Introduction
Idiopathic orbital inflammation (IOI) is a type of
cryptogenic, non-infectious, inflammatory infiltrating orbital
disease that can involve any tissue in the orbit (1). The diagnosis of IOI requires the
exclusion of tumors, infections and systemic inflammatory diseases.
Due to the large number of non-specific inflammatory diseases and
how complex the diseases are (2),
the clinical diagnosis and the pathological diagnosis require
further regulation. Different types of inflammatory pseudotumors
vary greatly, and each has a different response to treatment
(3). Notably, orbital inflammatory
pseudotumor is a chronic non-specific inflammatory proliferative
disease that originates in the eyelids (4). Clinically, it has been demonstrated
that the clinical manifestations of inflammatory pseudotumors are
diverse and may be similar to various other diseases, including
lymphoma or systemic connective tissue inflammation (5). Its diagnosis and treatment
difficulties, etiology and pathogenesis are unknown, and it is a
challenge for ophthalmologists (4).
At present, the majority of studies have identified
that non-specific eyelid inflammation is associated with systemic
immune diseases, including IgG4-related systemic diseases (6). Immunoglobulin G4-related orbital
disease (IgG4-ROD) is an autoimmune disease characterized by
infiltration of IgG4+ plasma cells accompanied by tissue
fibrosis of multiple organs throughout the body and swelling or
tumor-like, nodular or proliferative lesions (6).
The timely identification, and correct diagnosis and
proper handling of IgG4-ROD are essential for the diagnosis and
treatment of IOI, in which patients typically experience painless
swelling of both eyes as the first symptom (7). The majority of newly diagnosed patients
are diagnosed with non-specific inflammation, such as lacrimal
gland or orbital inflammatory pseudotumor (8). In the treatment of patients requiring
hormone therapy based on the condition, poor treatment or relapse
of patients through tissue biopsy, a number of IgG4+
plasma cells have been identified to infiltrate tissues, and the
possibility of eyelid IgG4-RODs should be considered.
Materials and methods
Participants
Pathological eyelid specimens were collected from 23
patients with non-specific orbital inflammation in the Department
of Ophthalmology at the Tianjin First Center Hospital (Tianjin,
China) between June 2011 and May 2015. All patients underwent
orbital lesion resection and histopathological examinations 2 weeks
after admission. Patients with lymphocyte and plasmacyte
infiltration of the orbital region as the main pathological
features on their pathological records were included in the study.
A total of 9 patients with IgG4-ROD (6 males and 3 females) and 14
patients without IgG4-ROD (8 males and 6 females) were recruited to
the present study. The mean age of the patients with IgG4-ROD was
53.2±11.8 years and patients without IgG4-ROD was 49.5±9.3 years.
The exclusion criteria of the IgG4-ROD group were as follows:
Patients with lymphoma, a mesenchymal tumor, an epithelial tumor or
a metastatic tumor. The present study was approved by the Ethics
Committee of Tianjin First Center Hospital (Tianjin, China;
approval no. 2016N056KY). All patients provided written informed
consent.
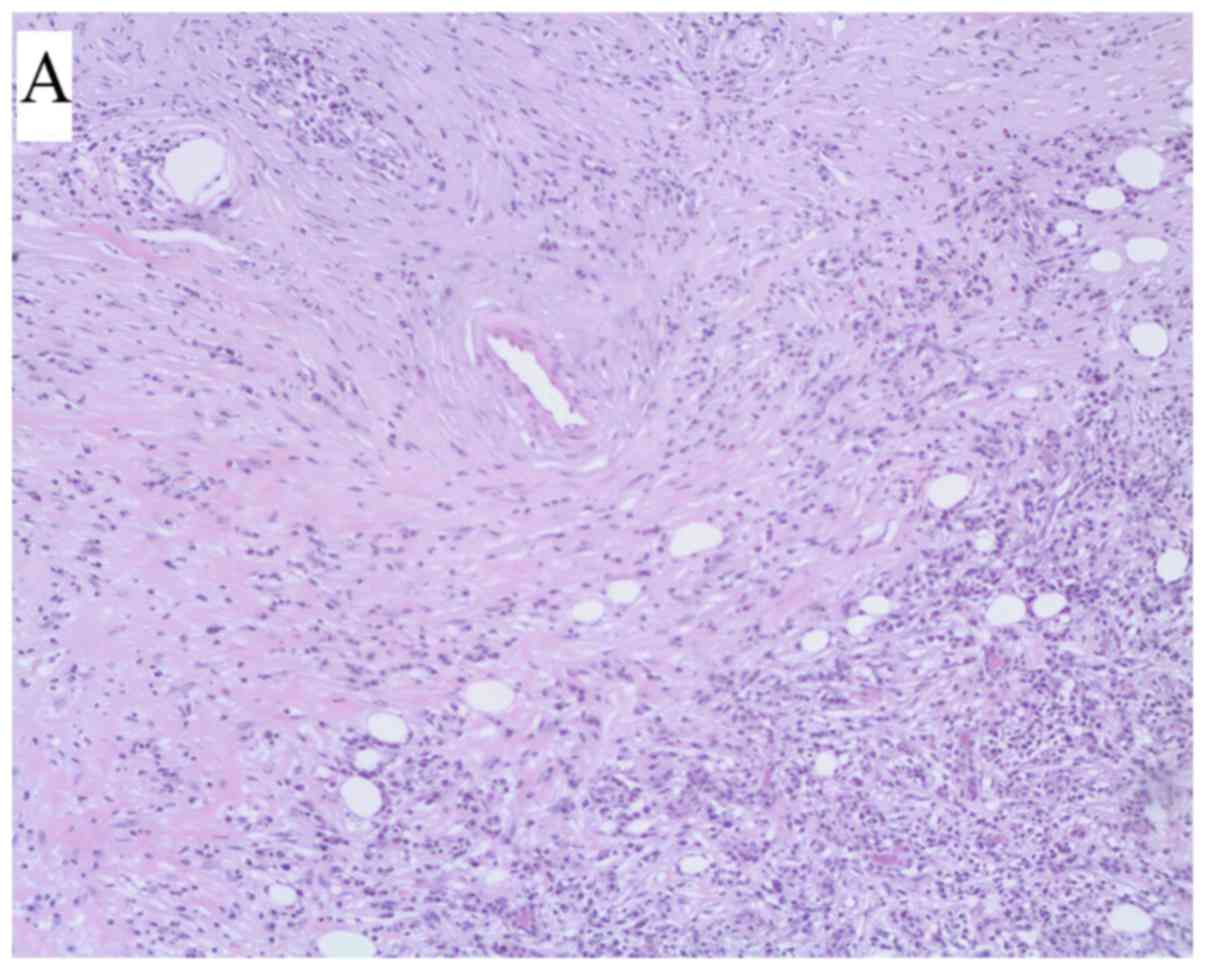
Hematoxylin and eosin (H&E)
staining
Eyelid specimens were sliced into 4-µm-thick
sections. All sections were fixed with 4% formaldehyde solution at
4°C for 24 h and embedded in paraffin. After rinsing with distilled
water for 2 min the sections, the sections were placed in 95%
ethanol for 2 min, hydrated for 5 min and stained with hematoxylin
for 3 min at 40°C. The sections were then wash with water for 30
sec and counterstained with eosin for 60 sec at 50°C. The images
were observed using a fluorescence microscope at a magnification of
×100.
Serological tests
A week after enrollment, the blood from the patients
was centrifuged at 1,000 × g for 7–10 min at 4°C to extract serum.
Serum IgG4 levels were measured by immunoturbidimetry using an
automatic turbidimeter (Behring BN II Nephelometer) and N Latex
IgG4 (both Siemens AG, Munich, Germany) at 10°C for 15 min.
Immunohistochemical staining
Eyelid specimens were sliced into 3–4-µm-thick
sections and fixed with 4% formaldehyde solution at 4°C for 24 h
and embedded in paraffin. The sections were stained with anti-IgG
primary antiobodies from a immunohistochemistry kit (cat. no.
ZA-0448; 1:500; Beijing Zhongshan Jinqiao Biotechnology Co., Ltd.,
Beijing, China) and anti-IgG4 primary antiobodies from a
immunohistochemistry kit (cat. no. IM-0041; 1:500; Shanghai Jie Hao
Biotechnology Co., Ltd., Shanghai, China) at 37°C for 2 h and a
enzyme-labeled sheep anti-mouse/rabbit IgG polymer (cat. no.
PV-6000; 1:1,000; Beijing Zhongshan Jinqiao Biotechnology Co.,
Ltd., Beijing, China) at 37°C for 30 min. IgG and IgG4 were
expressed in the cytoplasm, and were brownish yellow or dark
brownish yellow particles when positively stained. The images were
observed using a light microscope at a magnification of ×400.
Routine visual inspection using a 5-meter
logarithmic vision chart, slit lamp, computer intraocular pressure
measurement, fundus examination, Hertel eyeball out of focus
measurement of the eyeball and nine eye movements was performed 1
week prior to orbital lesion resection (9), in addition to computed tomography (CT)
and magnetic resonance imaging (MRI).
The preoperative CT examination was performed using
a Toshiba Aquilion 16-slice spiral CT scanner (Toshiba Corporation,
Tokyo, Japan) with axial and coronal scanning. The patients
undergoing axial scanning were in a supine position, the
radiographic base line was perpendicular to the table and the
spiral scans were conducted from the upper to the lower edge of the
eyelid. The patients undergoing coronal scanning were in the prone
position, the hearing line is parallel to the table, and the spiral
scans were conducted from the front edge of the orbital crest to
the posterior edge of the optic canal.
The MRI examination was performed using the Siemens
ESSENZA 1.5T superconducting MRI scanner (Siemens AG, Munich,
Germany). The scanning method was as follows: The conventional
sequence of the scanning method consisted of the sagittal (T1WI,
T2WI) and coronal (T: WI + pressure fat) plain scans.
Follow-up
A total of 19 patients were followed-up 6 months
after enrollment; 9 patients with IgG4-ROD and 10 patients without
IgG4-ROD.
Statistical analysis
SPSS 19.0 statistical software (IBM Corp., Armonk,
NY, USA) was used for statistical analysis. The χ2 test was used to
compare data for males and females. The difference in the age of
onset between the two groups was compared using the two-sample
t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinical features and laboratory
tests
No significant difference in the age at onset
(P=0.26) or sex (P=0.53) was identified between the two groups.
Serological tests were performed. Notably, the serum IgG4 titer in
9 patients ranged from 4.58 to 46.70 g/l (reference value,
0.03–1.35 g/l) (10), with an mean
value of 21.93±2.18 g/l. Notably, the degree of increase was
different regarding serological IgG4, but all were >1.35 g/l
(Table I). These findings suggested
that increased serological IgG4 levels were elevated (>1.35
g/l), which is an important serological feature to consider in
IgG4-ROD. In IgG+ plasma cells, the absolute value was
≤50 and the HPF-IgG4/IgG+ plasma cell ratio was >40%
(Fig. 1A-C).
 | Table I.Serum IgG4 levels in all patients 1
week after recruitment. |
Table I.
Serum IgG4 levels in all patients 1
week after recruitment.
| Variable | IgG4 (g/l) |
|---|
| Patients with
IgG4-ROD |
|
| Case
1 | 12.40 |
| Case
2 | 15.19 |
| Case
3 | 42.75 |
| Case
4 | 5.72 |
| Case
5 | 20.41 |
| Case
6 | 39.05 |
| Case
7 | 4.58 |
| Case
8 | 46.70 |
| Case
9 | 10.53 |
| Mean ±
standard deviation | 21.93±2.18 |
| Patients without
IgG4-ROD |
|
| Case
10 | 0.21 |
| Case
11 | 0.37 |
| Case
12 | 0.65 |
| Case
13 | 0.05 |
| Case
14 | 0.92 |
| Case
15 | 0.07 |
| Case
16 | 0.12 |
| Case
17 | 0.14 |
| Case
18 | 0.42 |
| Case
19 | 1.08 |
| Case
20 | 0.97 |
| Case
21 | 0.03 |
| Case
22 | 0.74 |
| Case
23 | 0.38 |
| Mean ±
standard deviation | 0.43±0.19 |
Eye performance
A total of 16 patients out of 23 exhibited no
significant vision loss. The ocular manifestations of patients with
IgG4-ROD were primarily eyelid swelling (9 cases), ocular
protrusion (4 cases) and limited eyeball movement (3 cases). The
ocular manifestations of patients with non-IgG4-ROD were primarily
eyelid swelling (8 cases), ocular protrusion (7 cases), limited eye
movement (6 cases; Table II).
 | Table II.Symptom distribution in the IgG4-ROD
and non-IgG4-ROD group assessed 1 week after recruitment. |
Table II.
Symptom distribution in the IgG4-ROD
and non-IgG4-ROD group assessed 1 week after recruitment.
| Ocular symptoms | Number of cases | IgG4-ROD group
(n=9) | Non-IgG4-ROD group
(n=14) |
|---|
| Eyelid swelling | 17 | 9 (100.0) | 8 (57.1) |
| Exophthalmia | 11 | 4 (44.4) | 7 (50.0) |
| Eye pain | 5 | 2 (22.2) | 3 (21.4) |
| Vision loss | 7 | 3 (33.3) | 4 (28.6) |
| Eye itching | 1 | 0 (0.0) | 1 (7.1) |
| Tears | 3 | 1 (11.1) | 2 (14.3) |
| Eye congestion | 1 | 0 (0.0) | 1 (7.1) |
| Diplopia | 1 | 1 (11.1) | 0 (0.0) |
| Eye movement
restriction | 11 | 3 (33.3) | 6 (42.9) |
Imaging findings
CT and MRI scans from patients with IgG4-ROD
revealed orbital tissue involvement and clear invasion of the
lesion into the lacrimal gland tissue. A total of 9 out of 5 cases
involved the lacrimal gland tissue, mostly predominantly with
bilateral lacrimal gland diffuse symmetry. CT examinations
indicated medium density changes, unclear boundaries, uniform
density, no calcification and no destructive changes in the
surrounding bone wall. There were 6 cases of infraorbital nerve
thickening (Fig. 1D), 3 cases of
extraocular muscle thickening and 1 patient with IgG4-ROD had an
orbital tissue lesion extending along the inferior temporal septum
to the left pterygopalatine fossa, with left sacral fissure
widening and involvement of the left maxillary sinus. In 9 cases,
IgG4-ROD CT scans indicated that the lesions were of moderate
density and that there was no destructive change in the peripheral
bone wall, suggesting that the disease was a less aggressive
lesion. Of these cases, 3 had signs of limited eye movements. The
examinations revealed that the corresponding extraocular muscles
were invaded to different degrees, indicating that the functions of
the extraocular muscles were affected when the extraocular muscles
were affected.
Relevant examination of the patient's eye prior to
and following sectioning demonstrated that the disease had little
effect on vision. Furthermore, poor vision correction was primarily
due to the opacity of the lens or fundus lesions.
Therapeutic effect
Of the 9 cases of IgG4-ROD, 7 had follow-up data, of
which 5 were treated with glucocorticoids, which lead to symptoms
being relieved and controlled, with only 1 patient experiencing
symptom recurrence when glucocorticoids were reduced. Follow-up
data were available for 10 of the 14 patients with non-IgG4-ROD.
Symptoms were controlled in 1 case by treatment with
glucocorticoids. Symptoms improved in 13 cases following
surgery.
Discussion
The most common type of clinical non-specific
orbital inflammation is orbital inflammatory pseudotumor (4). Orbital inflammatory pseudotumor occurs
predominantly in young and middle-aged individuals with more than
one eye (11). No significant
difference regarding sex was observed in the present study.
However, due to the small number of cases observed, it is necessary
to increase the sample size in the future. Typical clinical
manifestations of IgG4-ROD include hyperplasia of the eyelids,
exophthalmos and eye movement (12).
Chronic or severe cases of obstruction, eyelid and conjunctival
congestion, edema, diplopia and vision loss may appear outside of
the eye content protruding from the chalazion (13). In the present study, by clinically
observing eyelid IgG4-ROD, it was revealed that the clinical
imaging examination exhibited a characteristic imaging change of
submental nerve thickening, which may aid in early and correct
diagnosis. In addition to histopathological examination, the
ability to perform an early diagnosis from outside the eye enabled
the standardization of treatment and the avoidance of blind
repeated surgery. According to previously published studies,
infraorbital nerve enlargement, referring to the coronal position,
is a characteristic imaging change of IgG4-ROD when the
infratemporal nerve is thicker than the optic nerve (14). In the present study, the IgG4-ROD
lesion exhibited a high signal in the T1-weighted and T2-weighted
images, but a low signal in MRI, as well as a homogeneous
enhancement in contrast-enhanced MRI with iliac crest. Usually, no
bone destruction was observed. Therefore, the present study aimed
to encourage clinicians to focus on to imaging examinations for
recurrent eyelid circumferences. In patients with lumps or
swelling, by observing and summarizing the clinical and imaging
characteristics of IgG4-ROD a better diagnosis basis and treatment
plan could be selected as soon as possible in order to achieve an
improved prognosis.
Simple inflammatory pseudotumor occurs in multiple
directions, which may cause the extraocular muscles of the eyelid,
lacrimal ducts, hernia sac and meninges to occur around the optic
nerve and adjacent tissues (15). It
has been reported that orbital inflammatory pseudotumor and benign
orbital lymphoid hyperplasia (OBLH) are benign and idiopathic,
accounting for 30–70% of all eyelid biopsies (16,17). In
eyelid disease, the lesion starts in a supercellular lymph plasma
cytoplasm with a morphology that is not like OBLH. Over time,
lesions may gradually harden and are similar to IOI (18,19). If
IgG4 staining is not performed to reveal the diagnosis, the case
may be misdiagnosed as OBLH or IOI (8,20).
IgG4-related diseases have recently been considered
to be autoimmune diseases in almost every organ and tissue in the
body (21–23). A total of 4–13% of patients with
IgG4-related diseases exhibit eyelid involvement, which becomes
IgG4-ROD (24). The majority of
these patients present with enlarged lacrimal glands, prominent
eyeballs, orbital masses and blindness (13). IgG4-ROD involving the extraocular
muscles is primarily associated with lacrimal gland enlargement,
submental neuropathy or periorbital soft tissue lesions (9). In the cases of extraocular muscle
involvement, the majority of the patients experienced unrestricted
eye movement, there was no clear regularity in extraocular muscle
hypertrophy and there was usually multiple muscle involvement
(6,25).
IgG4-ROD can affect a variety of eyelid tissues and
organs (13). Non-specific eyelid
inflammation is a type of eyelid disease reported in fewer studies
than IgG4-ROD, of which the majority are case reports, with only
one large sample multi-center randomized controlled study (26). It is expected that the association
between eyelid diseases and IgG4-related disease will be fully
elucidated, and only through IgG4-related studies is it possible to
identify the specific role of IgG4 in IgG-ROD and its mechanisms in
order to fundamentally improve the diagnosis, treatment effect and
prognosis of these diseases.
In conclusion, the present findings suggest the
clinical feature of IgG4-ROD is bilateral lacrimal gland
enlargement with thickening of the inferior tibial nerve,
extraocular myositis and oppressive optic neuropathy. The disease
is characterized by tumor-like hyperplasia, fibrosis,
IgG4+ plasma cell infiltration and markedly elevated
blood IgG4 levels. The present study demonstrated that submaxillary
nerve enlargement is a characteristic imaging change of IgG4-ROD.
Since IgG4-ROD is a recurrent progressive disease, early diagnosis
and early intervention therapy are of great importance in
preventing the progression of the disease to irreversible
fibrosis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study available from the corresponding author on reasonable
request.
Authors' contributions
NW and FYS participated in the literature search,
study design, writing and critical revision. NW primarily
participated in data collection, data analysis and data
interpretation. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Tianjin First Center Hospital (Tianjin, China;
approval no. 2016N056KY). All patients provided written informed
consent.
Patient consent for publication
The patient has provided consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McNab AA and McKelvie P: IgG4-related
ophthalmic disease. Part I: Background and pathology. Ophthal Plast
Reconstr Surg. 31:83–88. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Patnana M, Sevrukov AB, Elsayes KM,
Viswanathan C, Lubner M and Menias CO: Inflammatory pseudotumor:
The great mimicker. AJR Am J Roentgenol. 198:W217–W227. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sato Y, Ohshima K, Ichimura K, Sato M,
Yamadori I, Tanaka T, Takata K, Morito T, Kondo E and Yoshino T:
Ocular adnexal IgG4-related disease has uniform clinicopathology.
Pathol Int. 58:465–470. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jin R, Zhao P, Ma X, Ma J, Wu Y, Yang X,
Zhang J, Zhong R and Zeng Y: Quantification of Epstein-Barr virus
DNA in patients with idiopathic orbital inflammatory pseudotumor.
PLoS One. 8:e508122013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mombaerts I, Goldschmeding R, Schlingemann
RO and Koornneef L: What is orbital pseudotumor? Surv Ophthalmol.
41:66–78. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Umehara H, Okazaki K, Masaki Y, Kawano M,
Yamamoto M, Saeki T, Matsui S, Sumida T, Mimori T, Tanaka Y, et al:
A novel clinical entity, IgG4-related disease (IgG4RD): General
concept and details. Mod Rheumatol. 22:1–14. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wallace ZS, Khosroshahi A, Jakobiec FA,
Deshpande V, Hatton MP, Ritter J, Ferry JA and Stone JH:
IgG4-related systemic disease as a cause of ‘idiopathic’ orbital
inflammation, including orbital myositis, and trigeminal nerve
involvement. Surv Ophthalmol. 7:26–33. 2012. View Article : Google Scholar
|
|
8
|
Andrew N, Kearney D and Selva D:
IgG4-related orbital disease: A meta-analysis and review. Acta
Ophthalmoi. 9l:694–700. 2013. View Article : Google Scholar
|
|
9
|
Higashiyama T, Nishida Y, Ugi S, Ishida M,
Nishio Y and Ohji M: A case of extraocular muscle swelling due to
IgG4·related sclerosing disease. Jpn J Ophthalmol. 55:315–317.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Takahashi Y, Kitamura A and Kakizaki H:
Bilateral optic nerve involvement in immunoglobulin G4-related
ophthalmic disease. J Neuroophthalmol. 34:16–19. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Umehara H, Okazaki K, Masaki Y, Kawano M,
Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S, et
al: Comprehensive diagnostic criteria for IgG4-related disease
(IgG4-RD), 2011. Mod Rheumatol. 22:21–30. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Paulus YM, Cockerham KP, Coekerham GC and
Gratzinger D: IgG4-positive sclerosing orbital inflammation
involving the conjunctiva: A case report. Ocul Immunol Inflamm.
20:375–377. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morel N, Rigolet A, Schleinitz N, Garnier
A and Costedoat-Chalumeau N: Bilateral enlargement of the lacrimal
glands from IgG4-related systemic disease. Ann Intern Med.
156:669–670. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ohshima K, Sogabe Y and Sato Y: The
usefulness of infraorbital nerve enlargement on MRI imaging in
clinical diagnosis of IgG4-related orbital disease. Jpn J
Ophthalmol. 56:380–382. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Strehl JD, Hartmann A and Agaimy A:
Numerous IgG4-positive plasma cells are ubiquitous in diverse
localised non-specific chronic inflammatory conditions and need to
be distinguished from IgG4-related systemic disorders. J Clin
Pathol. 64:237–243. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
von Holstein SL, Therkildsen MH, Prause
JU, Stenman G, Siersma VD and Heegaard S: Lacrimal gland lesions in
Denmark between 1974 and 2007. Acta Ophthalmol. 91:349–354. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shields CL, Shields JA, Eagle RC and
Rathmell JP: Clinicopathologic review of 142 cases of lacrimal
gland lesions. Ophthalmology. 96:431–435. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jakobiec FA: Ocular adnexal lymphoid
tumors: Progress in need of clarification. Am J Ophthalmol.
145:941–950. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cheuk W, Yuen HK and Chan JK: Chronic
sclerosing dacryoadenitis: Part of the spectrum of IgG4-related
Sclerosing disease? Am J Surg Pathol. 31:643–645. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Andrew N, Sladden N, Kearney D, Crompton J
and Selva D: Sequential biopsies from immunoglobulin G4-related
orbital disease demonstrate progressive fibrosis. Clin Experiment
Ophthalmol. 42:789–791. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Frulloni L and Lunardi C: Serum IgG4 in
autoimmune pancreatitis: A marker of disease severity and
recurrence? Dig Liver Dis. 43:674–675. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Carruthers MN, Khosroshahi A, Augustin T,
Deshpande V and Stone JH: The diagnostic utility of serum IgG4
concentrations in IgG4-related disease. Ann Rheum Dis. 74:14–18.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dua P, Shinder R, Laskar DB, Lazzaro DR
and Rizzuti AE: A case of hypertrophic herpes simplex virus
affecting the eyelid and cornea masquerading as IgG4-related
disease. Am J Ophthalmol Case Rep. 9:68–71. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mulay K, Aggarwal E, Jariwala M and
Honavar SG: Orbital immunoglobulin-G4-related disease: Case series
and literature review. Clin Exp Ophthalmol. 42:682–687. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wallace ZS, Deshpande V and Stone JH:
Ophthalmic manifestations of IgG4-related disease: Single-center
experience and literature review. Semin Arthritis Rheum.
43:806–817. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kubota T and Mofitani S: Orbital
IgG4-related disease: Clinical features and diagnosis. ISRN
Rheumatol. 2012:4128962012. View Article : Google Scholar : PubMed/NCBI
|