Introduction
Crohn's disease is a recurrent chronic inflammatory
bowel disease based on genetic susceptibility, with environmental
factors involved. It occurs mostly in young and middle-aged people
with an incidence of approximately 1 in 200. Many patients with
Crohn's disease experience feeble physical symptoms (such as
emergency diarrhea, hemoproctia, vomiting, anorexia and lethargy)
throughout their lives, seriously affecting their mental health and
quality of life (1,2). At present, the etiology and
pathogenesis of Crohn's disease have not been fully studied, so
there is a lack of specific treatment for it. In addition, it is
often accompanied by recurrent complications such as intestinal
obstruction and fistulization, so its medical expenses are also
higher, which can be as high as 2 billion USD in the United States.
Therefore, it is very important to find cost-effective drugs
(3,4).
Currently, many studies show that intestinal tissue
damage is mainly caused by abnormalities in the immune response of
intestinal mucosa with genetic susceptibility as a result of
genetic and environmental factors (5,6). In
recent years, some studies have found that in addition to
regulating calcium and phosphorus metabolism, vitamin D also
regulates immune function. Studies report that vitamin D deficiency
is prevalent in patients with Crohn's disease, correlated with the
degree of disease activity (7,8). Vitamin
D has been currently reported to be able to alleviate the symptoms
of Crohn's disease (9,10), but its specific mechanism of action
has not been fully studied. Secreted by Th17 cells, interleukin
(IL)-17 exerts anti- and pro-inflammatory effects by binding to
IL-17 receptor (IL-17R) (11). It
has been reported that IL-17 can inhibit the differentiation of
CD4+ T cells into Th1 cells and regulate immune
function, and its expression level significantly increases in
Crohn's disease (12).
It is hypothesized that the therapeutic effects of
vitamin D may be related to IL-17/IL-17R pathway. Therefore,
Crohn's disease rat models were established, to study the immune
regulation mechanism of vitamin D level and IL-17/IL-17R pathway in
Crohn's disease.
Materials and methods
Study objects
A total of 40 clean mature healthy Sprague-Dawley
(SD) rats were purchased from the Experimental Animal Center of
Guangzhou University of Traditional Chinese Medicine (Guangdong,
China; production license no. SCXK 2013-0034), with an average age
of 43.6±1.7 days and an average body weight of 235.3±7.6 g. They
were fed with ordinary nutrient feed (Jiangsu Synergy
Pharmaceutical Bioengineering Co., Ltd., Jiangsu, China), with
acidified drinking water that had a pH value between 2.5 and 3
after autoclaved sterilization, a feeding temperature of 17–21°C
and a relative humidity of 45–65%. They were fed separately in
terrariums, with bedding changed regularly every morning and
evening; ambient noise less than 85 decibels; ammonia concentration
less than 20 PPm; 8–12 times of ventilation per hour; 1–2 times of
nest changing, cleaning and disinfection every week; fluorescent
lamp with a 12-h cycle of light. Ten rats were used as control
group with random number table, the remaining 30 rats to establish
Crohn's disease rat models. After successful modeling, 30 rats were
divided into model group, low-dose group and high-dose group based
on random number table.
This study was approved by the Ethics Committee of
Luoyang Central Hospital Affiliated to Zhengzhou University
(Luoyang, China).
Modeling methods
After fed for 7 days, all rats were fasted for 24 h,
routinely and disinfected in their abdomen. Then 10% chloral
hydrate (Shanghai Shifeng Biotechnology Co., Ltd., Shanghai, China;
300 µg/g body weight) was intraperitoneally injected for
anesthesia. A silicone catheter (Beijing Huakang Pumei Technology
Co., Ltd., Beijing, China) was inserted into the colon,
approximately 6–8 cm from the anus. The prepared
trinitrobenzenesulfonic acid (TNBS; Shanghai Shifeng Biotechnology
Co., Ltd.) solution (TNBS mixed with 40% ethanol solution at a
ratio of 2:1) was perfused through a catheter at a dose of 150
mg/kg, to establish Crohn's disease rat models. Rats in control
group were perfused with an equal volume of saline. All rats were
routinely fed after modeling operation. The day of the modeling
operation was the 0 day.
Administration methods
On the 1st day after modeling, rats in control group
and model group were routinely supplied with feed and drinking
water, rats in low-dose group given a single dose of 1,750 IU of
vitamin D (Shanghai Yihe Biotechnology Co., Ltd., Shanghai, China;
item no. YH-011523S), and rats in high-dose group given a single
dose of 7,500 IU of vitamin D. Rats in low-dose group and high-dose
group were intragastrically fed and administered for consecutive 10
days. After 10 days of administration, relevant indicators were
detected.
Observation indicators
Changes in the condition of rats after modeling were
observed and scored based on the scoring standards of disease
activity index. After 10 days of administration, the colon of rats
was taken during operation. ELISA was used for detecting IL-12,
IL-17 and CXCL11 levels in colon tissues, western blotting for
detecting IL-17R level in colon tissues, flow cytometry for
detecting Th1 cell and Th17 cell levels in the lamina propria of
colon mucosa. Rats were sacrificed by acute blood loss. Specific
operations referred to the instructions of reagents and
instruments. Detection kits were purchased from Shanghai Jingkang
Bioengineering Co., Ltd. (Shanghai, China).
Statistical analysis
SPSS version 19.0 (AsiaAnalytics, Formerly SPSS
China, Shanghai, China) was used. Enumeration data were expressed
as [n(%)]. χ2 test was used for the comparison of ratio.
Measurement data are expressed as mean ± standard deviation.
Student's t-test was used for comparison between the two groups,
ANOVA for repeated measurement for comparison at different times in
the group, and ANOVA for comparison among multiple groups with LSD
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
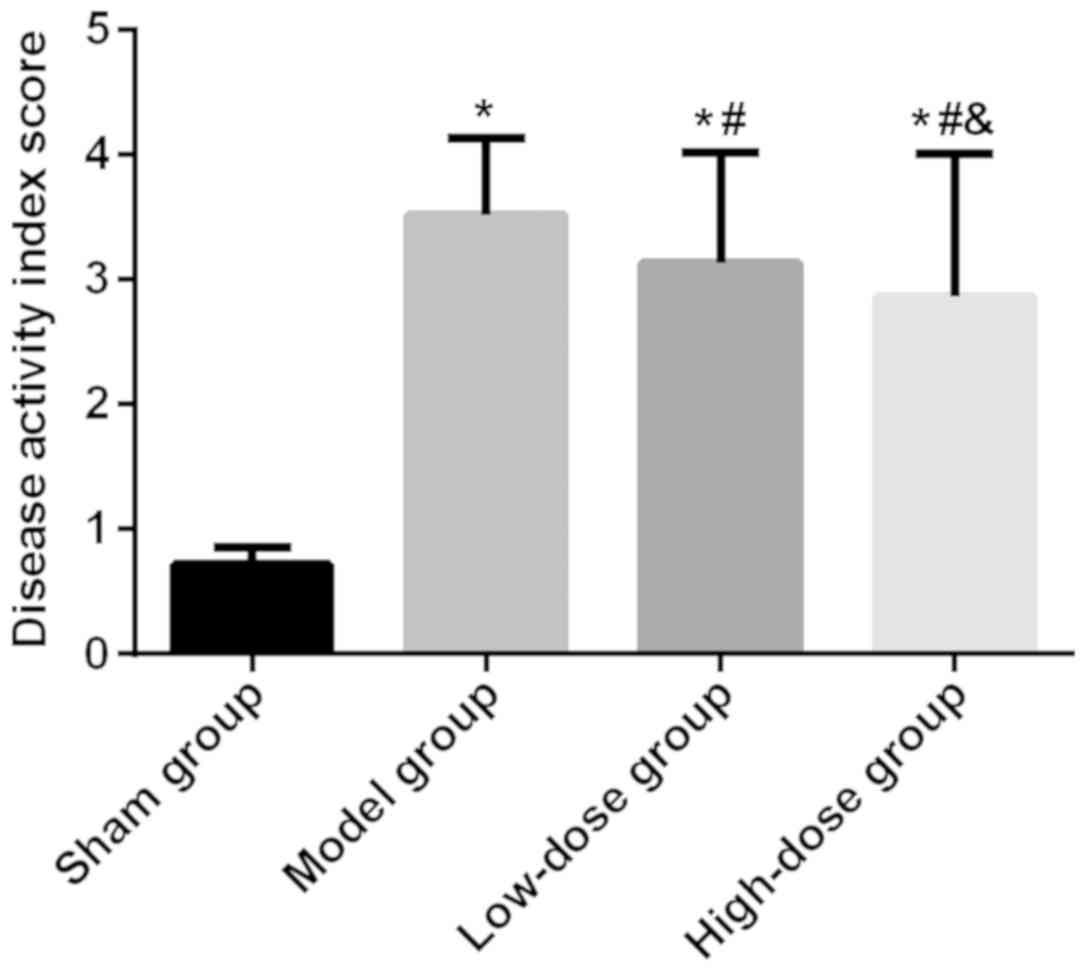
Disease activity index scores
There were significant differences in disease
activity index scores among the four groups of rats (P<0.05).
Disease activity index scores were significantly higher in model
group, low-dose group and high-dose group of rats than those in
control group (P<0.05), and were significantly lower in low-dose
group and high-dose group of rats than those in model group
(P<0.05), and were significantly lower in high-dose group of
rats than those in low-dose group (P<0.05; Fig. 1).
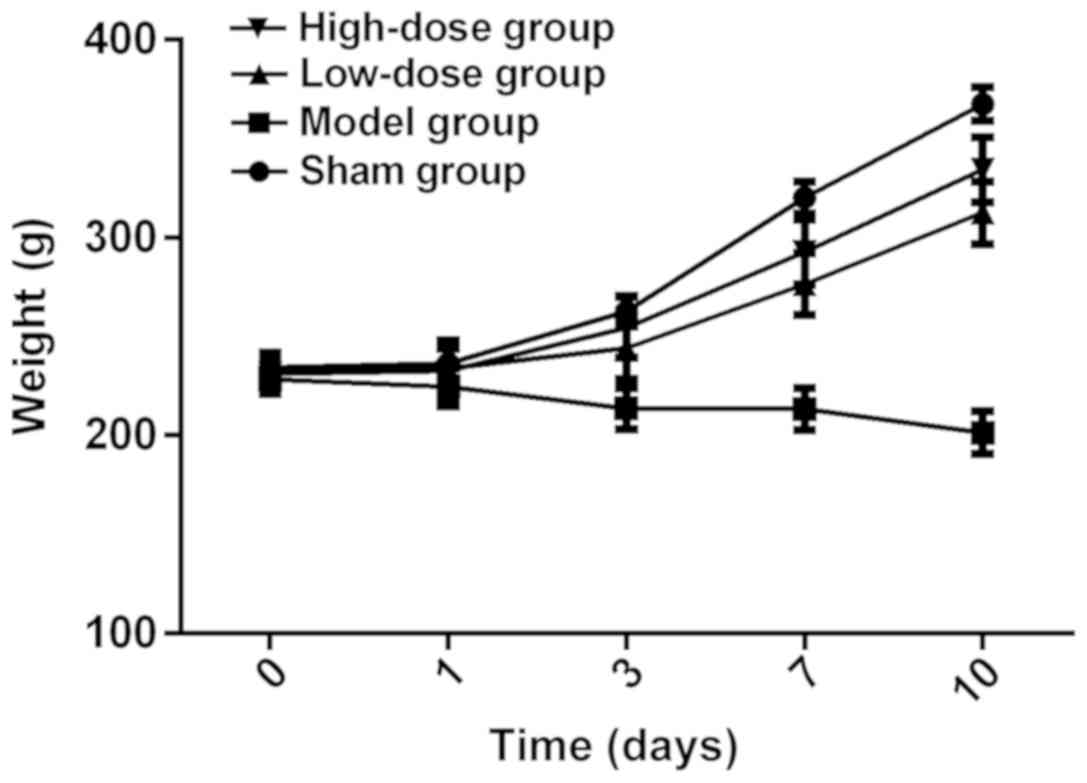
Changes in body weight of rats
There were no statistical differences in body weight
among the four groups of rats on the 0 and 1st day (P>0.05), but
there were statistical differences on the 3rd, 7th and 10th day
(P<0.05). On the 3rd, 7th and 10th day, the body weight was
lower in model group, low-dose group and high-dose group of rats
than that in control group (P<0.05). The difference was higher
in low-dose group and high-dose group of rats than that in model
group (P<0.05), and was higher in high-dose group of rats than
that in low-dose group (P<0.05). There were no statistical
difference in the body weight in the group on the 0 and 1st day in
the four groups of rats (P>0.05). From the 3rd day, the body
weight in control group, low-dose group and high-dose group of rats
began to continuously increase (P<0.05). In model group of rats,
the body weight was lower on the 3rd day than that on the 0 and 1st
day (P<0.05). There was no statistical difference on the 3rd,
7th and 10th day (P>0.05), which was lower than that on the 0
and 1st day (P<0.05; Table I and
Fig. 2).
 | Table I.Changes in body weight of rats. |
Table I.
Changes in body weight of rats.
| Day | Control group | Model group | Low-dose group | High-dose group | t | P-value |
|---|
| 0 | 234.28±7.65 | 228.47±7.58 | 232.64±7.72 | 231.15±7.42 | 1.056 | 0.380 |
| 1 | 236.36±7.46 | 224.56±9.62 | 233.75±14.43 | 232.68±15.35 | 1.752 | 0.174 |
| 3 | 262.73±7.68 | 213.69±10.43 | 244.13±15.39 | 254.47±15.41 | 28.634 | <0.001 |
| 7 | 320.12±8.33 | 212.33±10.69 | 276.42±15.58 | 292.68±16.49 | 117.462 | <0.001 |
| 10 | 367.49±8.64 | 201.48±10.72 | 312.57±15.84 | 334.37±16.56 | 289.855 | <0.001 |
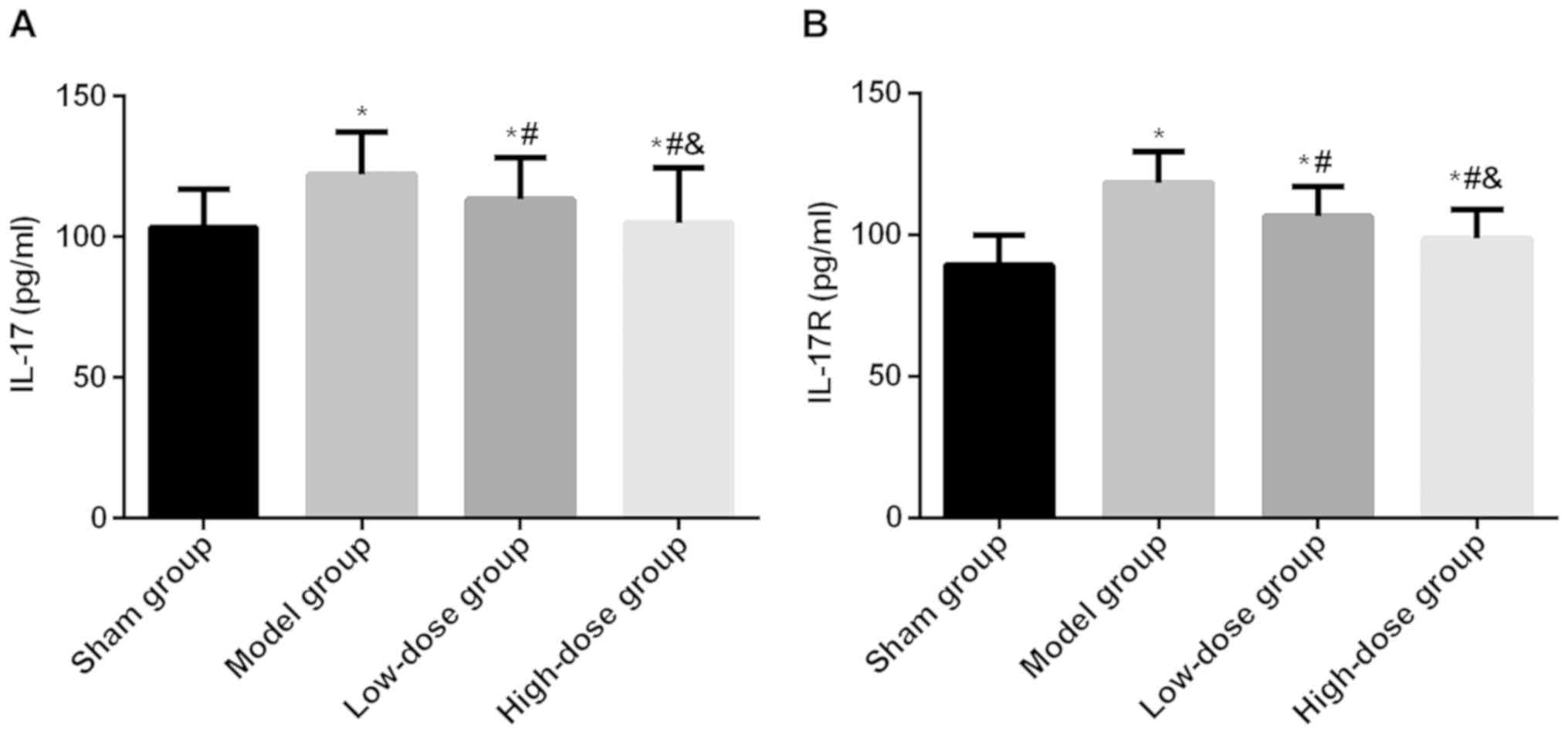
IL-17 and IL-17R levels
There were significant differences in IL-17 and
IL-17R levels among the four groups of rats (P<0.05). IL-17 and
IL-17R levels were significantly higher in model group, low-dose
group and high-dose group of rats than those in control group
(P<0.05), and were significantly lower in low-dose group and
high-dose group of rats than those in model group (P<0.05), and
were significantly lower in high-dose group of rats than those in
low-dose group (P<0.05; Fig.
3).
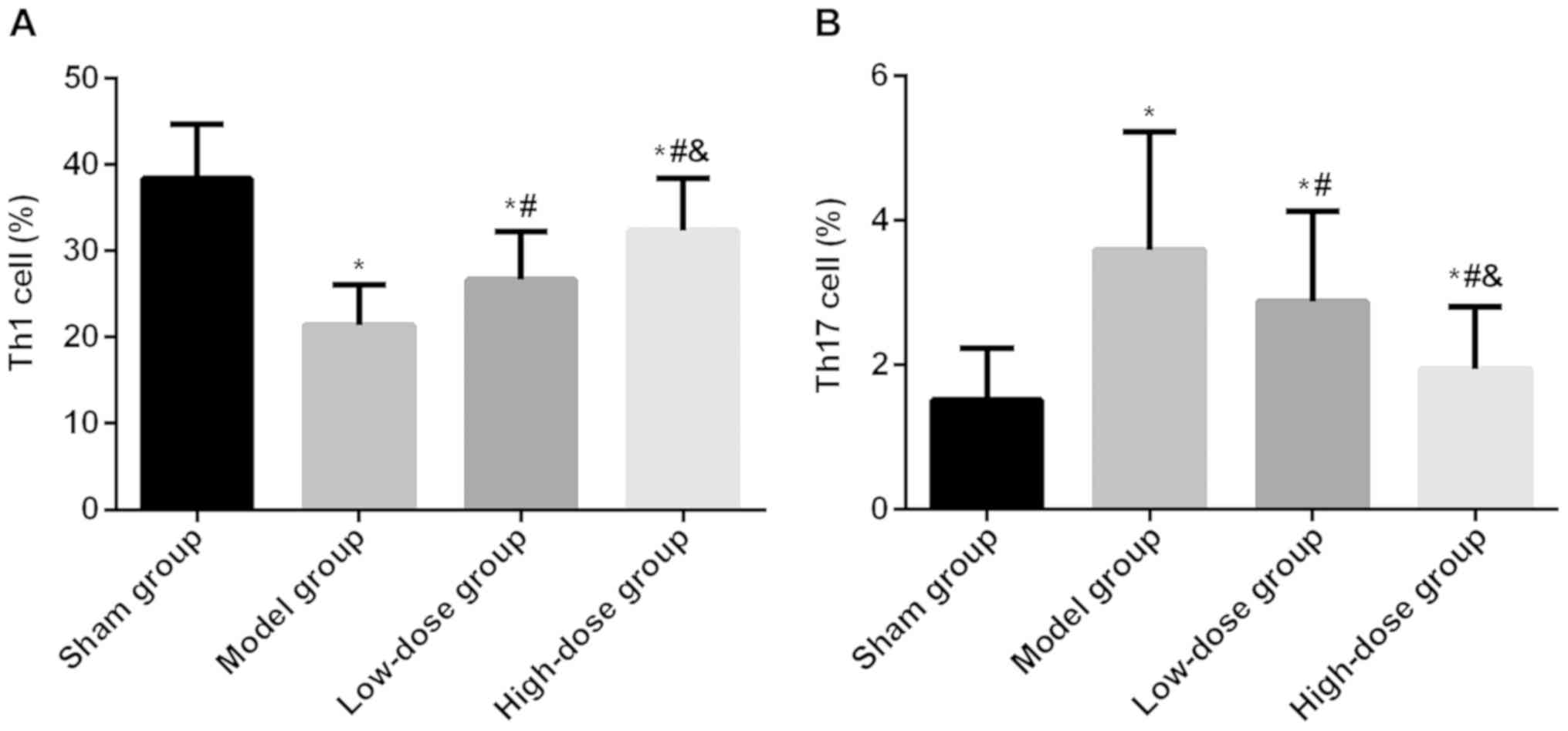
Th1 and Th17 cell levels
There were significant differences in Th1 and Th17
cell levels among the four groups of rats (P<0.05). Th1 cell
level was significantly lower in model group, low-dose group and
high-dose group of rats than that in control group (P<0.05), but
Th17 cell level was higher than that in control group (P<0.05).
Th1 cell level was significantly higher in low-dose group and
high-dose group of rats than that in model group (P<0.05), but
Th17 cell level was lower than that in model group (P<0.05). Th1
cell level was significantly higher in high-dose group of rats than
that in low-dose group (P<0.05), but Th17 cell level was lower
than that in low-dose group (Fig.
4).
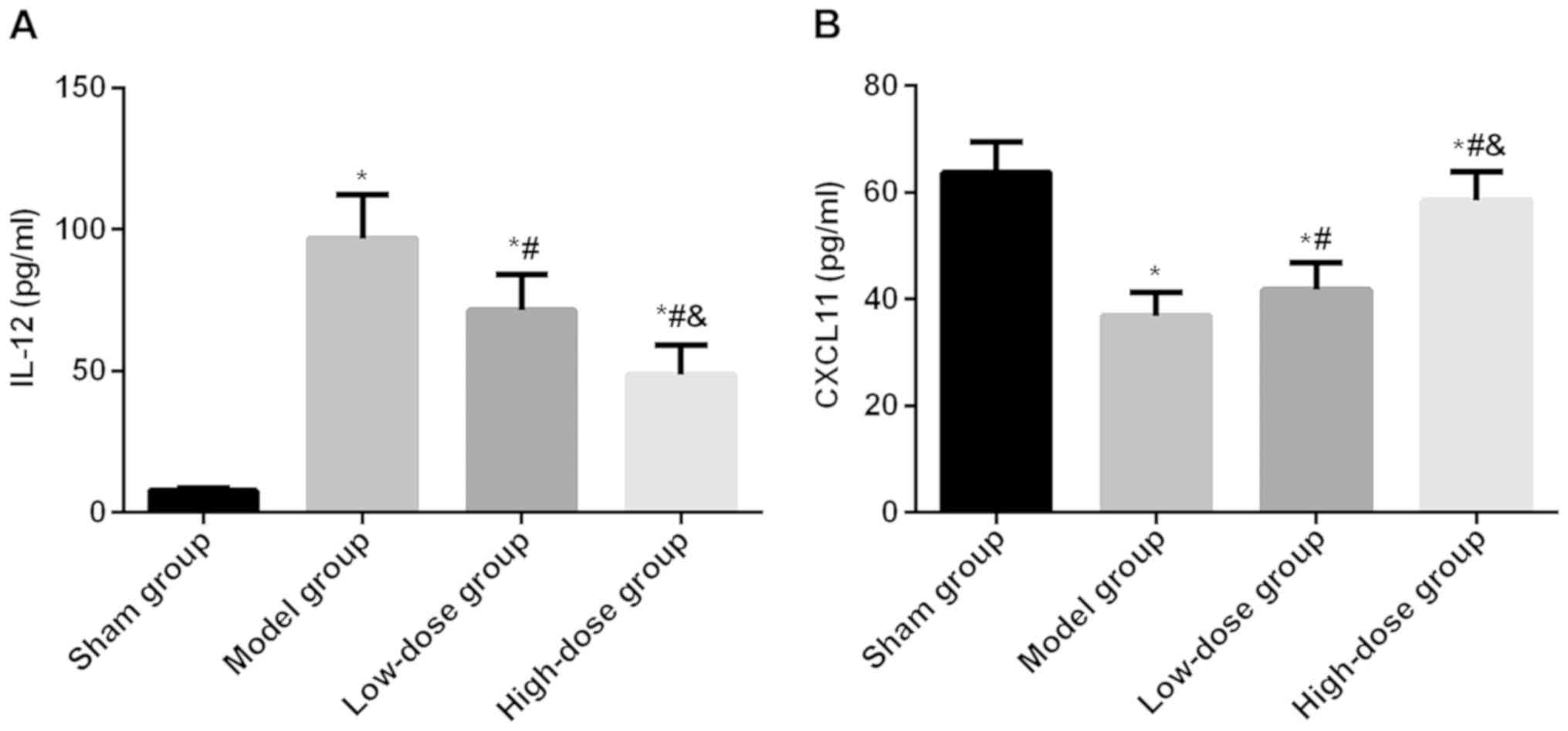
IL-12 and CXCL11 levels
There were significant differences in IL-12 and
CXCL11 levels among the four groups of rats (P<0.05). IL-12
levels were significantly higher in model group, lowdose group and
highdose group of rats than those in control group (P<0.05).
CXCL11 levels were significantly lower in model group, low-dose
group and high-dose group of rats than those in control group
(P<0.05). IL-12 levels were significantly lower in low-dose
group and high-dose group of rats than those in model group
(P<0.05). CXCL11 levels were significantly higher in lowdose
group and highdose group of rats than those in model group
(P<0.05). IL-12 level was significantly lower in highdose group
of rats than those in lowdose group (P<0.05). CXCL11 level was
significantly higher in highdose group of rats than those in
lowdose group (P<0.05; Fig.
5).
Discussion
Crohn's disease occurs mostly in developed
countries, with lower incidence in developing countries, but its
incidence is also rising with the development of economy (13). At present, Crohn's disease lacking
effective treatment cannot be completely cured, thus increasing
attention has been paid to it (3,4). Vitamin
D deficiency is common in patients with Crohn's disease, and
vitamin D supplementation can effectively improve their quality of
life and inflammatory response level (9,10).
Currently, the mechanism of action of vitamin D to alleviate the
symptoms of Crohn's disease is not completely clear. Few reports
exist on vitamin D and IL-17/IL-17R in Crohn's disease. Studies
have reported (14) that vitamin D
can reduce CD8+ cell level with positive IL-17
expression in psoriasis patients and improve their clinical
symptoms. It has also (15) been
reported that it can inhibit T cell proliferation, and reduce IL-17
level in inflammatory bowel disease and scleremus models. It is
hypothesized that vitamin D may exert its therapeutic effects on
Crohn's disease by acting on IL-17/IL-17R pathway.
In this study, the classical TNBS-induced Crohn's
disease was used to replicate the pathological model of rats. After
induction, rats in model group showed obvious symptoms of Crohn's
disease, such as diarrhea, bloody stool, significant decrease in
body weight, and increased disease activity index with the
increased number of stimulation, suggesting successful modeling in
the experiment. Patients with Crohn's disease also have
osteoporosis (16). For adult
patients with osteoporosis, the recommended daily supplemental dose
is 200 IU, and that of the elderly can be increased to 400–800 IU.
However, the American Endocrine Association guidelines suggest that
patients with Crohn's disease have a malabsorption of vitamin D, so
their daily supplemental dose should be more than 2–3 times
patients of the same age, with a recommended daily dose of
1,500–2,000 IU. Therefore, combined with experimental conditions,
the lowest dose of vitamin D was set to 1,750 IU, and the highest
dose to 7,500 IU in this experiment (17). The results of this study showed that
after the 1st day of treatment, low-dose group and high-dose group
of rats showed significant decrease in the disease activity index,
and the body weight began to increase when compared to model group.
High-dose group of rats showed more significant decrease and
increase when compared to low-dose group. It is indicated that the
condition of rats in low-dose group and high-dose group was
improved, while the body weight in model group of rats continued to
decrease. In related research reports, vitamin D is effective in
the treatment of Crohn's disease (9,10), and
the cyclic 25-hydroxy-vitamin D level is negatively correlated with
the degree of Crohn's disease (18).
Studies have reported that the oral high-dose of 10,000 IU of
vitamin D3 per day can significantly increase the serum
25-hydroxy-vitamin D level, reducing clinical recurrence rate.
Vitamin D3 is one of the manifestations of vitamin D in the human
body (10). These studies also
confirm our results, further affirming the therapeutic effects of
vitamin D on Crohn's disease.
In order to verify our hypothesis, IL-17, IL-17R,
IL-12 and CXCL11 levels in colon tissues, and Th1 cell and Th17
cell levels in the lamina propria of colon mucosa were analyzed.
IL-17 is the most representative in the IL-17 family. By binding to
IL-17R, it inhibits the increase of Th1 cell level, exerting
anti-inflammatory effects, and promotes the expression of Th17
cells and neutrophil chemotactic factors, exerting pro-inflammatory
effects. This is also one of the immune regulation mechanisms of
IL-17 (19,20). IL-12 is one of the most important
regulators of Th0 cells differentiating into Th1 cells (21), and CXCL11 is a chemokine of Th1 cells
(22). The results of this study
showed that after 10 days of administration, model group of rats
showed increased IL-17, IL-17R and Th17 levels in colon tissues,
but showed significantly increased IL-12 and decreased CXCL11
levels when compared to control group. Low-dose group and high-dose
group of rats showed significantly decreased IL-17, IL-17R and Th17
levels in colon tissues, but showed significantly decreased IL-12
and decreased CXCL11 levels when compared to model group. The
increase or decrease in high-dose group of rats was more
significant than that in low-dose group. The results validate the
inhibitory effects of IL-17 on Th1, which also confirm to some
extent our hypothesis. In Crohn's disease models, IL-17 can inhibit
the chemotaxis and differentiation of Th1 cells, which may break
Th1/Th2 cell balance, thereby leading to abnormal immune response
and colonic tissue damage (23).
Vitamin D can alleviate this breaking of balance, playing a
therapeutic role in Crohn's disease.
There are still some shortcomings in this study. At
present, there is no way to completely simulate the clinical
features of Crohn's disease. TNBS-induced rat models mainly cause
changes in Th1 cells, which may lead to some offset in the analysis
of result. Therefore, the results of this study still require more
animal models and large clinical data for further verification.
In summary, vitamin D can effectively treat Crohn's
disease, which may improve the chemotaxis and differentiation of
Th1 cells by inhibiting IL-17/IL-17R pathway, thereby improving
immune function and reducing the severity of disease.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YX wrote the manuscript. YX, JY and ZL observed and
scored the changes of rates after modeling. HC and HX detected
indicators. YW, TY and BW were responsible for statistical
analysis. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Luoyang Central Hospital Affiliated to Zhengzhou University
(Luoyang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chuang LS, Villaverde N, Hui KY, Mortha A,
Rahman A, Levine AP, Haritunians T, Evelyn Ng SM, Zhang W, Hsu NY,
et al: A frameshift in CSF2RB predominant among Ashkenazi jews
increases risk for Crohn's disease and reduces monocyte signaling
via GM-CSF. Gastroenterology. 151:710–723.e2. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ananthakrishnan AN, Huang H, Nguyen DD,
Sauk J, Yajnik V and Xavier RJ: Differential effect of genetic
burden on disease phenotypes in Crohn's disease and ulcerative
colitis: Analysis of a North American cohort. Am J Gastroenterol.
109:395–400. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gevers D, Kugathasan S, Denson LA,
Vázquez-Baeza Y, Van Treuren W, Ren B, Schwager E, Knights D, Song
SJ, Yassour M, et al: The treatment-naive microbiome in new-onset
Crohn's disease. Cell Host Microbe. 15:382–392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cleynen I, Boucher G, Jostins L, Schumm
LP, Zeissig S, Ahmad T, Andersen V, Andrews JM, Annese V, Brand S,
et al: International inflammatory bowel disease genetics
consortium: Inherited determinants of Crohn's disease and
ulcerative colitis phenotypes: A genetic association study. Lancet.
387:156–167. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Feagan BG, Sandborn WJ, Gasink C,
Jacobstein D, Lang Y, Friedman JR, Blank MA, Johanns J, Gao LL,
Miao Y, et al: UNITI–IM-UNITI Study Group: Ustekinumab as induction
and maintenance therapy for Crohn's disease. N Engl J Med.
375:1946–1960. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
De Cruz P, Kamm MA, Hamilton AL, Ritchie
KJ, Krejany EO, Gorelik A, Liew D, Prideaux L, Lawrance IC, Andrews
JM, et al: Crohn's disease management after intestinal resection: A
randomised trial. Lancet. 385:1406–1417. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Del Pinto R, Pietropaoli D, Chandar AK,
Ferri C and Cominelli F: Association between inflammatory bowel
disease and vitamin D deficiency: A systematic review and
meta-analysis. Inflamm Bowel Dis. 21:2708–2717. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Suibhne TN, Cox G, Healy M, O'Morain C and
O'Sullivan M: Vitamin D deficiency in Crohn's disease: Prevalence,
risk factors and supplement use in an outpatient setting. J Crohn's
Colitis. 6:182–188. 2012. View Article : Google Scholar
|
|
9
|
Raftery T, Martineau AR, Greiller CL,
Ghosh S, McNamara D, Bennett K, Meddings J and O'Sullivan M:
Effects of vitamin D supplementation on intestinal permeability,
cathelicidin and disease markers in Crohn's disease: Results from a
randomised double-blind placebo-controlled study. United European
Gastroenterol J. 3:294–302. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Narula N, Cooray M, Anglin R, Muqtadir Z,
Narula A and Marshall JK: Impact of high-dose vitamin D3
supplementation in patients with Crohn's disease in remission: A
pilot randomized double-blind controlled study. Dig Dis Sci.
62:448–455. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Monin L, Gudjonsson JE, Childs EE, Amatya
N, Xing X, Verma AH, Coleman BM, Garg AV, Killeen M, Mathers A, et
al: MCPIP1/regnase-1 restricts IL-17A- and IL-17C-dependent skin
inflammation. J Immunol. 198:767–775. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen K, Eddens T, Trevejo-Nunez G, Way EE,
Elsegeiny W, Ricks DM, Garg AV, Erb CJ, Bo M, Wang T, et al: IL-17
receptor signaling in the lung epithelium is required for mucosal
chemokine gradients and pulmonary host defense against K.
pneumoniae. Cell Host Microbe. 20:596–605. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Monteleone G, Neurath MF, Ardizzone S, Di
Sabatino A, Fantini MC, Castiglione F, Scribano ML, Armuzzi A,
Caprioli F, Sturniolo GC, et al: Mongersen, an oral SMAD7 antisense
oligonucleotide, and Crohn's disease. N Engl J Med. 372:1104–1113.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dyring-Andersen B, Bonefeld CM, Bzorek M,
Løvendorf MB, Lauritsen JP, Skov L and Geisler C: The Vitamin D
analogue calcipotriol reduces the frequency of CD8+
IL-17+ T cells in psoriasis lesions. Scand J Immunol.
82:84–91. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cantorna MT, Snyder L, Lin YD and Yang L:
Vitamin D and 1,25(OH)2D regulation of T cells. Nutrients.
7:3011–3021. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gomollón F, Dignass A, Annese V, Tilg H,
Van Assche G, Lindsay JO, Peyrin-Biroulet L, Cullen GJ, Daperno M,
Kucharzik T, et al: ECCO: 3rd European evidence-based consensus on
the diagnosis and management of Crohn's disease 2016: Part 1:
Diagnosis and medical management. J Crohn's Colitis. 11:3–25. 2017.
View Article : Google Scholar
|
|
17
|
Gharib H, Papini E, Garber JR, Duick DS,
Harrell RM, Hegedüs L, Paschke R, Valcavi R and Vitti P;
AACE/ACE/AME Task Force on Thyroid Nodules, : American Association
of Clinical Endocrinologists, American College of Endocrinology,
and Associazione Medici Endocrinologi Medical Guidelines for
Clinical Practice for the Diagnosis and Management of Thyroid
Nodules - 2016 Update. Endocr Pract. 22:622–639. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sadeghian M, Saneei P, Siassi F and
Esmaillzadeh A: Vitamin D status in relation to Crohn's disease:
Meta-analysis of observational studies. Nutrition. 32:505–514.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Maxwell JR, Zhang Y, Brown WA, Smith CL,
Byrne FR, Fiorino M, Stevens E, Bigler J, Davis JA, Rottman JB, et
al: Differential roles for interleukin-23 and interleukin-17 in
intestinal immunoregulation. Immunity. 43:739–750. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim J, Bissonnette R, Lee J, Correa da
Rosa J, Suárez-Fariñas M, Lowes MA and Krueger JG: The spectrum of
mild to severe psoriasis vulgaris is defined by a common activation
of IL-17 pathway genes, but with key differences in immune
regulatory genes. J Invest Dermatol. 136:2173–2182. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Marchant A, Amedei A, Azzurri A, Vekemans
J, Benagiano M, Tamburini C, Lienhardt C, Corrah T, McAdam KP,
Romagnani S, et al: Polarization of PPD-specific T-cell response of
patients with tuberculosis from Th0 to Th1 profile after successful
antimycobacterial therapy or in vitro conditioning with
interferon-alpha or interleukin-12. Am J Respir Cell Mol Biol.
24:187–194. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu Z, Wang M, Zhou S, Ma J, Shi Y, Peng
J, Hou M and Guo C: Pulsed high-dose dexamethasone modulates
Th1-/Th2-chemokine imbalance in immune thrombocytopenia. J Transl
Med. 14:3012016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Brand S: Crohn's disease: Th1, Th17 or
both? The change of a paradigm: new immunological and genetic
insights implicate Th17 cells in the pathogenesis of Crohn's
disease. Gut. 58:1152–1167. 2009. View Article : Google Scholar : PubMed/NCBI
|