Introduction
Acute respiratory distress syndrome (ARDS) is edema
that appears in diffuse pulmonary interstitial and alveolus and is
caused by a variety of serious intrapulmonary and extrapulmonary
diseases. The diseases facilitate the increase of lung water
content, the decrease of lung volume, the continuous reduction of
lung compliance and the collapse of alveolus. ARDS severely affects
the function of ventilation and blood flow exchange (1,2). The
fatality rate of ARDS is extremely high, and progressive
respiratory distress and refractory hypoxemia are clinical
syndromes characterized by ARDS (3,4). ARDS is
a complicated syndrome whose nosogenesis is multifactorial due to
the involvement of different pathogenies (5,6).
Respiratory mechanics, early central drive and hemodynamics are
commonly used as observation indicators of ARDS (7,8).
Mechanical ventilation therapy and non-mechanical
ventilation therapy are the two main methods for the treatment of
ARDS (9). Recruitment maneuver (RM)
is mechanical ventilation therapy, which reopens the alveoli
without ventilation or hypoventilation and improves the compliance
of oxygenation and respiratory system. Mechanical ventilation
therapy is an important treatment for ARDS (10). The common RM techniques include
sustained inflation (SI) (11),
pressure-controlled ventilation (PCV) (12), and IP (13). The most basic mechanical modes for
patients with ARDS are SI and PCV (14). As a method which promotes RM of
collapsed alveoli, SI can significantly improve lung compliance,
oxygenation, and offset the disadvantages that collapsed alveoli
hardly can achieve RM when the lung protective ventilation is
strategized (15). PCV refers to a
process in which the airway pressure and inspiratory time of the
respirator are set up in advance. When the airflow enters the lungs
quickly and the pressure level in the lungs is equal to the preset
pressure level, the speed of the ventilative airflow will slow down
and the preset pressure level of the respirator is maintained until
the termination of inhaling and then exhaling (12). However, there are few studies
relating to advantages and disadvantages of the effects of SI and
PCV on respiratory mechanics, early central drive and hemodynamics
in the treatment of patients with ARDS. This study compared the
efficacy and safety of the two RM methods by observing the effects
of SI and PCV on respiratory mechanics, early central drive and
hemodynamics in patients with ARDS.
Patients and methods
Patient information
Twenty-six patients with ARDS who were admitted to
the Yiwu Central Hospital (Yiwu, China) from March 2015 to March
2016 were selected. According to the ventilation method adopted by
the patients with ARDS, 13 patients with ARDS who were treated with
SI were included in the SI group, including 8 males and 5 females.
The age range was from 30 to 66 years, and the average age was
48.03±10.01 years; 13 patients with ARDS who were treated with PCV
were included in the PCV group, including 7 males and 6 females.
The age range was from 29 to 65 years, and the average age was
48.04±10.03 years. Inclusion and exclusion criteria were: All
selected people conformed to the diagnostic criteria of WHO for
ARDS (3). Patients who were <18
years old and had serious intracranial hypertension; with
pneumothorax, bronchopleural fistula, chronic obstructive pulmonary
disease, and hemodynamic instability (systolic pressure >180 or
<90 mmHg); who received pulmonary lobectomy within 2 weeks; who
had arrhythmia during RM (heart rate >140 beats/min); whose
heart rates increased by 20 times/min after RM; whose arterial
systolic pressure was abnormal (systolic pressure <90 mmHg);
whose arterial systolic pressure decreased by 30 mmHg after RM;
whose percutaneous arterial oxyhemoglobin saturation was abnormal
(percutaneous arterial oxyhemoglobin saturation <90%) and whose
percutaneous arterial oxyhemoglobin saturation decreased by >5%
after RM, were excluded.
This study was approved by the Ethics Committee of
the Yiwu Central Hospital. Patients who participated in this
research had complete clinical data. The signed informed consents
were obtained from the patients or the guardians. When comparing
the general data of the patients in the two groups, there was no
statistically significant differences (P>0.05) (Table I).
 | Table I.Comparison of the general data of the
patients in the two groups. |
Table I.
Comparison of the general data of the
patients in the two groups.
| General data | SI group (n=13) | PCV group (n=13) | t/χ2
test | P-value |
|---|
| Sex |
| Male | 8 (61.54) | 7 (53.85) | 0.158 | 0.691 |
|
Female | 5 (38.46) | 6 (46.15) |
|
|
| Age (years) |
| ≤48 | 5 (38.46) | 6 (46.15) | 0.158 | 0.691 |
|
>48 | 8 (61.54) | 7 (53.85) |
|
|
| BMI
(kg/m2) |
|
≤18.25 | 9 (69.23) | 8 (61.54) | 0.170 | 0.680 |
|
>18.25 | 4 (30.77) | 5 (38.46) |
|
|
| Blood routine |
| Hb
(gm/dl) | 8.23±1.86 | 11.63±2.63 | 3.806 | <0.001 |
| RBC
(×1012/l) | 4.28±0.37 | 4.19±0.35 | 0.637 | 0.530 |
| PLT
(×109/l) | 148.63±22.78 | 151.63±25.61 | 0.316 | 0.755 |
| Liver function |
| ALT
(U/l) | 22.41±10.43 | 20.41±8.45 | 0.537 | 0.596 |
| AST
(U/l) | 19.35±8.63 | 17.48±7.24 | 0.599 | 0.555 |
| Renal function |
| TP
(g/l) | 130.50±10.44 | 75.98±10.23 | 13.450 | <0.001 |
| UREA
(mmol/l) | 8.09±1.03 | 4.12±1.67 | 7.295 | <0.001 |
| CRE
(µmol/l) | 200.56±20.12 | 98.49±18.08 | 13.610 | <0.001 |
| UA
(µmol/l) | 629.45±40.76 | 204.84±56.19 | 22.050 | <0.001 |
Main instruments
Puritan Bennett 840 respirator (20160077; Shanghai
Jumu Medical Devices Co., Ltd., Shanghai, China).
Methods
All patients with ARDS took the supine position
during the mechanical ventilation. The secretions in airway of
patients were completely cleared away before the artificial airway
was established, and after patients were sedated and given
analgesic, they were treated with ventilation therapy by connecting
Puritan Bennett 840 respirator (20160077; Shanghai Jumu Medical
Devices Co., Ltd.). A low tidal volume of 6–8 ml/k were used to
control ventilation, and breathing rate was regulated at the
frequency of 15 times/min. The vital signs and blood gas analysis
of all patients were closely monitored during the RM. The RM was
used once in each group. Controlling lung expansion, one of the RM
strategies, was used in the SI group: The respirator mode was
adjusted to CPAP mode. The positive end-expiratory pressure
ventilation was maintained at 5 cm H2O, the inspiratory
pressure was from 30 to 45 cm H2O, and the duration was
20 sec. Pressure controlled ventilation was used in the PCV group:
The respirator mode was adjusted to BIPAP mode. The pressure was
adjusted to a high pressure of 40 cm H2O and a low
pressure of 20 cm H2O, and this condition was maintained
for 2 min, then the ventilation condition and mode were recovered
to what it used to be.
Observation indicators
i) Respiratory mechanics
The indicators of respiratory mechanics before and
after RM at 1, 10, 20 and 30 min were monitored: Peak inflation
pressure (PIP) cmH2O, plateau pressure (Pplate)
cmH2O, and compliance of the respiratory system (Crs)
ml/cmH2O/kg.
ii) Early central drive
The indicators of central-mechanical-ventilation
coupling before and after RM were monitored, including VE/RMS
(l/µV), VT/RMS (ml/µV), ΔPdi/RMS (cmH2O/µV); VT/RMS and
VE/RMS reflected central-ventilation coupling and ΔPdi/RMS
reflected central-mechanical coupling.
iii) Hemodynamics
Heart rate (HR), mean arterial pressure (MAP), and
central venous pressure (CVP) were monitored and recorded before
and after RM at 1, 10, 20 and 30 min.
Statistical analysis. SPSS 17.0 software system
(SPSS, Inc., Chicago, IL, USA) was used to carry out the
statistical analysis. The enumeration data were expressed in the
form of [n (%)]. The measurement data were expressed as the mean ±
SD. Independent-samples t-test was used in the comparison of the
data between two groups, and χ2 test was used in the
enumeration data. One-way ANOVA test with Least Significant
Difference test was used in the comparison of the data between
groups. At P<0.05 the difference was statistically
significant.
Results
Comparison of each indicator of
respiratory mechanics between two groups
i) Comparison of PIP between two
groups
The differences were not statistically significant
when comparing PIP in patients in the SI group and the PCV group
before RM with that after RM at 1, 10, 20 and 30 min (P>0.05).
The comparison within the group showed that when the peak of PIP in
patients in the SI group and the PCV group appeared at 1 min after
RM, PIP was significantly higher than that before RM (P<0.05).
PIP of both groups gradually decreased after RM, and the comparison
of PIP at different time-points showed that the differences were
statistically significant (P<0.05) (Table II).
 | Table II.Comparison of PIP (cmH2O)
in the patients in the two groups. |
Table II.
Comparison of PIP (cmH2O)
in the patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 27.01±8.34 | 28.46±8.05 | 0.451 | 0.656 |
| After RM at 1
min |
48.35±6.75a |
46.02±6.48a | 0.898 | 0.378 |
| After RM at 10
min |
31.51±6.01b |
34.39±5.04b | 1.324 | 0.198 |
| After RM at 20
min | 26.77±8.01 | 27.39±5.97 | 0.825 | 0.224 |
| After RM at 30
min | 23.58±7.93 | 25.59±6.49 | 0.707 | 0.486 |
| F-test | 22.720 | 21.400 |
|
|
| P-value | <0.001 | <0.001 |
|
|
ii) Comparison of Pplate between two
groups
The differences were not statistically significant
when comparing Pplate in patients in the SI group and the PCV group
before RM with that after RM at 1, 10, 20 and 30 min (P>0.05).
The comparison within the group showed that when the peak of Pplate
in patients in the SI group and the PCV group appeared at 1 min
after RM, Pplate was significantly higher than that before RM
(P<0.05). Pplate of both groups gradually decreased after RM,
and the comparison of Pplate at different time-points showed that
the differences were statistically significant (P<0.05)
(Table III).
 | Table III.Comparison of Pplate
(cmH2O) in the patients in the two groups. |
Table III.
Comparison of Pplate
(cmH2O) in the patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 23.74±5.07 | 23.01±5.27 | 0.722 | 0.360 |
| After RM at 1
min |
39.43±6.68a |
39.47±4.52a | 0.018 | 0.986 |
| After RM at 10
min | 24.19±4.06 | 25.56±5.02 | 0.765 | 0.452 |
| After RM at 20
min | 23.06±3.96 | 23.03±3.74 | 0.020 | 0.984 |
| After RM at 30
min | 20.83±4.69 | 21.79±4.99 | 0.505 | 0.618 |
| F-test | 29.210 | 31.180 |
|
|
| P-value | <0.001 | <0.001 |
|
|
iii) Comparison of Crs between two
groups
The differences were not statistically significant
when comparing Crs in patients in the SI group and the PCV group
before RM with that after RM at 1, 10, 20 and 30 min (P>0.05).
The comparison within the group showed that when the valley value
of Crs in patients in the SI group and the PCV group appeared at 1
min after RM, Crs was significantly lower than that before RM
(P<0.05). Crs in the two groups showed an upward trend from 1 to
10 min after RM, but Crs in the two groups showed a downward trend
from 10 to 30 min after RM, and the comparison of Crs at different
time-points showed that the differences were statistically
significant (P<0.05) (Table
IV).
 | Table IV.Comparison of Crs
(ml/cmH2O/kg) in the patients in the two groups. |
Table IV.
Comparison of Crs
(ml/cmH2O/kg) in the patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 39.34±11.82 | 38.49±12.03 | 0.182 | 0.858 |
| After RM at 1
min |
28.03±8.33a |
27.57±7.92a | 0.144 | 0.887 |
| After RM at 10
min | 38.90±10.36 | 37.64±11.57 | 0.293 | 0.772 |
| After RM at 20
min | 36.94±6.69 | 35.59±6.81 | 0.510 | 0.615 |
| After RM at 30
min | 34.90±7.04 | 34.78±6.88 | 0.044 | 0.965 |
| F-test | 3.342 | 2.786 |
|
|
| P-value | 0.016 | 0.034 |
|
|
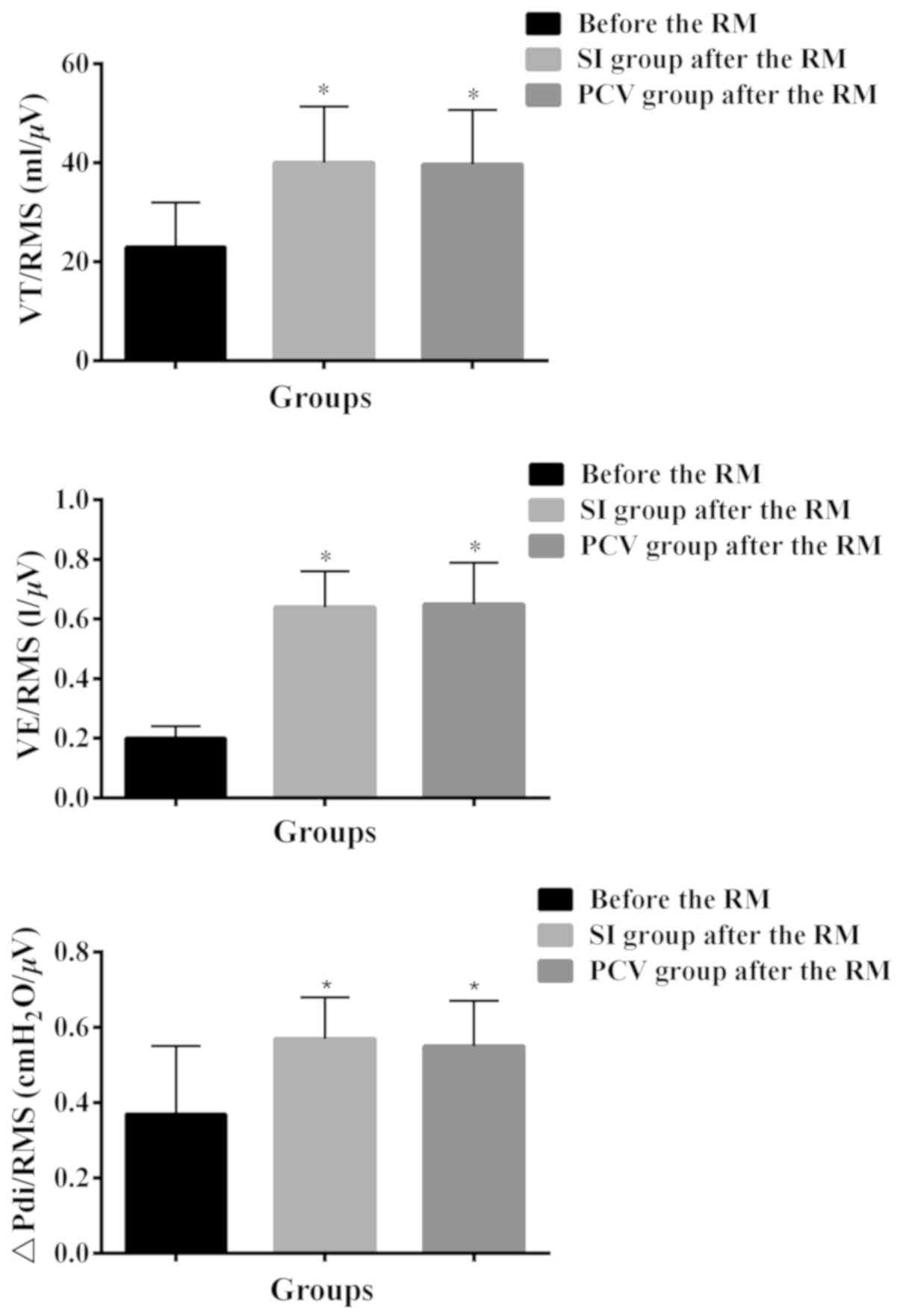
Comparison of the changes of each indicator of early
central drive in the two groups before and after RM. Before RM,
VT/RMS was 23.01±9.02 ml/µV, VE/RMS was 0.20±0.04 l/µV, ΔPdi/RMS
was 0.37±0.18 cm H2O/µV. VT/RMS in the SI group and the
PCV group after RM was respectively 40.03±11.36 and 39.65±11.06
ml/µV, which were both significantly higher than VT/RMS before RM,
and the differences were statistically significant (P<0.05);
VE/RMS in the SI group and the PCV group after RM, respectively
were 0.64±0.12 and 0.65±0.14 l/µV, which were significantly higher
than VE/RMS before RM, and the differences were statistically
significant (P<0.05); ΔPdi/RMS in the SI group and the PCV group
after RM respectively were 0.57±0.11 cm H2O/µV and
0.55±0.12 cm H2O/µV, which were both significantly
higher than ΔPdi/RMS before RM, and the differences were
statistically significant (P<0.05); the differences were not
statistically significant when comparing VT/RMS, VE/RMS, ΔPdi/RMS
in the SI group with those in the PCV group after RM (P>0.05)
(Table V and Fig. 1).
 | Table V.Comparison of the changes of each
indicator of early central drive in the two groups before and after
RM. |
Table V.
Comparison of the changes of each
indicator of early central drive in the two groups before and after
RM.
|
|
| After RM |
|
|
|---|
|
|
|
|
|
|
|---|
| Index | Before RM | SI group
(n=13) | PCV group
(n=13) | F-test | P-value |
|---|
| VT/RMS (ml/µV) | 23.01±9.02 |
40.03±11.36a |
39.65±11.06a | 11.070 | <0.001 |
| VE/RMS (l/µV) | 0.20±0.04 |
0.64±0.12a |
0.65±0.14a | 72.34 | <0.001 |
| ΔPdi/RMS
(cmH2O/µV) | 0.37±0.18 |
0.57±0.11a |
0.55±0.12a | 8.034 | 0.001 |
Comparison of each indicator of
hemodynamics in the two groups
i) Comparison of HR between two
groups
The differences were not statistically significant
when comparing HR in patients in the SI group and the PCV group
before RM with that after RM at 1, 10, 20 and 30 min (P>0.05).
The comparison within the group showed that when the peak of HR in
patients in the SI and the PCV group appeared at 1 min after RM, HR
was significantly higher than that before RM (P<0.05). HR of
both groups gradually decreased after RM, and the comparison of HR
at different time-points showed that the differences were
statistically significant (P<0.05) (Table VI).
 | Table VI.Comparison of HR (beat/min) in the
patients in the two groups. |
Table VI.
Comparison of HR (beat/min) in the
patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 107.20±19.09 | 108.27±22.46 | 0.131 | 0.131 |
| After RM at 1
min |
127.34±24.95a |
126.66±25.01b | 0.069 | 0.945 |
| After RM at 10
min | 123.63±21.03 | 110.41±21.68 | 1.578 | 0.128 |
| After RM at 20
min | 117.99±19.45 | 108.05±20.85 | 1.257 | 0.221 |
| After RM at 30
min | 110.38±20.11 | 109.42±20.43 | 0.121 | 0.905 |
| F-test | 2.140 | 1.670 |
|
|
| P-value | 0.087 | 0.169 |
|
|
ii) Comparison of MAP between two
groups
The differences were not statistically significant
when comparing MAP in patients in the SI group and the PCV group
before RM with that after RM at 1, 10, 20 and 30 min (P>0.05).
The comparison within the group showed that when the valley value
of MAP in patients in the SI group and the PCV group appeared at 1
min after RM, MAP was significantly lower than that before RM
(P<0.05). MAP of both groups gradually increased after RM, and
the comparison of MAP at different time-points showed that the
differences were statistically significant (P<0.05) (Table VII).
 | Table VII.Comparison of MAP (mmHg) in the
patients in the two groups. |
Table VII.
Comparison of MAP (mmHg) in the
patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 83.21±18.26 | 81.57±15.02 | 0.250 | 0.805 |
| After RM at 1
min |
70.86±11.40a |
71.34±12.56b | 0.102 | 0.920 |
| After RM at 10
min | 71.94±12.73 | 80.59±18.01 | 1.414 | 0.170 |
| After RM at 20
min | 77.80±14.99 | 82.04±18.69 | 0.638 | 0.530 |
| After RM at 30
min | 82.92±18.76 | 83.12±17.59 | 0.028 | 0.980 |
| F-test | 1.851 | 1.086 |
|
|
| P-value | 0.131 | 0.372 |
|
|
iii) Comparison of CVP between two
groups
When the two groups were compared, it was found that
there were no significant differences between the two groups before
RM and at 1 and 30 min after RM. CVP in patients in the SI group at
10 and 20 min after RM was significantly higher than that in the
PCV group, and the difference was statistically significant
(P<0.05). The comparison within the group showed that when the
peak of CVP in patients in the SI group and the PCV group appeared
at 1 min after RM, CVP was significantly higher than that before RM
(P<0.05). CVP of both groups gradually decreased after RM, and
the comparison of CVP at different time-points showed that the
difference was statistically significant (P<0.05) (Table VIII).
 | Table VIII.Comparison of CVP (cmH2O)
in the patients in the two groups. |
Table VIII.
Comparison of CVP (cmH2O)
in the patients in the two groups.
| Index | SI group
(n=13) | PCV group
(n=13) | t-test | P-value |
|---|
| Before RM | 10.24±1.43 | 10.68±1.11 | 0.876 | 0.390 |
| After RM at 1
min | 15.46±1.92 | 14.89±1.69 | 0.804 | 0.430 |
| After RM at 10
min |
14.12±1.59a | 11.61±2.01 | 3.531 | 0.002 |
| After RM at 20
min |
13.68±2.01a | 10.01±1.02 | 5.871 | <0.001 |
| After RM at 30
min | 10.39±1.03 | 9.59±1.30 | 1.739 | 0.095 |
| F-test | 26.70 | 26.85 |
|
|
| P-value | <0.001 | <0.001 |
|
|
Discussion
The mortality of patients with ARDS is up to 39–69%.
The obvious decrease of pulmonary volume and the uneven lesions are
the important features of ARDS (16). It has been reported that the
incidence of patients with ARDS is closely related to the
indicators of respiratory function in their own biological
mechanism, including PIP, Pplate, Crs, the condition of
central-mechanical-ventilation coupling before and after RM,
hemodynamics, HR, MAP, and CVP (8).
The treatment of ARDS is mainly based on the active treatment of
protopathy, and patients with ARDS are treated with mechanical
ventilation to prevent further lung damage and reduce acute lung
damage or the case fatality rate of ARDS (16,17). In
the process of mechanical ventilation, the occurrence of high
airway pressure is frequent, which will result in barotrauma. The
traditional volumetric ventilation mode easily results in
barotrauma due to the constant volume and high peak pressure, and
different ventilation modes may have different effects on patients
with ARDS (18,19). RM is an important means for the
treatment of ARDS. There are many types of RM used in clinical
practice, among which SI and PCV are commonly used for the
treatment of ARDS (20). At present,
there are few studies on the advantages and disadvantages of the
effects of SI and PCV on respiratory mechanics, early central drive
and hemodynamics in the treatment of patients with ARDS. This study
compared the efficacy and safety of the two RM methods by observing
the effects of SI and PCV on respiratory mechanics, early central
drive and hemodynamics in patients with ARDS.
In this study, according to the ventilation method
adopted by patients with ARDS, 13 patients who received SI
treatment were included in the SI group. At the same time, 13
patients who received PCV treatment were included in the PCV group.
The changes of respiratory mechanics, early central drive and
hemodynamics in the two groups before RM were compared with those
after RM. The comparison of each indicator of respiratory mechanics
in the two groups showed that the differences were not
statistically significant when comparing PIP, Pplate and Crs in
patients in the SI group and the PCV group before RM with those
after RM at 1, 10, 20 and 30 min (P>0.05). However, the
comparison of each indicator of hemodynamics in the two groups
showed that the differences were not statistically significant when
comparing HR and MAP in patients in the SI group and the PCV group
before RM with those after RM at 1, 10, 20 and 30 min (P>0.05).
When comparing the two groups with each other, the CVP in patients
in the SI group after RM at 10 and 20 min was significantly higher
than that in the PCV group, and the differences were statistically
significant (P<0.05). Based on the above results, we speculated
that there was little difference in the effect between SI and PCV
on respiratory mechanics in patients with ARDS, but the CVP in
patients in the SI group after RM at 10 and 20 min was
significantly higher than that in the PCV group, which suggested
that SI had a greater effect than PCV on hemodynamics in patients
with ARDS. At present, there are few studies related to the effects
of the mechanical ventilation methods SI and PCV, on respiratory
mechanics and hemodynamics in patients with ARDS. Some studies have
shown that there is little difference in the effect between SI and
PCV on respiratory mechanics and hemodynamics in patients with
ARDS; the two mechanical ventilation methods, SI and PCV, are
equally available for patients with ARDS. There is no conclusion
that one ventilation method could replace another kind of
ventilation method (21,22). The changes of each indicator of early
central drive in patients in the two groups before and after RM
showed that VT/RMS, VE/RMS and ΔPdi/RMS in the SI group and the PCV
group after RM were both significantly higher than those before RM,
and the differences were statistically significant (P<0.05).
However, when respectively comparing VT/RMS, VE/RMS and ΔPdi/RMS in
the SI group after RM with those in the PCV group after RM, and the
differences were not statistically significant (P>0.05).
Therefore, we believed that the two mechanical ventilation methods,
SI and PCV, had similar effects on early central drive in patients
with ARDS, and could enhance the effect of
central-mechanical-ventilation coupling after RM. There are few
studies on the effects of SI and PCV on early central drive in
patients with ARDS, but we still consulted a small number of
studies which were related to the effect of early central drive in
patients with ARDS to support the rationality of the results of
this study (23).
In this study, the number of enrolled patients was
small, which may result in some contingency on the results. In
conclusion, there is little difference between the effect of SI and
PCV on respiratory mechanics and early central drive and
hemodynamics in patients with ARDS, and both of the mechanical
ventilation methods can enhance the effect of
central-mechanical-ventilation coupling after RM. Therefore, the
mechanical ventilation methods SI and PCV, are equally available
for patients with ARDS.
Acknowledgements
Not applicable.
Funding
This study was supported by Yiwu General Scientific
Research Program in 2017 (17–1-07).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MJ was in charge of the study and drafted the
manuscript. MC, TC, YJ, JZ, XW and XHo acquired the data. XHu and
NZ were responsible for observation indicators and analyzed the
data. NZ reviewed the manuscript and finalized it. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yiwu Central Hospital (Yiwu, China). Each patient who participated
in this research, signed an informed consent and had complete
clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Papazian L, Calfee CS, Chiumello D, Luyt
CE, Meyer NJ, Sekiguchi H, Matthay MA and Meduri GU: Diagnostic
workup for ARDS patients. Intensive Care Med. 42:674–685. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bein T, Grasso S, Moerer O, Quintel M,
Guerin C, Deja M, Brondani A and Mehta S: The standard of care of
patients with ARDS: Ventilatory settings and rescue therapies for
refractory hypoxemia. Intensive Care Med. 42:699–711. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duan EH, Adhikari NK, D'Aragon F, Cook DJ,
Mehta S, Alhazzani W, Goligher E, Charbonney E, Arabi YM, Karachi
T, et al: Management of ARDS and refractory hypoxemia: A
multicenter observational study. Ann Am Thorac Soc. 14:1818–1826.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pipeling MR and Fan E: Therapies for
refractory hypoxemia in acute respiratory distress syndrome. JAMA.
304:2521–2527. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Madotto F, Pham T, Bellani G, Bos LD,
Simonis FD, Fan E, Artigas A, Brochard L, Schultz MJ and Laffey JG:
LUNG SAFE Investigators the ESICM Trials Group. Resolved versus
confirmed ARDS after 24 h: Insights from the LUNG SAFE study.
Intensive Care Med. 44:564–577. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Marik PE and Long A: ARDS complicating
pustular psoriasis: Treatment with low-dose corticosteroids,
vitamin C and thiamine. BMJ Case Rep. Feb 2–2018.(Epub ahead of
print). doi: 10.1136/bcr-2017-223475. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ding LC, Liu XF, Chao HE, Zuo J, Wang S,
Li W and Lin Z: Study of Shenfu injection on blood flow volume of
lungs and breathing mechanics in ARDS. Zhongguo Zhong Yi Ji Ζheng.
5:774–775,792. 2010.(In Chinese).
|
|
8
|
Vieillard-Baron A, Matthay M, Teboul JL,
Bein T, Schultz M, Magder S and Marini JJ: Experts' opinion on
management of hemodynamics in ARDS patients: Focus on the effects
of mechanical ventilation. Intensive Care Med. 42:739–749. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhu GF, Wang DJ, Liu S, Jia M and Jia SJ:
Efficacy and safety of noninvasive positive pressure ventilation in
the treatment of acute respiratory failure after cardiac surgery.
Chin Med J (Engl). 126:4463–4469. 2013.PubMed/NCBI
|
|
10
|
Girard TD and Bernard GR: Mechanical
ventilation in ARDS: A state-of-the-art review. Chest. 131:921–929.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arnal JM, Paquet J, Wysocki M, Demory D,
Donati S, Granier I, Corno G and Durand-Gasselin J: Optimal
duration of a sustained inflation recruitment maneuver in ARDS
patients. Intensive Care Med. 37:1588–1594. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Santos CL, Santos RS, Moraes L, Samary CS,
Felix NS, Silva JD, Morales MM, Huhle R, Abreu MG, Schanaider A, et
al: Effects of pressure support and pressure-controlled ventilation
on lung damage in a model of mild extrapulmonary acute lung injury
with intra-abdominal hypertension. PLoS One. 12:e01782072017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sahetya SK, Goligher EC and Brower RG:
Fifty years of research in ARDS. Setting positive end-expiratory
pressure in acute respiratory distress syndrome. Am J Respir Crit
Care Med. 195:1429–1438. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rozé H, Doassans G, Repusseau B and
Ouattara A: Decrease of thoracopulmonary compliance with pressure
assist controlled ventilation in ARDS patients under ECMO and
transported to a referral centre. Intensive Care Med. 43:148–149.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Becher T, Rostalski P, Kott M, Adler A,
Schädler D, Weiler N and Frerichs I: Global and regional assessment
of sustained inflation pressure-volume curves in patients with
acute respiratory distress syndrome. Physiol Meas. 38:1132–1144.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guérin C, Papazian L, Reignier J, Ayzac L,
Loundou A and Forel JM: investigators of the Acurasys Proseva
trials. Effect of driving pressure on mortality in ARDS patients
during lung protective mechanical ventilation in two randomized
controlled trials. Crit Care. 20:3842016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takeuchi M and Tachibana K: Mechanical
ventilation for ARDS patients - for a better understanding of the
2012 Surviving Sepsis Campaign Guidelines. Cardiovasc Hematol
Disord Drug Targets. 15:41–45. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Aydın V, Kabukcu HK, Sahin N, Mesci A,
Arici AG, Kahveci G and Ozmete O: Comparison of pressure and
volume-controlled ventilation in laparoscopic cholecystectomy
operations. Clin Respir J. 10:342–349. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Davies SW, Leonard KL, Falls RK Jr, Mageau
RP, Efird JT, Hollowell JP, Trainor WE 2nd, Kanaan HA, Hickner RC,
et al: Lung protective ventilation (ARDSNet) versus airway pressure
release ventilation: ventilatory management in a combined model of
acute lung and brain injury. J Trauma Acute Care Surg. 78:240–249.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang JG, Chen XJ, Liu F, Zeng ZG and Qian
KJ: Lung recruitment maneuver effects on respiratory mechanics and
extravascular lung water index in patients with acute respiratory
distress syndrome. World J Emerg Med. 2:201–205. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Parida S and Bidkar PU: Advanced pressure
control modes of ventilation in cardiac surgery: Scanty evidence or
unexplored terrain? Indian J Crit Care Med. 20:169–172. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tugrul S, Akinci O, Ozcan PE, Ince S, Esen
F, Telci L, Akpir K and Cakar N: Effects of sustained inflation and
postinflation positive end-expiratory pressure in acute respiratory
distress syndrome: Focusing on pulmonary and extrapulmonary forms.
Crit Care Med. 31:738–744. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mauri T, Grasselli G, Suriano G, Eronia N,
Spadaro S, Turrini C, Patroniti N, Bellani G and Pesenti A: Control
of respiratory drive and effort in extracorporeal membrane
oxygenation patients recovering from severe acute respiratory
distress syndrome. Anesthesiology. 125:159–167. 2016. View Article : Google Scholar : PubMed/NCBI
|