Introduction
Osteosarcoma accounts for ~0.2% of human solid
malignant tumors. The age of onset is generally between 15 and 25
years old (1). Osteosarcoma is more
common in males compared with females and frequently occurs in the
metaphysis of long bones (1). Of
these, the distal and proximal femurs are the most common, followed
by the proximal fibula and other limb bones (1). Osteosarcoma may also occur in other
bone tissues, including the spine and upper femur (1). The growth invasiveness of osteosarcoma
can cause periosteal reaction, which forms a Codman triangle
(2). Patients with osteosarcoma are
prone to developing early lung metastasis (2). This may be one of the reasons for the
5-year survival rate of patients with osteosarcoma after amputation
of only 5–20% (2).
Osteosarcoma primarily occurs in young people. It
has a high malignancy grade and severely harms the health of young
patients (3). A large body of
research has deepened our understanding of osteosarcoma, but its
pathogenesis is quite complex (4).
It is associated with various genetic factors, including abnormal
activation, gene silencing and regulation of pathways (5). Recent research has also indicated that
miRNA and lncRNA are involved in the pathogenesis of osteosarcoma
(4).
The Human Genome Project was completed in 2003
(6), and the function of RNA in
biological processes has been increasingly emphasized (7). MicroRNA (miRNA) was rated as one of the
ten major breakthroughs in science and technology by Science
in 2002 and 2003 (8). It has become
a popular topic in the field of RNA research. At present, almost
1,400 miRNAs have been reported in biological species (8). These species include Drosophila
melanogaster, rodents, humans and plants. MiRNAs are closely
associated with tissue and organ development, cell proliferation,
differentiation and apoptosis. In addition, they are associated
with fat metabolism and other activities of animals and plants
(4).
Osteosarcoma is a vascular malignant tumor (9). Previous results have demonstrated that
vascular endothelial growth factor (VEGF) expression level is
associated with microvessel density and metastasis of osteosarcoma
(9). A previous study reported that
favorable conditions for the survival of malignant tumors are
associated with increased microvessel density in osteosarcoma
(10). VEGF is the most typical
angiogenic factor (10). It can
stimulate endothelial cell proliferation, migration and vascular
maturation (10). When VEGF is
combined with the VEGF receptor, a number of different signaling
pathways will be activated (10).
Furthermore, nitric oxide, phospholipase Cy and protein kinase C
will be released. This can promote angiogenesis (10). Cheng et al (11) observed that miR-638 inhibits cell
proliferation in human gastric carcinoma. The present study aimed
to investigate the function and mechanism of miRNA-638 in
osteosarcoma.
Materials and methods
Clinical samples
Serum (10 ml) of male osteosarcoma patients (n=6;
age, 51–64 years) and male healthy volunteers (n=6; age, 55–62
years) was collected at the Department of Physiology, Xuzhou
Medical University (Xuzhou, China) from Dec 2015 to Feb 2016 and
centrifuged at 8,000 × g for 10 min at 4°C. Serum samples were snap
frozen in liquid nitrogen immediately after resection and stored at
−80°C. The study protocol was approved by the Medical Ethics
Committee of the Xuzhou Hospital of Traditional Chinese Medicine.
Written informed consent was obtained from all participants for
their inclusion in the present study.
Cell lines and transfection
The human osteosarcoma cell line MG63 was purchased
from Shanghai Cell Bank of Chinese Academy of Sciences (Shanghai,
China) and grown in RPMI-1640 medium (Hyclone; GE Healthcare Life
Sciences, Logan, UT, USA) containing 10% fetal bovine serum (FBS;
Hyclone; GE Healthcare Life Sciences) at 37°C in a humidified
atmosphere of 5% CO2. MiR-638
(5′-GTGAGCGGGCGCGGCAGGGATCGCGGGCGG-3′), anti-miR-638
(5′-AGGCCGCCACCCGCCCGCGATCCCT-3′), negative control mimics
(5′-TGACTGTACTGAACTCGACTG-3′) and phospholipase D1 (PLD1) plasmids
were supplied by GenePharma Co., Ltd. (Shanghai, China). The MG63
cell line was plated in a 12-well plate and transfected with 100 nM
of miR-638, anti-miR-638, negative control mimics and PLD1 plasmid
using Lipofectamine 3000 (Thermo Fisher Scientific, Inc., Waltham,
MA, USA) and then incubated for 6 h.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from serum samples or MG63
cells using RNAiso reagent (Takara Bio, Inc., Otsu, Japan) and cDNA
was synthesized using the PrimeScript RT reagent kit (Takara Bio,
Inc.). qPCR was conducted to quantify relative mRNA expression
using SYBR Premix Ex Taq (Takara Bio, Inc.). The primers for
miR-638 were: Forward, 5′-GAGAGGATCCTGCCGCAGATCGCTG-3′ and reverse,
5′-GAGTAAGCTTCAGGGAGTCCTCTGCC-3′. The primers for U6 were: Forward,
5′-CTCGCTTCGGCAGCACA-3′ and reverse, 5′-AACGCTTCACGAATTTGCGT-3′.
The reactions were incubated at 95°C for 5 min, followed by 40
cycles of 95°C for 30 sec and 60°C for 30 sec. The
2−ΔΔCq method was used to analyze the relative
expression of target genes (12).
Cell proliferation assay
Cells (1×105) were plated in 96-well
culture plates following transfection for 6 h, and incubated for 0,
24, 48 and 72 h at 37°C. Cell proliferation was evaluated with Cell
Counting Kit-8 (Beyotime Institute of Biotechnology, Shanghai,
China) for 2 h, and examined by measuring absorbance at 450 nm.
Transwell invasion assay
Following transfection for 6 h, cells were plated in
24-well Transwell inserts coated with Matrigel (8-µm; BD
Biosciences, San Jose, CA, USA) for cell invasion assays. Cells
(1×105 cell/well) were plated in the upper chamber in
RPMI-1640 medium and the lower chamber contained RPMI-1640 medium
with 10% FBS. The cells on the upper chamber were removed using
cotton swabs following 48 h incubation. The cells on the lower
surface were fixed with 4% formaldehyde solution for 15 min at room
temperature and stained with hematoxylin for 5 min at room
temperature. Cells were observed using a light microscope and
analyzed using Image Lab 3.0 (Bio-Rad Laboratories, Inc., Hercules,
CA, USA).
Flow cytometry
After transfection for 48 h, cells were stained with
PBS containing propidium iodide (50 µg/ml)/Annexin V (BD
Biosciences) for 15 min in the dark at room temperature. The
percentage of apoptotic cells was measured using a BD FACSCalibur
system (FACScan; BD Biosciences) and analyzed using FlowJo version
7.6.1 (FlowJo LLC, Ashland, OR, USA).
Western blotting analysis
Protein was isolated from cells following 48 h of
transfection using radioimmunoprecipitation assay buffer (Beyotime
Institute of Biotechnology) and measured using the BCA method
(Beyotime Institute of Biotechnology). Proteins (50 µg) were then
subjected to 8–12% SDS-PAGE for separation before being transferred
onto a polyvinylidene membrane (EMD Millipore, Billerica, MA, USA).
The membrane was blocked with 5% nonfat milk for 1 h at 37°C and
incubated with antibodies against Bcl-2-associated X (Bax; cat. no.
5023), cyclin D1 (cat. no. 2978), PLD1 (cat. no. 3832), VEGF (cat.
no. 2463) (all dilution 1:2,000) and GAPDH (cat. no. 5174; dilution
1:5,000) (all Cell Signaling Technology, Inc., Danvers, MA, USA) at
4°C overnight. The membranes were subsequently incubated with a
goat anti-rabbit horseradish peroxidase secondary antibody (cat.
no. 7074; dilution 1:5,000; Cell Signaling Technology, Inc.) at 37
°C for 1 h and detected using enhanced chemiluminescence reagents
(Pierce; Thermo Fisher Scientific, Inc.), and Image-Pro Plus
software version 6.0 (Media Cybernetics, Inc., Rockville, MD,
USA).
Caspase-3 activity
Protein was isolated from cells following 48 h of
transfection as described above. A total of 10 µg protein was used
to measure the caspase-3 activity using a caspase-3 activity kit
(cat. no. C1116; Beyotime Institute of Biotechnology) and the
absorbance was measured at 405 nm.
Statistical analysis
Data are presented as the mean ± standard deviation
using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). Statistical
comparisons were performed using a Student's t-test or one-way
analysis of variance followed by Dunnett's test. Each experiment
was performed a minimum of three times. P<0.05 was considered to
indicate a statistically significant difference.
Results
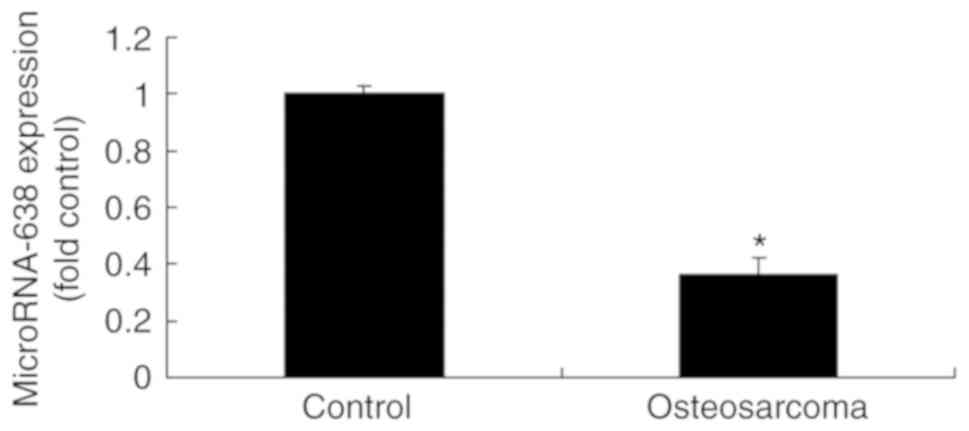
MiR-638 expression change in patients
with osteosarcoma
The expression of miR-638 was evaluated in the serum
of patients with osteosarcoma and normal controls. As indicated in
Fig. 1, the miR-638 serum level was
significantly decreased in patients with osteosarcoma compared with
the normal controls.
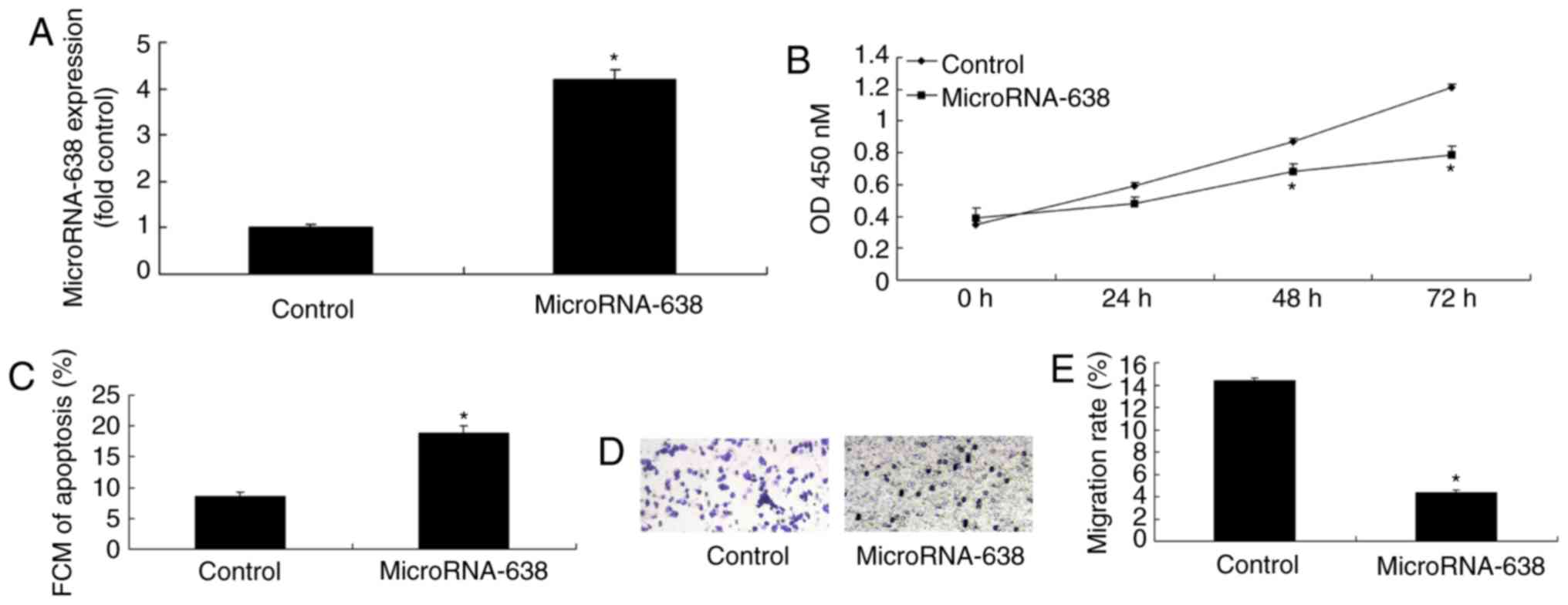
Overexpression of miR-638 induces
apoptosis, and inhibits cell proliferation and invasion of
osteosarcoma cells
In order to verify the function of miR-638 in
osteosarcoma, miR-638 expression was upregulated in osteosarcoma
cells using miR-638 mimics. As indicated in Fig. 2, miR-638 expression was significantly
upregulated in osteosarcoma cells transfected with miR-638 compared
with the control. In addition, overexpression of miR-638
significantly induced apoptosis, and significantly inhibited cell
proliferation (at 48 and 72 h) and invasion of osteosarcoma cells
compared with the control (Fig.
2).
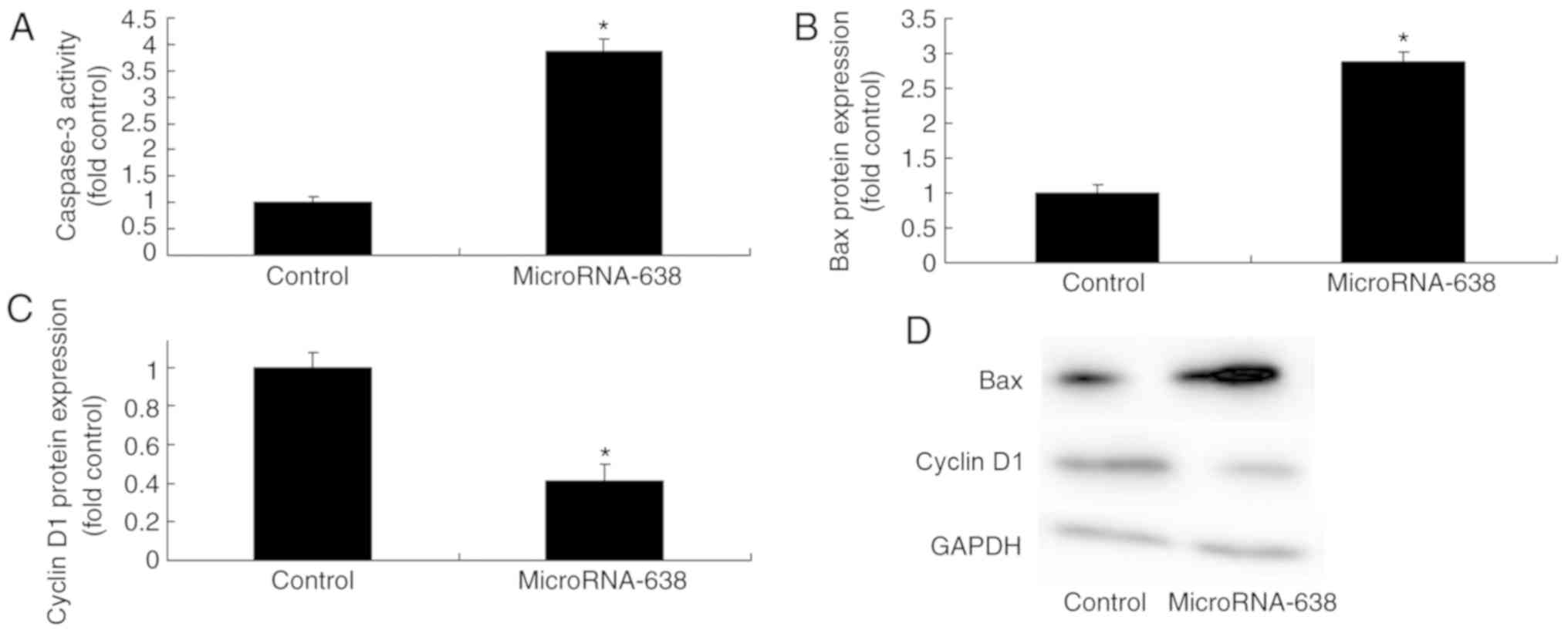
Overexpression of miR-638 affects Bax,
caspase-3 and cyclin D1 protein expression in osteosarcoma
cells
Overexpression of miR-638 significantly increased
caspase-3 activity and Bax protein expression, and significantly
decreased cyclin D1 protein expression in osteosarcoma cells
compared with the control group (Fig.
3).
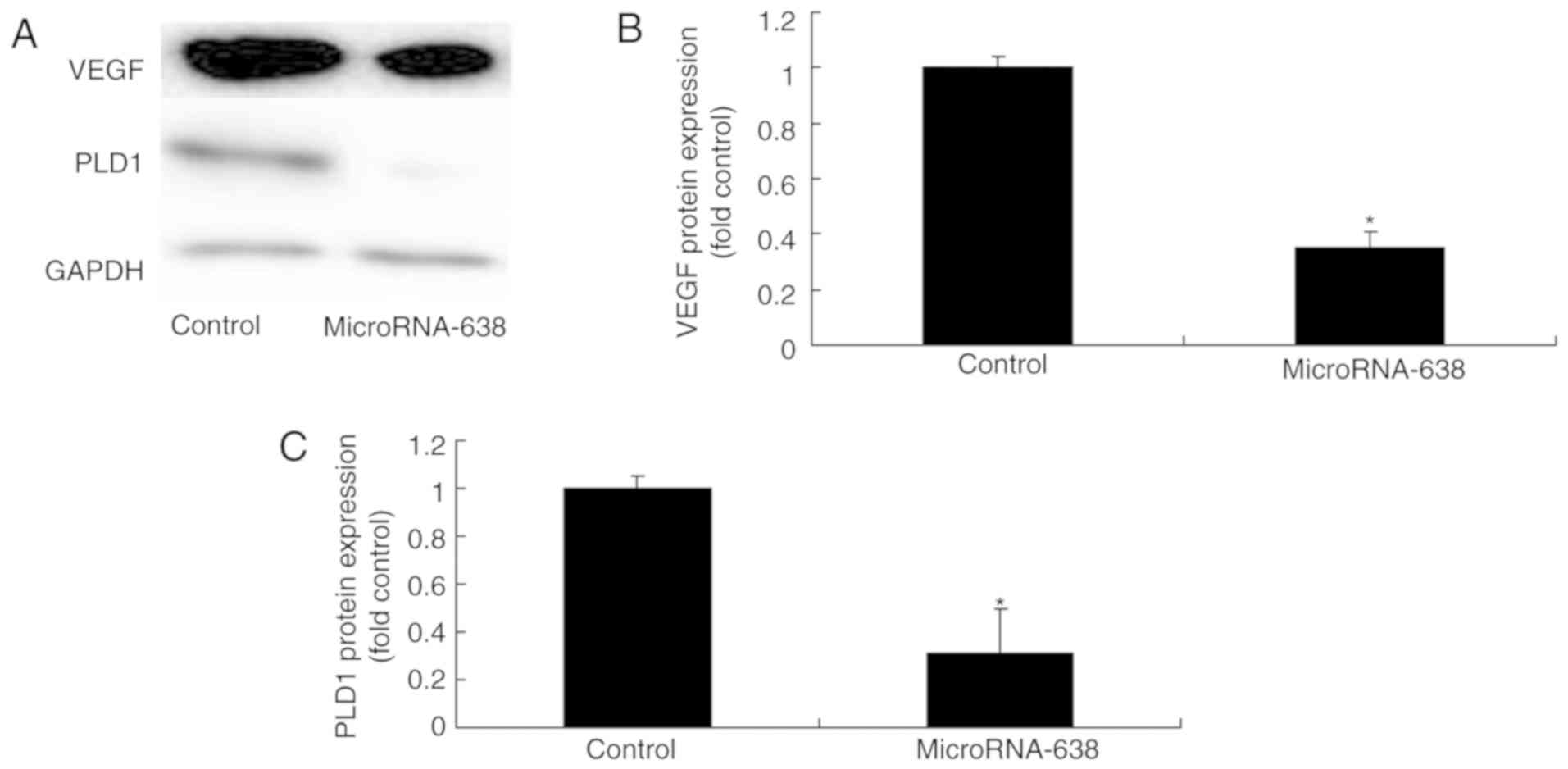
Overexpression of miR-638 affects PLD1
and VEGF protein expression of osteosarcoma
To elucidate the mechanism underlying
miR-638-mediated suppression of cell proliferation, PLD1 and VEGF
protein expression were measured using western blotting analysis.
The results demonstrated that overexpression of miR-638
significantly reduced PLD1 and VEGF protein expression in
osteosarcoma cells compared with the control group (Fig. 4).
Downregulation of miR-638 inhibits
apoptosis, and promotes cell growth and invasion of osteosarcoma
cells
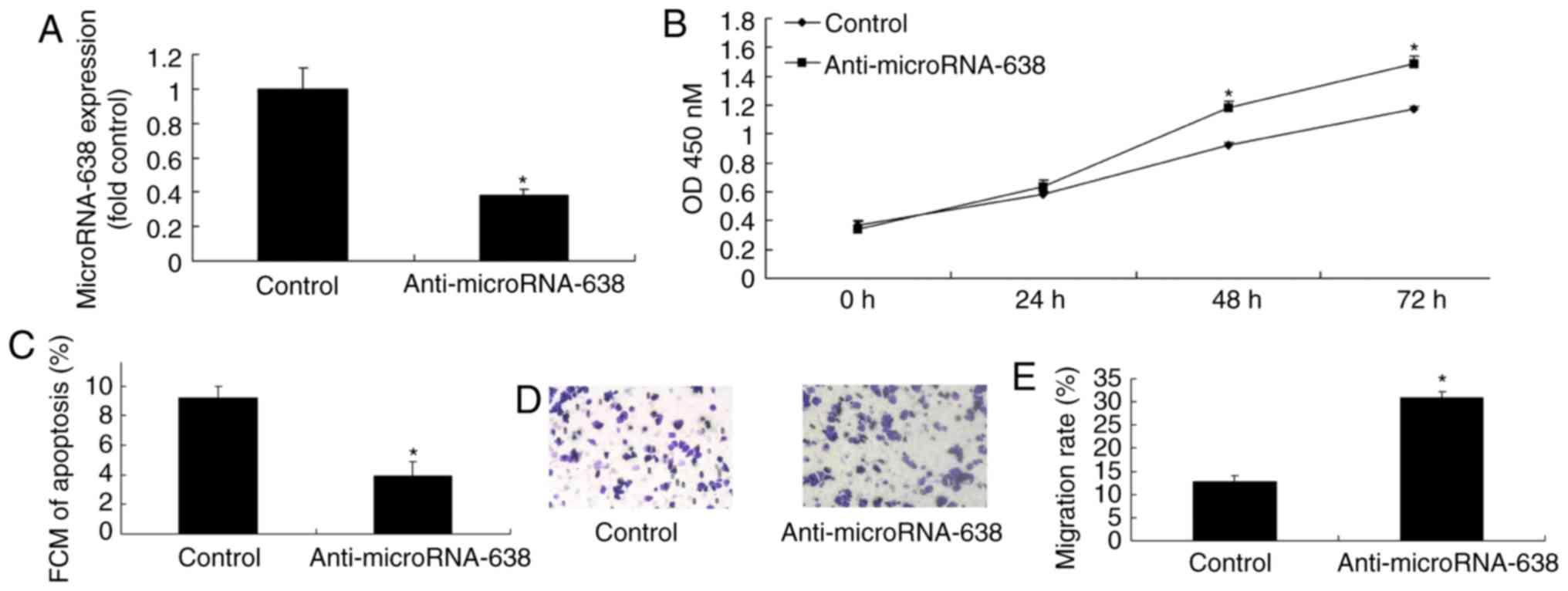
To further verify the function of miR-638 in
apoptosis of osteosarcoma cells, miR-638 expression was
downregulated using anti-miR-638 mimics. The expression of miR-638
was significantly lower in the anti-miR-638 group compared with the
control group. In addition, downregulation of miR-638 significantly
inhibited apoptosis, and significantly promoted cell proliferation
(at 48 and 72 h) and invasion of osteosarcoma cells compared with
the control (Fig. 5).
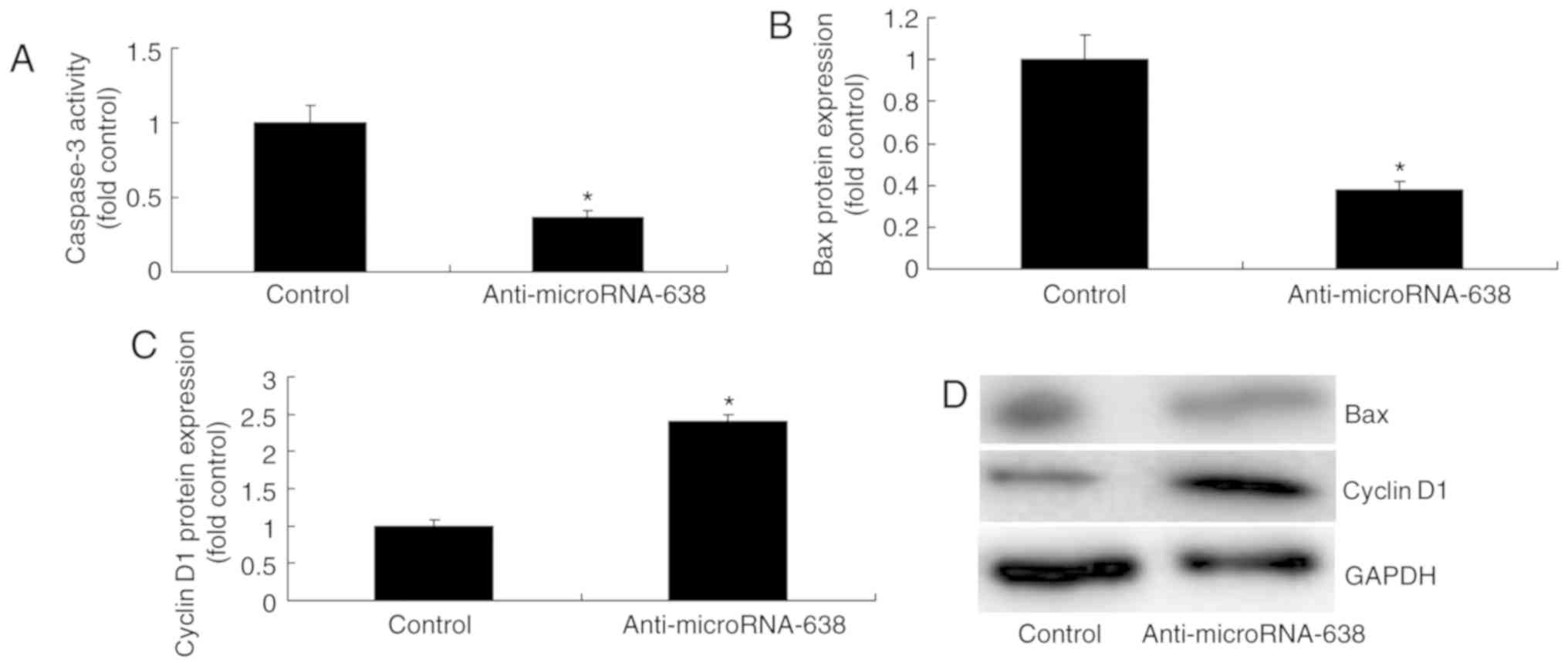
Downregulation of miR-638 affects
caspase-3 activity and Bax and cyclin D1 protein expression in
osteosarcoma cells
Downregulation of miR-638 significantly reduced
caspase-3 activity and Bax protein expression, and significantly
increased cyclin D1 protein expression in osteosarcoma cells
compared with the control group (Fig.
6).
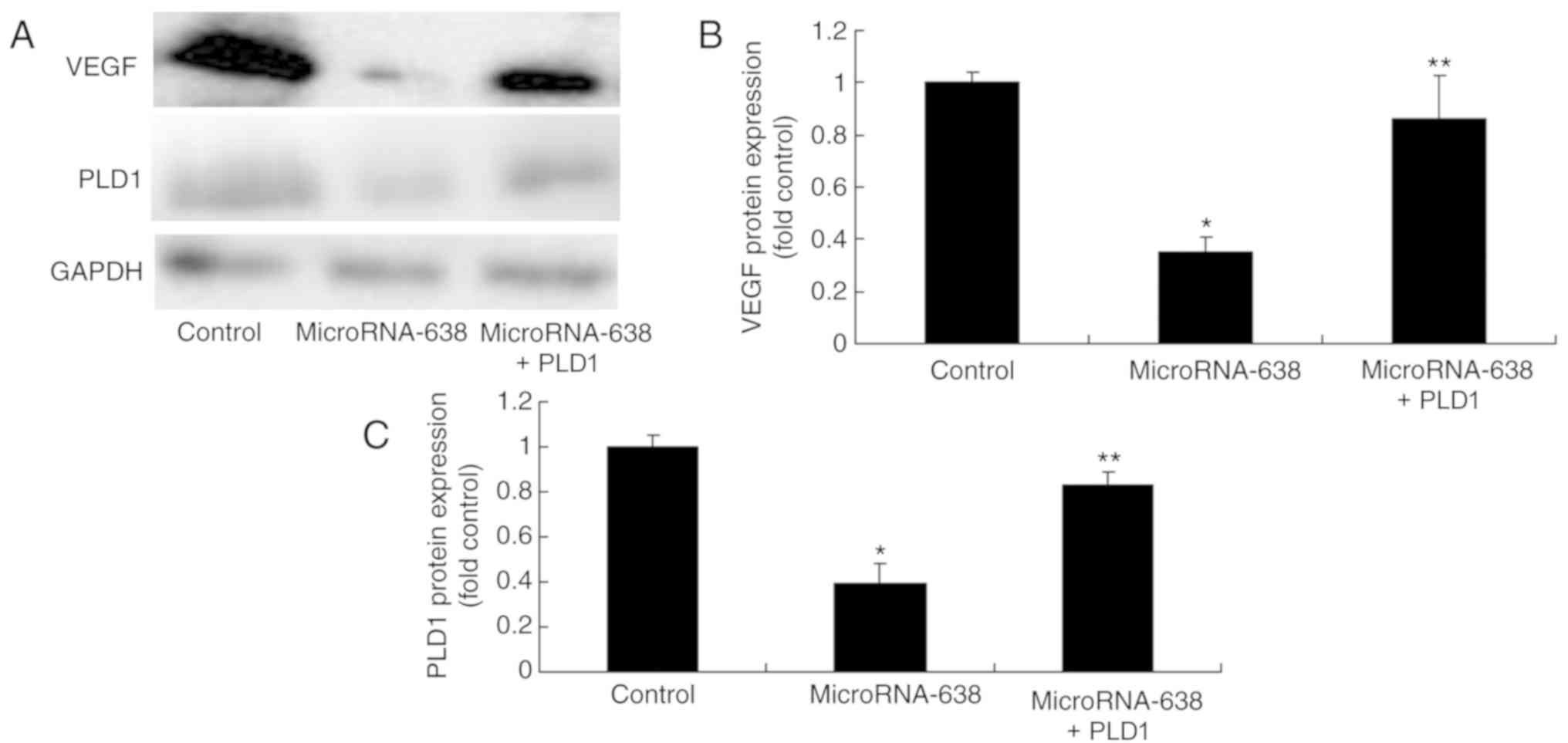
Downregulation of miR-638 affects PLD1
and VEGF protein expression in osteosarcoma cells
It was investigated whether miR-638 downregulation
affected PLD1 and VEGF protein expression in osteosarcoma cells.
Downregulation of miR-638 significantly increased PLD1 and VEGF
protein expression in osteosarcoma cells compared with the control
group (Fig. 7).
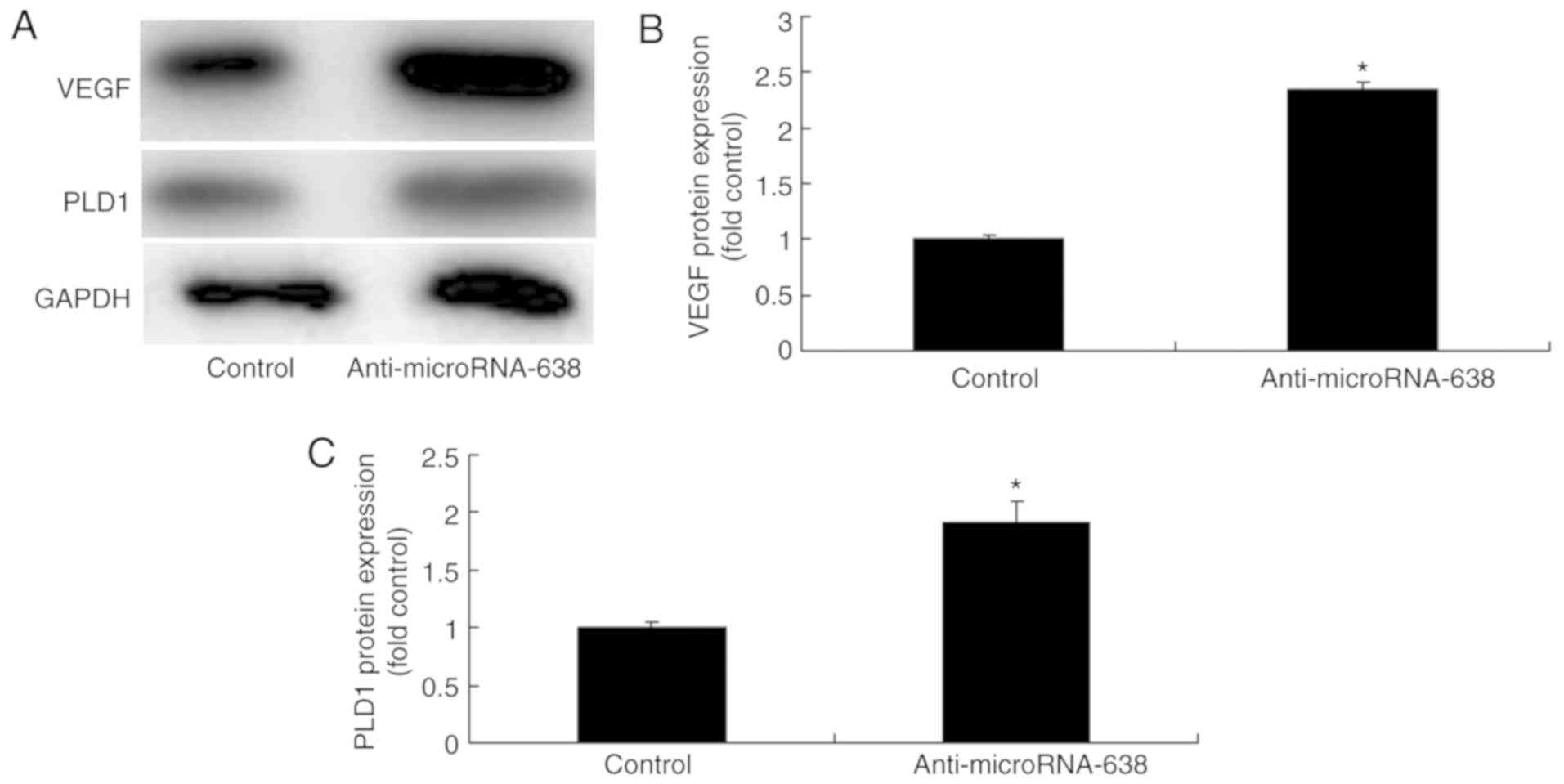
Promotion of PLD1 expression induces
PLD1 protein expression in osteosarcoma cells following
microRNA-638
In order to evaluate the association between miR-638
and PLD1 in human osteosarcoma, PLD1 expression was promoted using
PLD1 plasmids. As indicated in Fig.
8, PLD1 and VEGF protein expression were significantly
increased in osteosarcoma cells following promotion of microRNA-638
+ PLD1 as compared with the miR-638 group.
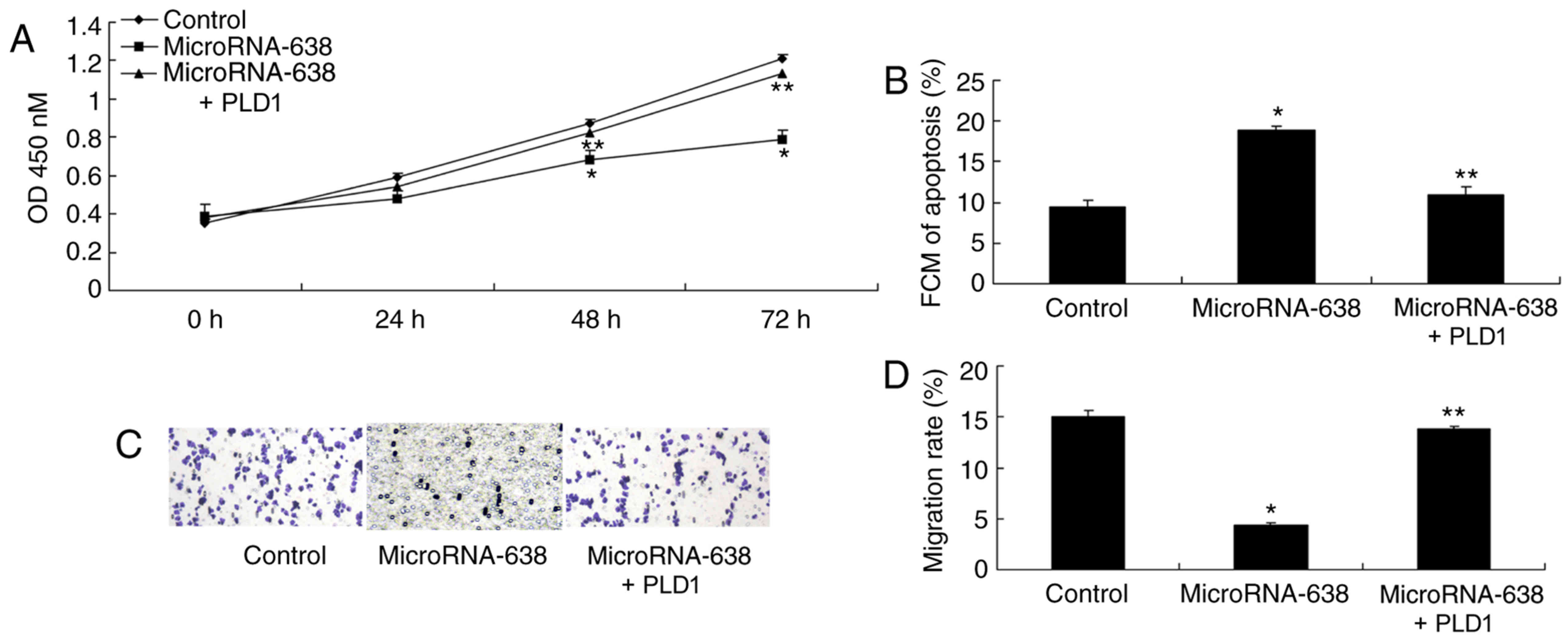
Promotion of PLD1 expression affects
cell apoptosis, cell growth and invasion of osteosarcoma cells
following miR-638 transfection
Promotion of PLD1 expression significantly increased
cell proliferation (at 48 and 72 h) and invasion, and significantly
reduced cell apoptosis of osteosarcoma cells following miR-638
transfection, as compared with the miR-638 group (Fig. 9).
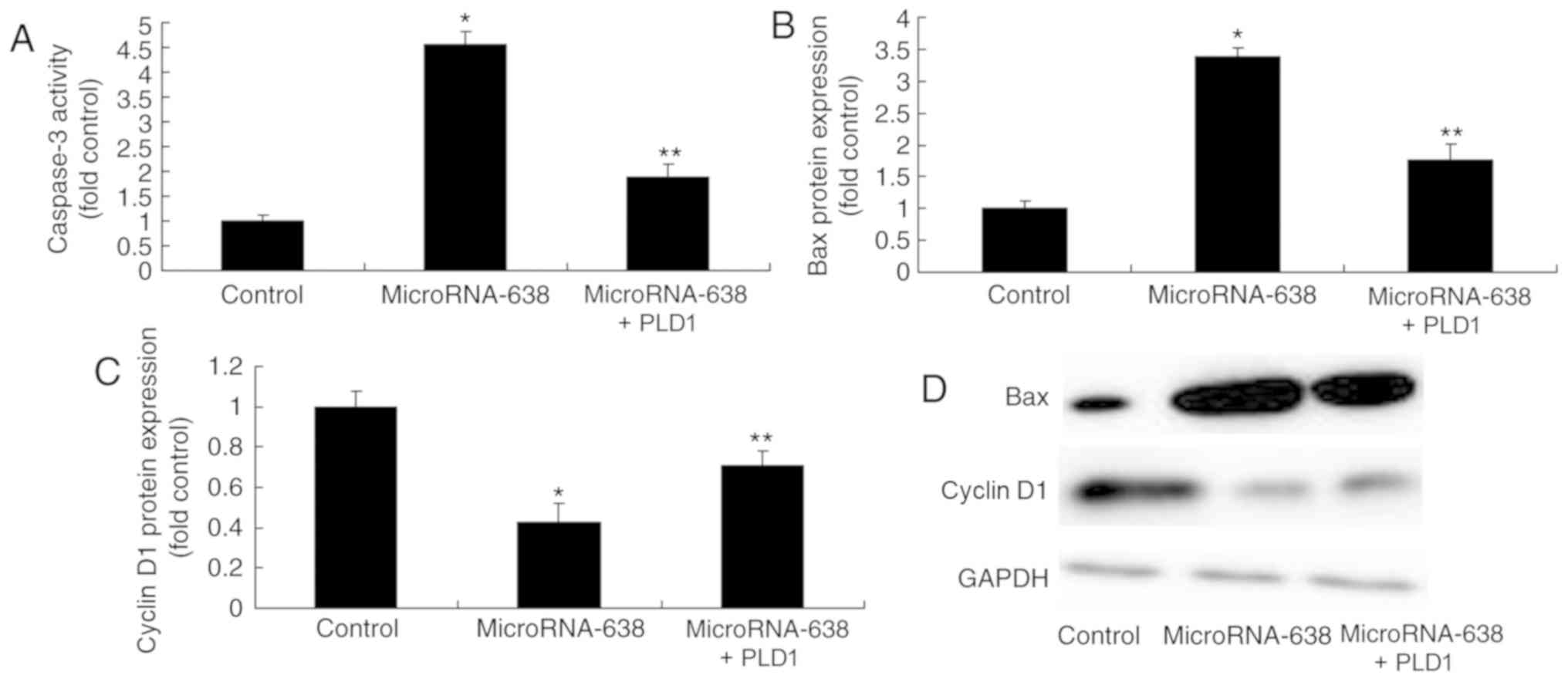
Promotion of PLD1 expression affects
caspase-3 activity and Bax and cyclin D1 protein expression in
osteosarcoma cells following miR-638 transfection
The promotion of PLD1 expression significantly
suppressed caspase-3 activity and Bax protein expression, and
significantly increased cyclin D1 protein expression in
osteosarcoma cells following miR-638 transfection, as compared with
the miR-638 group (Fig. 10).
Discussion
In recent years, the treatment of osteosarcoma has
developed in two aspects. One is the application of comprehensive
treatment based on neoadjuvant chemotherapy (13). The other is the development of limb
salvage surgery (13), which greatly
reduces amputation rate. In the future a surgery-based
comprehensive treatment of osteosarcoma should be adopted, which
includes surgery, chemotherapy and radiotherapy (14). Early diagnosis, careful preoperative
typing, and standardized treatment of osteosarcoma can
significantly improve the prognosis of osteosarcoma patients
(15).
In the present study, it was demonstrated that
miR-638 serum level was downregulated in patients with osteosarcoma
compared with the normal group. Cheng et al (11) observed that miR-638 inhibits cell
proliferation in human gastric carcinoma. However, in the present
study, only six samples were obtained, which was insufficient for
this type of investigation. A larger number of clinical samples
will be used in a future study.
Osteosarcoma is a type of vascular malignant tumor.
Previous research has indicated that VEGF expression level is
significantly correlated with microvessel density and metastasis of
osteosarcoma (10). However, there
is also research suggesting that the correlation may be attributed
to a large tumor being dependent on mature blood vessel
functionality (16). A previous
study reported that the beneficial survival conditions of
osteosarcoma were associated with increased microvessel density in
osteosarcoma (9). In the present
study, it was identified that miR-638 was downregulated in
osteosarcoma and in vitro studies indicated that this was
associated with increased protein expression of PLD1 and VEGF.
Cheng et al (11) identified
that the downregulation of miR-638 promotes angiogenesis and growth
by targeting VEGF in hepatocellular carcinoma. In the present
study, only an osteosarcoma cell line MG63 was used, which was
insufficient for this type of study. Additional osteosarcoma cell
lines will be used in future studies.
VEGF increased the activity of matrix
metalloproteinases (MMPs) and fibrinolytic enzymes and suppressed
VEGF degradation of the extracellular matrix by binding with MMPs
on the cell membrane (17). VEGF
also has an inductive effect on anti-apoptosis factors Bcl-2 and
survivin, which can induce the proliferation of vascular
endothelium (18). Abnormal
proliferation and uncontrolled differentiation of cells are the
basic pathological mechanisms of malignant tumors (19). It has been reported that the abnormal
proliferation and differentiation of cells are associated with
imbalances in the mechanism of apoptosis (18). Research has indicated that the Bcl-2
family serves a key function in regulating apoptosis (18). When the normal apoptosis mechanism is
disrupted, tumors may occur. Bcl-2 is an apoptosis suppressor gene
and also serves as an important proto-oncogene by acting on the
signal transduction pathway of apoptosis (18). Bcl-2 can inhibit cell apoptosis and
prolong the survival of cells. Thus, it creates an opportunity for
the development of tumors (5). Bcl-2
family proteins are divided into two types: Pro-apoptosis and
anti-apoptosis. Bax is a promoting apoptosis member, while Bcl-2 is
an anti-apoptosis member (5). Bcl-2
regulates apoptosis and further activates caspase signal cascades
by targeting cell mitochondria (5).
The present study indicated that the promotion of PLD1 decreased
the effects of miR-638 on osteosarcoma cell proliferation. MiR-638
may affect MMPs, particularly MMP-2 and −9, to influence invasion
activity. Thus, the protein expression of MMP-2 and −9 will be
investigated in future studies.
Cyclin D1 is a key molecule for cells to transform
from G1 phase to S phase (20).
siRNA targeting Cyclin D1 can interfere with the expression of
Cyclin D1 (21). This leads to tumor
cell arrest in G1 phase. Inhibition of Cyclin D1 expression can
change the distribution pattern of the cell cycle (21). The proportion of G0/1 phase
increases, S phase decreases and G1/S increases significantly,
indicating cell cycle arrest at G1/S. In the present study, it was
identified that overexpression of miR-638 suppressed cyclin D1
protein expression in osteosarcoma. Li et al (22) indicated that miR-638 inhibits cell
proliferation and migration through cyclin D1 expression.
In conclusion, the results of the current study
indicate that miR-638 may serve a function in tumor growth and
metastasis by suppressing osteosarcoma cell proliferation in an
in vitro model. The present study demonstrates the
importance of miR-638/PLD1/VEGF signaling in osteosarcoma
development.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Science Youth Foundation of China (grant no. 81500914).
Availability of data and materials
The analyzed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
BS designed the experiment. MX, JS, JC, JW, WQ, ND
and CS performed the experiments. BS and MX analyzed the data. BS
wrote the manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Medical
Ethics Committee of the Xuzhou Hospital of Traditional Chinese
Medicine and written informed consent was obtained from all
participants prior to their inclusion within the study.
Patient consent for publication
Written informed consent was obtained from all
participants for the publication of their data.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Morris CD, Teot LA, Bernstein ML, Marina
N, Krailo MD, Villaluna D, Janeway KA, DuBois SG, Gorlick RG and
Randall RL: Assessment of extent of surgical resection of primary
high-grade osteosarcoma by treating institutions: A report from the
children's oncology group. J Surg Oncol. 113:351–354. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nataraj V, Batra A, Rastogi S, Khan SA,
Sharma MC, Vishnubhatla S and Bakhshi S: Developing a prognostic
model for patients with localized osteosarcoma treated with uniform
chemotherapy protocol without high dose methotrexate: A
single-center experience of 237 patients. J Surg Oncol.
112:662–668. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xie L, Liao Y, Shen L, Hu F, Yu S, Zhou Y,
Zhang Y, Yang Y, Li D, Ren M, et al: Identification of the
miRNA-mRNA regulatory network of small cell osteosarcoma based on
RNA-seq. Oncotarget. 8:42525–42536. 2017.PubMed/NCBI
|
|
4
|
Fujiwara T, Uotani K, Yoshida A, Morita T,
Nezu Y, Kobayashi E, Yoshida A, Uehara T, Omori T, Sugiu K, et al:
Clinical significance of circulating miR-25-3p as a novel
diagnostic and prognostic biomarker in osteosarcoma. Oncotarget.
8:33375–33392. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gai P, Sun H, Wang G, Xu Q, Qi X, Zhang Z
and Jiang L: miR-22 promotes apoptosis of osteosarcoma cells via
inducing cell cycle arrest. Oncol Lett. 13:2354–2358. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang C, Long F, Wan J, Hu Y and He H:
MicroRNA-205 acts as a tumor suppressor in osteosarcoma via
targeting RUNX2. Oncol Rep. 35:3275–3284. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu M, Jin H, Xu CX, Sun B, Mao Z, Bi WZ
and Wang Y: miR-382 inhibits tumor growth and enhance
chemosensitivity in osteosarcoma. Oncotarget. 5:9472–9483. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dai N, Qing Y, Cun Y, Zhong Z, Li C, Zhang
S, Shan J, Yang X, Dai X, Cheng Y, et al: miR-513a-5p regulates
radiosensitivity of osteosarcoma by targeting human
apurinic/apyrimidinic endonuclease. Oncotarget. 9:25414–25426.
2016.PubMed/NCBI
|
|
9
|
He S, Xiao Z, Chen L and Xiong S: Comment
on Xu XW et al: Prognostic significance of VEGF expression
in osteosarcoma: A meta-analysis. Tumour Biol. 35:6193–6194. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ohba T, Cates JM, Cole HA, Slosky DA, Haro
H, Ando T, Schwartz HS and Schoenecker JG: Autocrine VEGF/VEGFR1
signaling in a subpopulation of cells associates with aggressive
osteosarcoma. Mol Cancer Res. 12:1100–1111. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheng J, Chen Y, Zhao P, Liu X, Dong J, Li
J, Huang C, Wu R and Lv Y: Downregulation of miRNA-638 promotes
angiogenesis and growth of hepatocellular carcinoma by targeting
VEGF. Oncotarget. 7:30702–30711. 2016.PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kudawara I, Aoki Y, Ueda T, Araki N, Naka
N, Nakanishi H, Matsumine A, Ieguchi M, Mori S, Myoui A, et al:
Neoadjuvant and adjuvant chemotherapy with high-dose ifosfamide,
doxorubicin, cisplatin and high-dose methotrexate in non-metastatic
osteosarcoma of the extremities: A phase II trial in Japan. J
Chemother. 25:41–48. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao J, Xu H, He M, Wang Z and Wu Y: Rho
GTPase-activating protein 35 rs1052667 polymorphism and
osteosarcoma risk and prognosis. Biomed Res Int. 2014:3969472014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grignani G, Palmerini E, Ferraresi V,
D'Ambrosio L, Bertulli R, Asaftei SD, Tamburini A, Pignochino Y,
Sangiolo D, Marchesi E, et al: Sorafenib and everolimus for
patients with unresectable high-grade osteosarcoma progressing
after standard treatment: A non-randomised phase 2 clinical trial.
Lancet Oncol. 16:98–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin CY, Tzeng HE, Li TM, Chen HT, Lee Y,
Yang YC, Wang SW, Yang WH and Tang CH: WISP-3 inhibition of miR-452
promotes VEGF-A expression in chondrosarcoma cells and induces
endothelial progenitor cells angiogenesis. Oncotarget.
8:39571–39581. 2017.PubMed/NCBI
|
|
17
|
Wang Z, Wen P, Luo X, Fang X, Wang Q, Ma F
and Lv J: Association of the vascular endothelial growth factor
(VEGF) gene single-nucleotide polymorphisms with osteosarcoma
susceptibility in a Chinese population. Tumour Biol. 35:3605–3610.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang C, Zhao Y and Zeng B: Enhanced
chemosensitivity by simultaneously inhibiting cell cycle
progression and promoting apoptosis of drug-resistant osteosarcoma
MG63/DXR cells by targeting Cyclin D1 and Bcl-2. Cancer Biomark.
12:155–167. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu Y, Zheng Q, Wu H, Guo X, Li J and Hao
S: Rapamycin increases pCREB, Bcl-2, and VEGF-A through ERK under
normoxia. Acta Biochim Biophys Sin (Shanghai). 45:259–267. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang J, Ni J, Yi S, Song D and Ding M:
Protein inhibitor of activated STAT xalpha depresses cyclin D and
cyclin D kinase, and contributes to the inhibition of osteosarcoma
cell progression. Mol Med Rep. 13:1645–1652. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wu J, Cui LL, Yuan J, Wang Y and Song S:
Clinical significance of the phosphorylation of MAPK and protein
expression of cyclin D1 in human osteosarcoma tissues. Mol Med Rep.
15:2303–2307. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li P, Liu Y, Yi B, Wang G, You X, Zhao X,
Summer R, Qin Y and Sun J: MicroRNA-638 is highly expressed in
human vascular smooth muscle cells and inhibits PDGF-BB-induced
cell proliferation and migration through targeting orphan nuclear
receptor NOR1. Cardiovasc Res. 99:185–193. 2013. View Article : Google Scholar : PubMed/NCBI
|