Introduction
Multiple organ dysfunction syndrome (MODS), a final
stage of numerous fatal infections and non-infectious diseases, is
the leading cause of death in critically ill patients (1). It is widely thought that an
uncontrolled inflammatory response is the pathophysiological basis
of MODS. Inflammatory mediators, including interleukin (IL)-6, IL-8
and tumor necrosis factor (TNF)-α, cause tissue damage, blood
hypercoagulability and microcirculation disturbances, thereby
leading to MODS and multiple organ failure (2–5).
Therefore, eliminating or reducing the level of inflammatory
factors is the key in the prevention and treatment of MODS.
For >70 years, renal replacement therapy has been
used to treat patients with acute renal injury. Recently,
continuous blood purification (CBP) for the treatment of patients
with non-renal diseases has drawn increasing attention, and has
been widely used in various clinical departments, including
critical care medicine units (6).
The aim of CBP in the treatment of non-renal diseases is to
maintain the blood volume (e.g., in cases of heart failure),
eliminate toxins, restore the electrolyte balance, control the body
temperature and eliminate inflammatory mediators (7). Critical illness, usually accompanied by
MODS, is characterized by diverse causes, rapid progression and a
complicated pathophysiology (8). At
times, it is difficult for clinicians to perform the CBP procedure
for these patients. It has been indicated that, while it improves
the prognosis of patients, early CBP treatment may cause
complications, including hypotension, coagulation dysfunction,
nutrition and therapeutic drug loss and catheter-associated
infections (9). At present, there is
no standard regarding the suitable timing for CBP treatment
(10), which needs to be determined
for critically ill patients.
There is a positive correlation between Acute
Physiology And Chronic Health Evaluation (APACHE) II, a scoring
system used to evaluate the severity of a patient's illness, and
the risk of mortality (11,12). Other scoring systems, including MODS
and systemic inflammatory response syndrome (SIRS), are also used
to evaluate the severity of a patient's illness (13–16). In
the present study, the clinical data of critically ill patients who
had been admitted to the intensive care unit (ICU) were
retrospectively reviewed and the value of the APACHE II score in
guiding early CBP treatment was investigated.
Materials and methods
Patients
The present study included a total of 115 critically
ill patients admitted to the ICU of the First Hospital of Wuhan
(Wuhan, China) from January 2013 to December 2016. The inclusion
criteria were as follows: i) An APACHE II score of >15 points;
and ii) no history of any obvious organ dysfunction. Exclusion
criteria included i) allergic reaction to the filter or the refusal
of blood transfusion and ii) the time from ICU admission to death
was <24 h. All patients were provided with the appropriate
treatment according to the primary disease, e.g., anti-infection,
organ function support, liquid management or nutritional support.
The current study was approved by the Ethics Committee of the First
Hospital of Wuhan (Wuhan, China). Written informed consent was
obtained from all patients or their parents or next of kin.
Experimental design
The patients enrolled were divided into 3 groups
based on their APACHE II score on the first day at the ICU. The
patients in group A had an APACHE II score of 15–19, while those in
group B had a score of 20–29 points and those in group C had a
score of ≥30 points. These APACHE II scores were arbitrarily
selected to group the patients based on an analysis of the clinical
data from critically patients over the last five years. Each group
was then further divided into 2 subgroups depending on whether the
patients received CBP treatment or not. Patients in groups A1, B1
and C1 received CBP treatment, while patients in groups A2, B2 and
C2 did not.
CBP treatment
A single needle double lumen catheter was inserted
into the femoral vein or internal jugular vein for the
establishment of an extracorporeal circulation. All patients in the
first group (group 1) underwent pre-dilution continuous veno-venous
hemofiltration (CVVH) and received blood purification. CVVH was
performed using the Fresenius multiFitrate system and Ultraflux
AV600S hemofilters (Fresenius Medical Care, Bad Homburg v.d.H.,
Germany). The blood flow rate was 150–200 ml/min and the
displacement fluid velocity was 2,000–3,500 ml/h. CVVH was
performed at a dose of 30 ml/kg/h. The volume load of the patients
was dynamically assessed to adjust the liquid balance and the
results of the blood gas analysis and biochemical examination were
monitored. For anti-coagulation, patients with no elevated risk of
bleeding were treated with heparin with a loading dose of 10–50
U/kg and a loading speed of 2.5–20 U/min to maintain the activated
partial thromboplastin time at 30–60 sec. Patients with an elevated
risk of bleeding or with bleeding were treated with non-heparin
anti-coagulants.
Cytokine measurement
Plasma levels of inflammatory proteins [endotoxin
and procalcitonin (PCT)] in patients were measured prior to or 72 h
after CBP treatment using an automatic biochemical analyzer
(HF-240; Jinan Chinese Medical Instrument Ltd., Jinan, China).
Plasma levels of cytokines were detected using TNF-α (cat. no.
EK0525), IL-6 (cat. no. EK0410) and IL-8 (cat. no. EK0413) ELISA
kits supplied by Wuhan Boster Biological Technology, Ltd. (Wuhan,
China).
Severity scoring
Severity scoring was performed every 24 h using
APACHE II, MODS and SIRS ICU scoring systems (14,17,18). The
APACHE II score for each patient was determined on the first day at
the ICU. The incidence of MODS and mortality were recorded two
weeks after admission to the ICU. The length of stay at the ICU was
also recorded.
Statistical analysis
Statistical analysis was performed using SPSS 18
statistical software (SPSS, Inc., Chicago, IL, USA). Values are
expressed as the mean ± standard deviation. Student's t-test was
used to determine differences between the two groups. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient characteristics
A total of 115 patients with critical illness, of
which 60 were male and 55 were female, were enrolled in the present
study. The characteristics of the patients are listed in Table I. There was no significant difference
in gender, age, primary disease, course of disease, basic renal
function and cardiac function between groups A1 and A2, B1 and B2,
or C1 and C2 (P>0.05). Of note, treatments given to patients
based on the primary disease were not different between groups
(A1-C1 vs. A2-C2). Steroids were not used in the patients of this
cohort.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
|
|
|
|
| Primary disease |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|---|
| Group | n | Gender (M/F) | Age (years) | SAP n (%) | Sepsis n (%) | ARDS n (%) | Other n (%) | Disease course
(days) | Cr (µmol/l) | BUN (mmol/l) | NT-proBNP (ng/l) |
|---|
| A1 | 19 | 10/9 | 56±14 | 4 (21.1) | 9 (47.3) | 4 (21.1) | 2 (10.5) | 2.4±1.3 | 152.3±21.4 | 14.7±4.4 | 14,136±396.4 |
| A2 | 19 | 10/9 | 54±15 | 4 (21.1) | 10 (52.6) | 4 (21.1) | 1 (5.3) | 2.5±1.4 | 154.5±22.1 | 14.9±4.5 | 14,251±399.3 |
| B1 | 19 | 9/10 | 57±13 | 4 (21.1) | 9 (47.3) | 5 (26.3) | 1 (5.3) | 2.6±1.2 | 150.6±25.2 | 14.4±4.9 | 14,521±432.6 |
| B2 | 20 | 10/10 | 55±13 | 5 (26.3) | 10 (52.6) | 4 (21.1) | 1 (5.3) | 2.5±1.3 | 149.3±24.8 | 14.8±5.2 | 14,462±396.5 |
| C1 | 19 | 10/9 | 56±14 | 4 (21.1) | 9 (47.3) | 4 (21.1) | 2 (10.5) | 2.6±1.4 | 156.9±24.9 | 15.1±4.3 | 14,568±387.8 |
| C2 | 19 | 9/10 | 56±13 | 4 (21.1) | 8 (42.1) | 5 (26.3) | 2 (10.5) | 2.6±1.3 | 156.1±25.1 | 15.2±5.2 | 14,606±406.4 |
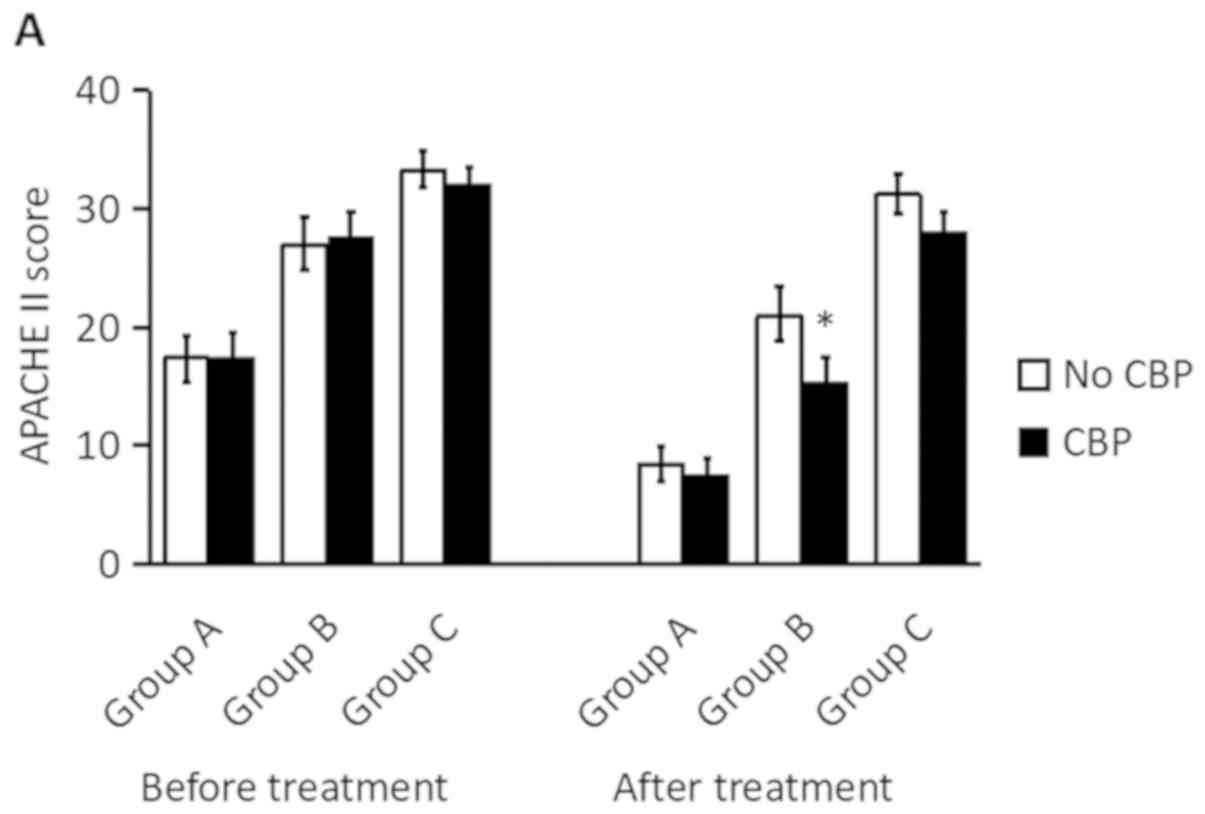
Effect of CBP treatment on the
severity scores of critically ill patients
To determine whether the APACHE II score prior to
treatment was associated with the outcome, the APACHE II, MODS and
SIRS severity scores of the critically ill patients were recorded
at 72 h after treatment. As presented in Fig. 1, as expected, the APACHE II, MODS and
SIRS scores were decreased at 72 h after treatment with CBP
compared with those without treatment, which suggests a clinical
improvement after treatment with CBP in all groups. It was observed
that patients with lower APACHE II, MODS or SIRS scores
demonstrated a greater improvement than those with higher scores,
i.e., the scores in patient group A exhibited a larger decrease
after treatment compared with those in group C.
It was then assessed which group of patients
benefited the most from CBP. As presented in Fig. 1, CBP treatment did not provide a
significant benefit for patients with an APACHE II score of 15–19
(Group A) or >30 points (Group C): The improvement in the APACHE
II, MODS or SIRS score for patients receiving CBP treatment (Group
A1 or C1) was not significantly different from that of patients who
did not (Group A2 or C2). However, for patients with an APACHE II
score between 20 and 29 (Group B), CBP treatment significantly
decreased the APACHE II, MODS and SIRS scores when compared with
those of patients who did not (P<0.05, B1 vs. B2). Taken
together, these results suggest that CBP treatment has a
differential effect on patients with different APACHE II
scores.
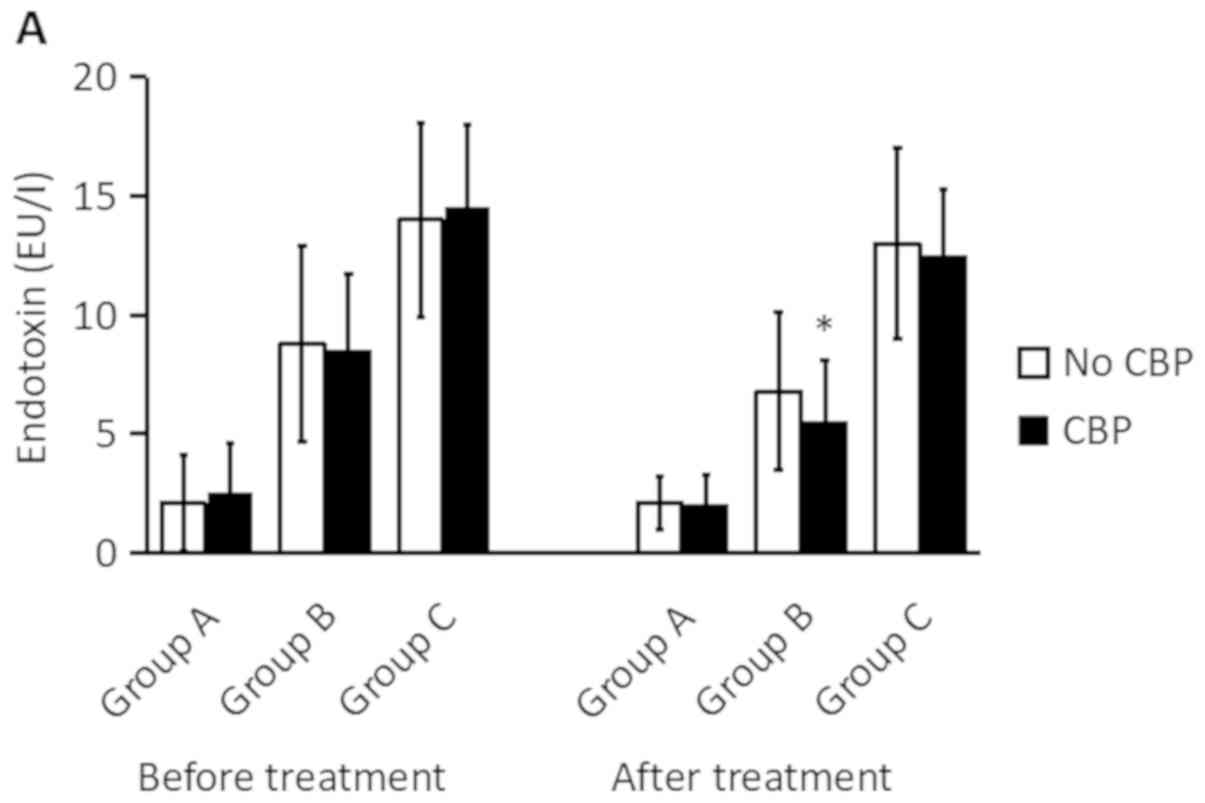
Effect of CBP treatment on the plasma
levels of inflammatory proteins in critically ill patients
Next, it was assessed whether CBP treatment affected
the levels of inflammatory proteins and cytokines in patients with
different APACHE II scores treated with or without CBP. As
presented in Fig. 2, it appeared
that treatment for 72 h slightly decreased the levels of endotoxin
and PCT in each group. The results indicated that in groups A and
C, there was no significant difference in the endotoxin levels
between patients treated with or without CBP. By contrast, for
patients in group B, CBP treatment significantly decreased the
endotoxin levels (P<0.05, B1 vs. B2; Fig. 2A). Regarding the levels of PCT, while
CBP did not achieve any significant improvement in patient group A
(P>0.05, A1 vs. A2), the level of PCT in groups B and C was
significantly lower in patients who received CBP treatment
(P<0.05, B1 vs. B2 or C1 vs. C2; Fig.
2B).
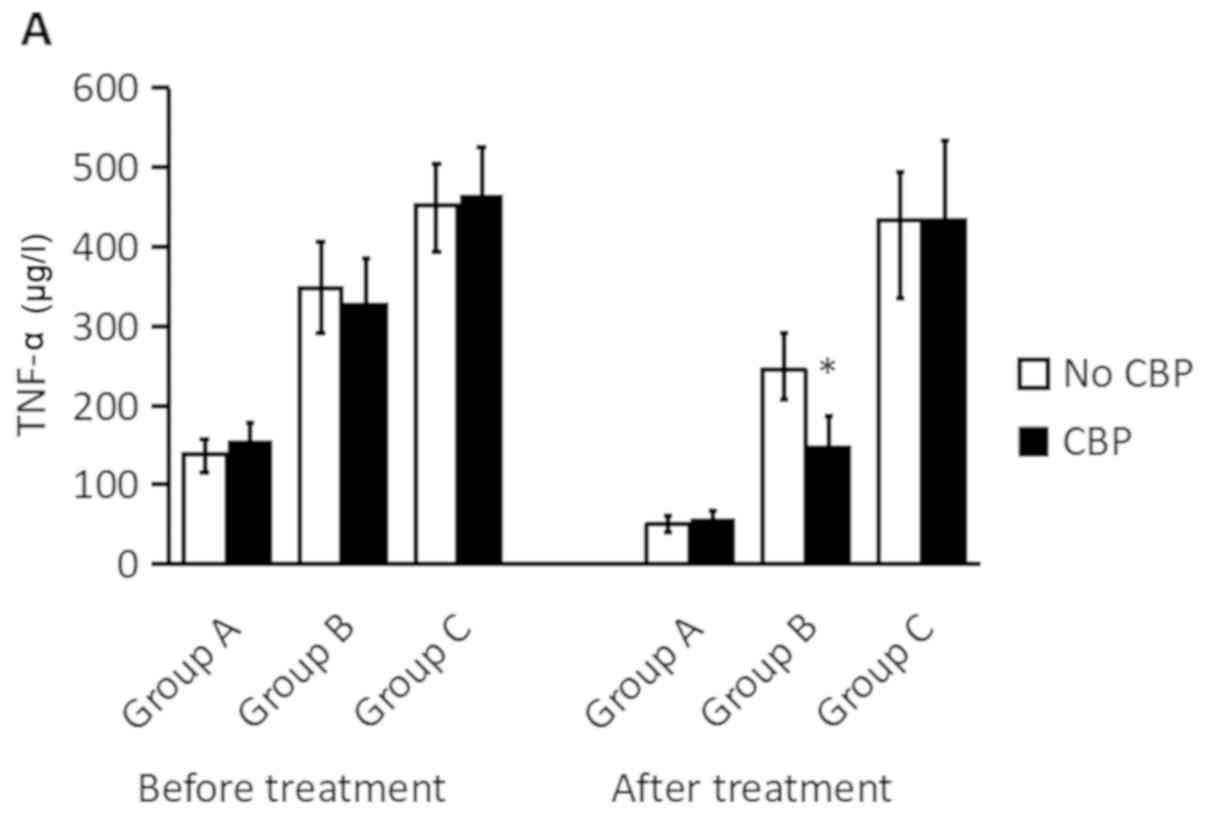
Regarding the inflammatory cytokine levels, CBP
treatment did not significantly improve the levels of TNF-α, IL-6
or IL-8 in patient group A, while CBP treatment significantly
decreased the levels of IL-6 and IL-8 in patient group B and C
(P<0.05, B1 vs. B2 or C1 vs. C2; Fig.
3). Taken together, these results suggest that CBP treatment
preferentially impacts patients with APACHE II scores of 20–29 and
>30.
Effect of CBP treatment on clinical
indicators in critically ill patients
Given the improved severity scores and reduced
levels of pro-inflammatory proteins and cytokines by CBP treatment
in patient group B, the present study then aimed to determine
whether CBP treatment improves other clinical indicators. For this,
the occurrence of MODS, the mortality rate and the length of stay
at the ICU in these three patient groups was determined. As
presented in Table II, after 2
weeks of treatment, the mortality rate and the occurrence of MODS
were was significantly lower in patient groups B and C who received
CBP treatment than in those who received no CBP treatment
(P<0.05). In addition, the length of stay at the ICU was shorter
for patient groups B and C who received CBP treatment than those
without CBP treatment (P<0.05; Table
II). Furthermore, the percentage of cases with MODS was
slightly but not significantly reduced in group B1 vs. B2. In the
patients of groups A and C, CBP treatment did not significantly
affect the percentage of cases of MODS, the mortality rate and the
length of stay at the ICU (Table
II).
 | Table II.Effect of CBP treatment on clinical
indicators. |
Table II.
Effect of CBP treatment on clinical
indicators.
|
|
| Clinical
Indicators |
|---|
|
|
|
|
|---|
| Group | n | MODS n (%) | Mortality n
(%) | Length of ICU stay
(days) |
|---|
| A1 | 19 | 5 (26.3) | 2 (10.5) | 5.5±1.6 |
| A2 | 19 | 6 (31.5) | 2 (10.5) | 4.5±1.4 |
| B1 | 19 | 6
(26.3)a | 2
(10.5)a |
8.2±3.8a |
| B2 | 20 | 11 (55.0) | 4 (40.0) | 11.9±3.7 |
| C1 | 19 | 9
(47.4)a | 5
(26.3)a |
11.5±4.2a |
| C2 | 19 | 14 (73.7) | 10 (52.6) | 14.0±3.8 |
Discussion
A systemic inflammatory response is common in
critically ill patients (19). When
it is excessive or out of control, inflammation causes severe
tissue damage (1). It has been
reported that the plasma levels of IL-6 and TNF-α are associated
with the severity of the disease (20). Among cytokines and inflammatory
mediators, TNF-α and IL-6 have a key role in initiating the
anti-inflammatory response (21). An
elevation of IL-6 and TNF-α stimulates the body to produce a large
number of inflammatory factors, resulting in a cascade
amplification of the inflammatory response (22). Therefore, dynamic monitoring of TNF-α
and IL-6 levels is of significance for the detection of the
occurrence and progression of MODS (23–25).
Furthermore, the prevention and treatment of any exacerbation of
SIRS is key in the treatment of critically ill patients, which may
be performed by either inhibiting the release or lowering the
levels of pro-inflammatory cytokines (26). Therefore, elimination of multiple
pro-inflammatory cytokines simultaneously and non-selectively may
have therapeutic potential in preventing the aggravation of
MODS.
As one of the most important advances in critical
care medicine in recent years, the clinical application of CBP has
been extended to the treatment of various types of critical illness
of non-renal origin, including sepsis, MODS, decompensated
cirrhosis, drug poisoning, acute decompensated heart failure and
severe acute pancreatitis (27,28).
CVVH, a widely used CBP method in the clinic, has the advantage of
clearing small- and medium-sized solutes. In the case of large
volume displacement, CVVH also removes large solute molecules
(29).
In the present study, it was observed that the
levels of plasma inflammatory cytokines (TNF-α, IL-6 and IL-8), PCT
and endotoxin were significantly lower in patients treated with CBP
(B1 and C1) than in those without CBP treatment (B2 and C2). This
result indicates that CVVH effectively eliminates these circulating
inflammatory factors. Similarly, 2 weeks after treatment, the
improvement in certain clinical indicators, including the mortality
rate and the length of stay at the ICU, in patients of the CBP
group were significantly superior to those in the group that did
not receive CBP. Of note, it appeared that CBP only provided a
significant clinical benefit for a group of patients with a certain
range of APACHE II score. It was observed that in patients with an
APACHE II score between 15 and 19, CBP did not significantly
improve the severity scores, cytokine levels, mortality rate and
length of stay at the ICU. However, for patients with an APACHE II
score of 20–29 or >30, all of the clinical indicators were
improved by CBP intervention, as indicated by reduced severity
scores and cytokine levels, a decreased mortality rate and a
shortened length of stay at the ICU. The APACHE II score represents
the disease severity and it has been demonstrated that it is
positively associated with the risk of mortality (30,31). The
results of the present study suggest that an APACHE II score of
20–29 may be regarded as a selection criterion for blood
purification treatment in the early stage of critical illness. In
order to reduce the mortality rate of critically ill patients, CBP
treatment should be performed as soon as possible. Our data showed
that patients with APPACHEII score >30 also benefit from the CBP
treatment. From the perspective of health economics and which
patient group benefit most, we believe that it is more appropriate
to perform CBP treatment when the patient's APPACHE II score is
≥20.
In summary, the present study performed a
comprehensive analysis to assess which group of critically ill
patients benefited the most from CBP treatment based on their
APACHE II score. The severity scores (APACHE II, MODS and SIRS),
the plasma levels of inflammatory proteins (endotoxin, PCT, TNF-α,
IL-6 and IL-8) and clinical parameters (mortality rate and ICU
length of stay) were measured, and it was observed that patients
with an APACHE II score of 20–29 benefited the most from CBP
treatment, which is consistent with previous observations that CBP
inhibits the inflammatory cascade amplification reaction by an
‘off-peak effect’, prevents the occurrence of MODS and reduces the
mortality rate (32,33). The present results indicate that the
APACHE II score may be used to guide the treatment of patients with
critical illness.
Acknowledgements
Not applicable.
Funding
The current study was supported by grants from the
Scientific Research Project of Medical Research Program of Hubei
Province (grant no. WJ2015MB240), the Wuhan Clinical Medical
Research Project of Hubei Province (grant no. WX15A09) and the
Wuhan Clinical Medical Research Project of Hubei Province (grant
no. WX16E24).
Availability of data and materials
All datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RXZ designed the study. WD and CLH performed the
experiments. RXZ, WD and CLH analyzed the data and prepared the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of The First Hospital of Wuhan (Wuhan, China). Written
informed consent was obtained from all patients or their next of
kin.
Patient consent for publication
Not applicable.
Competing interests
The authors declare thst they have no competing
interests.
References
|
1
|
Gong H, Sheng X, Xue J and Zhu D:
Expression and role of TNIP2 in multiple organ dysfunction syndrome
following severe trauma. Mol Med Rep. 19:2906–2912. 2019.PubMed/NCBI
|
|
2
|
Jastrow KM III, Gonzalez EA, McGuire MF,
Suliburk JW, Kozar RA, Iyengar S, Motschall DA, McKinley BA, Moore
FA and Mercer DW: Early cytokine production risk stratifies trauma
patients for multiple organ failure. J Am Coll Surg. 209:320–331.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saadia R and Schein M: Multiple organ
failure. How valid is the ‘two hit’ model? J Accid Emerg Med.
16:163–167. 1999. View Article : Google Scholar
|
|
4
|
Yao YM, Redl H, Bahrami S and Schlag G:
The inflammatory basis of trauma/shock-associated multiple organ
failure. Inflamm Res. 47:201–210. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
St John RC and Dorinsky PM: Immunologic
therapy for ARDS, septic shock, and multiple-organ failure. Chest.
103:932–943. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hanafusa N: Application of continuous
replacement therapy: What should we consider based on existing
evidence? Blood Purif. 40:312–319. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Intensive Care Society: Standards and
recommendations for the provision of renal replacement therapy on
intensive care units in the United Kingdom. Intensive Care Society.
2009.
|
|
8
|
Lee S, Hwang H, Yamal JM, Goodman JC,
Aisiku IP, Gopinath S and Robertson CS: IMPACT probability of poor
outcome and plasma cytokine concentrations are associated with
multiple organ dysfunction syndrome following traumatic brain
injury. J Neurosurg. Jan 11–2019.(Epub ahead of print). View Article : Google Scholar
|
|
9
|
Finkel KW and Podoll AS: Complications of
continuous renal replacement therapy. Semin Dial. 22:155–159. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cheng J, Hu S, Lu H, Lei Q, Liu J, Yuan F
and Chen R: Comparison of the therapeutic effectiveness of
sustained low-efficiency dialysis (SLED) with continuous blood
purification (CBP) in critically ill patients. Cell Biochem
Biophys. 67:923–927. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dehghani A, Abdeyazdan G and
Davaridolatabadi E: An overview of the predictor standard tools for
patient weaning from mechanical ventilation. Electron Physician.
8:1955–1963. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sadaka F, EthmaneAbouElMaali C, Cytron MA,
Fowler K, Javaux VM and O'Brien J: Predicting mortality of patients
with sepsis: A comparison of APACHE II and APACHE III scoring
systems. J Clin Med Res. 9:907–910. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Baue E: MOF, MODS, and SIRS: What is in a
name or an acronym? Shock. 26:438–449. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marshall JC, Cook DJ, Christou NV, Bernard
GR, Sprung CL and Sibbald WJ: Multiple organ dysfunction score: A
reliable descriptor of a complex clinical outcome. Crit Care Med.
23:1638–1652. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Baek JH, Kim MS, Lee JC and Lee JH:
Systemic inflammation response syndrome score predicts the
mortality in multiple trauma patients. Korean J Thorac Cardiovasc
Surg. 47:523–528. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
NeSmith EG, Weinrich SP, Andrews JO,
Medeiros RS, Hawkins ML and Weinrich M: Systemic inflammatory
response syndrome score and race as predictors of length of stay in
the intensive care unit. Am J Crit Care. 18:339–346. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Knaus WA, Draper EA, Wagner DP and
Zimmerman JE: APACHE II: A severity of disease classification
system. Crit Care Med. 13:818–829. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jacobs S, Zuleika M and Mphansa T: The
multiple organ dysfunction score as a descriptor of patient outcome
in septic shock compared with two other scoring systems. Crit Care
Med. 27:741–744. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou Z, Guo F and Huan J: Fournier's
gangrene with septic shock and multiple organ dysfunction syndrome.
Int J Low Extrem Wounds. 18:94–96. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zeng J: Values of detection of NF-κB
activation level combined with IL-6 and TNF-α levels in peripheral
neutrophils in the prediction of multiple organ dysfunction
syndrome in patients with severe multiple trauma. Exp Ther Med.
16:2478–2482. 2018.PubMed/NCBI
|
|
21
|
Wang F, Guan X, Yang J, He W, Wei Y, Chen
H and Li Y: Differential expression and significance of endoplasmic
reticulum golgi intermediate compartment 1 in precancerous gastric
lesions and gastric cancer. Am J Med Sci. 355:228–234. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li A, Xiong J and Chen Z: IL-6, TNF-α, and
iNOS is associated with decreased colonic contraction in rats with
multiple organ dysfunction syndrome. J Surg Res. 178:e51–e57. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee JH, Kim HY, Bae EH, Kim SW and Ma SK:
Biomarkers predicting survival of sepsis patients treated with
continuous renal replacement therapy. Chonnam Med J. 53:64–68.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shimazui T, Matsumura Y, Nakada TA and Oda
S: Serum levels of interleukin-6 may predict organ dysfunction
earlier than SOFA score. Acute Med Surg. 4:255–261. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Seymour CW, Liu VX, Iwashyna TJ,
Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM,
Shankar-Hari M, Singer M, et al: Assessment of clinical criteria
for sepsis: For the third international consensus definitions for
sepsis and septic shock (Sepsis-3). JAMA. 315:762–774. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lee YJ, Park CH, Yun JW and Lee YS:
Predictive comparisons of procalcitonin (PCT) level, arterial
ketone body ratio (AKBR), APACHE III score and multiple organ
dysfunction score (MODS) in systemic inflammatory response syndrome
(SIRS). Yonsei Med J. 45:29–37. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ávalos-López M, Pérez-López MJ,
Aguilar-Martínez C, Díaz-Franco AMC, Esquivel-Chávez A and
Baltazar-Torres JA: Prediction of acute kidney injury in critically
ill patients treated with intermittent hemodialysis versus CRRT.
Rev Med Inst Mex Seguro Soc. 55:696–703. 2017.(In Spanish).
PubMed/NCBI
|
|
28
|
Yoon J, Kim Y, Kym D, Hur J, Yim H, Cho YS
and Chun W: Subgroup analysis of continuous renal replacement
therapy in severely burned patients. PLoS One. 12:e01890572017.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li YN, Zhou LX, Qiang XH, Yu TO, Mao KJ,
Feng B, Wen WB, Zou YC, Li WY and Li C: Effect of continuous blood
purification and thymosin alpha1 on the cellular immunity in
patients with severe sepsis: A prospective, randomized, controlled
clinical trial. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 21:139–142.
2009.PubMed/NCBI
|
|
30
|
Zhou R, Weng F, Dai W and Yan J: The organ
protective effects and timing of continuous blood purification in
the treatment of severe sepsis: A double-blind randomized
controlled trial. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue.
28:241–245. 2006.(In Chinese).
|
|
31
|
Sabatino A, Theilla M, Hellerman M, Singer
P, Maggiore U, Barbagallo M, Regolisti G and Fiaccadori E: Energy
and protein in critically ill patients with AKI: A prospective,
multicenter observational study using indirect calorimetry and
protein catabolic rate. Nutrients. 9(pii): E8022017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Allegretti AS, Steele DJ, David-Kasdan JA,
Bajwa E, Niles JL and Bhan I: Continuous renal replacement therapy
outcomes in acute kidney injury and end-stage renal disease: A
cohort study. Crit Care. 17:R1092013. View
Article : Google Scholar : PubMed/NCBI
|
|
33
|
Quinto BM, Iizuka IJ, Monte JC, Santos BF,
Pereira V, Durão MS, Dalboni MA, Cendoroglo M, Santos OF and
Batista MC: TNF-α depuration is a predictor of mortality in
critically ill patients under continuous veno-venous
hemodiafiltration treatment. Cytokine. 71:255–260. 2015. View Article : Google Scholar : PubMed/NCBI
|