-1 + ECCE |
| 53/F | Mycotic corneal
ulcer | 1 | KPro-1 + ECCE |
| 45/M | Mycotic corneal ulcer
+ Mooren's ulcer | 1 | KPro-1 ×2 |
| 56/F | Mycotic corneal
ulcer | 1 | KPro-1 |
| 55/M | Leukoma | 1 | KPro-1+ AV |
| 61/F | Glaucoma + CED |
| KPro-1 + AV |
| 65/F | Leukoma +
glaucoma | 1 | KPro-1 + iridectomy +
AV |
| 64/M | Alkali burn | 1 | KPro-1 + AV |
| 36/M | Viral corneal
ulcer | 1 | KPro-1 + cataract
removal + ILI |
Visual acuity
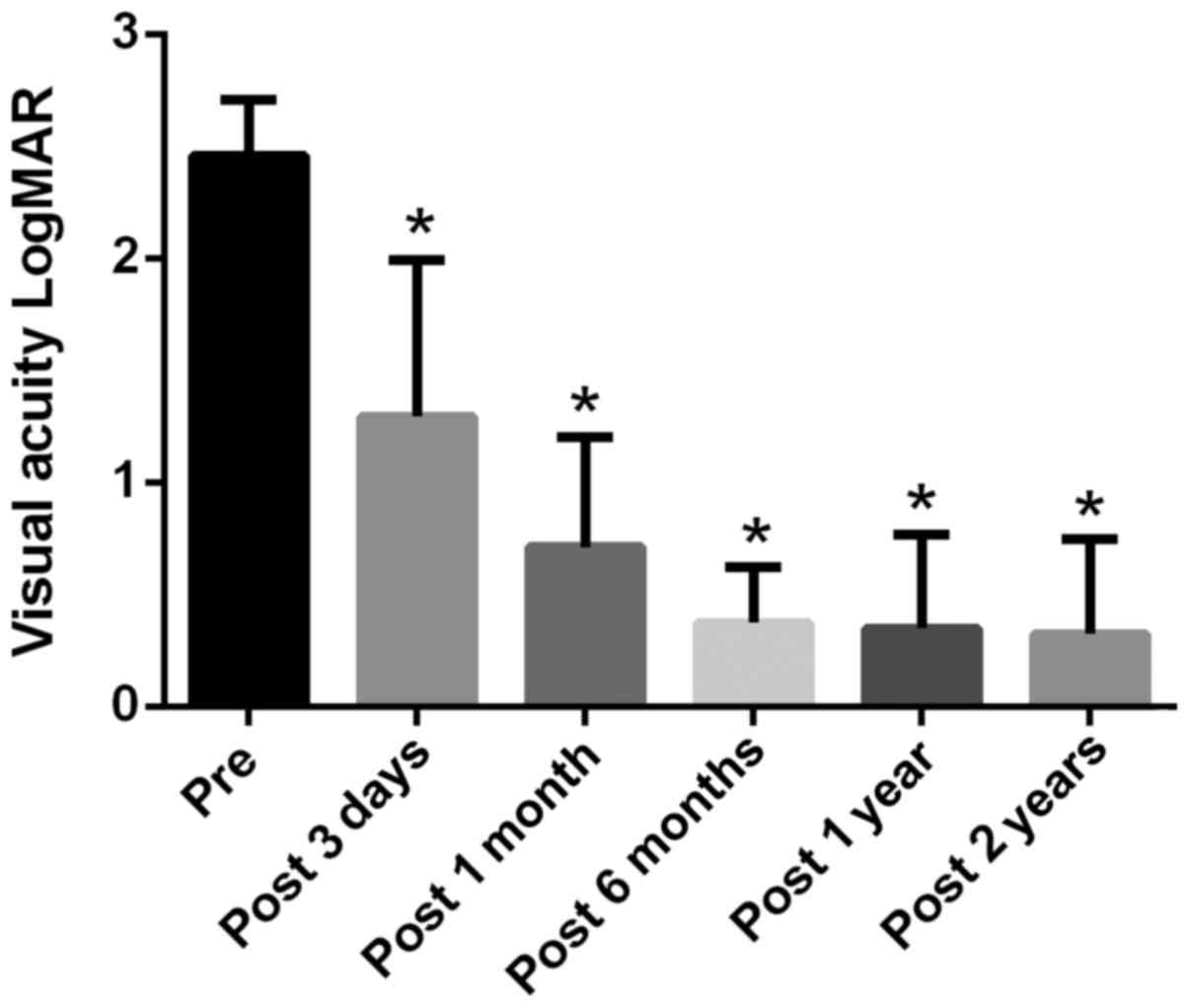
Patients exhibited poor vision and decreased levels
of light perception prior to surgery. Following Kpro-1
implantation, visual improvement was observed in all 20 eyes
(100%). The LogMAR values obtained at 3 days, 1 month, 6 month, 1
year and 2 year post-surgery were significantly decreased compared
with the pre-operative values (P<0.05; Fig. 2).
Prosthesis retention
The mean follow-up period was 2.89±1.56 years
post-implantation (range, 3–5 years). During the follow-up period,
the initial Kpro-1 was retained in 16 eyes (80%). In addition,
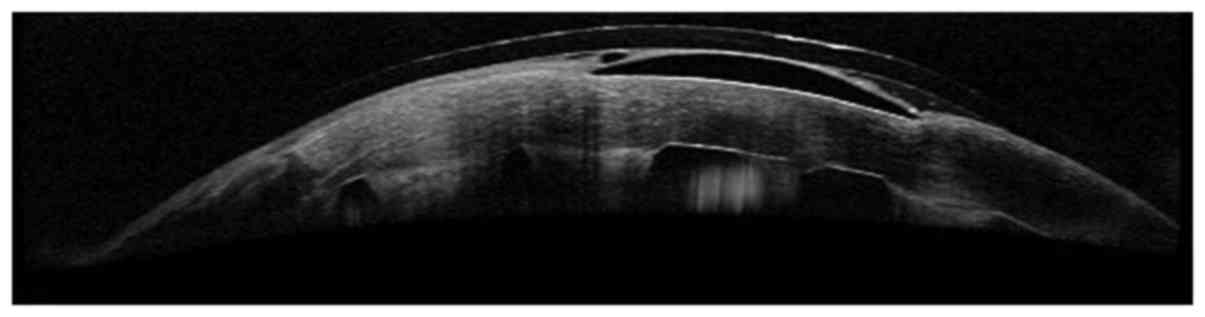
corneal images (Fig. 1) and
swept-source optical coherence tomography imaging (Fig. 3) revealed that the artificial and
donor corneas in 14 patients were completely healed 1 year
following Kpro-1 implantation.
Complications and management
Post-operative complications exhibited by patients
are listed in Table II. A total of
seven patients (35%) experienced one or more post-operative
complications. A total of six patients developed retroprosthetic
membrane formation (RPM) and mild-to-moderate visual loss. In these
six patients, five eyes affected were treated using a
neodymium-doped yttrium aluminum garnet (YAG) laser, and one eye
was treated via surgical membrane removal; all eyes subsequently
exhibited visual improvement. Optical cylinder detachment was
observed in two patients at 1- and 2-year time intervals
post-surgery, and their LogMAR values were slightly decreased to
0.25 and 1.85, respectively. Corneal ulcers occurred in three
patients; however, inflammation was effectively managed and the
visual acuity was improved following administration of active
systemic and local anti-infective treatment. Retinal detachment
occurred in two patients at 1 and 4 years post-operation. The
retina was repositioned in one patient following vitrectomy,
retinal reposition and silicone oil filling; the other patient also
developed secondary endophthalmitis, however, this was subsequently
managed via conservative and surgical treatment. Corneal melting
occurred in two patients: One patient refused to undergo a second
KPro implantation and the other patient received ophthalmectomy due
to additional infective endophthalmitis. In total, endophthalmitis
was observed in two patients. Secondary optic neuropathy occurred
in one patient at a total of 4 years post-surgery; however,
following 3 days of systemic hormone shock therapy combined with
oral hormone sequential therapy, the patient's visual acuity
remained at 0.2. Secondary glaucoma was detected in two patients.
Following the administration of cyclocryotherapy and compound
trabeculectomy to these patients, the IOP of the two eyes returned
to normal.
 | Table II.Post-operative complications. |
Table II.
Post-operative complications.
| Complication | Cases |
|---|
| Retroprosthetic
membrane formation | 6 |
|
Endophthalmitis | 2 |
| Secondary
glaucoma | 2 |
| Optical cylinder
detachment | 2 |
| Corneal
melting | 2 |
| Retinal
detachment | 2 |
| Corneal ulcer | 3 |
| Secondary optic
neuropathy | 1 |
Discussion
PK has provided patients with diseased, opacified or
otherwise compromised corneas with a chance to regain sight.
Although this procedure represents the primary treatment option for
such conditions, graft failure is a huge obstacle for surgical
success. Despite the development of numerous novel drugs and
increasingly advanced surgical techniques, ~40% of patients with PK
have been reported to exhibit immunological rejection following
corneal grafts over a 10-year follow-up period, and in half of
these cases, this results in graft failure (7,8,25,26). The
success rate of secondary corneal graft surgery is markedly lower
(4).
Specific indications for Kpro implantation include
PK surgical failure, chemical burns and severe corneal scarring
vascularization (27,28). To identify patients that may be
suitable for Kpro implantation, surgeons should consider causes of
visual loss, lid position, ocular surface condition, and
concomitant ocular and systemic diseases (29). In addition, Farias et al
(30) demonstrated the successful
use of intraocular videoendoscopic examination in the pre-operative
evaluation of candidates for KPro implantation.
In the present study, the results revealed that the
majority of patients exhibited a significant improvement in
post-operative visual acuity following KPro implantation due to the
removal of retro-KPro membranes and cataracts. Other factors
resulting in poor eyesight following artificial cornea
transplantation included secondary glaucoma with high intraocular
pressure, vitreous opacity and optical cylinder detachment.
The incidence of RPM in the present study was 30%. A
previous study by Stacy et al (31) reported an RPM incidence of 25–65%
following Boston type 1 implantation and ~45% of those cases
affected required further treatment, including YAG laser treatment
or surgical membranectomy. In the present study, two patients
presented with secondary glaucoma after the implantation. The
development and progression of glaucoma in patients with KPro
implants may be due to a compromised angle as a result of a crowded
anterior chamber, routine topical steroid therapy or debris
accumulation in the trabecular meshwork (22). In the present study, endophthalmitis
occurred in two patients, which represents one of the most damaging
and challenging complications associated with KPro surgery
(32). Retinal detachment was
observed in two patients of the present study. Patients with
underlying autoimmune systemic disorders should be closely
monitored for the development of retinal detachment following KPro
surgery (33). In the present study,
corneal melting occurred in two patients (10%), the rate of which
was decreased compared with that reported by Cade et al
(34). A recent study by
Kammerdiener et al (35)
suggested that the absence of lens implantation following KPro
surgery may increase the risk of post-operative complications,
including corneal melting. Therefore, extensive forniceal
reconstruction performed to retain the lens may contribute to
prolonged retention of the implanted KPros in patients with
late-stage corneal blindness.
Of note, the present study had certain limitations.
First, the study lacked a concurrent control group and follow-up
data of 3 months post-surgery. Furthermore, all procedures in the
present study were performed by a single surgeon. Therefore, no
data were available for comparison between different surgical
procedures or different surgeons. In addition, the size of the
study population and the quantity of available OCT data were small.
Therefore, future large-scale studies with long-term follow-up
periods are required.
In conclusion, the results of the present study
suggested that Kpro-1 represents an alternative therapeutic
strategy for patients with previously failed keratoplasty in
Northeast China. Serious complications are common, and thus,
suitable patient selection, continuous follow-ups and early
treatment interventions are recommended.
Acknowledgements
Not applicable.
Funding
The present study was partly funded by the China
Postdoctoral Science Fund (grant no. 2015M572800) and the Natural
Science Foundation of Liaoning Province in China (grant no.
20170540978).
Availability of data and materials
The data used to support the results of this study
are available from the corresponding author upon request.
Authors' contributions
MG was a major contributor in the writing of the
manuscript and performed the surgery. YC designed the present study
and performed literature searches. JW analysed and interpreted the
patient data. CW collected and assembled the data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the ethical committee of
the General Hospital of Shenyang Military Area Command (approval
no. 2010L05; Shenyang, China).
Patient consent for publication
Written informed consent was obtained from all
patients prior to surgery, including for the use of personal
information for research purposes.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Oliva MS, Schottman T and Gulati M:
Turning the tide of corneal blindness. Indian J Ophthalmol.
60:423–427. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pascolini D and Mariotti SP: Global
estimates of visual impairment: 2010. Br J Ophthalmol. 96:614–618.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Resnikoff S, Pascolini D, Etya'ale D,
Kocur I, Pararajasegaram R, Pokharel GP and Mariotti SP: Global
data on visual impairment in the year 2002. Bull World Health
Organ. 82:844–851. 2004.PubMed/NCBI
|
|
4
|
Beckingsale P, Mavrikakis I, Al-Yousuf N,
Mavrikakis E and Daya SM: Penetrating keratoplasty: Outcomes from a
corneal unit compared to national data. Br J Ophthalmol.
90:728–731. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bersudsky V, Blum-Hareuveni T, Rehany U
and Rumelt S: The profile of repeated corneal transplantation.
Ophthalmology. 108:461–469. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ma JJ, Graney JM and Dohlman CH: Repeat
penetrating keratoplasty versus the Boston keratoprosthesis in
graft failure. Int Ophthalmol Clin. 45:49–59. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muraine M, Sanchez C, Watt L, Retout A and
Brasseur G: Long-term results of penetrating keratoplasty. A
10-year-plus retrospective study. Graefes Arch Clin Exp Ophthalmol.
241:571–576. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ing JJ, Ing HH, Nelson LR, Hodge DO and
Bourne WM: Ten-year postoperative results of penetrating
keratoplasty. Ophthalmology. 105:1855–1865. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kremer I, Rajpal RK, Rapuano CJ, Cohen EJ
and Laibson PR: Results of penetrating keratoplasty in aniridia. Am
J Ophthalmol. 115:317–320. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tugal-Tutkun I, Akova YA and Foster CS:
Penetrating keratoplasty in cicatrizing conjunctival diseases.
Ophthalmology. 102:576–585. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yaghouti F, Nouri M, Abad JC, Power WJ,
Doane MG and Dohlman CH: Keratoprosthesis: Preoperative prognostic
categories. Cornea. 20:19–23. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Barber JC: Keratoprosthesis: Past and
present. Int Ophthalmol Clin. 28:103–109. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aldave AJ, Sangwan VS, Basu S, Basak SK,
Hovakimyan A, Gevorgyan O, Kharashi SA, Jindan MA, Tandon R,
Mascarenhas J, et al: International results with the Boston type I
keratoprosthesis. Ophthalmology. 119:1530–1538. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chew HF, Ayres BD, Hammersmith KM, Rapuano
CJ, Laibson PR, Myers JS, Jin YP and Cohen EJ: Boston
keratoprosthesis outcomes and complications. Cornea. 28:989–996.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ciolino JB, Belin MW, Todani A, Al-Arfaj K
and Rudnisky CJ; Boston Keratoprosthesis Type 1 Study Group, :
Retention of the Boston keratoprosthesis type 1: Multicenter study
results. Ophthalmology. 120:1195–1200. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dunlap K, Chak G, Aquavella JV, Myrowitz
E, Utine CA and Akpek E: Short-term visual outcomes of Boston type
1 keratoprosthesis implantation. Ophthalmology. 117:687–692. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Greiner MA, Li JY and Mannis MJ:
Longer-term vision outcomes and complications with the Boston type
1 keratoprosthesis at the University of California, Davis.
Ophthalmology. 118:1543–1550. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kamyar R, Weizer JS, de Paula FH, Stein
JD, Moroi SE, John D, Musch DC and Mian SI: Glaucoma associated
with Boston type I keratoprosthesis. Cornea. 31:134–139. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Patel AP, Wu EI, Ritterband DC and Seedor
JA: Boston type 1 keratoprosthesis: The New York Eye and Ear
experience. Eye (Lond). 26:418–425. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Robert MC and Harissi-Dagher M: Boston
type 1 keratoprosthesis: The CHUM experience. Can J Ophthalmol.
46:164–168. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zerbe BL, Belin MW and Ciolino JB; Boston
Type 1 Keratoprosthesis Study Group, : Results from the multicenter
Boston Type 1 Keratoprosthesis Study. Ophthalmology. 113(1779):
e1–7. 2006.
|
|
22
|
Gu J, Zhai J, Zhou S and Chen J: Boston
keratoprosthesis outcomes in severe ocular chemical burns in
Southern China: A retrospective study. Adv Ther. 33:760–773. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dohlman CH, et al: Introduction to the use
of the Boston keratoprosthesis. Expert Rev Ophthalmology. 1:41–48.
2006. View Article : Google Scholar
|
|
24
|
Aquavella JV, Qian Y, McCormick GJ and
Palakuru JR: Keratoprosthesis: The Dohlman-Doane device. Am J
Ophthalmol. 140:1032–1038. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sellami D, Abid S, Bouaouaja G, Ben Amor
S, Kammoun B, Masmoudi M, Dabbeche K, Boumoud H, Ben Zina Z and
Feki J: Epidemiology and risk factors for corneal graft rejection.
Transplant Proc. 39:2609–2611. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Price FW and Price MO: Adult keratoplasty:
Has the prognosis improved in the last 25 years? Int Ophthalmol.
28:141–146. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
De La Paz MF, De Toledo JÁ, Charoenrook V,
Sel S, Temprano J, Barraquer RI and Michael R: Impact of clinical
factors on the long-term functional and anatomic outcomes of
osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis. Am
J Ophthalmol. 151(829–839): e12011.
|
|
28
|
Muñoz-Gutierrez G, de Toledo Alvarez J,
Barraquer RI, Vera L, Valeria Couto R, Nadal J and de la Paz MF:
Post-surgical visual outcome and complications in Boston type 1
keratoprosthesis. Arch Soc Esp Oftalmol. 88:56–63. 2013.(In
English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Williamson SL and Cortina MS: Boston type
1 keratoprosthesis from patient selection through postoperative
management: A review for the keratoprosthetic surgeon. Clin
Ophthalmol. 10:437–443. 2016.PubMed/NCBI
|
|
30
|
Farias CC, Ozturk HE, Albini TA, Berrocal
AM, Amescua G, Betancurt C, Parel JM, Oliveros MC, Gibbons A,
Vargas JM and Perez VL: Use of intraocular video endoscopic
examination in the preoperative evaluation of keratoprosthesis
surgery to assess visual potential. Am J Ophthalmol. 158(80–86):
e22014.
|
|
31
|
Stacy RC, Jakobiec FA, Michaud NA, Dohlman
CH and Colby KA: Characterization of retrokeratoprosthetic
membranes in the Boston type 1 keratoprosthesis. Arch Ophthalmol.
129:310–316. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Robert MC, Moussally K and Harissi-Dagher
M: Review of endophthalmitis following Boston keratoprosthesis type
1. Br J Ophthalmol. 96:776–780. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jardeleza MS, Rheaume MA, Chodosh J, Lane
AM and Dohlman CH: Retinal detachments after Boston
Keratoprosthesis: Incidence, predisposing factors, and visual
outcomes. Digit J Ophthalmol. 21:1–15. 2015.PubMed/NCBI
|
|
34
|
Cade F, Grosskreutz CL, Tauber A and
Dohlman CH: Glaucoma in eyes with severe chemical burn, before and
after keratoprosthesis. Cornea. 30:1322–1327. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kammerdiener LL, Speiser JL, Aquavella JV,
Harissi-Dagher M, Dohlman CH, Chodosh J and Ciolino JB: Protective
effect of soft contact lenses after boston keratoprosthesis. Br J
Ophthalmol. 100:549–552. 2016. View Article : Google Scholar : PubMed/NCBI
|