Introduction
Rapid progress has been made in the development of
minimally invasive surgery. Laparoscopic surgery has the advantages
of less pain, more rapid recovery and less discomfort (1), and increasing numbers of patients are
opting for this method. However, laparoscopic surgery is one of the
high-risk surgical factors for post-operative nausea and vomiting
(PONV) (2). A variety of studies
have indicated that the incidence of PONV is ~30% after general
anaesthesia and 50–70% after laparoscopic surgery (3,4). Females
are more susceptible to PONV than males (5). An estimated 71–80% of patients suffer
from PONV after general anaesthesia for gynaecological laparoscopy
(6). Thus, PONV is one of the most
common complaints after laparoscopic surgery together with
post-operative pain. PONV is a distressing symptom after general
anaesthesia and may increase patient discomfort and clinical
problems, including disruption of the surgical wound, dehydration,
electrolyte imbalance, aspiration pneumonia and haemorrhage
(7,8). Furthermore, it may prolong recovery
time, increase hospital costs and delay patient discharge (9). Therefore, reducing the incidence of
PONV is conducive to the recovery of patients.
Numerous methods and drugs may prevent PONV,
including 5-HT3 receptor antagonists, dopamine receptor
antagonists, neurokinin-1 receptor antagonists, dexamethasone and
propofol (10). However, these drugs
are expensive or have numerous adverse effects. Peri-operative
intravenous lidocaine is beneficial to the recovery of patients and
has been widely used in clinical surgery (11). Clinical trials have indicated that
intravenous lidocaine markedly reduces the incidence of PONV
(12). Lidocaine has
well-established analgesic, anti-hyperalgesic and anti-inflammatory
characteristics (13). Certain
studies have indicated that lidocaine accelerates the restoration
of bowel function after surgery, which may be attributed to its
anti-inflammatory effect. The favourable effects of lidocaine
infusion include reduction of nausea and vomiting, pain scores, the
duration of post-operative ileus and the duration of hospital stay
according to a clinical trial on colon surgery (14). McKay et al (15) did not obtain the same positive
results in a previous study regarding ambulatory surgery. In that
study, lidocaine only reduced the consumption of narcotics and
maintained a temporary reduction in pain scores (15). The reduction of post-operative opioid
consumption and the anti-inflammatory properties of lidocaine may
be involved in the improvement of opioid-induced bowel dysfunction,
but the results of studies are contradictory, with certain studies
supporting the hypothersis (16,17)
while another does not (18).
Another study demonstrated that intravenous lidocaine did not
improve the opioid consumption or nausea and vomiting in patients
who underwent open abdominal hysterectomy (19). However, the effect of pre-operative
and intra-operative lidocaine infusion on PONV and quality of
recovery in gynaecological laparoscopy surgery has remained to be
investigated. Instead of the length of hospital stay, the quality
of recovery score (QoR-40) (20) has
become the most widely used measure of patient-assessed quality of
recovery after surgery, as it is highly sensitive to clinical
changes, valid, reliable, responsive and simple to use (21). In the present study, the effect of
lidocaine infusion on nausea, vomiting and QoR-40 after
gynaecological laparoscopic surgery was evaluated.
Materials and methods
Research subjects
The present study was approved by the ethics
committee of the Affiliated Hospital of Yangzhou University
(Yangzhou, China) and all patients provided written informed
consent. According to a preliminary experiment, the required sample
size was calculated and it was determined that a minimum of 20
patients were needed in each group (α error of 0.05 and β error of
0.2). Thus, a total of 40 patients aged 30–50 years with an
American Society of Anaesthesiologists' physical status of I–II
(22) who were scheduled for
elective laparoscopic gynaecological surgery for ovarian and
uterine disease were enrolled. All patients were randomly assigned
to two groups, namely the lidocaine group (Group L: Age, 41.1±7.4
years) and the control group (Group C: Age, 40.6±8.3 years).
Subjects were randomized with the aid of SPSS statistical analysis
software (version 13; SPSS, Inc., Chicago, IL, USA) to receive one
of two treatments in a double-blinded manner. The patients and
anaesthesia providers were blinded with regard to the study group
allocation throughout the study period. The solutions for
injection/infusion were prepared by an independent researcher. The
solution administered to Group L consisted of 1% lidocaine (China
Resources Shuanghe Pharmaceutical Co., Ltd., Beijing, China) in
coded 50-ml syringes, and the solution administered to Group C
consisted of an equal volume of saline.
Inclusion and exclusion criteria
Patients with the following characteristics were
excluded from the study: Cardiovascular diseases, metabolic
diseases, renal diseases, liver diseases, neurological disorders,
acid-base balance electrolyte disorders, shock, pregnancy, history
of tobacco use, history of PONV, pre-existing disorders of the
gastrointestinal tract, use of anti-emetics within 48 h prior to
surgery, chronic use of anti-cholinergic medication or chronic
treatment with opioids, and an operation time of <30 min or
>90 min. All operations were performed in the morning, were the
first surgeries that day and followed a standardized procedure
without additional procedures including irrigation, laparotomy and
blood transfusion. Surgery and nursing were performed by the same
team. All patients were enrolled between April and August 2017.
Anesthesia method
Patients fasted after midnight the night prior to
surgery, and 30 min prior to the induction of anaesthesia, they
were orally pre-medicated with midazolam (0.04 mg/kg; Jiangsu Nhwa
Pharmaceutical Co., Ltd., Xuzhou, China) and scopolamine (0.3 mg;
Guangzhou Baiyunshan Guanghua Pharmaceutical Co., Ltd., Guangzhou,
China). Immediately prior to the induction of anaesthesia, the
patients in Group L received an intravenous bolus injection of 1.5
mg/kg lidocaine. In Group L, the lidocaine infusion was continued
at a rate of 2 mg/kg/h throughout the operation, and patients were
transferred to the post-anaesthesia care unit after surgery. The
patients in the control group were given a saline infusion
administered in a similar manner. Prior to the induction of
anaesthesia, the patients' electrocardiogram, heart rate, and
oxygen saturation were monitored continuously, and non-invasive
arterial blood pressure was recorded at 5-min intervals throughout
the procedure. For anaesthetic induction, 2 mg/kg propofol
(AstraZeneca UK Limited, London, UK) and 4 µg/kg fentanyl (Yichang
Renfu Pharmaceutical Co., Ltd., Yichang, China) were intravenously
administered prior to tracheal intubation. In each of the two
groups, tracheal intubation was facilitated with 0.2 mg/kg
cis-atracurium (Jiangsu Hengrui Pharmaceutical Co., Ltd.,
Lianyungang, China), and cis-atracurium was also used for
intra-operative muscle relaxation in all patients. Full muscle
relaxation was maintained during surgery. Anaesthesia was
maintained with 70–90 µg/kg/min propofol and 0.2–0.5 µg/kg/min
remifentanil (Yichang Renfu Pharmaceutical Co., Ltd.). During
surgery, maintenance doses of anaesthetics were adjusted to
maintain bispectralindex (BIS) within 40–60 in each group. Lactated
Ringer's solution (8 ml/kg/h; China Resources Shuanghe
Pharmaceutical Co., Ltd.) was infused throughout the surgery.
Record indicator
Mean arterial pressure, heart rate and oxygen
saturation were recorded prior to the operation, at the time of
intubation, during pneumoperitoneum, at the time of extubation, at
1 min after extubation and at 5 min after extubation. The
anaesthesia time, operating time, pneumoperitoneum time, recovery
time, extubation time, dosage of remifentanil, first flatus time,
defecation time and length of hospital stay were recorded for each
patient. The Ramsay sedation scale (RSS) score (23) was recorded at 1 min, 5 min and 30 min
after extubation.
The incidence of PONV, the nausea score and the use
of anti-emetics at 1, 6 and 24 h after surgery were also recorded.
Pain scores were assessed using the visual analogue scale (VAS)
(24) every 6 h until 48 h after the
operation. The recovery of the patients was evaluated by using the
QoR-40 at 1 day prior to the operation and at 1, 3 and 5 days after
the operation.
According Eberhart et al (25), the severity of PONV during the 24 h
after surgery was divided into four categories: None (absence of
nausea and vomiting), mild (the patient suffered only mild nausea),
moderate (the patient suffered 1–2 emetic episodes or moderate or
severe nausea without exogenous stimulus and anti-emetics were
required), and severe (the patient vomited at least once or
experienced nausea at least twice, and anti-emetics were required
at least once).
The QoR-40 contains 40 items measuring five aspects
of patient recovery: Psychological support (7 items), physical
comfort (12 items), emotional wellbeing (9 items), physical
independence (5 items) and pain (7 items) (17). Each item is divided into five levels
(for positive items: 1, none of the time; 2, some of the time; 3,
often; 4, most of the time; and 5; all of the time. For negative
items, the scoring was reversed). The individual scores are then
added up and the resulting QoR-40 scores range from 40 (extremely
poor quality of recovery) to 200 (excellent quality of recovery),
with a higher QoR-40 score indicating a better recovery.
At 1 day prior to surgery, the QoR-40 instrument was
explained to the patients. After they understood the meaning of the
questionnaire, the QoR-40 scores were evaluated and recorded as the
pre-operative baseline health status at day 0 (D0) by the assigned
medical professional. QoR-40 scores were also recorded at the same
time of day at 1 day post-surgery (D1), D3 and D5 by the assigned
medical professional.
Statistical analysis
The major results are expressed as the mean ±
standard deviation, the median (range) or the number of patients.
Student's t-test was used to compare continuous variables between
the groups. The χ2 test or Fisher's exact test was used
for categorical variables. Statistical analysis was performed using
SPSS 13.0 for Windows (SPSS, Inc.).
Results
General information
A total of 45 patients were initially recruited to
the current study, but 5 patients were excluded. The remaining 40
patients were subsequently allocated to the two equally sized
groups and completed the study. The data from these patients were
used in the analysis. No significant differences were observed
between the two groups in terms of age, body weight or body height.
Intraoperative data, including the duration, the CO2
pressure, the length of anaesthesia and pneumoperitoneum were
similar between the two groups (Table
I).
 | Table I.Patient and surgical data. |
Table I.
Patient and surgical data.
| Parameter | Group C (n=20) | Group L (n=20) | P-value |
|---|
| Age (years) | 40.6±8.3 | 41.1±7.4 | 0.826 |
| Weight (kg) | 59.1±5.1 | 58.2±4.9 | 0.552 |
| Body height
(cm) | 162.3±3.8 | 161.4±3.1 | 0.412 |
| Surgery duration
(min) | 54.9±20.7 | 53.2±18.5 | 0.792 |
| Duration of
anaesthesia (min) | 59.4±21.8 | 59.9±16.7 | 0.936 |
| Duration of
pneumoperitoneum (min) | 44.3±17.9 | 45.4±18.8 | 0.844 |
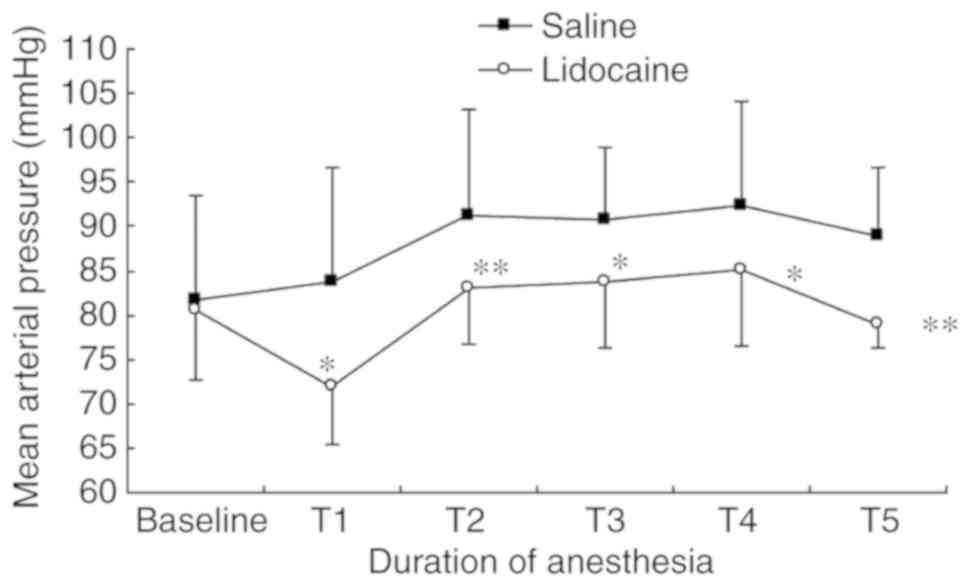
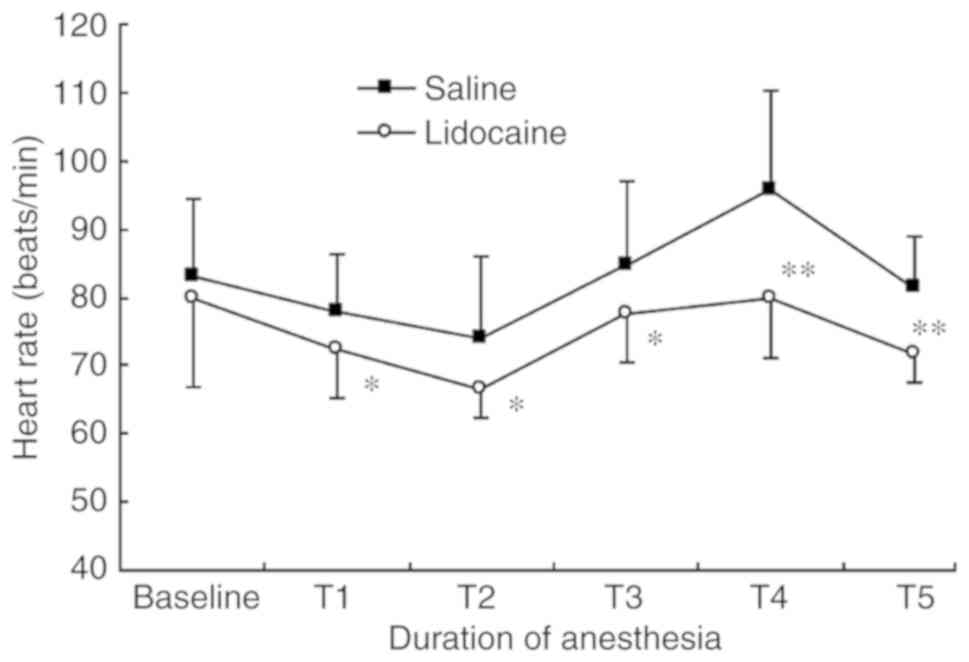
Peri-operative remifentamil dose, mean
arterial pressure and heart rate are lower in the lidocaine
group
The total dose of remifentanil administered
peri-operatively to patients in the lidocaine group was
significantly lower than that given to the saline group:
472.5±134.2 µg (saline) vs. 167.5±94.9 µg (P<0.001). Despite the
decreased use of remifentanil, the mean arterial pressure and heart
rate at the time-points T1-T5 were lower in the lidocaine group
than those in the saline group (Figs.
1 and 2).
Patients in Group C recover quickly
compared with those in Group L
The recovery and extubation times were shorter in
Group C than they were in Group L (Table II). The first flatus time (1,752±342
min) and the defecation time (1,972±363 min) in Group C were longer
than those in Group L (1,452±273 and 1,664±353 min, respectively),
but the length of the hospital stay was not significantly shorter
in Group L (P=0.32; Table II).
 | Table II.Peri-operative parameters. |
Table II.
Peri-operative parameters.
| Parameter | Group C (n=20) | Group L (n=20) | P-value |
|---|
| Recovery time
(min) | 7.4±4.3 | 11.7±4.9 | 0.005 |
| Extubation time
(min) | 12.1±3.8 | 16.8±3.2 | <0.001 |
| Peri-operative
remifentanil usage (µg) | 472.5±134.2 | 167.5±94.9 | <0.001 |
| First flatus time
(min) | 1,752±342 | 1,452±273 | 0.004 |
| Defecation time
(min) | 1,972±363 | 1,664±353 | 0.009 |
| Discharge time
(days) | 7.2±1.8 | 6.7±1.3 | 0.325 |
PONV incidence is similar in the two
groups
There were no significant differences in the
incidence of PONV between the groups at 1 and 24 h after surgery;
however, the incidence of PONV was significantly lower at 6 h after
surgery in Group L compared with that in Group C. The severity of
PONV was not significantly different between the groups at any
given time-point. Compared to Group C, fewer anti-emetic agents
were used in Group L (Table
III).
 | Table III.Details regarding PONV. |
Table III.
Details regarding PONV.
| Parameter | Group C (n=20) | Group L (n=20) | P-value |
|---|
| Patients with
symptoms of PONV at specific time-points (h) |
| 1 | 7 (35) | 4 (20) | 0.288 |
| 6 | 10 (50) | 4 (20) | 0.047 |
| 24 | 2 (10) | 1 (5) | 0.999 |
| Nausea
(none/mild/moderate/severe) at specific time-points (h) |
| 1 | 13/5/2/0 | 16/3/1/0 | 0.288 |
| 6 | 10/6/3/1 | 16/3/1/0 | 0.047 |
| 24 | 18/2/0/0 | 19/1/0/0 | 0.999 |
| Anti-emetics usage
(%) | 8 (40) | 3 (15) | 0.077 |
Patients in Group C have a faster
recovery time compared with those in Group L
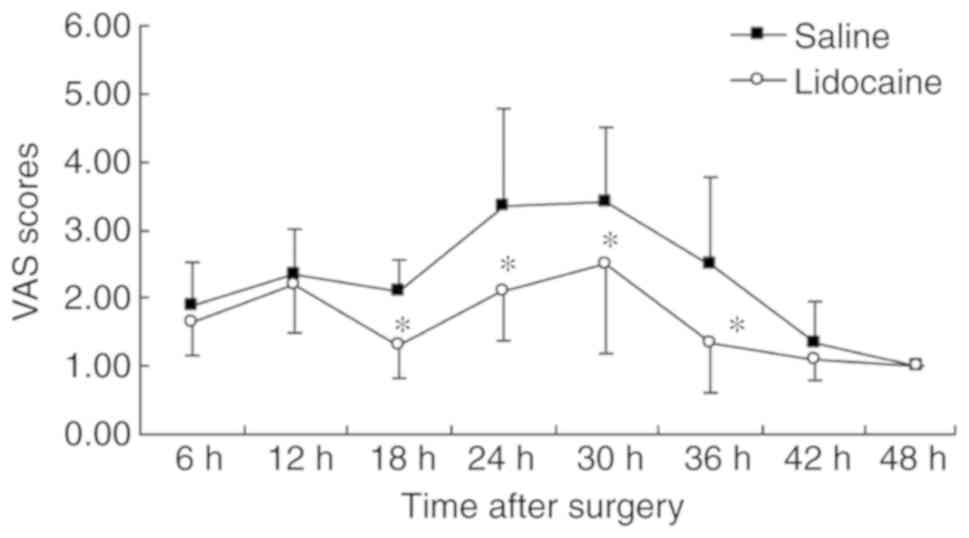
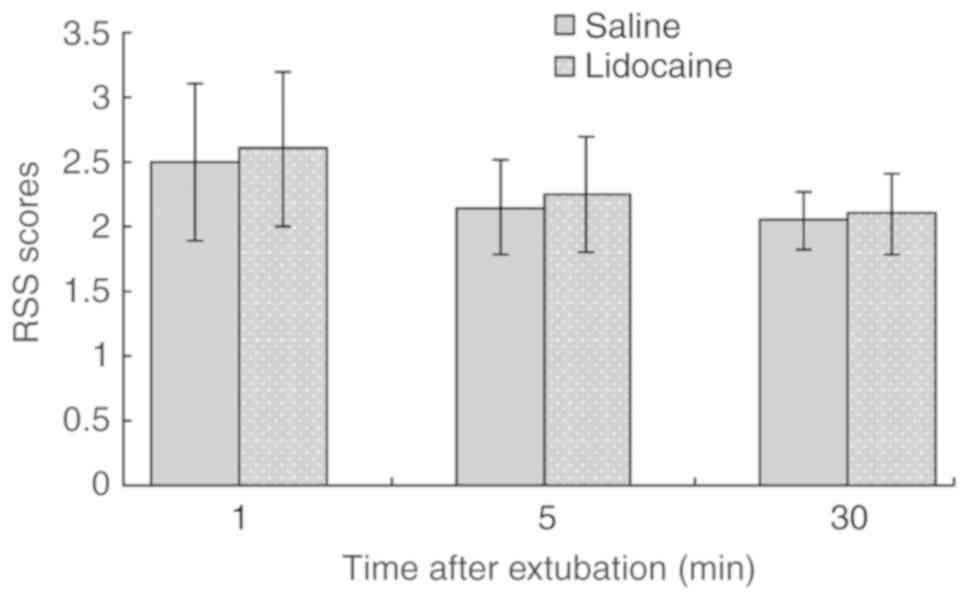
The VAS scores in Group L were lower compared with
those in Group C at 18, 24, 30 and 36 h after the operation. The
RSS score was not significantly different between the groups at any
time-point after extubation (Figs. 3
and 4). The QoR-40 scores of Group C
were significantly lower compared with those of Group L at 1 and 3
days after the operation. No significant difference was observed at
5 days (Table IV).
 | Table IV.Quality of recovery score in the two
groups. |
Table IV.
Quality of recovery score in the two
groups.
| Parameter | Group C (n=20) | Group L (n=20) | P-value |
|---|
| 1 day prior to
operation | 191.2±3.8 | 191.4±3.4 | 0.862 |
| 1 day
post-operatively | 166.3±8.2 | 173.0±9.8 | 0.025 |
| 3 days
post-operatively | 179.5±5.9 | 183.3±6.5 | 0.046 |
| 5 days
post-operatively | 189.2±4.3 | 189.3±5.6 | 0.949 |
Discussion
PONV more frequently occurs in cases with the
presence of peri-operative haemodynamic instability and in female
patients, non-smokers and patients with past histories of PONV or
motion sickness (5). General
anaesthesia with inhalational anaesthetics or nitrous oxide with
the peri-operative use of opioids may increase nausea and vomiting
(26). Laparoscopic gynaecological
surgery is more likely to cause PONV (2), which led to the choice of this type of
surgery for the present study. According to a previous study, there
was no significant difference in the incidence of PONV when the
duration of anaesthesia was 30–90 min. The incidence increased
significantly after 90 min (27).
Therefore, patients with a duration of anaesthesia between 30 and
90 min were selected for the present study.
Lidocaine is a commonly used local anaesthetic and
anti-arrhythmic drug. It reversibly inhibits the generation and
propagation of action potentials by blocking sodium currents,
resulting in sedative and antalgic effects (28). A study by Kaba et al (16) indicated that the induction of
anaesthesia with an intravenous administration of 1.5 mg/kg
lidocaine and the maintenance of anaesthesia with 2.0 mg/kg/h
lidocaine until the end of the surgery result in plasma
concentrations of lidocaine reaching 2.4±0.6 µg/ml, which is
effective for pain control. It is lower than the toxic plasma
concentration of lidocaine (5 µg/ml) (29). Therefore, the manner of
administration of lidocaine in the present study was safe.
The present study indicated that the use of opioids
in the lidocaine group was less than that in the control group,
consistent with the results of a previous study (30). Intravenous lidocaine may inhibit the
discharge of neurons and fibres by blocking sodium channels
(31) and reduce the threshold of
peripheral noxious stimulation to achieve analgesic and pain
desensitization effects (32). In
addition, intravenous lidocaine may inhibit G protein-coupled
receptors, N-methyl-D-aspartate receptors, the release of
inflammatory factors and the function of leukocytes. Therefore, it
has anti-inflammatory, analgesic, anti-hyperalgesic and immune
regulatory effects (33–36). A previous study indicated that the
major mechanism of the anaesthetic action of propofol is the
inhibition of sodium channels in the central nervous system, and
lidocaine is able to enhance the effect of propofol by also
inhibiting sodium channels (37).
The present study indicated that the blood pressure and heart rate
were lower but more consistent in the lidocaine group than they
were in the control group at all time-points. Although the recovery
and extubation times were longer in the lidocaine group than those
in the control group, the RSS score was not significantly different
between the two groups after extubation. A probable reason for this
was that the patients in the lidocaine group were more tolerant to
catheter stimulation, but it did not affect the sobriety after
extubation. The haemodynamics of the patients in the lidocaine
group were more consistent at the time of extubation and during the
recovery period, and the patients also felt more comfortable. This
may be due to the sedative, analgesic and stress-reducing effects
of lidocaine (29,38).
The half-life of lidocaine is 1.5–2.0 h with
continuous intravenous infusion. A previous study by Koppert et
al (39) indicated that the
analgesic effect of intravenous lidocaine lasted for almost 72 h
after the surgery. The present study indicated that continuous
infusion of lidocaine is able to significantly relieve
post-operative pain, and the greatest difference in pain was
observed between 12 and 42 h after surgery. This may occur due to
the pain of endoscopic surgery being relatively less than that
associated with invasive surgery, and the greatest pain had passed
at 2 days after the surgery. In addition, most patients refused to
endure the acute pain and requested post-operative analgesia in the
preliminary experiment. In order to enhance the comfort level of
patients and reduce doctor-patient disputes, patients in two groups
were intravenously given flurbiprofen axetil (1 mg/kg) for
post-operative analgesia at the end of the operation (40). The half-life of flurbiprofen axetil
is ~5.8 h (41), and therefore, the
pain within the first 6 h after the operation was not evaluated.
This is also a shortcoming of the present study. Therefore, it is
necessary to further investigate the analgesic effect of lidocaine
on the acute pain period within 6 h after surgery.
The damage of intestinal function after surgery is
associated with post-operative systemic inflammatory responses. A
previous study by Kuo et al (42) indicated that intravenous lidocaine
may reduce pro-inflammatory factors and is beneficial to the
recovery of intestinal function. Furthermore, stimuli including
intra-operative traction and pneumoperitoneal pressure may activate
the intestinal nerve plexus, leading to injury of intestinal
function. Intravenous lidocaine may excite the intestinal smooth
muscle by blocking the mesenteric plexus and is beneficial to the
recovery of intestinal function (14). In the present study, the first flatus
and defecation times were earlier in the lidocaine group than they
were in the control group, indicating that lidocaine is helpful in
the early recovery of intestinal function.
The results of the present study suggested that the
incidence of PONV was significantly lower in the lidocaine group
than that in the control group, and the severity PONV was also
significantly reduced. This may be due to the following factors:
Improvement of the senses of patients during the recovery period
from anaesthesia, reduction of the use of opioid agents,
maintenance of haemodynamic stability during the peri-operative
stage, reduction of post-operative pain and promotion of the early
recovery of the gastrointestinal tract. However, the mechanism by
which lidocaine prevents PONV remains elusive.
QOR40 is an effective, reliable and simple scale
used to evaluate the quality of the post-operative recovery of
patients. It has been successfully used to assess the quality of
post-operative recovery in different patients and after different
types of surgery, including heart surgery, laparoscopic gallbladder
surgery and joint replacement surgery (43–45). The
present study indicated that the recovery quality was much better
in the lidocaine group than that in the control group at 1 and 3
days after surgery. However, the recovery quality was not
significantly different between the groups at 5 days after surgery.
Therefore, intravenous lidocaine may accelerate the early recovery
of patients undergoing endoscopic gynaecological surgery. This
promotion of early recovery may be associated with the beneficial
effects of lidocaine mentioned above. However, the definite
duration and efficiency of the promotion of post-operative recovery
by lidocaine remain elusive. In addition, in the present study,
patients with small surgical trauma, short operation times and good
general health were selected. Therefore, further studies are
required to determine whether lidocaine has the same effect on
patients with comparatively greater surgical trauma, longer
operation times and poor general health.
In conclusion, intravenous lidocaine used in
patients undergoing laparoscopic gynaecological surgery may safely
and effectively prevent PONV, and it may promote patients' early
recovery, thus making it worthwhile to increase the use of
lidocaine in the clinical setting.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YJZ conceived the study and revised the manuscript.
TW wrote the manuscript. HL processed and analysed the data, and
was involved in designing the study. TW, LW and HJS performed the
experiments and collected the data. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of the Affiliated Hospital of Yangzhou University
(Yangzhou, China) and all subjects provided written informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Buia A, Stockhausen F and Hanisch E:
Laparoscopic surgery: A qualified systematic review. World J
Methodol. 5:238–254. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gan TJ: Risk factors for postoperative
nausea and vomiting. Anesth Analg. 102:1884–1898. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Franck M, Radtke FM, Apfel CC, Kuhly R,
Baumeyer A, Brandt C, Wernecke KD and Spies CD: Documentation of
post-operative nausea and vomiting in routine clinical practice. J
Int Med Res. 38:1034–1041. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Choi DH, Ko JS, Ahn HJ and Kim JA: A
Korean predictive model for postoperative nausea and vomiting. J
Korean Med Sci. 20:811–815. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Apfel CC, Heidrich FM, Jukar-Rao S, Jalota
L, Hornuss C, Whelan RP, Zhang K and Cakmakkaya OS: Evidence-based
analysis of risk factors for postoperative nausea and vomiting. Br
J Anaesth. 109:742–753. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu O, Belo SE and Koutsoukos G: Additive
antiemetic efficacy of prophylactic ondansetron with droperidol in
out-patient gynecological laparoscopy. Can J Anaesth. 47:529–536.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Achuthan S, Singh I, Varthya SB,
Srinivasan A, Chakrabarti A and Hota D: Gabapentin prophylaxis for
postoperative nausea and vomiting in abdominal surgeries: A
quantitative analysis of evidence from randomized controlled
clinical trials. Br J Anaesth. 114:588–597. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Apfel CC: Postoperative nausea and
vomiting. Miller's anesthesia. 7th. Miller RD: Churchill
Livingstone; Philadelphia, PA: pp. 2729–2755. 2010, View Article : Google Scholar
|
|
9
|
Swaika S, Pal A, Chatterjee S, Saha D and
Dawar N: Ondansetron, ramosetron, or palonosetron: Which is a
better choice of antiemetic to prevent postoperative nausea and
vomiting in patients undergoing laparoscopic cholecystectomy?
Anesth Essays Res. 5:182–186. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shaikh SI, Nagarekha D, Hegade G and
Marutheesh M: Postoperative nausea and vomiting: A simple yet
complex problem. Anesth Essays Res. 10:388–396. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Herminghaus A, Wachowiak M, Wilhelm W and
Gottschalk A, Eggert K and Gottschalk A: Intravenous administration
of lidocaine for perioperative analgesia. Review and
recommendations for practical usage. Anaesthesist. 60:152–160.
2011.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jendoubi A, Naceur IB, Bouzouita A, Trifa
M, Ghedira S, Chebil M and Houissa M: A comparison between
intravenous lidocaine and ketamine on acute and chronic pain after
open nephrectomy: A prospective, double-blind, randomized,
placebo-controlled study. Saudi J Anaesth. 11:177–184. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Weibel S, Jokinen J, Pace NL, Schnabel A,
Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Afshari A and
Kranke P: Efficacy and safety of intravenous lidocaine for
postoperative analgesia and recovery after surgery: A systematic
review with trial sequential analysis. Br J Anaesth. 116:770–783.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tikuišis R, Miliauskas P, Samalavičius NE,
Žurauskas A, Samalavičius R and Zabulis V: Intravenous lidocaine
for post-operative pain relief after hand-assisted laparoscopic
colon surgery: A randomized, placebo-controlled clinical trial.
Tech Coloproctol. 18:373–380. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
McKay A, Gottschalk A, Ploppa A, Durieux
ME and Groves DS: Systemic lidocaine decreased the perioperative
opioid analgesic requirements but failed to reduce discharge time
after ambulatory surgery. Anesth Analg. 109:1805–1808. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kaba A, Laurent SR, Detroz BJ, Sessler DI,
Durieux ME, Lamy ML and Joris JL: Intravenous lidocaine infusion
facilitates acute rehabilitation laparoscopic colectomy.
Anesthesiology. 106:11–18. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lauwick S, Kim DJ, Mistraletti G and Carli
F: Functional walking capacity as an outcome measure of
laparoscopic prostatectomy: The effect of lidocaine infusion. Br J
Anaesth. 103:213–219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lauwick S, Kim DJ, Michelagnoli G,
Mistraletti G, Feldman L, Fried G and Carli F: Intraoperative
infusion of lidocaine reduces postoperative fentanyl requirements
in patients undergoing laparoscopic cholecystectomy. Can J Anaesth.
55:754–760. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Grady MV, Mascha E, Sessler DI and Kurz A:
The effect of perioperative intravenous lidocaine and ketamine on
recovery after abdominal hysterectomy. Anesth Analg. 115:1078–1084.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Myles PS, Weitkamp B, Jones K, Melick J
and Hensen S: Validity and reliability of a postoperative quality
of recovery score: The QoR-40. Br J Anaesth. 84:11–15. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gornall BF, Myles PS, Smith CL, Burke JA,
Leslie K, Pereira MJ, Bost JE, Kluivers KB, Nilsson UG, Tanaka Y
and Forbes A: Measurement of quality of recovery using the QoR-40:
A quantitative systematic review. Br J Anaesth. 111:161–169. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Aronson WL, McAuliffe MS and Miller K:
Variability in the American society of anesthesiologists physical
status classification scale. AANA J. 71:265–274. 2003.PubMed/NCBI
|
|
23
|
Ramsay MA, Savege TM, Simpson BR and
Goodwin R: Controlled sedation with alphaxalone-alphadolone. Br Med
J. 2:656–659. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Carlsson AM: Assessment of chronic pain.
I. Aspects of the reliability and validity of the visual analogue
scale. Pain. 16:87–101. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Eberhart LH, Seeling W, Ulrich B, Morin AM
and Georgieff M: Dimenhydrinate and metoclopramide alone or in
combination for prophylaxis of PONV. Can J Anaesth. 47:780–185.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Phillips C, Brookes CD, Rich J, Arbon J
and Turvey TA: Postoperative nausea and vomiting following
orthognathic surgery. Int J Oral Maxillofac Surg. 44:745–751. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sinclair DR, Chung F and Mezei G: Can
postoperative nausea and vomiting be predicted? Anesthesiology.
91:109–118. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cardoso FC and Lewis RJ: Sodium channels
and pain: From toxins to therapies. Br J Pharmacol. 175:2138–2157.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lauretti GR: Mechanisms of analgesia of
intravenous lidocaine. Rev Bras Anestesiol. 58:280–286. 2008.(In
English). View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nakhli MS, Kahloul M, Guizani T, Zedini C,
Chaouch A and Naija W: Intravenous lidocaine as adjuvant to general
anesthesia in renal surgery. Libyan J Med. 13:14334182018.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kalso E: Sodium channel blockers in
neuropathic pain. Curr Pharm Des. 11:3005–3011. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kawamata M, Sugino S, Narimatsu E,
Yamauchi M, Kiya T, Furuse S and Namiki A: Effects of systemic
administration of lidocaine and QX-314 on hyperexcitability of
spinal dorsal horn neurons after incision in the rat. Pain.
122:68–80. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hahnenkamp K, Durieux ME, Hahnenkamp A,
Schauerte SK, Hoenemann CW, Vegh V, Theilmeier G and Hollmann MW:
Local anaesthetics inhibit signalling of human NMDA receptors
recombinantly expressed in Xenopus laevis oocytes: Role of protein
kinase C. Br J Anaesth. 96:77–87. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sugimoto M, Uchida I and Mashimo T: Local
anaesthetics have different mechanisms and sites of action at the
recombinant N-methyl-D aspartate (NMDA) receptors. Br J Pharmacol.
138:876–882. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yousefshahi F, Predescu O and Asenjo JF:
The efficacy of systemic lidocaine in the management of chronic
pain: A literature review. Anesth Pain Med. 7:e447322017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yardeni IZ, Beilin B, Mayburd E, Levinson
Y and Bessler H: The effect of perioperative intravenous lidocaine
on postoperative pain and immune function. Anesth Analg.
109:1464–1469. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hans GA, Lauwick SM, Kaba A, Bonhomme V,
Struys MM, Hans PC, Lamy ML and Joris JL: Intravenous lidocaine
infusion reduces bispectral index-guided requirements of propofol
only during surgical stimulation. Br J Anaesth. 105:471–479. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ahn E, Kang H, Choi GJ, Park YH, Yang SY,
Kim BG and Choi SW: Intravenous lidocaine for effective pain relief
after a laparoscopic colectomy: A prospective, randomized,
double-blind, placebo-controlled study. Int Surg. 100:394–401.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Koppert W, Weigand M, Neumann F, Sittl R,
Schuettler J, Schmelz M and Hering W: Perioperative intravenous
lidocaine has preventive effects on postoperative pain and morphine
consumption after major abdominal surgery. Anesth Analg.
98:1050–1055. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang J, Zhang H, Zhao L, Gu J, Feng Y and
An H: Population pharmacokinetic modeling of flurbiprofen, the
active metabolite of flurbiprofen axetil, in Chinese patients with
postoperative pain. J Pain Res. 11:3061–3070. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Fujii Y and Itakura M: Comparison of
lidocaine, metoclopramide, and flurbiprofen axetil for reducing
pain on injection of propofol in Japanese adult surgical patients:
A prospective, randomized, double-blind, parallel-group,
placebo-controlled study. Clin Ther. 30:280–286. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kuo CP, Jao SW, Chen KM, Wong CS, Yeh CC,
Sheen MJ and Wu CT: Comparison of the effects of thoracic epidural
analgesia and i.v. infusion with lidocaine on cytokine response,
postoperative pain and bowel function in patients undergoing
colonic surgery. Br J Anaesth. 97:640–646. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Myles PS, Hunt JO, Fletcher H, Solly R,
Woodward D and Kelly S: Relation between quality of recovery in
hospital and quality of life at 3 months after cardiac surgery.
Anesthesiology. 95:862–867. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Murphy GS, Szokol JW, Greenberg SB, Avram
MJ, Vender JS, Nisman M and Vaughn J: Preoperative dexamethasone
enhances quality of recovery after laparoscopic cholecystectomy:
Effect on in-hospital and postdischarge recovery outcomes.
Anesthesiology. 114:882–890. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Poitras S, Beaule PE and Dervin GF:
Validity of a short-term quality of life questionnaire in patients
undergoing joint replacement: The quality of recovery-40. J
Arthroplasty. 27:1604–1608. 2012. View Article : Google Scholar : PubMed/NCBI
|