Introduction
Spinal cord injury (SCI) is a traumatic event
resulting in serious disability and neurological deficits, which
results in a high economic burden and huge psychological pressures
for individuals and their families (1). The greatest harm following SCI is nerve
damage (2,3). Previous studies have demonstrated that
nerve injury is caused by two mechanisms, comprising primary
mechanical injury and secondary injury (4,5).
Secondary injury is triggered by a series of cellular events and
gene expression alterations, accompanied by a variety of extended
neuropathophysiological alterations and inflammatory responses over
a few minutes to a few weeks following the initial injury (6,7).
Apoptosis is the process of programmed cell death and serves a
crucial role in secondary lesions (8). Caspases have previously been observed
to exhibit proteolytic activity and are able to cleave substrate
proteins at aspartic acid residues, and serve an essential role in
apoptosis (9). Caspase-3 is
activated by initiator caspases, including caspase-8, caspase-9 and
caspase-10, and is well-established as the most critical member of
the executioner caspases; it can induce cell apoptosis irreversibly
by cleaving substrate proteins including poly-adenosine
diphosphate-ribose polymerase (PARP) (10). The anti-apoptotic protein Bcl-2 and
pro-apoptotic protein Bax belong to the Bcl-2 family, and serve a
vital role in cell apoptosis by regulating the permeability of the
mitochondrial membrane (11).
SCI is a worldwide medical problem, there are
179,312 novel traumatic spinal cord injury cases per year (12). No effective pharmacotherapy is
currently available other than methylprednisolone (MP), which is a
potent anti-inflammatory agent (13). However, the use of MP is subject to
much debate, due to its limited efficacy and numerous adverse side
effects (14). At present, there is
still no effective, standardized method of treating SCI, therefore
the identification and development of novel therapeutics would be
of great clinical significance in the field of SCI treatment.
Pectolinarigenin (PG) is an active component of medicinal thistle
plants and Eupatorium odoratum L., and exerts significant
anti-inflammatory and hemostatic effects (15). However, there are few studies
examining the function of PG (16).
Therefore, the aim of the present study was to investigate the role
of PG in SCI.
The data obtained in the present study suggested
that PG significantly improved functional recovery and reduced
tissue loss, and neuronal apoptosis in rats with SCI. In addition,
the results of western blotting assay demonstrated that the
expression of pro-apoptotic proteins (caspase-3, caspase-9 and
PARP) were downregulated and the Bax: Bcl2 ratio was reduced
following treatment with PG.
Materials and methods
Animals and grouping
A total of 36 adult male Sprague-Dawley rats,
obtained from the Shanghai SLAC Laboratory Animal Co., Ltd.,
(Shanghai, China), weighing between 200 and 250 g were used for the
experiments. All rats were housed at 22–25°C, at 40–60% humidity
with a 12-h light-dark cycle and free access of food and water. For
the spinal cord injury (SCI) rat model, a dorsal longitudinal
incision was made to expose T9-T11 following the administration of
anesthetics. A laminectomy was subsequently performed at T10 and
the modified Allen method was conducted to induce acute SCI as
described previously, dropping a 10 g rod from a 4 cm height onto
the dorsal surface of the spinal cord (17,18).
Rats in the sham-surgery group received a laminectomy only. All
animal handling procedures and experimental protocols were
consistent with the National Institutes of Health Guide for the
Care and Use of Laboratory Animals (GB 14925-2001).
The animals were randomly divided into six
experimental groups (n=6 in each group) as follows: i) Sham-surgery
group (in which rats were only treated with a laminectomy without
SCI for comparison); ii) SCI + saline; iii) SCI + low-dose PG (10
mg/kg); iv) SCI + middle-dose PG (30 mg/kg); v) SCI + high-dose PG
(50 mg/kg) and vi) SCI + MP (30 mg/kg), which was used as a
positive control. PG or MP was administered to rats
intraperitoneally, every 2 days.
Behavioral assessment
Basso-Beattie-Bresnahan (BBB) locomotor rating
scoring was performed to assess the functional recovery of the rat
hind limbs. The neurological outcome for each animal was examined
in an open field using the BBB locomotor rating scale, ranging from
0 (complete paralysis) to 21 (normal locomotion) (19). Scores from 0 to 7 were considered to
indicate the early stages of recovery and were used to judge the
joint activities of the hind limbs; scores from 8 to 13 indicated
the intermediate recovery phase, and were used to assess the gait
of the animals and the coordination of the hind limbs. Finally,
scores from 14 to 21 were considered to indicate the late phase of
recovery and were used to assess the fine motions of the paw during
animal movement. BBB testing was performed on days 1, 3, 7, 14, 21
and 28 following spinal cord surgery. Each rat was scored once a
day in double-blind model for a period of 4 min by two examiners
and an average value per animal was calculated.
Nissl staining
Following the behavioral tests, tissue blocks
comprising 1-cm sections of spinal cord centered on the lesion site
were embedded in paraffin. Sample sections (5 µm) of the lesion
site were stained for Nissl with cresyl-violet acetate
(Sigma-Aldrich, Merck KGaA, Darmstadt, Germany) at room temperature
for 10 min. The tissue sections were cleared using xylene and
rehydrated with anhydrous ethanol at 95, 80, and 70% alcohol and
double-distilled water. Sections were then stained in 0.1%
cresyl-violet acetate (Sigma-Aldrich; Merck KGaA) at room
temperature for 10 min. The tissues were rinsed in double-distilled
water and differentiated in 70% ethanol with acetic acid for 2 min.
The tissues were subsequently dehydrated with 70, 80 and 95%
alcohol, washed in xylene, and placed on a cover-slip with slide
mounting medium. Image-Pro Plus 6.0 (Media Cybernetics, Inc.,
Rockville, MA, USA) software was used to count the number of
surviving neurons.
Terminal dUTP nick-end labeling
(TUNEL) staining
The TUNEL assay was performed to assess cell
apoptosis. Spinal cords were excised and fixed in 4%
paraformaldehyde overnight at room temperature and embedded in
paraffin. Samples were stained with terminal TUNEL kit (40307ES20;
Yeasen, Shanghai, China) according to the manufacturer's protocol.
Sample sections (5 µm) were cleared using xylene and rehydrated
with anhydrous ethanol at 90, 80 and 70% alcohol and deionized
water. Sections were then stained with an Alexa Fluor 488-12-dUTP
Labeling Mix (Yeasen) at 37°C for 1 h. TUNEL-stained slides were
observed under fluorescence microscopy (Olympus Corporation, Tokyo,
Japan) at ×400 magnification, and five fields of view for each
section were randomly selected for subsequent calculations. The
number of TUNEL positive cells was counted, and the average value
was collected. Data were collected from three independent
experimental repeats.
Western blot analysis
Total protein was extracted from T9-T11 spinal cord
tissues using a lysis buffer, which contained 50 mM Tris-HCl, pH
7.4; 5 mM EDTA; 1% (v/v) NP-40 with 1 mM phenylmethylsulfonyl
fluoride. A bicinchoninic assay kit (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) was used to measure the protein concentration.
Protein samples (40 µg/lane) were separated via SDS-PAGE (10%
resolving gels, 4% stacking gels) and blotted onto polyvinylidene
difluoride membranes (Thermo Fisher Scientific, Inc., Waltham, MA,
USA). The membranes were blocked in 5% non-fat milk for 1 h at room
temperature, followed by incubation overnight at 4°C with the
primary antibodies. Subsequently, secondary antibodies were
incubated at room temperature for an additional 2 h.
Chemiluminescent signals were visualized using the ECL detection
reagent (EMD Millipore, Billerica, MA, USA). ImageJ software 1.4
(National Institutes of Health, Bethesda, MD, USA) was used to
analyze the relative protein expression. The antibodies used are
listed as follow: Cleaved-caspase-3 (1:500; cat. no. 9664S; Cell
Signaling Technology, Inc., Danvers, MA, USA), cleaved-caspase-9
(1:500; cat. no. 9509), cleaved-PARP (1:500; cat. no. 94885), Bcl-2
(1:1,000; cat. no. 3498), Bax (1:1,000; cat. no. 14796; all Cell
Signaling Technology, Inc.), β-actin (1:1,000; cat. no. sc-517582),
horseradish peroxidase (HRP) conjugated rabbit anti-mouse
immunoglobulin G (IgG; 1:5,000; cat. no. sc-358914), HRP-mouse
anti-rabbit IgG (1:10,000; cat. no. sc-2357; all Santa Cruz
Biotechnology, Inc.).
Statistical analysis
Data are presented as the mean ± standard deviation
and each experiment was repeated three times. GraphPad Prism
version 6 (GraphPad Software Inc., La Jolla, CA, USA) was used to
perform the statistical analyses. One-way analysis of variance was
used to compare the significant differences among multiple groups,
followed by Tukey's post-hoc analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
Protective effects of PG on functional
recovery in rats following acute SCI
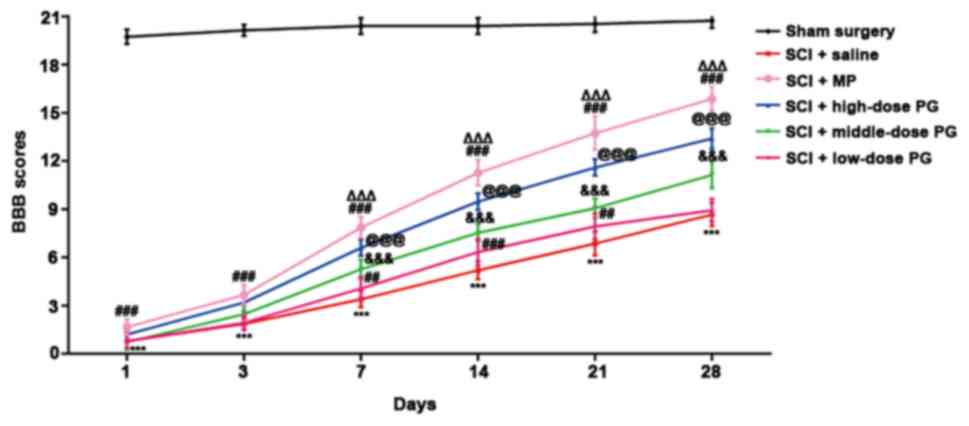
In order to assess the effects of PG on functional
recovery following acute SCI in each group, BBB locomotor rating
scoring was performed on days 1, 3, 7, 14, 21 and 28 following SCI
(Fig. 1). The BBB locomotor test is
a sensitive and reliable method of detecting locomotor function
following SCI. MP and saline were used as a positive control and
normal control, respectively. Different doses of PG (10, 30 and 50
mg/kg) were administered to the appropriate groups, and the mean
BBB scores were collected. It was observed that the middle-dose PG
group and high-dose PG group exhibited functional recovery by days
7 and 3 respectively, and the effect lasted until day 28 following
SCI (Fig. 1). However, BBB scores in
the low-dose PG group were significantly increased only on days 7,
14 and 21 (P<0.01; Fig. 1). From
day 7–28, the scores in the high-dose PG group were increased
compared with the middle-dose PG group and the differences were
statistically significant (P<0.001; Fig. 1). Similarly the middle-dose PG group
exhibited higher scores than low-dose PG group (Fig. 1). These data demonstrated that PG
exerted protective effects on the spinal cord in a dose-dependent
manner. Treatment with PG 50 mg/kg was demonstrated to be the most
effective dose, with an effect comparable to that of MP at 30
mg/kg.
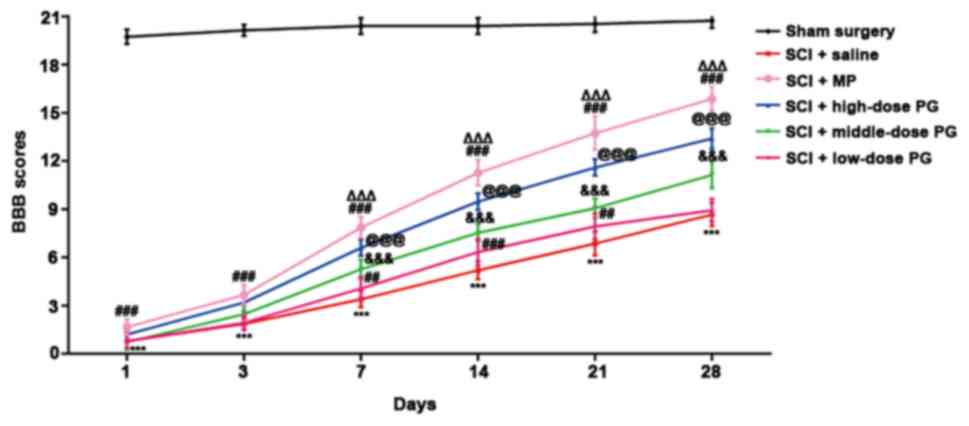 | Figure 1.PG promotes functional recovery in
rats following SCI. BBB locomotor rating scoring was performed on
days 1, 3, 7, 14, 21 and 28 following SCI. ***P<0.001 SCI +
saline vs. Sham surgery, ΔΔΔP<0.001 SCI + MP vs.
high-dose PG (50 kg/ml), @@@P<0.001 SCI + high-dose PG (50 kg/ml)
vs. SCI + saline, &&&P<0.001 SCI +
middle-dose PG vs. SCI + low-dose PG, ##P<0.01,
###P<0.001SCI + low-dose PG or SCI + MP vs. SCI +
saline. BBB, Basso-Beattie-Bresnahan; SCI, spinal cord injury; MP,
methylprednisolone; PG, pectolinarigenin. |
Protective effects of PG on neuron
damage in the spinal cord of SCI rats
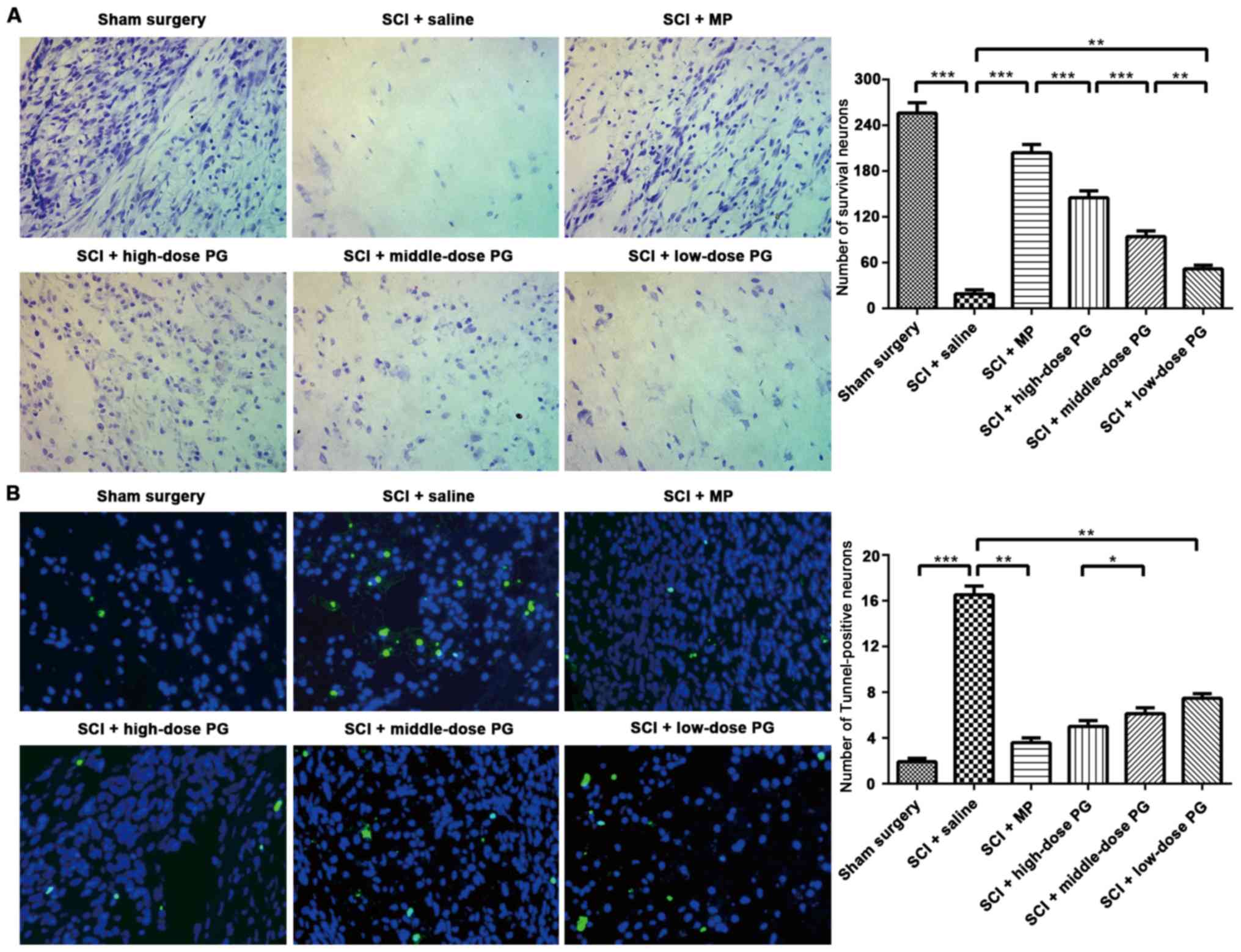
In order to further examine the underlying mechanism
of the protective function of PG in SCI, Nissl staining was
performed to observe any potential neuroprotective effects on day
28 post-SCI. Nissl staining indicated that neurons in the sham
group displayed an integrative and granular-like morphology. The
SCI + saline group exhibited significantly fewer surviving neurons
in the lesions of the spinal cord compared with the sham group
(P<0.001; Fig. 2A). In addition,
the neurons appeared swollen and exhibited irregular morphologies
(Fig. 2A). The number of surviving
neurons increased significantly at 28 days post-SCI in the three
PG-treated groups and the SCI + MP (30 mg/kg) group (P<0.001;
Fig. 2A). Taken together, these data
indicated that PG intervention increased the number of surviving
neurons, normalized the morphology of neurons and restored neuronal
function, which is represented by the increased number of Nissl
bodies. In addition, this experiment revealed that PG exhibited a
dose-dependent effect, with higher PG resulted in better
neuroprotective effect.
PG inhibits cell apoptosis in rats
following SCI
TUNEL staining was performed to assess the effect of
PG on apoptotic cells following SCI. The results demonstrated that
in the SCI + saline group, positive cells were significantly
increased and widely distributed, compared with the sham group
(P<0.001; Fig. 2B). The different
doses of PG markedly reduced the number of TUNEL-positive neurons
when compared with the SCI + saline group (Fig. 2B). The results exhibited a certain
level of dose-dependent efficacy; however there was no
statistically significant difference between the middle-dose and
low-dose PG groups (Fig. 2B).
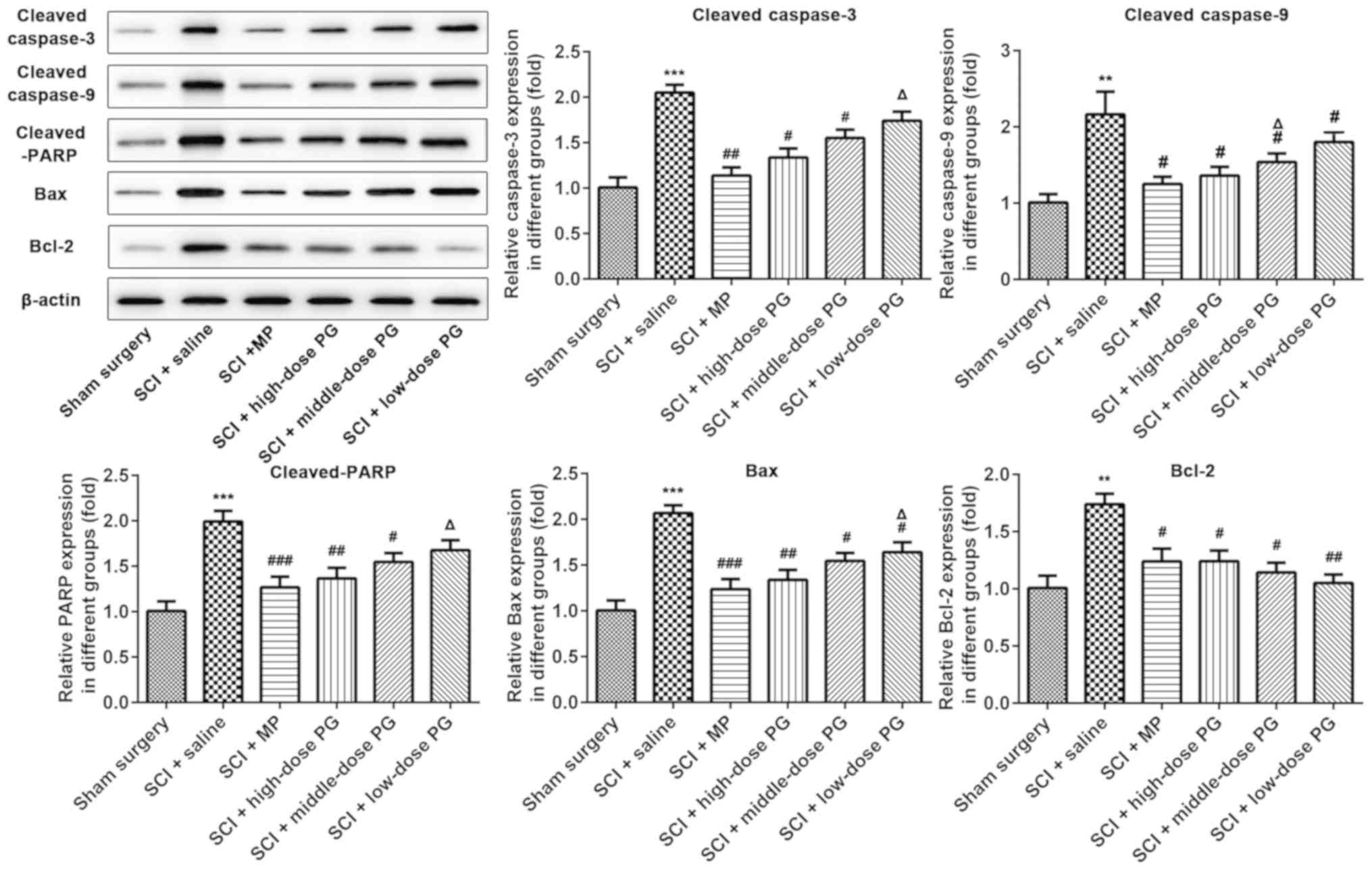
Subsequently, western blot analysis was performed to detect the
expression of apoptosis-associated proteins at day 28 post-SCI. The
results revealed that the expression of activated caspase-3,
caspase-9 and cleaved-PARP were dramatically increased in the SCI +
saline group, compared with the Sham surgery group (Fig. 3). Treatment with PG markedly
downregulated the levels of activated caspase-3, caspase-9 and
cleaved-PARP (Fig. 3). Additionally,
the expression of Bcl-2 was decreased, whereas the Bcl2 level was
increased with the increasing PG concentration (Fig. 3). These data demonstrated that PG
inhibited cellular apoptosis by downregulating cleaved caspase-3
and −9 and PARP expression and reducing the Bax: Bcl2 ratio.
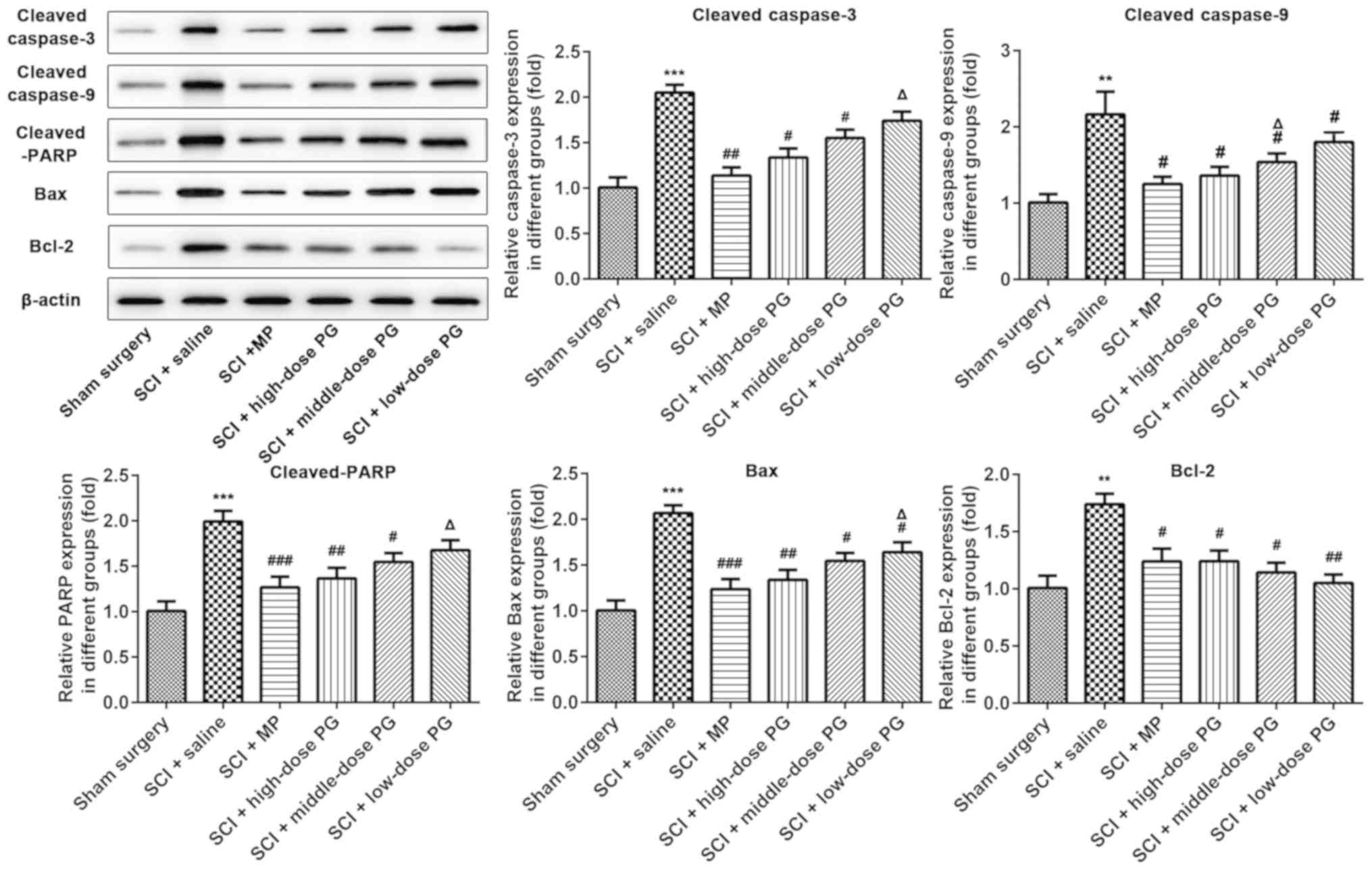 | Figure 3.Apoptosis-associated protein and gene
expression at day 28 post-SCI. Western blot analysis was performed
to detect the protein expression of cleaved caspase-3, caspase-9,
cleaved PARP, Bax and Bcl-2. **P<0.01, ***P<0.001 vs. Sham
surgery; #P<0.05, ##P<0.01,
###P<0.001 vs. SCI + saline; ΔP<0.05
vs. SCI + MP. SCI, spinal cord injury; MP, methylprednisolone; PG,
pectolinarigenin; PARP, poly-ADP-ribose polymerase. |
Discussion
In present study, acute spinal cord injury was
induced in a rat model and a modified version of the Allen method
was conducted, in order to investigate the role of PG in SCI. MP,
the most widely used clinical medicine for the treatment of SCI
(13), was used as a positive
control drug. The BBB locomotor test was performed to detect the
motor function following SCI and the results demonstrated that PG
exerted protective effects on the spinal cord. Among the different
PG treatment groups, 50 mg/kg was determined to be the most
effective dose, with similar effects to those of MP at 30 mg/kg.
Nissl staining confirmed that PG markedly increased the number of
surviving neurons, normalized the morphology of neurons and
restored neuronal function.
Secondary injury may cause nerve damage, accompanied
by a variety of cellular events and occurs minutes to weeks
following initial mechanical injury, eventually culminating in
damage to tissues (6). Due to the
irreversibility of the initial injury, the majority of studies have
focused on the therapy and mechanisms of secondary injury (20–22).
Apoptosis, which is principally mediated by the caspase and Bcl-2
families, serves a crucial role in secondary lesions and culminates
in the cell death of neurons (23,24). The
loss of neuronal cells that are not replaced following injury may
contribute greatly to disability following SCI (7,25).
Taking this into account, the present study further investigated
the possible underlying mechanism of the protective effects of PG
on neuronal cells by performing TUNEL staining to assess cell
apoptosis following SCI. The results demonstrated that treatment
with PG reduced the number of TUNEL-positive neurons, suggesting
that PG inhibited cell apoptosis in rats following SCI. In
addition, the expression levels of the pro-apoptotic proteins Bax,
cleaved caspase-3 and 9, and cleaved-PARP were identified to be
decreased, and the anti-apoptotic protein Bcl-2 was upregulated,
following treatment with PG.
Numerous studies have reported the limitations and
side effects of MP, which has led to controversy regarding the
clinical application of MP for the treatment of SCI; however, at
present, there are no suitable effective drugs to replace MP
(26–28). The results of the present study
suggested that PG may have a protective effect against SCI in rats,
potentially by inhibiting neuronal apoptosis. There are few studies
on PG and a lot of those that do exist focus on its antitumor
activity (29–31). For example, a previous study on
nasopharyngeal carcinoma demonstrated that PG activates the caspase
signaling pathway and promotes cell apoptosis, further inhibiting
tumor growth in nasopharyngeal carcinoma (32). Zhang et al (29) suggested that PG prevents cancer
aggressiveness by inhibiting signal transducer and activator of
transcription 3 activity in osteosarcoma. By contrast, the data
obtained in the present study suggest that PG has a protective
effect against SCI in rats, potentially by inhibiting neuronal
apoptosis. Notably, Csupor et al (33) identified that PG, extracted from
Centaurea sadleriana, exhibited anti-inflammatory
activities, which is clinically relevant as inflammation is another
critical event in secondary injury following SCI (34). Several drugs have been assessed in
experimental and clinical trials that are aimed at reducing the
inflammatory response in SCI (35–37).
However, whether PG exhibits a role in SCI-induced inflammation
requires further study.
Taking the inefficiency and adverse effects of MP
into consideration, the identification and development of novel
medicines is of great clinical significance in the field of SCI
treatment. Although further studies are required, the findings
obtained in the current study suggested that PG promotes functional
recovery and prevents neuronal damage in rats following SCI by
inhibiting apoptosis, at least partially. Therefore PG may serve as
a potential therapeutic agent for the treatment of SCI.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BW and JL conceived and designed the experiments,
and performed data analysis. JL wrote the manuscript and BW
reviewed and edited the manuscript.
Ethics approval and consent to
participate
The present study was approved by the institutional
Animal Care and Use Committee of the People's Hospital of China
Three Gorges University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Calancie B, Molano MR and Broton JG:
Epidemiology and demography of acute spinal cord injury in a large
urban setting. J Spinal Cord Med. 28:92–96. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fox IK, Davidge KM, Novak CB, Hoben G,
Kahn LC, Juknis N, Ruvinskaya R and Mackinnon SE: Nerve transfers
to restore upper extremity function in cervical spinal cord injury:
Update and preliminary outcomes. Plast Reconstr Surg. 136:780–792.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moulin P, Gohritz A and Meunzel J: Spinal
cord injury: Still an interdisciplinary challenge [corrected].
Orthopade. 43:625–635. 2014.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Choi DW and Rothman SM: The role of
glutamate neurotoxicity in hypoxic-ischemic neuronal death. Annu
Rev Neurosci. 13:171–182. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fehlings MG and Nguyen DH: Immunoglobulin
G: A potential treatment to attenuate neuroinflammation following
spinal cord injury. J Clin Immunol. 30 (Suppl 1):S109–S112. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Song Y, Zeng Z, Jin C, Zhang J, Ding B and
Zhang F: Protective effect of ginkgolide B against acute spinal
cord injury in rats and its correlation with the Jak/STAT signaling
pathway. Neurochem Res. 38:610–619. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bareyre FM and Schwab ME: Inflammation,
degeneration and regeneration in the injured spinal cord: Insights
from DNA microarrays. Trends Neurosci. 26:555–563. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu C, Shi Z, Fan L, Zhang C, Wang K and
Wang B: Resveratrol improves neuron protection and functional
recovery in rat model of spinal cord injury. Brain Res.
1374:100–109. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shalini S, Dorstyn L, Dawar S and Kumar S:
Old, new and emerging functions of caspases. Cell Death Differ.
22:526–539. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Slee EA, Adrain C and Martin SJ:
Executioner caspase-3, −6, and −7 perform distinct, non-redundant
roles during the demolition phase of apoptosis. J Biol Chem.
276:7320–7326. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cory S and Adams JM: The Bcl2 family:
Regulators of the cellular life-or-death switch. Nat Rev Cancer.
2:647–656. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Meijles DN and Pagano PJ: Nox and
inflammation in the vascular adventitia. Hypertension. 67:14–19.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fehlings MG, Wilson JR and Cho N:
Methylprednisolone for the treatment of acute spinal cord injury:
Counterpoint. Neurosurgery. 61 (Suppl 1):S36–S42. 2014. View Article : Google Scholar
|
|
14
|
Samano C, Kaur J and Nistri A: A study of
methylprednisolone neuroprotection against acute injury to the rat
spinal cord in vitro. Neuroscience. 315:136–149. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lim H, Son KH, Chang HW, Bae K, Kang SS
and Kim HP: Anti-inflammatory activity of pectolinarigenin and
pectolinarin isolated from Cirsium chanroenicum. Biol Pharm Bull.
31:2063–2067. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lee S, Lee DH, Kim JC, Um BH, Sung SH,
Jeong LS, Kim YK and Kim SN: Pectolinarigenin, an aglycone of
pectolinarin, has more potent inhibitory activities on
melanogenesis than pectolinarin. Biochem Biophys Res Commun.
493:765–772. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Perot PL Jr, Lee WA, Hsu CY, Hogan EL, Cox
RD and Gross AJ: Therapeutic model for experimental spinal cord
injury in the rat: I. Mortality and motor deficit. Cent Nerv Syst
Trauma. 4:149–159. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Priestley JV, Michael-Titus AT and
Tetzlaff W: Limiting spinal cord injury by pharmacological
intervention. Handb Clin Neurol. 109:463–484. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Basso DM, Beattie MS and Bresnahan JC: A
sensitive and reliable locomotor rating scale for open field
testing in rats. J Neurotrauma. 12:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stampas A and Tansey KE: Spinal cord
injury medicine and rehabilitation. Semin Neurol. 34:524–533. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Quinzaños-Fresnedo J and Sahagun-Olmos RC:
Micro RNA and its role in the pathophysiology of spinal cord
injury-a further step towards neuroregenerative medicine. Cir Cir.
83:442–447. 2015.(In Spanish). PubMed/NCBI
|
|
22
|
Haller J, Bice M and Lawrence B: Mediating
the secondary effects of spinal cord injury through optimization of
key physiologic parameters. J Am Acad Orthop Surg. 24:160–171.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cai W and Shen WD: Anti-apoptotic
mechanisms of acupuncture in neurological diseases: A review. Am J
Chin Med. 46:515–535. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Oyinbo CA: Secondary injury mechanisms in
traumatic spinal cord injury: A nugget of this multiply cascade.
Acta Neurobiol Exp (Wars). 71:281–299. 2011.PubMed/NCBI
|
|
25
|
Mattson MP: Apoptosis in neurodegenerative
disorders. Nat Rev Mol Cell Biol. 1:120–129. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sunshine JE, Dagal A, Burns SP, Bransford
RJ, Zhang F, Newman SF, Nair BG and Sharar SR: Methylprednisolone
therapy in acute traumatic spinal cord injury: Analysis of a
regional spinal cord model systems database. Anesth Analg.
124:1200–1205. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wilson JR, Jaja BNR, Kwon BK, Guest JD,
Harrop JS, Aarabi B, Shaffrey CI, Badhiwala JH, Toups EG, Grossman
RG and Fehlings MG: Natural history, predictors of outcome, and
effects of treatment in thoracic spinal cord injury: A Multi-center
cohort study from the North American Clinical Trials Network. J
Neurotrauma. 35:2554–2560. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Karsy M and Hawryluk G: Pharmacologic
management of acute spinal cord injury. Neurosurg Clin N Am.
28:49–62. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhang T, Li S, Li J, Yin F, Hua Y, Wang Z,
Lin B, Wang H, Zou D, Zhou Z, et al: Natural product
pectolinarigenin inhibits osteosarcoma growth and metastasis via
SHP-1-mediated STAT3 signaling inhibition. Cell Death Dis.
7:e24212016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhang T, Li S, Li J, Yin F, Hua Y, Wang Z,
Lin B, Wang H, Zou D, Zhou Z, et al: Correction to: Natural product
pectolinarigenin inhibits osteosarcoma growth and metastasis via
SHP-1-mediated STAT3 signaling inhibition. Cell Death Dis.
9:9022018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lee HJ, Venkatarame Gowda Saralamma V, Kim
SM, Ha SE, Raha S, Lee WS, Kim EH, Lee SJ, Heo JD and Kim GS:
Pectolinarigenin induced cell cycle arrest, autophagy, and
apoptosis in gastric cancer cell via PI3K/AKT/mTOR signaling
pathway. Nutrients. 10(pii): E10432018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang C, Cheng Y, Liu H, Xu Y, Peng H, Lang
J, Liao J, Liu H, Liu H and Fan J: Pectolinarigenin suppresses the
tumor growth in nasopharyngeal carcinoma. Cell Physiol Biochem.
39:1795–803. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Csupor D, Widowitz U, Blazsó G,
Laczkó-Zöld E, Tatsimo JS, Balogh A, Boros K, Dankó B, Bauer R and
Hohmann J: Anti-inflammatory activities of eleven Centaurea species
occurring in the Carpathian Basin. Phytother Res. 27:540–544. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gal P, Kravcuková P, Mokry M and Kluchová
D: Chemokines as possible targets in modulation of the secondary
damage after acute spinal cord injury: A review. Cell Mol
Neurobiol. 29:1025–1035. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Cristante AF, Barros Filho TE, Marcon RM,
Letaif OB and Rocha ID: Therapeutic approaches for spinal cord
injury. Clinics. 67:1219–1224. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Song Y, Xue H, Liu TT, Liu JM and Chen D:
Rapamycin plays a neuroprotective effect after spinal cord injury
via anti-inflammatory effects. J Biochem Mol Toxicol. 29:29–34.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang YT, Lu XM, Chen KT, Shu YH and Qiu
CH: Immunotherapy strategies for spinal cord injury. Curr Pharm
Biotechnol. 16:492–505. 2015. View Article : Google Scholar : PubMed/NCBI
|