|
1
|
Wynn TA and Vannella KM: Macrophages in
tissue repair, regeneration, and fibrosis. Immunity. 44:450–462.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vannella KM and Wynn TA: Mechanisms of
organ injury and repair by macrophages. Annu Rev Physiol.
79:593–617. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Epelman S, Lavine KJ and Randolph GJ:
Origin and functions of tissue macrophages. Immunity. 41:21–35.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ginhoux F and Guilliams M: Tissue-resident
macrophage ontogeny and homeostasis. Immunity. 44:439–449. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gregory SH and Wing EJ: Neutrophil-Kupffer
cell interaction: A critical component of host defenses to systemic
bacterial infections. J Leukoc Biol. 72:239–248. 2002.PubMed/NCBI
|
|
6
|
Ganz T: Macrophages and systemic iron
homeostasis. J Innate Immun. 4:446–453. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schulz C, Gomez Perdiguero E, Chorro L,
Szabo-Rogers H, Cagnard N, Kierdorf K, Prinz M, Wu B, Jacobsen SE,
et al: A lineage of myeloid cells independent of Myb and
hematopoietic stem cells. Science. 336:86–90. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Davies LC, Jenkins SJ, Allen JE and Taylor
PR: Tissue-resident macrophages. Nat Immunol. 14:986–995. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Klein I, Cornejo JC, Polakos NK, John B,
Wuensch SA, Topham DJ, Pierce RH and Crispe IN: Kupffer cell
heterogeneity: Functional properties of bone marrow derived and
sessile hepatic macrophages. Blood. 110:4077–4085. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Murray PJ, Allen JE, Biswas SK, Fisher EA,
Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv LB, Lawrence
T, et al: Macrophage activation and polarization: Nomenclature and
experimental guidelines. Immunity. 41:14–20. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Stein M, Keshav S, Harris N and Gordon S:
Interleukin 4 potently enhances murine macrophage mannose receptor
activity: A marker of alternative immunologic macrophage
activation. J Exp Med. 176:287–292. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Laskin DL, Sunil VR, Gardner CR and Laskin
JD: Macrophages and tissue injury: Agents of defense or
destruction? Annu Rev Pharmacol Toxicol. 51:267–288. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martinez FO and Gordon S: The M1 and M2
paradigm of macrophage activation: Time for reassessment.
F1000Prime Rep. 6:132014. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
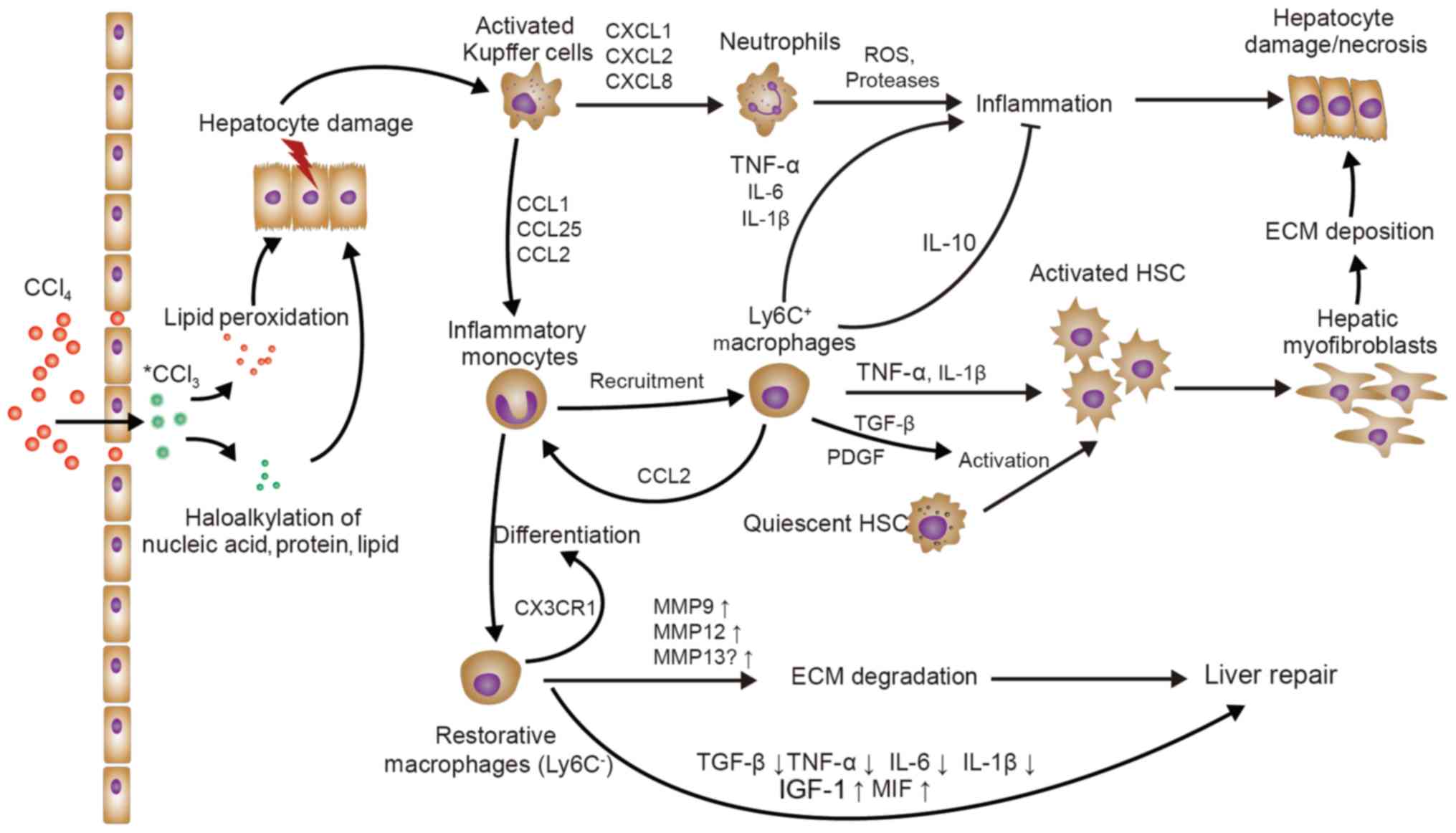
Weber LW, Boll M and Stampfl A:
Hepatotoxicity and mechanism of action of haloalkanes: Carbon
tetrachloride as a toxicological model. Crit Rev Toxicol.
33:105–136. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mehendale HM: Tissue repair: An important
determinant of final outcome of toxicant-induced injury. Toxicol
Pathol. 33:41–51. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tacke F: Functional role of intrahepatic
monocyte subsets for the progression of liver inflammation and
liver fibrosis in vivo. Fibrogenesis Tissue Repair. 5 (Suppl
1):S272012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karlmark KR, Weiskirchen R, Zimmermann HW,
Gassler N, Ginhoux F, Weber C, Merad M, Luedde T, Trautwein C and
Tacke F: Hepatic recruitment of the inflammatory Gr1+
monocyte subset upon liver injury promotes hepatic fibrosis.
Hepatology. 50:261–274. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Heymann F, Hammerich L, Storch D, Bartneck
M, Huss S, Russeler V, Gassler N, Lira SA, Luedde T, Trautwein C,
et al: Hepatic macrophage migration and differentiation critical
for liver fibrosis is mediated by the chemokine receptor C-C motif
chemokine receptor 8 in mice. Hepatology. 55:898–909. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Geissmann F, Manz MG, Jung S, Sieweke MH,
Merad M and Ley K: Development of monocytes, macrophages, and
dendritic cells. Science. 327:656–661. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Carlin LM, Stamatiades EG, Auffray C,
Hanna RN, Glover L, Vizcay-Barrena G, Hedrick CC, Cook HT, Diebold
S and Geissmann F: Nr4a1-dependent Ly6C(low) monocytes monitor
endothelial cells and orchestrate their disposal. Cell.
153:362–375. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mildner A, Schonheit J, Giladi A, David E,
Lara-Astiaso D, Lorenzo-Vivas E, Paul F, Chappell-Maor L, Priller
J, Leutz A, et al: Genomic characterization of murine monocytes
reveals C/EBPβ transcription factor dependence of Ly6C-Cells.
Immunity. 46:849–862 e847. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Duffield JS, Forbes SJ, Constandinou CM,
Clay S, Partolina M, Vuthoori S, Wu S, Lang R and Iredale JP:
Selective depletion of macrophages reveals distinct, opposing roles
during liver injury and repair. J Clin Invest. 115:56–65. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ramachandran P, Pellicoro A, Vernon MA,
Boulter L, Aucott RL, Ali A, Hartland SN, Snowdon VK, Cappon A,
Gordon-Walker TT, et al: Differential Ly-6C expression identifies
the recruited macrophage phenotype, which orchestrates the
regression of murine liver fibrosis. Proc Natl Acad Sci USA.
109:E3186–3195. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ma PF, Gao CC, Yi J, Zhao JL, Liang SQ,
Zhao Y, Ye YC, Bai J, Zheng QJ, Dou KF, et al: Cytotherapy with
M1-polarized macrophages ameliorates liver fibrosis by modulating
immune microenvironment in mice. J Hepatol. 67:770–779. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ramachandran P, Iredale JP and Fallowfield
JA: Resolution of liver fibrosis: Basic mechanisms and clinical
relevance. Semin Liver Dis. 35:119–131. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tacke F and Zimmermann HW: Macrophage
heterogeneity in liver injury and fibrosis. J Hepatol.
60:1090–1096. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wree A and Marra F: The inflammasome in
liver disease. J Hepatol. 65:1055–1056. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Weber LWD, Boll M and Stampfl A:
Hepatotoxicity and mechanism of action of haloalkanes: Carbon
tetrachloride as a toxicological model. Crit Rev Toxicol.
33:105–136. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marra F and Tacke F: Roles for chemokines
in liver disease. Gastroenterology. 147:577–594.e571. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nakamoto N, Ebinuma H, Kanai T, Chu PS,
Ono Y, Mikami Y, Ojiro K, Lipp M, Love PE, Saito H, et al:
CCR9+ macrophages are required for acute liver
inflammation in mouse models of hepatitis. Gastroenterology.
142:366–376. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chu PS, Nakamoto N, Ebinuma H, Usui S,
Saeki K, Matsumoto A, Mikami Y, Sugiyam K, Tomita K, Kanai T, et
al: C-C motif chemokine receptor 9 positive macrophages activate
hepatic stellate cells and promote liver fibrosis in mice.
Hepatology. 58:337–350. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hamidzadeh K, Christensen SM, Dalby E,
Chandrasekaran P and Mosser DM: Macrophages and the Recovery from
Acute and Chronic Inflammation. Annu Rev Physiol. 79:567–592. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zimmers TA, McKillop IH, Pierce RH, Yoo JY
and Koniaris LG: Massive liver growth in mice induced by systemic
interleukin 6 administration. Hepatology. 38:326–334. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Li Y, Schwabe RF, DeVries-Seimon T, Yao
PM, Gerbod-Giannone MC, Tall AR, Davis RJ, Flavell R, Brenner DA
and Tabas I: Free cholesterol-loaded macrophages are an abundant
source of tumor necrosis factor-alpha and interleukin-6: Model of
NF-kappaB- and map kinase-dependent inflammation in advanced
atherosclerosis. J Biol Chem. 280:21763–21772. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pradere JP, Kluwe J, De Minicis S, Jiao
JJ, Gwak GY, Dapito DH, Jang MK, Guenther ND, Mederacke I, Friedman
R, et al: Hepatic macrophages but not dendritic cells contribute to
liver fibrosis by promoting the survival of activated hepatic
stellate cells in mice. Hepatology. 58:1461–1473. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lotersztajn S, Julien B, Teixeira-Clerc F,
Grenard P and Mallat A: Hepatic fibrosis: Molecular mechanisms and
drug targets. Annu Rev Pharmacol Toxicol. 45:605–628. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Borkham-Kamphorst E, Kovalenko E, van
Roeyen CR, Gassler N, Bomble M, Ostendorf T, Floege J, Gressner AM
and Weiskirchen R: Platelet-derived growth factor isoform
expression in carbon tetrachloride-induced chronic liver injury.
Lab Invest. 88:1090–1100. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hao ZM, Fan XB, Li S, Lv YF, Su HQ, Jiang
HP and Li HH: Vaccination with Platelet-Derived Growth Factor B
Kinoids Inhibits CCl4-Induced Hepatic Fibrosis in Mice. J Pharmacol
Exp Ther. 342:835–842. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Perugorria MJ, Murphy LB, Fullard N,
Chakraborty JB, Vyrla D, Wilson CL, Oakley F, Mann J and Mann DA:
Tumor progression locus 2/Cot is required for activation of
extracellular regulated kinase in liver injury and toll-like
receptor-induced TIMP-1 gene transcription in hepatic stellate
cells in mice. Hepatology. 57:1238–1249. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Louis H, Van Laethem JL, Wu W, Quertinmont
E, Degraef C, Van den Berg K, Demols A, Goldman M, Le Moine O,
Geerts A and Devière J: Interleukin-10 controls neutrophilic
infiltration, hepatocyte proliferation, and liver fibrosis induced
by carbon tetrachloride in mice. Hepatology. 28:1607–1615. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Thompson K, Maltby J, Fallowfield J,
McAulay M, Millward-Sadler H and Sheron N: Interleukin-10
expression and function in experimental murine liver inflammation
and fibrosis. Hepatology. 28:1597–1606. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Fallowfield JA, Mizuno M, Kendall TJ,
Constandinou CM, Benyon RC, Duffield JS and Iredale JP:
Scar-associated macrophages are a major source of hepatic matrix
metalloproteinase-13 and facilitate the resolution of murine
hepatic fibrosis. J Immunol. 178:5288–5295. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wasmuth HE, Lammert F, Zaldivar MM,
Weiskirchen R, Hellerbrand C, Scholten D, Berres ML, Zimmermann H,
Streetz KL, Tacke F, et al: Antifibrotic effects of CXCL9 and its
receptor CXCR3 in livers of mice and humans. Gastroenterology.
137:309–319, 319 e301-303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Karlmark KR, Zimmermann HW, Roderburg C,
Gassler N, Wasmuth HE, Luedde T, Trautwein C and Tacke F: The
fractalkine receptor CX(3)CR1 protects against liver fibrosis by
controlling differentiation and survival of infiltrating hepatic
monocytes. Hepatology. 52:1769–1782. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Scott-Conner CE and Grogan JB: The
pathophysiology of biliary obstruction and its effect on phagocytic
and immune function. J Surg Res. 57:316–336. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lazar G, Paszt A, Kaszaki J, Duda E,
Szakacs J, Tiszlavicz L, Boros M, Balogh A and Lazar G: Kupffer
cell phagocytosis blockade decreases morbidity in endotoxemic rats
with obstructive jaundice. Inflamm Res. 51:511–518. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Faubion WA, Guicciardi ME, Miyoshi H,
Bronk SF, Roberts PJ, Svingen PA, Kaufmann SH and Gores GJ: Toxic
bile salts induce rodent hepatocyte apoptosis via direct activation
of Fas. J Clin Invest. 103:137–145. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Canbay A, Higuchi H, Bronk SF, Taniai M,
Sebo TJ and Gores GJ: Fas enhances fibrogenesis in the bile duct
ligated mouse: A link between apoptosis and fibrosis.
Gastroenterology. 123:1323–1330. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Canbay A, Feldstein AE, Higuchi H,
Werneburg N, Grambihler A, Bronk SF and Gores GJ: Kupffer cell
engulfment of apoptotic bodies stimulates death ligand and cytokine
expression. Hepatology. 38:1188–1198. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Gehring S, Dickson EM, San Martin ME, van
Rooijen N, Papa EF, Harty MW, Tracy TF Jr..Gregory SH: Kupffer
cells abrogate cholestatic liver injury in mice. Gastroenterology.
130:810–822. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Osawa Y, Seki E, Adachi M, Suetsugu A, Ito
H, Moriwaki H, Seishima M and Nagaki M: Role of acid
sphingomyelinase of kupffer cells in cholestatic liver injury in
mice. Hepatology. 51:237–245. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Seki E, De Minicis S, Osterreicher CH,
Kluwe J, Osawa Y, Brenner DA and Schwabe RF: TLR4 enhances TGF-beta
signaling and hepatic fibrosis. Nat Med. 13:1324–1332. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Meng F, Wang K, Aoyama T, Grivennikov SI,
Paik Y, Scholten D, Cong M, Iwaisako K, Liu X, Zhang M, et al:
Interleukin-17 Signaling in inflammatory, kupffer cells, and
hepatic stellate cells exacerbates liver fibrosis in mice.
Gastroenterology. 143:765–776.e3. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Steinman L: A brief history of T(H)17, the
first major revision in the T(H)1/T(H)2 hypothesis of T
cell-mediated tissue damage. Nat Med. 13:139–145. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ying HZ, Chen Q, Zhang WY, Zhang HH, Ma Y,
Zhang SZ, Fang J and Yu CH: PDGF signaling pathway in hepatic
fibrosis pathogenesis and therapeutics. Mol Med Report.
16:7879–7889. 2017. View Article : Google Scholar
|
|
56
|
Guillot A, Hamdaoui N, Bizy A, Zoltani K,
Souktani R, Zafrani ES, Mallat A, Lotersztajn S and Lafdil F:
Cannabinoid receptor 2 counteracts interleukin-17-induced immune
and fibrogenic responses in mouse liver. Hepatology. 59:296–306.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Popov Y, Sverdlov DY, Bhaskar KR, Sharma
AK, Millonig G, Patsenker E, Krahenbuhl S, Krahenbuhl L and
Schuppan D: Macrophage-mediated phagocytosis of apoptotic
cholangiocytes contributes to reversal of experimental biliary
fibrosis. Am J Physiol Gastrointest Liver Physiol. 298:G323–G334.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Chilakapati J, Shankar K, Korrapati MC,
Hill RA and Mehendale HM: Saturation toxicokinetics of
thioacetamide: Role in initiation of liver injury. Drug Metab
Dispos. 33:1877–1885. 2005.PubMed/NCBI
|
|
59
|
Kuramochi M, Izawa T, Pervin M, Bondoc A,
Kuwamura M and Yamate J: The kinetics of damage-associated
molecular patterns (DAMPs) and toll-like receptors during
thioacetamide-induced acute liver injury in rats. Exp Toxicol
Pathol. 68:471–477. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Erridge C: Endogenous ligands of TLR2 and
TLR4: Agonists or assistants? J Leukoc Biol. 87:989–999. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Fujisawa K, Miyoshi T, Tonomura Y, Izawa
T, Kuwamura M, Torii M and Yamate J: Relationship of heat shock
protein 25 with reactive macrophages in thioacetamide-induced rat
liver injury. Exp Toxicol Pathol. 63:599–605. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Andres D, Sanchez-Reus I, Bautista M and
Cascales M: Depletion of Kupffer cell function by gadolinium
chloride attenuates thioacetamide-induced hepatotoxicity-Expression
of metallothionein and HSP70. Biochem Pharmacol. 66:917–926. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Ide M, Kuwamura M, Kotani T, Sawamoto O
and Yamate J: Effects of gadolinium chloride (GdCl3) on the
appearance of macrophage populations and fibrogenesis in
thioacetamide-induced rat hepatic lesions. J Comp Pathol.
133:92–102. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Ide M, Yamate J, Machida Y, Nakanishi M,
Kuwamura M, Kotani T and Sawamoto O: Emergence of different
macrophage populations in hepatic fibrosis following
thioacetamide-induced acute hepatocyte injury in rats. J Comp
Pathol. 128:41–51. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Golbar HM, Izawa T, Wijesundera KK, Bondoc
A, Tennakoon AH, Kuwamura M and Yamate J: Depletion of hepatic
macrophages aggravates liver lesions induced in rats by
thioacetamide (TAA). Toxicol Pathol. 44:246–258. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
DiezFernandez C, Sanz N, Bosca L,
Hortelano S and Cascales M: Involvement of nitric oxide synthesis
in hepatic perturbations induced in rats by a necrogenic dose of
thioacetamide. Br J Pharmacol. 121:820–826. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Hernandez-Gea V, Ghiassi-Nejad Z,
Rozenfeld R, Gordon R, Fiel MI, Yue ZY, Czaja MJ and Friedman SL:
Autophagy releases lipid that promotes fibrogenesis by activated
hepatic stellate cells in mice and in human tissues.
Gastroenterology. 142:938–946. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Palacios RS, Roderfeld M, Hemmann S, Rath
T, Atanasova S, Tschuschner A, Gressner OA, Weiskirchen R, Graf J
and Roeb E: Activation of hepatic stellate cells is associated with
cytokine expression in thioacetamide-induced hepatic fibrosis in
mice. Lab Invest. 88:1192–1203. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Traber PG, Chou H, Zomer E, Hong F,
Klyosov A, Fiel MI and Friedman SL: Regression of fibrosis and
reversal of cirrhosis in rats by galectin inhibitors in
thioacetamide-induced liver disease. PLoS One. 8:e753612013.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Wijesundera KK, Izawa T, Tennakoon AH,
Murakami H, Golbar HM, Katou-Ichikawa C, Tanaka M, Kuwamura M and
Yamate J: M1- and M2-macrophage polarization in rat liver cirrhosis
induced by thioacetamide (TAA), focusing on Iba1 and galectin-3.
Exp Mol Pathol. 96:382–392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Yada A, Iimuro Y, Uyama N, Uda Y, Okada T
and Fujimoto J: Splenectomy attenuates murine liver fibrosis with
hypersplenism stimulating hepatic accumulation of Ly-6C(lo)
macrophages. J Hepatol. 63:905–916. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
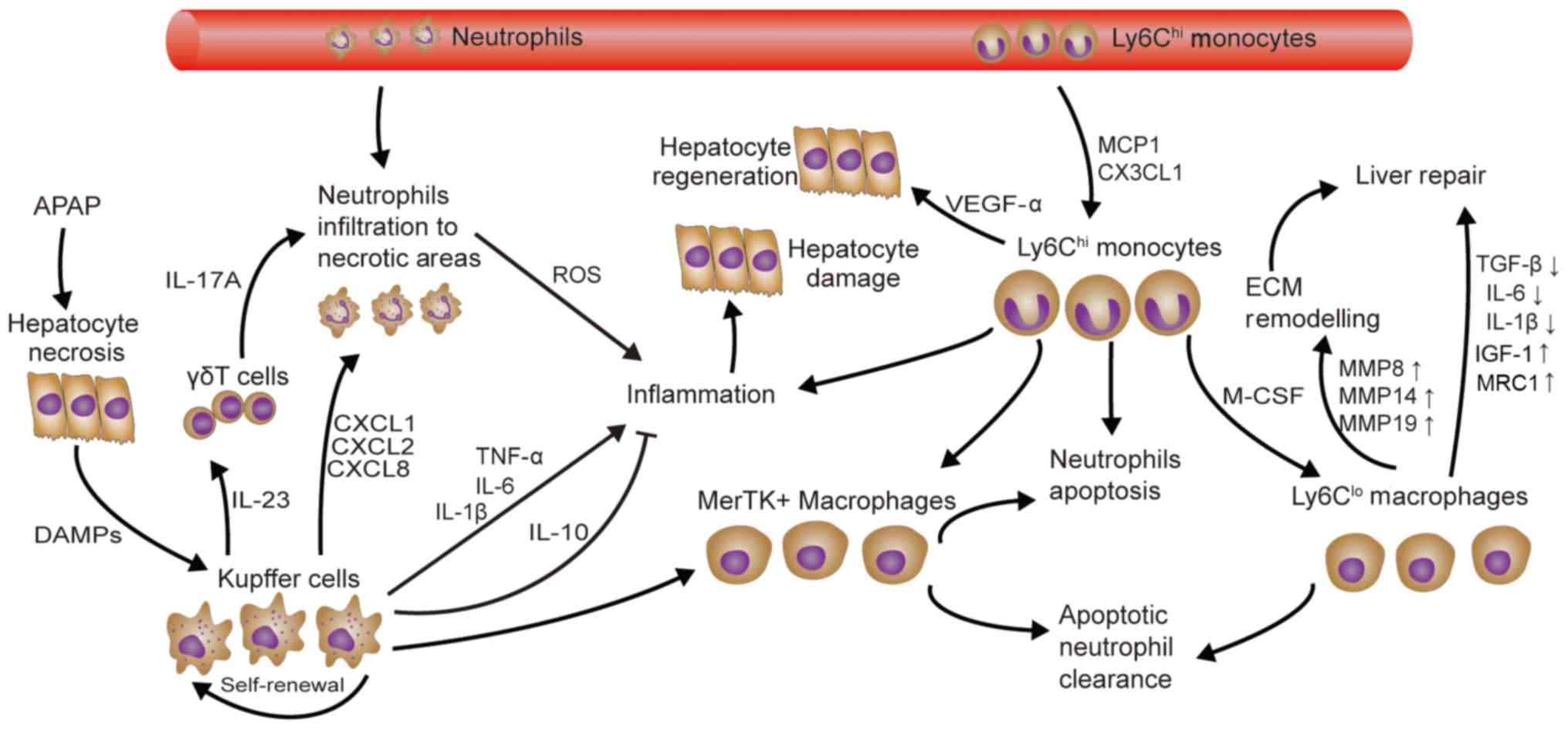
Jaeschke H and Bajt ML: Intracellular
signaling mechanisms of acetaminophen-induced liver cell death.
Toxicol Sci. 89:31–41. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Krenkel O, Mossanen Jana C and Tacke F:
Immune mechanisms in acetaminophen-induced acute liver failure.
Hepatobiliary Surgery and Nutrition. 3:331–343. 2014.PubMed/NCBI
|
|
74
|
Yang H, Hreggvidsdottir HS, Palmblad K,
Wang H, Ochani M, Li J, Lu B, Chavan S, Rosas-Ballina M, Al-Abed Y,
et al: A critical cysteine is required for HMGB1 binding to
Toll-like receptor 4 and activation of macrophage cytokine release.
Proc Natl Acad Sci USA. 107:11942–11947. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Wang X, Sun R, Wei H and Tian Z:
High-mobility group box 1 (HMGB1)-toll-like receptor
(TLR)4-interleukin (IL)-23-IL-17A axis in drug-induced
damage-associated lethal hepatitis: Interaction of γδ T cells with
macrophages. Hepatology. 57:373–384. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Marques PE, Amaral SS, Pires DA, Nogueira
LL, Soriani FM, Lima BH, Lopes GA, Russo RC, Avila TV, Melgaco JG,
et al: Chemokines and mitochondrial products activate neutrophils
to amplify organ injury during mouse acute liver failure.
Hepatology. 56:1971–1982. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Marques PE, Amaral SS, Pires DA, Nogueira
LL, Soriani FM, Lima BH, Lopes GA, Russo RC, Avila TV, Melgaco JG,
et al: Chemokines and mitochondrial products activate neutrophils
to amplify organ injury during mouse acute liver failure.
Hepatology. 56:1971–1982. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Williams CD, Bajt ML, Sharpe MR, McGill
MR, Farhood A and Jaeschke H: Neutrophil activation during
acetaminophen hepatotoxicity and repair in mice and humans. Toxicol
Appl Pharmacol. 275:122–133. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Jaeschke H, Williams CD, Ramachandran A
and Bajt ML: Acetaminophen hepatotoxicity and repair: The role of
sterile inflammation and innate immunity. Liver Int. 32:8–20. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Triantafyllou E, Pop OT, Possamai LA,
Wilhelm A, Liaskou E, Singanayagam A, Bernsmeier C, Khamri W, Petts
G, Dargue R, et al: MerTK expressing hepatic macrophages promote
the resolution of inflammation in acute liver failure. Gut.
67:333–347. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zigmond E, Samia-Grinberg S, Pasmanik-Chor
M, Brazowski E, Shibolet O, Halpern Z and Varol C: Infiltrating
monocyte-derived macrophages and resident kupffer cells display
different ontogeny and functions in acute liver injury. J Immunol.
193:344–353. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Mossanen JC, Krenkel O, Ergen C, Govaere
O, Liepelt A, Puengel T, Heymann F, Kalthoff S, Lefebvre E, Eulberg
D, et al: Chemokine (C-C motif) receptor 2-positive monocytes
aggravate the early phase of acetaminophen-induced acute liver
injury. Hepatology. 64:1667–1682. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Graubardt N, Vugman M, Mouhadeb O, Caliari
G, Pasmanik-Chor M, Reuveni D, Zigmond E, Brazowski E, David E,
Chappell-Maor L, et al: Ly6C(hi) monocytes and their macrophage
descendants regulate neutrophil function and clearance in
acetaminophen-induced liver injury. Front Immunol. 8:6262017.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Stachlewitz RF, Seabra V, Bradford B,
Bradham CA, Rusyn I, Germolec D and Thurman RG: Glycine and uridine
prevent D-galactosamine hepatotoxicity in the rat: Role of Kupffer
cells. Hepatology. 29:737–745. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Xiong QB, Hase K, Tezuka Y, Namba T and
Kadota S: Acteoside inhibits apoptosis in D-galactosamine and
lipopolysaccharide-induced liver injury. Life Sci. 65:421–430.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Galanos C, Freudenberg MA and Reutter W:
Galactosamine-induced sensitization to the lethal effects of
endotoxin. Proc Natl Acad Sci USA. 76:5939–5943. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Kitazawa T, Tsujimoto T, Kawaratani H,
Fujimoto M and Fukui H: Expression of Toll-like receptor 4 in
various organs in rats with D-galactosamine-induced acute hepatic
failure. J Gastroenterol Hepatol. 23:E494–E498. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ben Ari Z, Avlas O, Pappo O, Zilbermints
V, Cheporko Y, Bachmetov L, Zemel R, Shainberg A, Sharon E, Grief
F, et al: Reduced hepatic injury in toll-like receptor 4-deficient
mice following D-galactosamine/lipopolysaccharide-induced fulminant
hepatic failure. Cell Physiol Biochem. 29:41–50. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ilyas G, Zhao EP, Liu K, Lin Y, Tesfa L,
Tanaka KE and Czaja MJ: Macrophage autophagy limits acute toxic
liver injury in mice through down regulation of interleukin-1β. J
Hepatol. 64:118–127. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Li L, Duan CL, Zhao Y, Zhang XF, Yin HY,
Wang TX, Huang CX, Liu SH, Yang SY and Li XJ: Preventive effects of
interleukin-6 in lipopolysaccharide/D-galactosamine induced acute
liver injury via regulating inflammatory response in hepatic
macrophages. Int Immunopharmacol. 51:99–106. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Dejager L and Libert C: Tumor necrosis
factor alpha mediates the lethal hepatotoxic effects of poly(I:C)
in D-galactosamine-sensitized mice. Cytokine. 42:55–61. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Wolf AM, Wolf D, Rumpold H, Ludwiczek S,
Enrich B, Gastl G, Weiss G and Tilg H: The kinase inhibitor
imatinib mesylate inhibits TNF-alpha production in vitro and
prevents TNF-dependent acute hepatic inflammation. Proc Natl Acad
Sci USA. 102:13622–13627. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Jiang W, Sun R, Wei HM and Tian ZG:
Toll-like receptor 3 ligand attenuates LPS-induced liver injury by
down-regulation of toll-like receptor 4 expression on macrophages.
Proc Natl Acad Sci USA. 102:17077–17082. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zheng XF, Hu XY, Ma B, Fang H, Zhang F,
Mao YF, Yang FY, Xiao SC and Xia ZF: Interleukin-35 attenuates
D-galactosamine/lipopolysaccharide-induced liver injury via
enhancing interleukin-10 production in kupffer cells. Front
Pharmacol. 9:9592018. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lu L, Zhou HM, Ni M, Wang XH, Busuttil R,
Kupiec-Weglinski J and Zhai Y: Innate immune regulations and liver
ischemia-reperfusion injury. Transplantation. 100:2601–2610. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Tsung A, Sahai R, Tanaka H, Nakao A, Fink
MP, Lotze MT, Yang H, Li J, Tracey KJ, Geller DA, et al: The
nuclear factor HMGB1 mediates hepatic injury after murine liver
ischemia-reperfusion. J Exp Med. 201:1135–1143. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Mosher B, Dean R, Harkema J, Remick D,
Palma J and Crockett E: Inhibition of Kupffer cells reduced CXC
chemokine production and liver injury. J Surg Res. 99:201–210.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Jiang W, Tang W, Geng Q and Xu X:
Inhibition of toll-like receptor 4 with vasoactive intestinal
peptide attenuates liver ischemia-reperfusion injury. Transplant
Proc. 43:1462–1467. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Devey L, Ferenbach D, Mohr E, Sangster K,
Bellamy CO, Hughes J and Wigmore SJ: Tissue-resident macrophages
protect the liver from ischemia reperfusion injury via a heme
oxygenase-1-dependent mechanism. Mol Ther. 17:65–72. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Ellett JD, Atkinson C, Evans ZP, Amani Z,
Balish E, Schmidt MG, van Rooijen N, Schnellmann RG and Chavin KD:
Murine Kupffer cells are protective in total hepatic
ischemia/reperfusion injury with bowel congestion through IL-10. J
Immunol. 184:5849–5858. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Ke B, Shen XD, Gao F, Ji HF, Qiao B, Zhai
Y, Farmer DG, Busuttil RW and Kupiec-Weglinski JW: Adoptive
transfer of Ex Vivo HO-1 modified bone marrow-derived macrophages
prevents liver ischemia and reperfusion injury. Mol Ther.
18:1019–1025. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ke B, Shen XD, Ji H, Kamo N, Gao F,
Freitas MC, Busuttil RW and Kupiec-Weglinski JW: HO-1-STAT3 axis in
mouse liver ischemia/reperfusion injury: Regulation of TLR4 innate
responses through PI3K/PTEN signaling. J Hepatol. 56:359–366. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Ji H, Shen X, Gao F, Ke B, Freitas MC,
Uchida Y, Busuttil RW, Zhai Y and Kupiec-Weglinski JW: Programmed
death-1/B7-H1 negative costimulation protects mouse liver against
ischemia and reperfusion injury. Hepatology. 52:1380–1389. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Devisscher L, Verhelst X, Colle I, Van
Vlierberghe H and Geerts A: The role of macrophages in
obesity-driven chronic liver disease. J Leukoc Biol. 99:693–698.
2016. View Article : Google Scholar : PubMed/NCBI
|
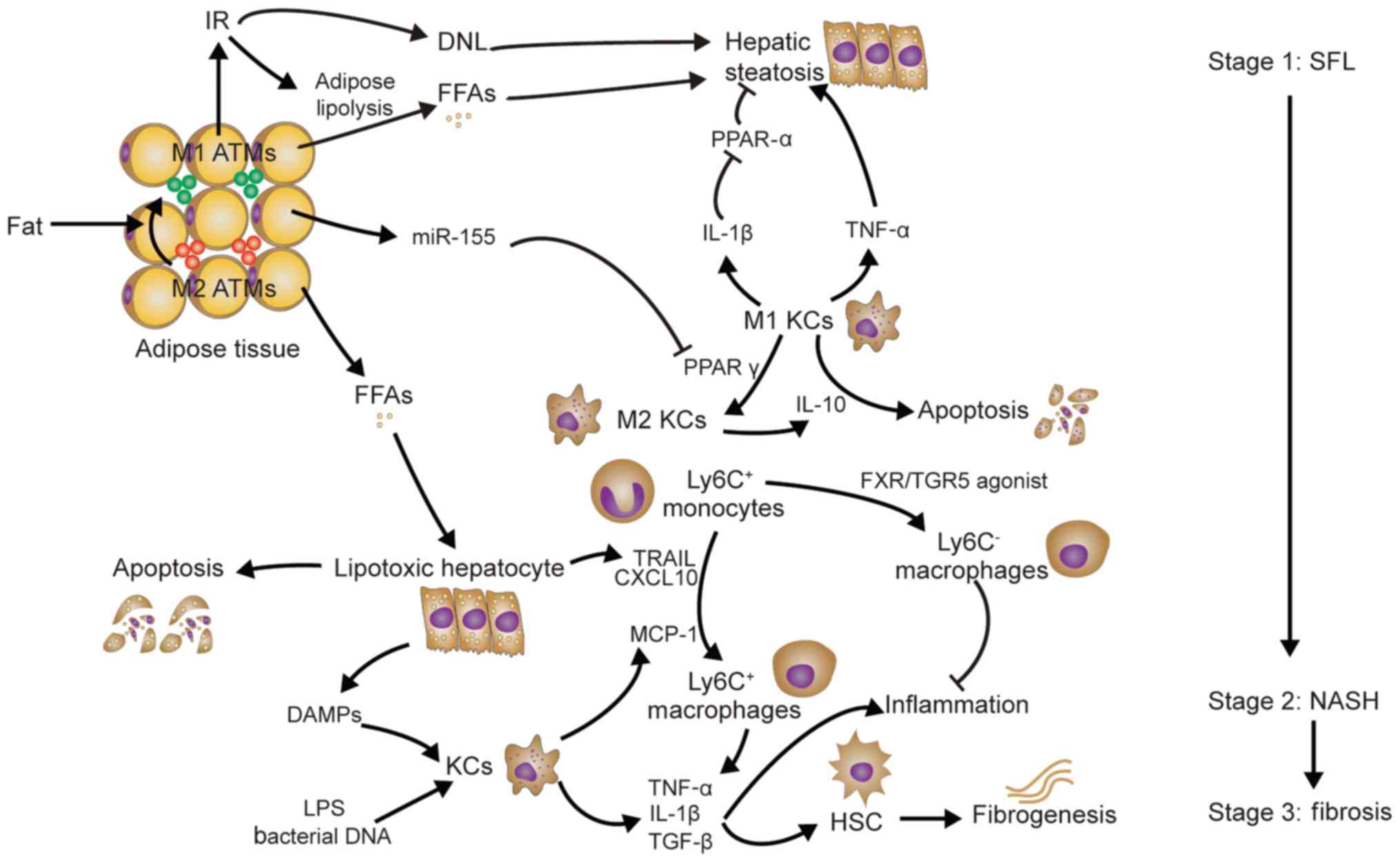
|
105
|
Lumeng Carey N, Bodzin Jennifer L and
Saltiel Alan R: Obesity induces a phenotypic switch in adipose
tissue macrophage polarization. J Clin Invest. 117:175–184. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Neuschwander-Tetri Brent A: Hepatic
lipotoxicity and the pathogenesis of nonalcoholic steatohepatitis:
The central role of nontriglyceride fatty acid metabolites.
Hepatology. 52:774–788. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Ying W, Riopel M, Bandyopadhyay G, Dong Y,
Birmingham A, Seo JB, Ofrecio JM, Wollam J, Hernandez-Carretero A,
Fu W, et al: Adipose tissue macrophage-derived exosomal miRNAs can
modulate in vivo and in vitro insulin sensitivity. Cell.
171:372–384 e312. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Luo W, Xu Q, Wang Q, Wu H and Hua J:
Effect of modulation of PPAR-γ activity on Kupffer cells M1/M2
polarization in the development of non-alcoholic fatty liver
disease. Sci Rep. 7:446122017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Stienstra R, Saudale F, Duval C, Keshtkar
S, Groener JE, van Rooijen N, Staels B, Kersten S and Mueller M:
Kupffer cells promote hepatic steatosis via interleukin-1
beta-dependent suppression of peroxisome proliferator-activated
receptor alpha activity. Hepatology. 51:511–522. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Huang W, Metlakunta A, Dedousis N, Zhang
P, Sipula I, Dube John J, Scott Donald K and O'Doherty Robert M:
Depletion of liver kupffer cells prevents the development of
diet-induced hepatic steatosis and insulin resistance. Diabetes.
59:347–357. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Wan J, Benkdane M, Teixeira-Clerc F,
Bonnafous S, Louvet A, Lafdil F, Pecker F, Tran A, Gual P, Mallat
A, et al: M2 kupffer cells promote M1 kupffer cell apoptosis: A
protective mechanism against alcoholic and nonalcoholic fatty liver
disease. Hepatology. 59:130–142. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Day CP and James OF: Steatohepatitis: A
tale of two ‘hits’? Gastroenterology. 114:842–845. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Tilg H and Moschen AR: Evolution of
inflammation in nonalcoholic fatty liver disease: The multiple
parallel hits hypothesis. Hepatology. 52:1836–1846. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Malhi H and Gores GJ: Molecular mechanisms
of lipotoxicity in nonalcoholic fatty liver disease. Semin Liver
Dis. 28:360–369. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Ibrahim SH, Hirsova P, Tomita K, Bronk SF,
Werneburg NW, Harrison SA, Goodfellow VS, Malhi H and Gores GJ:
Mixed lineage kinase 3 mediates release of C-X-C motif ligand
10-bearing chemotactic extracellular vesicles from lipotoxic
hepatocytes. Hepatology. 63:731–744. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Idrissova L, Malhi H, Werneburg NW,
LeBrasseur NK, Bronk SF, Fingas C, Tchkonia T, Pirtskhalava T,
White TA, Stout MB, et al: TRAIL receptor deletion in mice
suppresses the inflammation of nutrient excess. J Hepatol.
62:1156–1163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Li L, Chen L, Hu L, Liu Y, Sun HY, Tang J,
Hou YJ, Chang YX, Tu QQ, Feng GS, et al: Nuclear factor
high-mobility group box1 mediating the activation of toll-like
receptor 4 signaling in hepatocytes in the early stage of
nonalcoholic fatty liver disease in mice. Hepatology. 54:1620–1630.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Reid DT, Reyes JL, McDonald BA, Vo T,
Reimer RA and Eksteen B: Kupffer cells undergo fundamental changes
during the development of experimental NASH and are critical in
initiating liver damage and inflammation. PLoS One.
11:e01595242016. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Baeck C, Wehr A, Karlmark Karlin R,
Heymann F, Vucur M, Gassler N, Huss S, Klussmann S, Eulberg D,
Luedde T, et al: Pharmacological inhibition of the chemokine CCL2
(MCP-1) diminishes liver macrophage infiltration and
steatohepatitis in chronic hepatic injury. Gut. 61:416–426. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Miura K, Yang L, van Rooijen N, Ohnishi H
and Seki E: Hepatic recruitment of macrophages promotes
nonalcoholic steatohepatitis through CCR2. Am J Physiol-Gastroint
Liver Physiol. 302:G1310–G1321. 2012. View Article : Google Scholar
|
|
121
|
McMahan RH, Wang XXX, Cheng LL, Krisko T,
Smith M, El Kasmi K, Pruzanski M, Adorini L, Golden-Mason L, Levi
M, et al: Bile acid receptor activation modulates hepatic monocyte
activity and improves nonalcoholic fatty liver disease. J Biol
Chem. 288:11761–11770. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Miura K, Kodama Y, Inokuchi S, Schnabl B,
Aoyama T, Ohnishi H, Olefsky JM, Brenner DA and Seki E: Toll-like
receptor 9 promotes steatohepatitis by induction of interleukin-1
beta in mice. Gastroenterology. 139:323–334.e7. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Tomita K, Tamiya G, Ando S, Ohsumi K,
Chiyo T, Mizutani A, Kitamura N, Toda K, Kaneko T, Horie Y, et al:
Tumour necrosis factor alpha signalling through activation of
Kupffer cells plays an essential role in liver fibrosis of
non-alcoholic steatohepatitis in mice. Gut. 55:415–424. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Wang J, Leclercq I, Brymora JM, Xu N,
Ramezani-Moghadam M, London RM, Brigstock D and George J: Kupffer
cells mediate leptin-induced liver fibrosis. Gastroenterology.
137:713–723. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Tacke F: Targeting hepatic macrophages to
treat liver diseases. J Hepatol. 66:1300–1312. 2017. View Article : Google Scholar : PubMed/NCBI
|