Introduction
The cause of ejaculation obstruction may vary, and
may be divided into congenital and acquired causes. Congenital
causes include absence or atresia of vas deferens, rudimentary or
absent seminal vesicles, Mullerian duct cyst or Wolffian duct
cysts. Acquired causes include urinogenital infection, trauma and
tumor compression (1). Among these
causes, Mullerian duct cyst is relatively rare in the clinic. The
majority of patients affected are treated due to infertility. A
Mullerian cyst is the remnant from a secondary renal tube that was
not completely degenerated during the process of embryonic
development. Thin layer epithelium, which secretes cystic fluid,
lines the Mullerian cyst (2). At
present, affected patients are mainly treated due to prostatitis
symptoms, while the inflammation symptoms, hemospermia or male
infertility induced by Mullerian cyst have not received sufficient
attention in the clinic.
It has been reported that transurethral ejaculatory
incision was applied for the treatment of obstructive aspermia,
which raised the awareness of clinicians regarding the compression
of the ejaculatory duct by cysts as a type of obstructive aspermia;
therefore, seminal duct obstruction became more detectable and
correctable (3). At present, no
consensus has been reached regarding the optimal treatment for
Mullerian cysts with ejaculation tube obstruction. Therefore, the
present study retrospectively analyzed 20 Mullerian cyst patients
with obstruction-associated aspermia that were treated with
transurethral resection combined with seminal vesiculoscopy
(4). This is the first experience of
treating this condition at The First Affiliated Hospital of Nanjing
Medical University (Nanjing, China). The clinical efficacy and
therapeutic benefits of this procedure were assessed within a
follow-up period of 12 months.
Patients and methods
Patients and pre-operative
examination
A total of 20 patients diagnosed with Mullerian duct
cysts that received surgical treatment between March 2009 and March
2016 at the First Affiliated Hospital of Nanjing Medical University
were enrolled in the present study. The number of patients enrolled
was 20. All patients had experienced infertility for >2 years
following marriage. Patients were recruited if spouse-associated
factors could be excluded and if no spermatozoa were detected in
three consecutive semen routine examinations. Semen specimens of
all patients were obtained by masturbation or sperm collector and
were diagnosed as aspermia via semen analysis (including the
assessment of sperm count, semen volume, sperm density, pH and
fructose level). The patient age ranged from 22 to 38 years (median
age, 29.5 years). None of the patients had any particular symptoms.
The testicular size and genitalia were normal, and the vas deferens
were palpable in all patients. The levels of sex hormones,
including follicle-stimulating hormone, luteinizing hormone,
testosterone, estradiol and prolactin, were within the normal
ranges. Mature sperm production was confirmed in the testicles by
testicular biopsy, and the presence of serious infection,
pathogenic factors and abnormal test indicators was excluded.
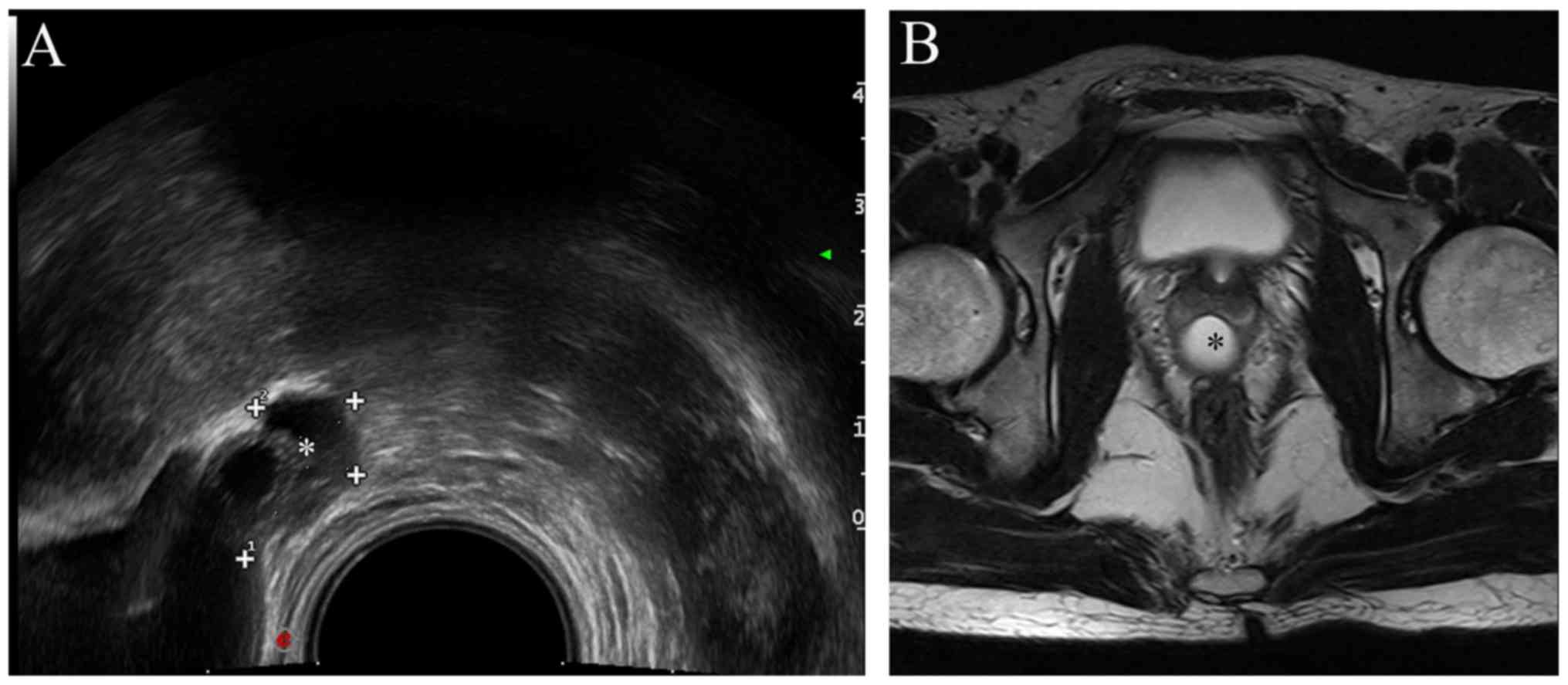
Cystoscopy with methylene blue staining and transrectal
ultrasonography (TRUS) were applied to diagnose the prostatic
midline cyst of eligible patients (Fig.
1A). Magnetic resonance imaging (MRI) also revealed the
Mullerian duct cyst in proximity to or deviated from the central
line of the verumontanum, indicating the seminal vesicle combined
with ejaculatory duct expansion (Fig.
1B).
Surgical procedure
All of the 20 patients were placed in the dorsal
lithotomy position under general or spinal anesthesia. A plasma
resectoscope of F24 (Olympus Corporation, Tokyo, Japan) was
selected for performing the operation, as it causes less damage to
the urethra due to being thinner than the 26F resectoscope. Using
this instrument, the operator is able to resect the cyst and stop
the bleeding more accurately and minimize injury to the adjoining
tissues with a smaller electric cutting ring compared to that of
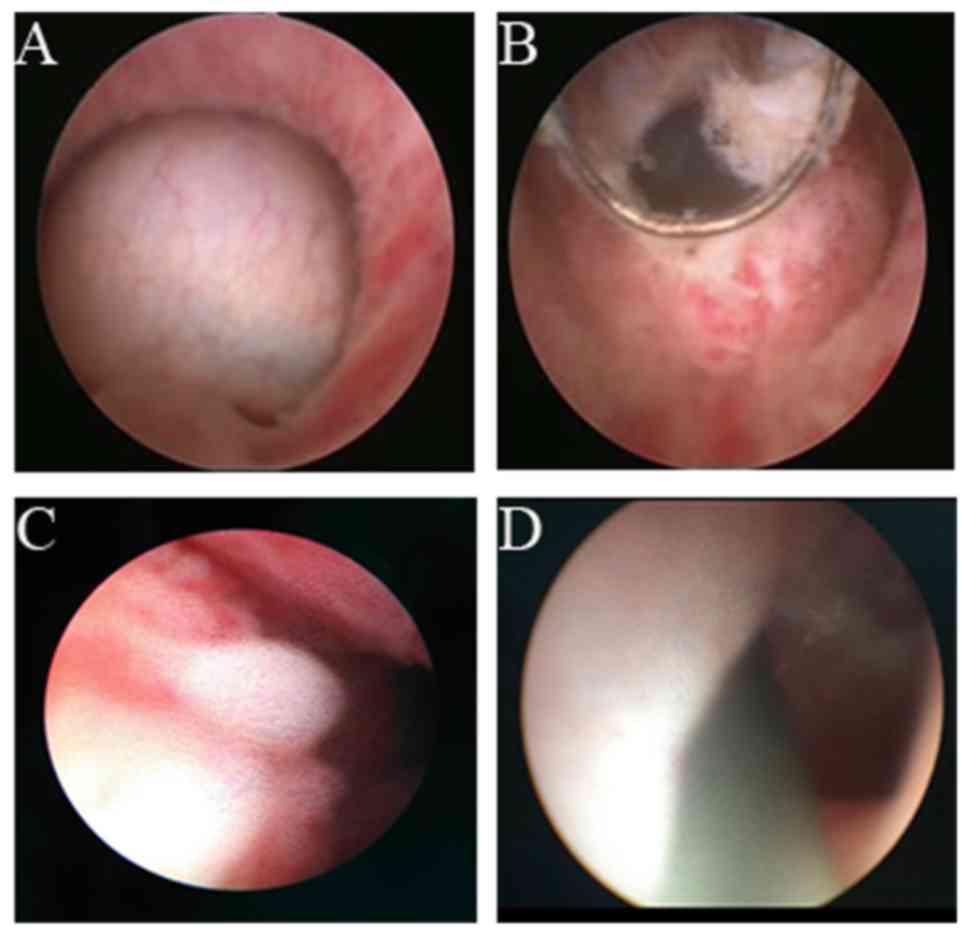
26F. The anatomical landmark was then clearly recognized under
direct vision (Fig. 2A). The
situation of the verumontanum, external urethral sphincter and
bladder neck were also carefully evaluated. Subsequently, the cyst
wall was carefully resected by using thin-layer electric cutting in
the vicinity of the verumontanum, and the distinct milky or
yellowish-brown liquid outflow was observed (Fig. 2B). Transurethral seminal
vesiculoscopy was performed using a 7-F or 8-F rigid ureteroscope
(Olympus Corporation). The ureteroscope was first inserted into the
prostatic urethra for initiatory observation of the verumontanum,
the anatomical landmark of which usually lies in proximity to the
seminal vesicle entrance (Fig. 2C).
Under the guidance of the guidewire, the bilateral ejaculatory duct
openings were identified in the prostatic utricle (Fig. 2D). Subsequently, the ureteroscope was
inserted into the ejaculatory ducts and seminal vesicles were
subjected to intermittent perfusion dilatation by using 0.90% (w/v)
sodium chloride (normal saline). The bilateral ejaculatory ducts
and seminal vesicles were carefully observed on the endoscopic
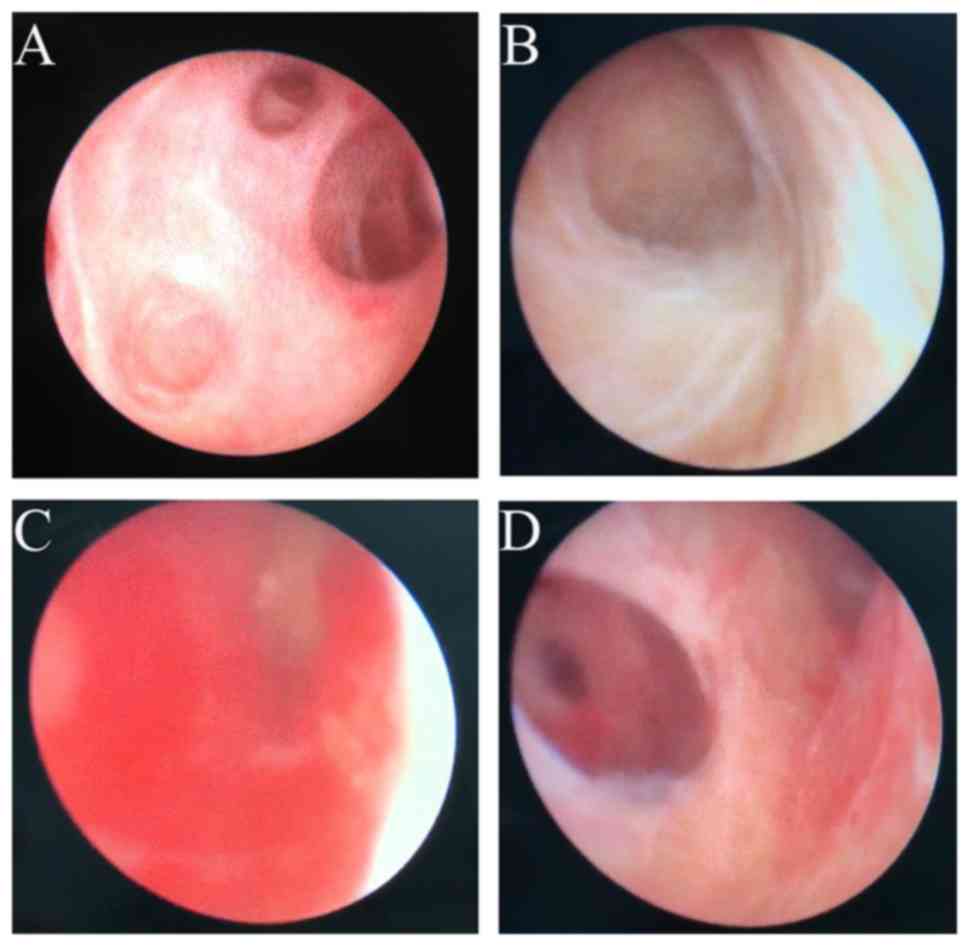
monitor. The seminal vesicles were clearly visible at this time,
revealing that they contained multiple compartments with numerous
folds in its wall and numerous small cavities with beams, as well
as milky seminal plasma in the seminal vesicles (Fig. 3A and B). A bloody substance was
observed in those patients with hematospermia (Fig. 3C). Furthermore, the clear region of
inflammation was washed with physiological saline until the bloody
liquid was rinsed away, and the seminal vesicle cavity was then
washed with normal saline containing antibiotics (levofloxacin, 5
mg/ml; Fig. 3D). If polyps were
present, they were removed using a laser (VersaPulse®
PowerSuite™ 80W; Lumenis, Inc., San Jose, CA, USA) and
sent for pathological examination. The ureteroscope was then
removed and an F18 air sac catheter was retained. The catheter was
removed at 1–2 days after the operation. After the surgery,
antibiotics (levofloxacin, 5 mg/ml) were intravenously injected for
3 days to prevent infection. All patients were instructed to
refrain from ejaculation for 3 weeks and were followed up at 3, 9
and 12 months following surgery by routine semen analysis for 12
months.
Statistical analysis
Values are expressed as the mean ± standard
deviation or the mean (range) and the statistical calculations were
performed using SPSS software (version 13.0; SPSS, Inc., Chicago,
IL, USA). Differences between two groups were compared with
Student's t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient clinical characteristics
All of the 20 patients successfully underwent the
operation combining transurethral resection and seminal
vesiculoscopy without any complications including major bleeding,
incontinence, epididymis or urethral rectum fistula. During the
intra-operative period, the resected cysts and ejaculatory ducts
were carefully identified. The duration of surgery was 19–55 min
(mean, 35 min), the amount of bleeding was 5–12 ml (mean, 7 ml) and
the duration of hospital stay was 3–6 days (mean, 4 days). All
cases were followed up for 12 months to evaluate the efficacy of
the treatment. The clinical characteristics of the patients
enrolled and details regarding the surgical procedure are presented
in Table I.
 | Table I.Clinical characteristics of enrolled
patients (n=20) and data regarding the surgical procedure. |
Table I.
Clinical characteristics of enrolled
patients (n=20) and data regarding the surgical procedure.
| Clinical
characteristic | Value |
|---|
| Age (years) | 30 (22–38) |
| Follow-up period
(months) | 12 |
| Duration of surgery
(min) | 35 (19–55) |
| Bleedinga (ml) | 7 (5–12) |
| Duration of hospital
stay (days) | 4 (3–6) |
Sperm quality improves following
surgery
After the surgery, the follow-up examination of the
semen indicated that the semen volume of the patients increased
constantly, and sperms were also observed in the semen specimens.
In addition, the quality of the semen markedly improved following
the 3 consecutive measurements determined over 12 months. A total
of 8 patients reached normal standard by the end of the follow-up.
Among the 20 patients, the presence of sperm was identified in the
semen of 9 cases at 3 months, in 7 patients at 9 months and the
remaining 4 cases at 12 months after surgery. Furthermore, the
spouses of 8 patients successfully conceived at 12–15 months after
surgery. In 6 patients, the volume of the seminal vesicle glands
was significantly reduced after the operation. The post-operative
semen volume and the seminal plasma fructose level were
significantly higher than those at the pre-operative stage
(P<0.05). A comparison of pre- and post-operative
characteristics is provided in Table
II.
 | Table II.Comparison of the pre- and
post-operative semen parameters. |
Table II.
Comparison of the pre- and
post-operative semen parameters.
| Parameter | Pre-operation | Post-operation | P-value | Normal
rangea |
|---|
| Semen volume
(ml) | 1.3±0.6 | 2.8±1.2 | <0.05 | ≥1.5 |
| Sperm count | 0 | 41.5±1.54 | <0.05 |
≥39×106 |
| Sperm density
(g/ml) | 0 | 15.2±2.90 | <0.05 |
≥15×106 |
| Semen α-glucosidase
(U/l) | 13.7±5.3 | 30.4±6.9 | <0.05 | ≥20 |
| Seminal plasma
fructose (mmol/l) | 11.5±3.2 | 16.2±5.4 | <0.05 | ≥13 |
Discussion
The clinical manifestation of a Mullerian duct cyst
mainly depends on the size of the cyst, concurrent infection and
secondary lesions or deformity. In clinical practice, the volume of
most prostatic Mullerian duct cysts is low, and patients usually do
not have any complaints or experience any discomfort. Mullerian
duct cyst is able to cause obstruction of the ejaculation canal,
thus reducing the volume of ejaculate. In addition, patients with a
less severe presentation may experience discomfort in the perineum,
while severe cases may present with persistent hematospermia and
infertility caused by obstructive aspermia (5–7).
Therefore, the enlargement of the seminal vesicle glands may be
attributed to retention of excreted semen due to the blockage.
In the present study, all patients exhibited a
reduced semen volume and male infertility. TRUS is able to clearly
display the cystic changes in the downstream region of the
prostate. Furthermore, through the location through the urethra and
ejaculatory duct, it was possible to accurately diagnose the
Mullerian duct cyst. The swelling of the seminal vesicle caused by
ejaculatory duct occlusion was simultaneously visualized. MRI scan
may also help to diagnose Mullerian duct cyst and indicate the
expansion of the ejaculatory duct and seminal vesicles (8–10). The
treatment of Mullerian duct cysts is mainly determined by clinical
symptoms and complications associated with it. Current therapeutic
options include TRUS-guided puncture and application of sclerosing
agents (11–13). The surgical treatments consist of
transurethral cyst incision drainage, open cyst resection and
laparoscopic cystectomy (14–16).
Coppens et al (17) suggested
that the treatment of Mullerian duct cysts is most suitable for
symptomatic or infertile patients. A smaller cyst may be observed
regularly without any additional treatment. Furthermore, for large
cysts that are limited to the prostate or beyond the bladder,
transurethral cyst incision is a viable surgical option. However,
this method may damage the verumontanum and cause urethral
stricture, resulting in acute or chronic inflammation of the vas
deferens, seminal vesicle and epididymis, or even occlusion.
Complete obstruction may occur after transurethral resection of
ejaculatory duct in patients with oligospermia or
asthenospermia.
The application of transurethral resection combined
with dilation of the ejaculatory duct for the treatment of
Mullerian duct cyst has been rarely described. In the present
study, the combination of transurethral resection and seminal
vesiculoscopy was utilized to effectively avoid the possibility of
probable adverse events during surgery, including not only the
obstruction of the vas deferens but also relevant complications.
During the surgical procedure, the relative association between
cyst and prostate requires careful evaluation. The range of
resection should not exceed the seminal colliculus and attention
should be paid to the depth of electric resection, as well as the
landmarks of the external urethral sphincter and bladder neck. As a
minimally invasive procedure performed in the urogenital tract, its
application may minimize the damage to the urethra to a certain
extent. However, cautious and elaborate operation is still required
due to the limited space in the urethra and prostate.
In conclusion, the present study provides a rational
surgical approach of transurethral resection combined with seminal
vesiculoscopy for the treatment of Mullerian duct cyst. Compared
with the pre-operative state, patients receiving surgery treatment
obtained an improvement of semen quality. The surgical approach
provided in the present study is highly efficacious in treating
Mullerian duct cyst with male infertility and worth recommending in
clinical practice.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81270685 and
81771640), the Six Talent Peak Project of High-Level Talents in
Jiangsu Province (grant no. WSW-017), the funded project of 333
High-level Talent Cultivation Project in Jiangsu Province, Qing Lan
Project Funding of Jiangsu Higher Education Institutions (grant no.
JX2161015100), A Project Funded by the Priority Academic Program
Development of Jiangsu Higher Education Institutions (grant no.
JX10231802), The Fifth Batch of Outstanding Young and Middle-aged
Teachers Support Plan of Nanjing Medical University, Jiangsu
Province's Key Provincial Talents Program (grant no. ZD RCA2016012)
and the Project of the Nanjing Science and Technology Committee
(grant no. 201605001).
Availability of data and materials
All data generated and/or analyzed during the
present study are included in this published article.
Authors' contributions
ZW and BL conceived and designed the current study.
CM, SL and KZ analyzed the data and wrote the manuscript. JZ, YT
and YW collected the patient data. All authors read and approved
the final version of the manuscript.
Ethics approval and consent to
participate
Approval for this study was granted by the Ethics
Committee of Nanjing Medical University (Nanjing, China) and
written informed consent was obtained from all enrolled
participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
personal or financial interests.
References
|
1
|
Fisch H, Lambert SM and Goluboff ET:
Management of ejaculatory duct obstruction: Etiology, diagnosis,
and treatment. World J Urol. 24:604–610. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kondi-Pafiti A, Grapsa D, Papakonstantinou
K, Kairi-Vassilatou E and Xasiakos D: Vaginal cysts: A common
pathologic entity revisited. Clin Exp Obstet Gynecol. 35:41–44.
2008.PubMed/NCBI
|
|
3
|
Jiang HT, Yuan Q, Liu Y, Liu ZQ, Zhou ZY,
Xiao KF and Yang JG: Multiple advanced surgical techniques to treat
acquired seminal duct obstruction. Asian J Androl. 16:912–916.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu B, Li J, Li P, Zhang J, Song N, Wang Z
and Yin C: Transurethral seminal vesiculoscopy in the diagnosis and
treatment of intractable seminal vesiculitis. J Int Med Res.
42:236–242. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhao H, Luo J, Wang D, Lu J, Zhong W, Wei
J and Chen W: The value of transrectal ultrasound in the diagnosis
of hematospermia in a large cohort of patients. J Androl.
33:897–903. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Paick JS: Transurethral resection of the
ejaculatory duct. Int J Urol. 7 Suppl:S42–S47. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Moukaddam HA, Haddad MC, El-Sayyed K and
Wazzan W: Diagnosis and treatment of midline prostatic cysts. Clin
Imaging. 27:44–46. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pastore AL, Palleschi G, Fuschi A, Porta
N, Cerbelli B, Di Cristofano C, Petrozza V and Carbone A:
Hematospermia and xanthogranulomatous prostatitis: An unusual onset
of a rare diagnosis. Can Urol Assoc J. 7:E820–E822. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Furuya R, Furuya S, Kato H, Saitoh N,
Takahash S and Tsukamoto T: New classification of midline cysts of
the prostate in adults via a transrectal ultrasonography-guided
opacification and dye-injection study. BJU Int. 102:475–478. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Guo Y, Liu G, Yang D, Sun X, Wang H, Deng
C, Zhang Y and Feng ST: Role of MRI in assessment of ejaculatory
duct obstruction. J Xray Sci Technol. 21:141–146. 2013.PubMed/NCBI
|
|
11
|
Fisch H, Kang YM, Johnson CW and Goluboff
ET: Ejaculatory duct obstruction. Curr Opin Urol. 12:509–515. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cheng G, Liu B, Song Z, Xu A, Song N and
Wang Z: A novel surgical management for male infertility secondary
to midline prostatic cyst. BMC Urol. 15:182015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Han CH, Liang Q, Dong BZ, Hao L, Fan T,
Zhang JJ, Zhang WD, Chen B, Qiu XZ, Zhou XJ and Pei CS: The
transurethral seminal vesiculoscopy in the diagnosis and treatment
of the seminal vesicle disease. Cell Biochem Biophys. 66:851–853.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Manohar T, Ganpule A and Desai M:
Transrectal ultrasound-and fluoroscopic-assisted transurethral
incision of ejaculatory ducts: A problem-solving approach to
nonmalignant hematospermia due to ejaculatory duct obstruction. J
Endourol. 22:1531–1535. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang H, Ye H, Xu C, Liu Z, Gao X, Hou J,
Wang L, Piao S and Sun Y: Transurethral seminal vesiculoscopy using
a 6F vesiculoscope for ejaculatory duct obstruction: Initial
experience. J Androl. 33:637–643. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang DX, Li XG, Gao Y, Liu YS, Wang JK,
Chen J, Chen L, Wang K, Cui XG and Xu DF: Transperitoneal
laparoscopic excision of seminal vesicle cyst: A single-center
experience. J Endourol. 26:1153–1158. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Coppens L, Bonnet P, Andrianne R and de
Leval J: Adult müllerian duct or utricle cyst: Clinical
significance and therapeutic management of 65 cases. J Urol.
167:1740–1744. 2002. View Article : Google Scholar : PubMed/NCBI
|