Introduction
Bouveret's syndrome is defined as gastric outlet
obstruction (GOO) caused by the duodenal impaction of a gallstone
after entering the small bowel through a fistulous tract (1,2). Léon
Bouveret initially described this syndrome in 1896, wherein two
cases of gastric outlet obstruction due to gall stones were
reported (3). As the symptoms are
frequently non-specific and initial presentations are often benign,
cases of Bouveret's syndrome are at risk of being undiagnosed
(4–6). The aim of the present case report,
accompanied by a brief overview of current diagnostic and
therapeutic modalities, is to enhance awareness of this overlooked
clinical entity in order to ensure timely diagnoses and treatments
for future patients. This enhanced awareness is also essential for
improving the prognosis of this syndrome.
Case report
In the present study, the patient was a 59-year-old
male with a medical history of gallbladder stones and an
unremarkable surgical history, who presented with complaints of
abdominal pain. The pain was described as being located in the
mid-upper quadrant of the abdomen and as severe, constant and
non-radiating. The pain for the preceding 5 days had also been
associated with nausea and non-bilious, non-bloody vomiting. The
patient denied any fever, chills, diarrhea, hematemesis, pruritis
or melena. On physical examination, the patient's vital signs were
within the normal limits, and no masses were palpable. Their
abdomen was soft and non-tender. A nasogastric tube was placed, and
it drained >1 l fluid. Routine laboratory tests revealed a white
blood cell count of 18.4×109/l (normal range,
4.0–11.0×109/l), an alkaline phosphatase level of 131
U/l (normal range, 40–120 U/l) and a γ-glutamyl transferase level
of 116 U/l (normal, <37 U/l) (7).
The remaining laboratory test results were unremarkable. The
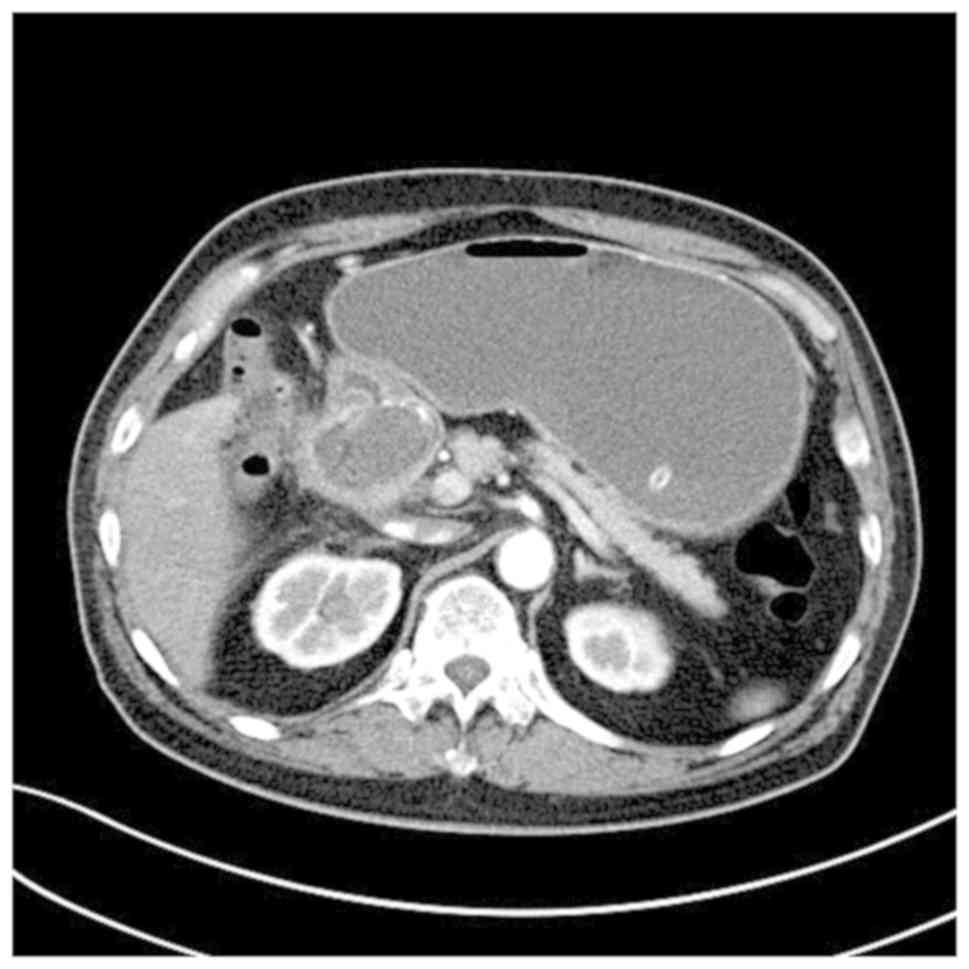
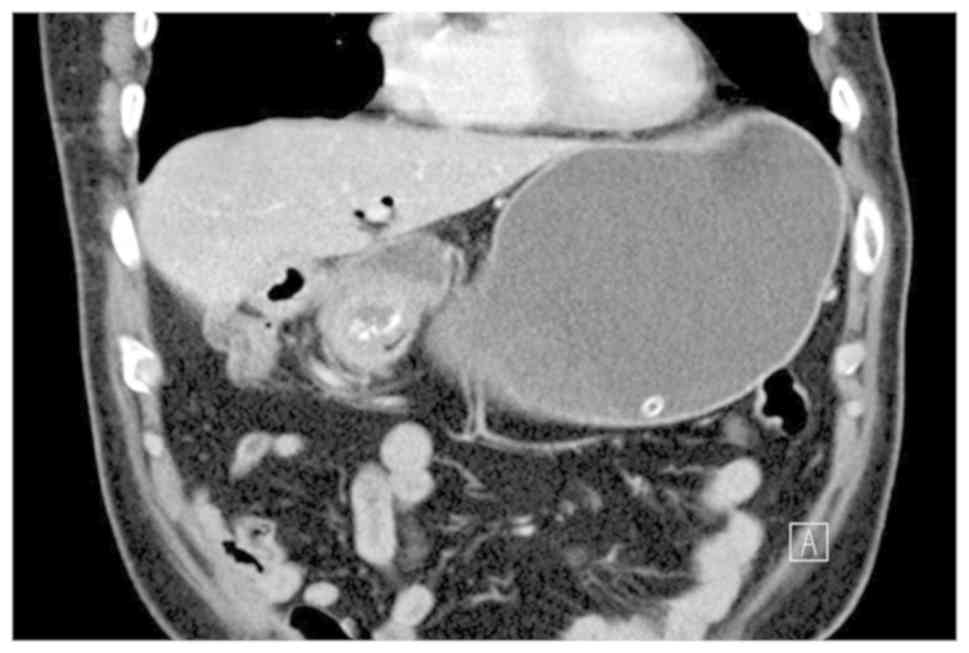
patient underwent a computed tomography (CT) scan, which revealed a
gastric outlet obstruction secondary to an impacted gallstone
within the duodenum, a cholecystoduodenal fistula and a collapased
gallbladder, with thickening of the gallbladder wall and air
present within the gallbladder (Figs.
1 and 2).
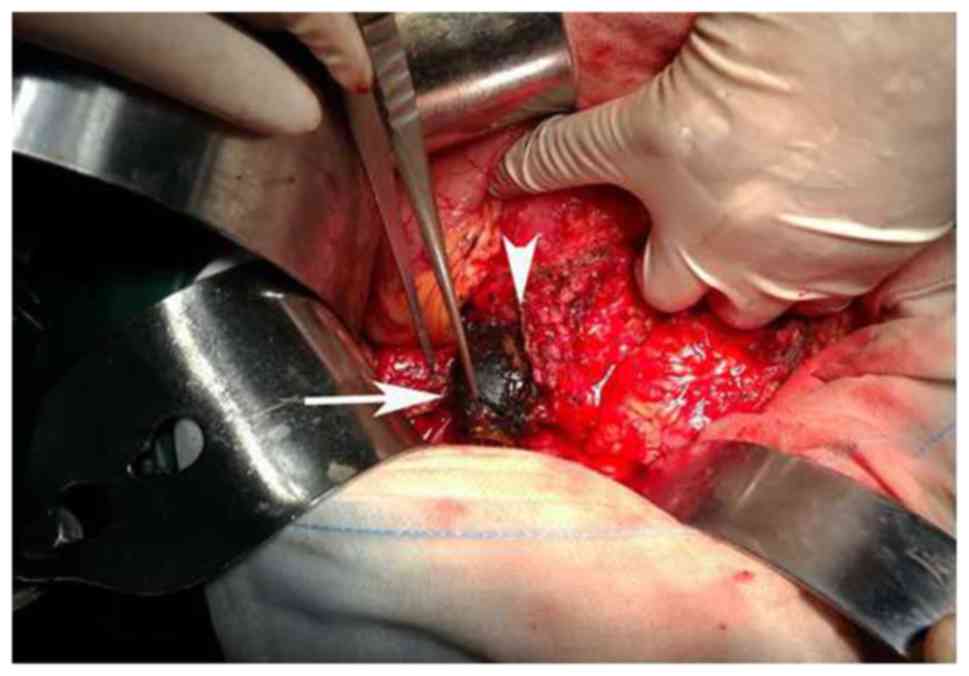
An exploratory laparotomy was planned with a working
diagnosis of GOO. Intraoperatively, it was observed that the stone
was impacted between the first and second part of the duodenum, and
that it could not be milked neither proximally nor distally. Then,
a Kocher incision was performed. The gallbladder was located
tightly adherent to the wall of the duodenum and blunt dissection
exposed the two openings of the fistula between the gallbladder
corpus and the first portion of the duodenum. A formal removal of
the gallbladder was then performed, with simultaneous resection of
the fistula. To aid the removal of the gallstone, a duodenotomy
that elongated the opening in the duodenal wall was performed
(Fig. 3). In order to avoid missing
the possible presence of other stones, the entire gastrointestinal
tract was then palpated. With one layer of interrupted 2–0
monofilament absorbable sutures, the defect in the duodenal wall
was closed and then reinforced with the use of a surgical adhesive
material. Finally, a gastrojejunostomy was carried out. One
duodenostomy tube was placed inside the duodenum. The size of the
extracted stone was 6.0×3.5 cm (Fig.
4). The type of gallstone was not assessed, which was a
limitation of the present report. The pathological results
suggested chronic inflammation of the gallbladder, but the
histopathological features were not assessed, which was a further
limitation of the present report. The patient recovered well
following surgery with no complications and was discharged on the
7th day. The patient is currently on a regular follow up program.
The patient had an uneventful recovery and remains in good health
at the time of writing.
Discussion
Bouveret's syndrome is an uncommon form of
gallstone-ileus caused by large gallstones that reach the duodenal
bulb and get lodged there through a biliodigestive fistula
(5). The gallstone volume may become
enlarged due to an accumulation of fecal matter and salts on its
surface (8). Recurrent inflammation
of the gallbladder frequently causes erosion and necrosis of the
gallbladder wall and allows the formation of biliary-enteric
fistulas (9). The size of the stones
associated with Bouveret's syndrome are typically >2.5 cm, and
it is accepted that larger stones are associated with more proximal
obstruction (10).
Risk factors for Bouveret's syndrome include
gallstones >2.5 cm in size, the female sex and age >70 years
(11). The cluster of symptoms,
including abdominal pain, nausea/vomiting, and dyspepsia, is caused
by gastric outlet obstruction. Abdominal imaging of gallstone ileus
typically reveals Rigler's triad of ectopic gallstone, pneumobilia
and small bowel obstruction (12).
However, only ~33% of gallstone ileus cases exhibit these changes
on conventional radiographs (13).
Due to the gastric outlet obstruction, a dilated stomach is
expected to be observed on plain abdominal radiographs in cases of
Bouveret's syndrome (14). Compared
with other imaging methods, ultrasound (US) is more sensitive with
respect to detecting ectopic gallstones and pneumobilia. The
combination of US and abdominal films has increased the sensitivity
to 74% for the diagnosis of gallstone ileus (15).
The Riglar's triad of findings on CT scans is more
readily apparent. CT scans can also reveal the presence of a
fistula; the degree of bowel obstruction; the degree of
inflammation in the surrounding tissue; and the size, number and
locations of the occluding gallstones. Edema and ischemia of the
affected gastrointestinal tract site can be detected by
contrast-enhanced CT scans (16,17).
Contrast-enhanced CT is of particular importance to making
decisions regarding the management of possible bowel ischemia. To
help provide correct diagnoses and rule out the presence of
intraductal concrements, magnetic resonance
cholangiopancreatography (MRCP) can be used. However, it may be
difficult to differentiate concrements and air using MRCP. MR
imaging is also sensitive for identifying a fistula and can be used
for the confirmation of findings prior to treatment (11,18,19).
Esophagogastroduodenoscopy (EGD) allows the visualization of a
dilated stomach and the impacted stone, which appears as a hard and
non-fleshy mass. It can also reveal the duodenal ostium of the
biliodigestive fistula (10). EGD in
Bouveret's syndrome is important due to it being of both diagnostic
and therapeutic significance.
The primary aim in treating Bouveret's syndrome is
to remove the obstructing gallstone. Both nonsurgical (endoscopic)
and surgical (open or laparoscopic) approaches are therapeutic
options (20). The documented cases
of Bouveret's syndrome being treated successfully with endoscopic
retrieval are few to date. One such literature review reported that
the success rate of endoscopic retrieval alone was only 10%
(21). Although endoscopic
modalities are less invasive and safer for patients with
comorbidities, they carry the risk of serious complications, such
as stone having the lodged in the patient's esophagus and fragments
lodged in the terminal ileum (22).
Therefore, surgery is the main treatment modality for Bouveret's
syndrome, especially when percutaneous or endoscopic approaches are
not first choice or have failed (23).
The therapeutic strategy should take into account
many parameters, including the general condition of the patient,
any comorbidities, age, the inflammatory status of surrounding
tissues, the location of the obstruction, the size of the fistula
and calculus (24), and the number
of gallstones. Whether biliary surgery should be carried out at the
same time as the relief of obstruction of the bowel (one-stage
procedure), performed later (two-stage procedure) or not at all has
been a long-standing controversy in the management of gallstone
ileus (25,26).
Compared with simple enterolithotomy alone, the
one-stage procedure has been associated with higher mortality and
morbidity rates. However, considering the appropriate available
surgical expertise, low-risk patients should be offered the
one-stage definite procedure (27).
In the present case, an open enterolithotomy with
cholecystectomy and fistula repair was performed. Gastrojejunostomy
was also conducted due to the extensive degree of obstruction in
the patient. The noted bulbar ulcer of duodenum may have led to
stricture formation. A pyloric bypass via gastrojejunostomy was
performed in order to spare the patient from future surgery for GOO
(due to a different cause), which would significantly increase
their morbidity. Many previous studies have recommended delayed
cholecystectomy and fistula repair considering that immediate
cholecystectomy or fistula dissection can be associated with
significant morbidity and mortality (28,29). As
the patient was relatively young with no comorbidities in the
present report, an enterolithotomy with cholecystectomy and fistula
repair was performed successfully. The patient had an uneventful
recovery and remains in good health at the time of writing.
In conclusion, Bouveret's syndrome is a rare form of
gallstone ileus. A tailored surgical strategy considering the
patient's age, general and local inflammatory status, and the
presence of comorbidities, in association with the morbidity and
mortality rates of each method should be applied for the successful
management of Bouveret's syndrome.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contribution
Y-BY, YS, J-BX and F-ZQ contributed to the
conception, design and data interpretation. All authors read and
approved the manuscript.
Ethics approval and consent to
participate
This report was approved by the Institutional Review
Board and Human Ethics Committee of the Affiliated Huaian No. 1
People's Hospital of Nanjing Medical University (Huaian, China).
The patient provided wrritten informed consent to participate.
Patient consent for publication
Consent for publication was obtained from the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gallego Otaegui L, Sainz Lete A, Gutiérrez
Ríos RD, Alkorta Zuloaga M, Arteaga Martín X, Jiménez Agüero R,
Medrano Gómez MÁ, Ruiz Montesinos I and Beguiristain Gómez A: A
rare presentation of gallstones: Bouveret s syndrome, a case
report. Rev Esp Enferm Dig. 108:434–436. 2016.PubMed/NCBI
|
|
2
|
Gandhi S and Jani N: Rare cause of gastric
outlet obstruction. J Community Hosp Intern Med Perspect. 8:84–86.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wickbom G: The man behind the syndrome:
Leon Bouveret. The internist who supported surgery. Lakartidningen.
90:162–165. 1993.PubMed/NCBI
|
|
4
|
Kalwaniya DS, Arya SV, Guha S, Kuppuswamy
M, Chaggar JG, Ralte L, Chejera R and Sharma A: A rare presentation
of gastric outlet obstruction (GOO)-The Bouveret's syndrome. Ann
Med Surg (Lond). 4:67–71. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yilmaz EM, Carti EB and Kandemir A: Rare
cause of duodenal obstruction: Bouveret syndrome. Turk J Surg.
28:1–3. 2018.
|
|
6
|
Ong J, Swift C and Ong S: Bouveret's
syndrome: Sense and sensitivity. J Community Hosp Intern Med
Perspect. 8:170–171. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Baharith H and Khan K: Bouveret syndrome:
When there are no options. Can J Gastroenterol Hepatol. 29:17–18.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
VanLandingham SB and Broders CW: Gallstone
ileus. Surg Clin North Am. 62:241–247. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Langhorst J, Schumacher B, Deselaers T and
Neuhaus H: Successful endoscopic therapy of a gastric outlet
obstruction due to a gallstone with intracorporeal laser
lithotripsy: A case of Bouveret's syndrome. Gastrointest Endosc.
51:209–213. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Koulaouzidis A and Moschos J: Bouveret's
syndrome. Narrative review. Ann Hepatol. 6:89–91. 2007.PubMed/NCBI
|
|
11
|
Doycheva I, Limaye A, Suman A, Forsmark CE
and Sultan S: Bouveret's syndrome: Case report and review of the
literature. Gastroenterol Res Pract. 2009:9149512009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gan S, Roy-Choudhury S, Agrawal S, Kumar
H, Pallan A, Super P and Richardson M: More than meets the eye:
Subtle but important CT findings in Bouveret's syndrome. AJR Am J
Roentgenol. 191:182–185. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nickel F, Müller-Eschner MM, Chu J, von
Tengg-Kobligk H and Müller-Stich BP: Bouveret's syndrome:
Presentation of two cases with review of the literature and
development of a surgical treatment strategy. BMC Surg. 13:332013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liew V, Layani L and Speakman D:
Bouveret's syndrome in Melbourne. ANZ J Surg. 72:161–163. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ripollés T, Miguel-Dasit A, Errando J,
Morote V, Gómez-Abril SA and Richart J: Gallstone ileus: Increased
diagnostic sensitivity by combining plain film and ultrasound.
Abdom Imaging. 26:401–405. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS,
Tyan YS, Hwang JI, Liou CH, Chang WC and Chen CY: Value of CT in
the diagnosis and management of gallstone ileus. World J
Gastroenterol. 11:2142–2147. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Balthazar EJ: George W. Holmes Lecture. CT
of small-bowel obstruction. AJR Am J Roentgenol. 162:255–261. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brennan GB, Rosenberg RD and Arora S:
Bouveret syndrome. Radiographics. 24:1171–1175. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pickhardt PJ, Friedland JA, Hruza DS and
Fisher AJ: Case report. CT, MR cholangiopancreatography, and
endoscopy findings in Bouveret's syndrome. AJR Am J Roentgenol.
180:1033–1035. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mavroeidis VK, Matthioudakis DI, Economou
NK and Karanikas ID: Bouveret syndrome-the rarest variant of
gallstone ileus: A case report and literature review. Case Rep
Surg. 2013:8393702013.PubMed/NCBI
|
|
21
|
Cappell MS and Davis M: Characterization
of Bouveret's syndrome: A comprehensive review of 128 cases. Am J
Gastroenterol. 101:2139–2146. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Moschos J, Pilpilidis I, Antonopoulos Z,
Paikos D, Tzilves D, Kadis S, Katsos I and Tarpagos A: Complicated
endoscopic management of Bouveret's syndrome. A case report and
review. Rom J Gastroenterol. 14:75–77. 2005.PubMed/NCBI
|
|
23
|
Hussain A, Obaid S and El-Hasani S:
Bouveret's syndrome: Endoscopic or surgical treatment. Updates
Surg. 65:63–65. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Iancu C, Bodea R, Al Hajjar N, Todea-Iancu
D, Bălă O and Acalovschi I: Bouveret syndrome associated with acute
gangrenous cholecystitis. J Gastrointestin Liver Dis. 17:87–90.
2008.PubMed/NCBI
|
|
25
|
Rodríguez-Sanjuán JC, Casado F, Fernández
MJ, Morales DJ and Naranjo A: Cholecystectomy and fistula closure
versus enterolithotomy alone in gallstone ileus. Br J Surg.
84:634–637. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Khan AZ, Escofet X, Miles WF and Singh KK:
The Bouveret syndrome: An unusual complication of gallstone
disease. J R Soc Promot Health. 122:125–126. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ravikumar R and Williams JG: The operative
management of gallstone ileus. Ann R Coll Surg Engl. 92:279–281.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Reisner RM and Cohen JR: Gallstone ileus:
A review of 1001 reported cases. Am Surg. 60:441–446.
1994.PubMed/NCBI
|
|
29
|
Halabi WJ, Kang CY, Ketana N, Lafaro KJ,
Nguyen VQ, Stamos MJ, Imagawa DK and Demirjian AN: Surgery for
gallstone ileus: A nationwide comparison of trends and outcomes.
Ann Surg. 259:329–335. 2014. View Article : Google Scholar : PubMed/NCBI
|