Introduction
Echinococcosis caused by Echinococcus
granulosus is a common type of zoonosis in farming and grazing
areas and is distributed worldwide (1). The major organ affected is the liver,
but extrahepatic disease is also possible. Only few cases of
thyroid cystic hydatid disease have been reported worldwide.
However, the possibility of cystic hydatid disease cannot be
ignored in those areas with a high incidence of hydatid
disease.
Echinococcosis in rare sites, including the thyroid,
is mostly misdiagnosed, predominantly due to its rarity. It is at
times diagnosed as cystic echinococcosis during surgery and even
treated on the basis of the incorrect diagnosis. For echinococcosis
in rare locations, including thyroid cystic echinococcosis, various
countries and regions have implemented different treatment
modalities, such as total thyroidectomy, partial thyroidectomy and
fine needle aspiration cytology (FNAC) (2,3).
The present study presents a case of hydatid
cyst-tracheal fistula in the thyroid. Furthermore, the literature
on cystic echinococcosis of the thyroid gland was reviewed to
summarize the characteristics of thyroid cystic echinococcosis, and
compare its diagnosis and treatment among studies.
Case report
A 54-year-old male patient without any history of
exposure to farm animals presenting with a gradual swelling on the
left side of the lower part of the neck over a period of two years
was admitted to the First Affiliated Hospital of Xinjiang Medical
University in November 2013. The swelling was first noticed ~20
years previously. Furthermore, the patient presented with fever and
productive cough with occasional hydatid daughter cyst for 2
months. Difficulty in breathing appeared twice and the symptoms
were alleviated after oxygen therapy and intramuscular injection of
dexamethasone. During physical examination, a non-tender, soft and
fluctuant mass was palpable on the left lateral side of the neck.
The size of the mass was measured as 7×4 cm. The computed
tomography (CT) scan of the abdomen and pelvis indicated no
evidence of hydatid cyst. Bronchoscopy examination revealed an
ulcer just 2 cm below the glottis and this ulcer was 8 mm in
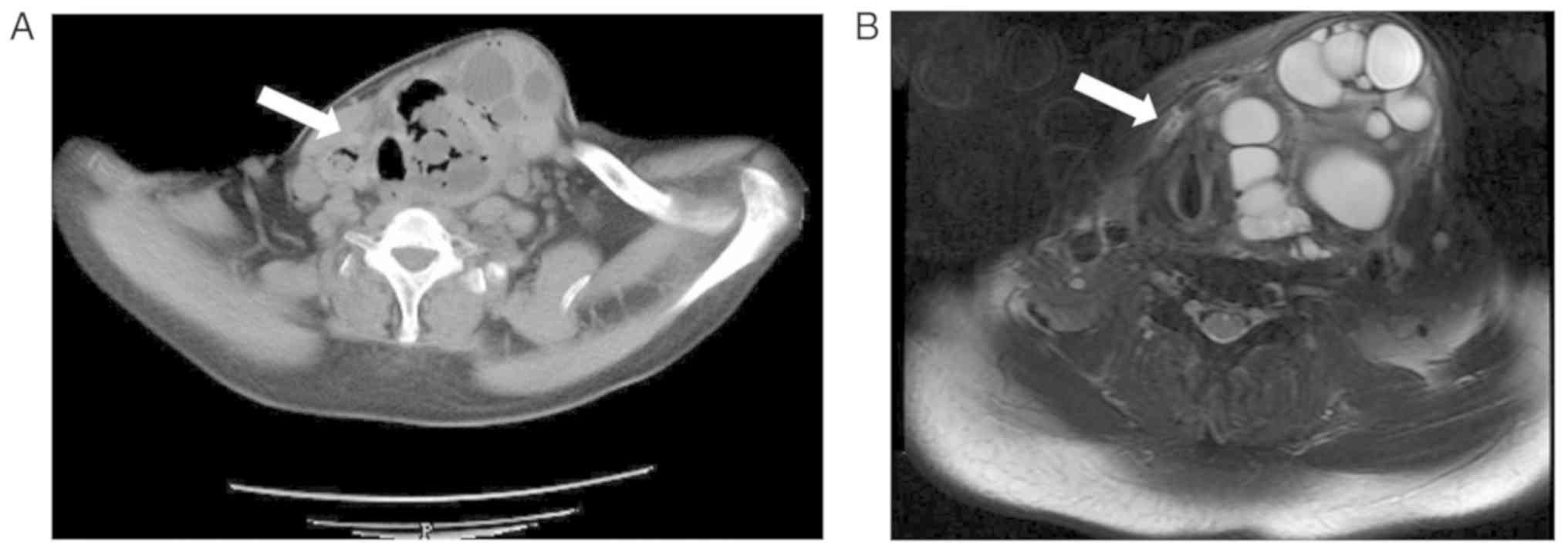
diameter. The hydatid immunology test was positive. CT (Fig. 1A) and magnetic resonance imaging
(MRI; Fig. 1B) revealed hydatid on
the two sides of the thyroid.
The patient received surgery for excision of the
internal capsule. During surgery, the hydatid cyst was removed,
while the surrounding area was protected. A fistula of 1 cm in
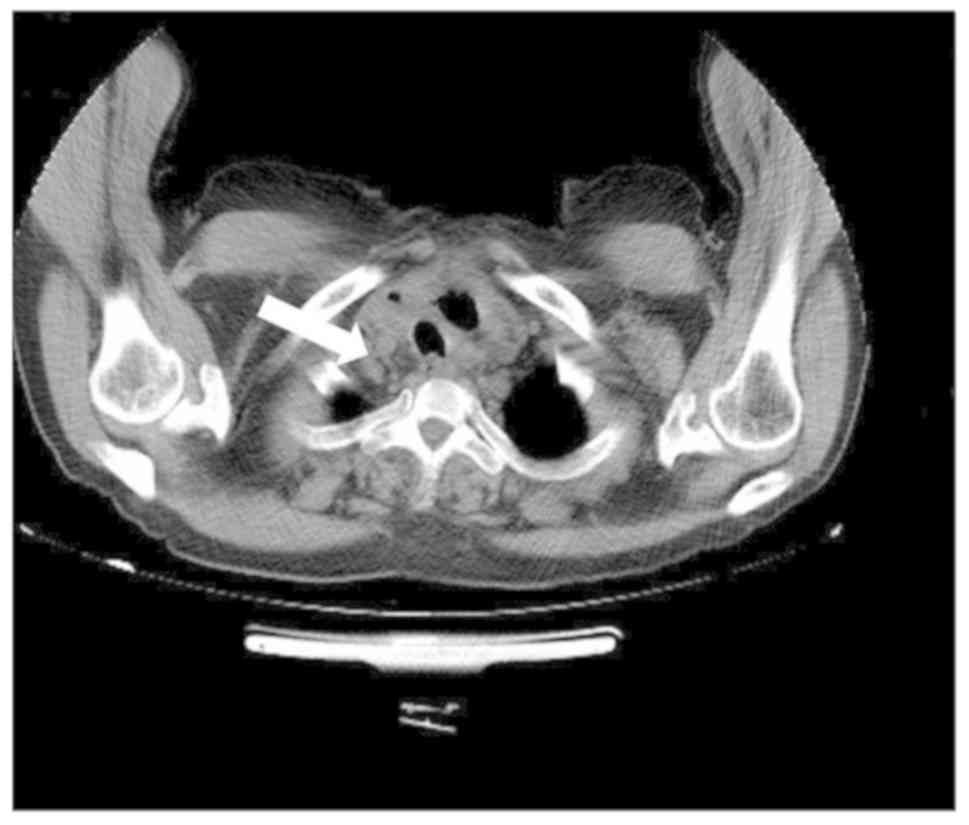
diameter was identified between the trachea and cyst (Fig. 2), and the fistula was repaired. Two
drainage tubes were placed in the operation area. The
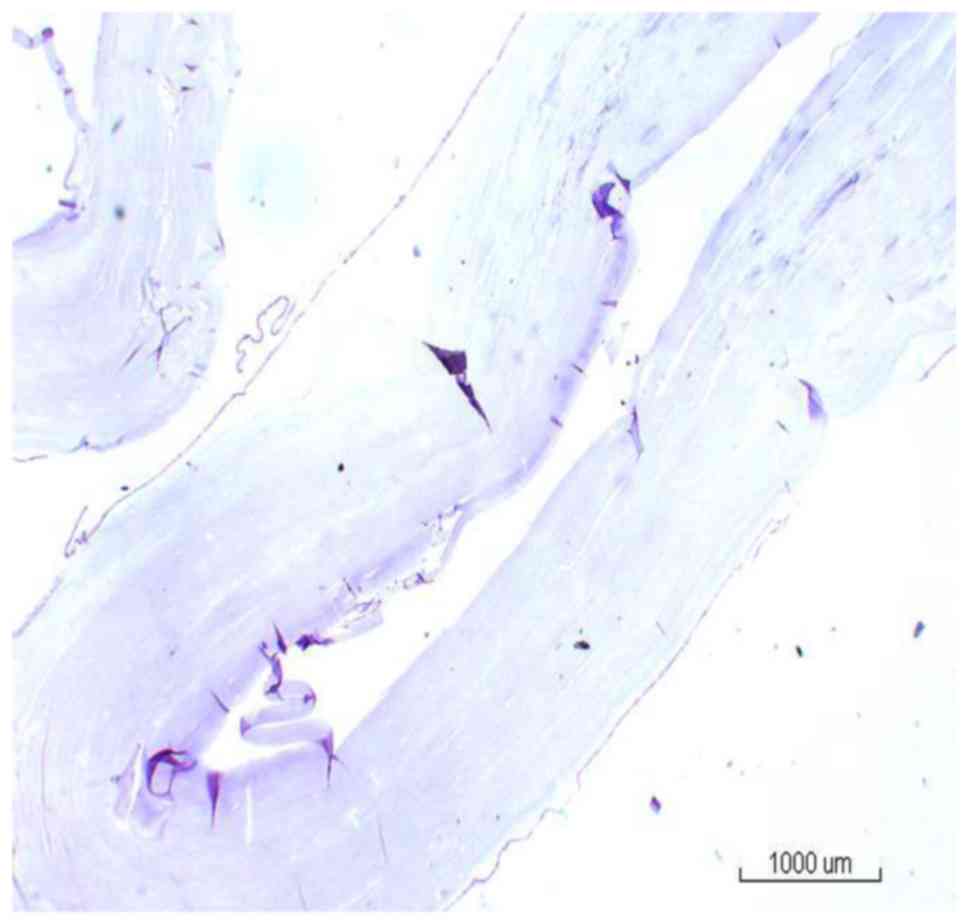
post-operative pathological diagnosis was echinococcosis granulosa
of the thyroid (Fig. 3). The fistula
orifice between the hydatid residual cavity and the trachea was
still visible on CT at 5 days after the surgery (Fig. 4). Inflammation in the lung was also
still visible. A small amount of gas (~50 cm3) appeared
in the drainage bag of the operated area when the patient coughed.
The gas volume was generally low. Due to the low quantity of the
gas, the tube was pulled out on the fifth day after the operation.
The fistula had disappeared in the review CT scan at 5 days after
the surgery. The patient continued to receive albendazole therapy
(15 mg/kg/day) for 1 year post-operatively. No recurrence was
observed in the thyroid during the 54-month post-operative
follow-up period.
Discussion
Hydatid disease is a parasitic infection with
worldwide prevalence (4). A hydatid
cyst of Echinococcus granulosus may develop in any part of
the body (5–8). Although it mostly tends to form cysts
in the liver (75%) or lung (15%), other organs of the body,
including the brain, heart, bones, muscle, kidney and pancreas, may
also be affected (8–11). While thyroid involvement of
echinococcosis is rare, thyroid hydatid with tracheal fistula is
even rarer.
A high circulatory flow rate in the thyroid gland
may have an important role in the development of the thyroid
hydatid cyst (6,8,9). It
remains elusive how the relatively high thyroid blood flow is
paralleled with a disproportionately low incidence of thyroid cyst
disease, but one theory indicates that the relatively small caliber
of the thyroid arteries together with their position at a right
angle to the carotids is an anatomical arrangement that is thought
to offer the thyroid gland a certain measure of protection against
the invading parasite (4).
Patients with thyroid hydatid cyst are at times
asymptomatic. A few hydatid patients present with symptoms
including hoarseness and dyspnea, which are caused by the
compression of surrounding tissues during the growth of the
hydatid. When the patients present with symptoms of cough and
expectoration, hydatid-bronchial fistula should be considered. If
the patient has coughed-up discharge of cystic fluid and even
daughter cyst of hydatid, hydatid-tracheal fistula may be
diagnosed.
Ultrasound, CT and MRI are of great value in the
diagnosis of thyroid primary disease. Thyroid hydatid should be
distinguished from thyroid cyst. The imaging findings of thyroid
hydatid and thyroid cyst are similar. Through analyzing the
patient's epidemiological history (such as history of exposure to
farm animals or history of living in an area with high prevalence)
and history of hepatic hydatid disease, and considering the
immunological results, thyroid hydatid may be diagnosed.
At present, the management of choice for hydatid
disease is early detection. Surgical intervention includes the
excision of the cyst and a part of the involved adjacent thyroid
gland (4). It is preferred to not
excise the thyroid or excise the thyroid as little as possible, as
this avoids post-operative hypothyroidism. Surgery should be
performed carefully to prevent extrusion of the hydatid fluid or
sac into the trachea. At present, surgical treatment is the first
choice for treating hydatid disease. However, drug treatment prior
to and after surgery may improve the cure rate and reduce the
recurrence rate of the disease (12).
A literature search was performed in the PubMed,
Medline and Google Scholar databases by using key words, including
‘Thyroid’, ‘Echinococcosis’, ‘Hydatid cyst’ and ‘Hydatid disease’,
in different combinations. Studies were limited to those in English
and Chinese language. The abstracts were retrieved and reviewed for
pre-selection, followed by retrieval of the full articles. A total
of 18 articles (4,7,13–28) with
detailed descriptions were identified, and 21 cases were reported
in them. Table I presents the
detailed data of these studies. Based on the specific data in these
studies, the diagnosis and treatment thyroid cystic echinococcosis
was summarized and analyzed.
 | Table I.Detailed characteristics of all
published cases of hydatid cyst of thyroid gland from 2010. |
Table I.
Detailed characteristics of all
published cases of hydatid cyst of thyroid gland from 2010.
| Authors (year) | Country | Age (years) | Sex | Signs | Cyst in other
organs | Treatment method | Puncture | Operation | Drug treatment | Recurrence | Post-operative
complications | (Refs.) |
|---|
| Xiong and Li
(2017) | China | 27 | F | Physical findings
(such as a mass) | No | Surgery | No | Partial
thyroidectomy | No | Not mentioned | Not mentioned | (13) |
| Rauhofer et
al, (2003) | Australian | 14 | F | Physical findings
(such as a mass) | No | Surgery+medical
therapy | No | Enucleation of
cyst | Postoperative
albendazole for 3 months | No | No | (14) |
| Akbulut et
al, (2015) | Turkey | 26 | F | Pain | Yes | Surgery | No | Total
thyroidectomy | No | No | Not mentioned |
|
|
|
| 57 | F | Hoarseness | Yes | Medical
therapy+surgery | No | Total
thyroidectomy | Preoperative
albendazole for 2 weeks | No | Hypocalcemia | (15) |
| Eken et al,
(2016) | Turkey | 65 | F | Dyspnea | Yes | Surgery+medical
therapy | No | Total
thyroidectomy | Postoperative
albendazole for 3 weeks | No | No | (16) |
| Moghimi et
al, (2009) | Iran | 35 | F | Enlarged
masses | No | Surgery | No | Total
thyroidectomy | No | No | No | (17) |
| Oksuz et al,
(2013) | Turkey | 23 | M | Hoarseness | No | Surgery+medical
therapy | No | Partial
thyroidectomy | Postoperative
albendazole for 2 months | No | No | (18) |
| Ozaydin et
al, (2009) | Turkey | 25 | M | Enlarged
masses | No | Surgery+medical
therapy | Yes | Partial
thyroidectomy | Postoperative
albendazole for 6 months | No | No | (7) |
| Yilmaz et
al, (2013) | Turkey | 18 | M | Enlarged
masses | Yes | Surgery+medical
therapy | No | Partial
thyroidectomy | Preoperative
albendazole 400 mg/day, postoperative albendazole for 2 months | No | No | (4) |
|
|
| 21 | M | Enlarged
masses | No | Surgery+medical
therapy | No | Total
thyroidectomy | Postoperative
albendazole for 6 weeks | No | No |
|
|
|
| 25 | F | Pain | No | Surgery+medical
therapy | No | Total
thyroidectomy | Postoperative
albendazole for 6 weeks | No | No |
|
| Capoglu et
al, (2002) | Turkey | 40 | F | Enlarged
masses | No | Surgery | No | Total
thyroidectomy | No | Not mentioned | No | (19) |
| Jain et al,
(2005) | India | 55 | F | Hoarseness and
dyspnea | No | Surgery+medical
therapy | No | Enucleation of
cyst | Mebendazole (no
mention of dosage and course of treatment) | No | No | (20) |
| Zulfikaroglu et
al, (2008) | Turkey | 50 | F | Enlarged
masses | No | Surgery | No | Partial
thyroidectomy | No | No | No | (21) |
| Dey et al,
(2014) | India | 30 | F | Enlarged
masses | Not mentioned | Surgery+medical
therapy | Not mentioned | FNAC | Postoperative
albendazole 400 mg/day for 28 days | No | No | (22) |
| Bartin et
al, (2014) | Turkey | 32 | F | Hoarseness | No | Surgery+medical
therapy | No | Total
thyroidectomy | Albendazole for 2
months (400 mg/day) | No | No | (23) |
| Avcut et al,
(2010) | Turkey | 48 | M | Enlarged
masses | No | Medical
therapy+Surgery | Not mentioned | PAIR | Preoperative
albendazole (10 mg/kg) for 1 week+ anti-allergy treatment for 15
minutes before surgery+postoperative albendazole (10 mg/kg) for 2
weeks | No | No | (24) |
| Azendour et
al, (2011) | Morocco | 23 | F | Enlarged
masses | No | Surgery+medical
therapy | No | Total
thyroidectomy | Postoperative
albendazole for 2 months (400 mg/day) | No | No | (25) |
| Erkilic et
al, (2004) | Turkey | 9 | M | Enlarged
masses | No | Surgery | No | Partial
thyroidectomy | Not mentioned | No | Not mentioned | (26) |
| Gokce et al,
(2003) | Turkey | 33 | M | Enlarged
masses | No | Surgery+medical
therapy | Pre-operative fine
needle aspiration | Total
thyroidectomy | Postoperative
albendazole for 6 months (400 mg/day) | No | No | (27) |
| Dissanayake et
al, (2016) | USA | 44 | F | Enlarged
masses | No | Surgery+medical
therapy | Yes | Not mentioned | Albendazole (no
mention of mentioned dosage and course of treatment) | Not mentioned | No | (28) |
Of the 18 studies from 7 countries, 11 studies from
Turkey reported on 14 patients, 2 studies from India reported on 2
cases and the remaining articles were from the USA, Morocco, Iran,
Australia and China, with each study reporting on one case. The
studies comprised a total of 21 patients (14 women and 7 men). The
age at onset was 9–65 years with the median age of 30 years.
The major complaints of the patients with thyroid
cystic echinococcosis were progressive enlarged neck mass, neck
pain, hoarseness and difficulty in breathing. Most of the patients
(14/21) presented with enlarged masses on the neck and had no
specific symptoms. A total of 4 patients complained of hoarseness
and 2 of neck pain, and 2 patients had dyspnea. Two patients
presented with thyroid cystic lesions revealed through physical
examination. The hydatid lesion itself appeared to cause no
specific symptoms and the abovementioned complaints were mainly
caused by compression of the increased hydatid lesions.
Pre-operative diagnosis is important for thyroid
hydatid disease. The diagnostic methods include review of the
patient history, physical examination, imaging examination,
serological examination and FNAC diagnosis (29). The imaging diagnosis is considered to
be the most important one (24,30,31). The
imaging diagnosis usually includes ultrasound, CT and MRI.
Ultrasonography is effective in detecting the cystic lesions and is
important for the pre-operative diagnosis (32). CT scan and MRI are usually
complementary diagnostic tools. For multiple hydatid cysts,
particularly in patients with a history of hydatid disease, the
diagnosis is straightforward; however, for a less experienced
clinician, it is difficult to identify a primary thyroid monocystic
echinococcosis from a single cyst. The most common misdiagnoses are
simple thyroid cysts. By ultrasound, the round and non-echo
lesions, visible floating small light spots in the dark area and
the ‘sand bag syndrome’ may be observed (33). The cystic wall is smooth and complete
and exhibits a double-layer sign (34). Regarding the differential diagnosis,
ultrasound is superior to CT and MRI (35). In addition, the patient's
epidemiological history and information on whether hydatid disease
is present in the liver are helpful for making a definite
diagnosis. CT examination is able to accurately display the
narrowing and displacement when the hydatid lesions involve the
blood vessels and trachea (36), and
may clearly display the association of the hydatid lesions with
surrounding tissues (37), which is
of significance in guiding pre-operative preparation and surgical
planning. However, bronchial fistula is characterized by the
presence of a shadow of gas density in the hydatid cavity. For
larger fistula, CT and MRI may indicate the size and location of
the fistula. Bronchoscopy may directly display the fistula and the
location of the fistula in lesions generally presents as the most
prominent site of the trachea.
FNAC is generally accepted in the clinical treatment
of the single thyroid nodules (38).
Although no study has reported any allergic reactions after FNAC,
this technique is not recommended, as it may cause the diffusion of
the cystic fluids or allergic reactions. Therefore, FNAC should be
avoided when differential diagnosis of thyroid hydatid cysts is
needed.
The immunological method is also an important
modality for the diagnosis of echinococcosis, particularly as a
differential diagnosis (39). The
traditional Casoni intradermal test has a high false-positive rate
and is overly sensitive. Immune disturbances seriously affect the
follow-up after treatment and have been removed from the World
Health Organization (WHO)'s Hydatid Disease Diagnosis and Treatment
Guidelines (2001 edition) (3). In
addition, the test strip and ELISA methods also have important
roles in the screening for echinococcosis.
Among all cases analyzed, thyroid hydatid was a
condition primary to the thyroid. Examination of patients (15/21)
revealed that only the thyroid gland contained cystic hydatid and
that no organs had any hydatid lesions. In general, the liver is
the most susceptible and the first site of infection for
echinococcosis (40). Among the 21
cases, only two were combined with hepatic cystic echinococcosis.
One case was combined with hydatid in multiple sites, including the
liver, lung and abdomen. One patient had lung hydatid 10 years
previously, which was removed by surgery. One patient had hepatic
hydatid 2 years previously, which was treated by surgery. In
another case, there was no mention of whether any other organs
exhibited any hydatid cysts.
Of the 21 cases, one patient received puncture
treatment twice prior to surgery. Three patients underwent FNAC
pathological examination in order to clarify the pre-operative
diagnosis. One case from Turkey reported in 2010 (24) received puncture-aspiration of cyst
contents-injection of hypertonic saline solution-reaspiration
(PAIR) treatment. In this case, two daughter cysts of the hydatid
lesions were punctured, 35% of cyst fluid was aspirated and 20%
hypertonic saline was injected into the cavity for 10 min. The
patient was subjected to post-operative albendazole treatment for 2
weeks and reported no complications during the treatment. During
the 4-month follow-up, a ‘pseudotumor appearance’ without any fluid
component or daughter vesicles was noted. In the case of the
present study, surgical treatment was preferred, as PAIR technology
may rather be suitable for monocystic hydatid cyst. For multiple
hydatid cysts, hypertonic saline cannot completely destroy the
capsule wall of the daughter cyst as well as inactivate the hydatid
sac. However, spillage of the cyst fluids may also occur, which may
even increase the risk of allergic reactions. Therefore, puncture
treatment of the hydatid cysts is not recommended at our medical
center. Among the reviewed literature, three studies (19,20,22) also
indicated that the hydatid puncture is considered to be associated
with a high risk and is not recommended. Therefore, the safety and
efficacy of PAIR remains controversial and requires further
investigation.
Surgical treatment remains the preferred method for
the treatment of thyroid hydatid cysts (41). Most of the patients underwent partial
or complete thyroidectomy. The cases reviewed comprised 17 cases of
thyroidectomy, including 9 cases of total thyroidectomy, 6 cases of
ipsilateral partial thyroidectomy and 2 cases of hydatid cyst
removal. One of the patients presented with hypocalcemia directly
after total thyroidectomy and during the post-operative 4-year
follow-up (42). The case reported
in the present study only received excision of the hydatid and
repair of the fistula orifice connected with the bronchus. Based on
previous experience, for the excision of the thyroid gland,
regardless of whether it is a total or an ipsilateral excision, the
removal of the normal thyroid tissue may be unnecessary and easily
causes other associated complications, including peripheral nerve
or parathyroid damage. Even if no other complications occur, total
resection of the thyroid may require lifelong treatment with
thyroid hormones. In summary, the surgical removal of hydatid cysts
followed by post-operative albendazole treatment is a safe and
effective method.
A total of 5 patients with total thyroidectomy and 2
with ipsilateral thyroidectomy did not take any anti-hydatid drugs
after the surgery, whereas the remaining 13 patients took
anti-hydatid drugs after the surgery. In the reviewed studies, most
patients were advised to take oral albendazole. Only one case from
India reported in 2005 (20) was
treated with oral mebendazole. Among the studies, a large
difference in the duration of drug intake was noted; for instance,
the duration of albendazole treatment was as short as 2 weeks in
one case (15) and the maximum time
was 6 months (27). The specific
duration of taking the drug was not specified in two of the
studies. The dose of albendazole was 400 mg/day in 4 of the studies
(22,23,25,27) and
10 mg/kg/day based on the weight of the patient in one study
(24).
At present, the preferred drugs for the treatment of
echinococcosis are benzimidazole drugs, of which the representative
drugs are mebendazole and albendazole (43,44). The
treatment effect of albendazole has been demonstrated to be
significantly better than that of mebendazole (3,12), and
it has now replaced mebendazole and become one of the drugs of
choice recommended by the WHO (2,3).
Albendazole is metabolized into albendazole and sulfoxide in the
liver and exerts an anti-helminthic effect; it significantly
inhibits the parasite's absorption of glucose, resulting in the
exhaustion of glucose or inhibition of the fumarate reductase
system. This mechanism impedes the formation of ATP, making
parasites unable to survive and reproduce. As echinococcosis has a
high recurrence rate (45) and each
patient has a different extent of disease, the post-operative drug
therapy for hydatidosis patients should be individualized based on
the activity of the hydatid lesions and the specific circumstances
of the patients. Even if a non-curative surgery is performed and
the activity of the hydatid lesions is not high or even in a state
of solid necrosis, the time for taking the drug may be reduced. For
single-capsule, multi-ascendant and internal capsule collapse
types, 3–12 months of post-operative drug therapy is recommended
(45). It is more clinically
significant to determine the dose according to the weight of the
patient. Based on our experience, the total daily dose is 10–15
mg/kg, half of which should be administered each morning and
evening. An individual study also reported the administration of
pre-operative prophylactic oral albendazole (24), and according to expert consensus,
pre-operative treatment for 3–7 days is also recommended.
Despite significant advances in diagnostic research,
as well as medical and surgical treatment, echinococcosis remains a
challenging disease with high morbidity. Hydatid cyst in the
thyroid is rare. The diagnosis of hydatid cyst in the thyroid
should be considered in epidemic regions of hydatid disease. The
diagnosis and treatment of thyroid cystic hydatid vary considerably
among different regions, particularly the choice of surgical
procedure and the duration and dosage of therapeutic drugs. At
present, there is no uniform standard of treatment. In conclusion,
the diagnosis and treatment of hydatid cyst in the thyroid reported
in recent years were reviewed. The present study may enhance the
understanding and awareness of hydatid cyst in the thyroid and
provide a reference for clinicians.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Science Foundation of China (grant nos. 81560098 and 81660108) and
Natural Science Foundation of Xinjiang Province (grant no.
2016D01C274).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TJ, BR, RZ and QG collected the data. TJ wrote the
manuscript. YS and TA conceived and designed the present study, and
revised the manuscript. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethics review
board of the First Affiliated Hospital of Xinjiang Medical
University (Xinjiang, China).
Patient consent for publication
Informed consent was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McManus DP, Zhang W, Li J and Bartley PB:
Echinococcosis. Lancet. 362:1295–1304. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Brunetti E, Kern P and Vuitton DA; Writing
Panel for the WHO-IWGE, : Expert consensus for the diagnosis and
treatment of cystic and alveolar echinococcosis in humans. Acta
Trop. 114:1–16. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Guidelines for treatment of cystic and
alveolar echinococcosis in humans, . WHO Informal Working Group on
Echinococcosis. Bull World Health Organ. 74:231–242. 1996.(In
English, French). PubMed/NCBI
|
|
4
|
Yilmaz M, Akbulut S, Sogutlu G, Arabaci E
and Kayaalp C: Hydatid cyst of the thyroid gland: Report of three
cases. Surg Today. 43:937–941. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Akbulut S, Senol A, Ekin A, Bakir S, Bayan
K and Dursun M: Primary retroperitoneal hydatid cyst: Report of 2
cases and review of 41 published cases. Int Surg. 95:189–196.
2010.PubMed/NCBI
|
|
6
|
Erbil Y, Barbaros U, Baspinar I, Deveci U,
Deveci U, Kapran Y, Bozbora A, Aral F and Özarmağan S: Hydatid cyst
of the thyroid gland: Two case reports. Infect Dis Clin Pract.
13:318–320. 2005. View Article : Google Scholar
|
|
7
|
Ozaydin I, Ozaydin C, Oksuz S and Yildirim
M: Primary Echinococcus cyst of the thyroid: A case report.
Acta Med Iran. 49:262–264. 2011.PubMed/NCBI
|
|
8
|
Azendour I, Boulaich M, Ayoubi A, Oujilal
A, Essakalli L and Kzadri M: Primary hydatid cyst of the thyroid
gland. Int J Otolaryngol. 2011:7130892011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gökçe C, Patiroğlu T, Akşehirli S, Durak
AC and Keleştimur F: Hydatic cyst in the thyroid gland diagnosed by
fine-needle aspiration biopsy. Thyroid. 13:987–989. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Özerkan E, Gürçınar M, Sarıoğlu B and
Aydınlıoğlu H: A case of cystic echinoccosis in thyroid gland: A
very rare localisation of echinoccosis infection. Turk J Endocrinol
Metabol. 4:181–183. 1999.
|
|
11
|
Pérez PJA, Felmer EO, Carrasco EC,
Gabrielli NM, Torrijos CC and Bastías NJA: Thyroid hydatid cyst:
Report of one case. Rev Med Chil. 136:896–899. 2008.(In Spanish).
PubMed/NCBI
|
|
12
|
Senyüz OF, Yeşildag E and Celayir S:
Albendazole therapy in the treatment of hydatid liver disease. Surg
Today. 31:487–491. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xiong W and Li L: A case of thyroid
hydatid in Tibet, China. Contemp Med. 28:1262017.(In Chinese).
|
|
14
|
Rauhofer U, Prager G, Hörmann M, Auer H,
Kaserer K and Niederle B: Cystic echinococcosis of the thyroid
gland in children and adults. Thyroid. 13:497–502. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Akbulut S, Demircan F and Sogutcu N:
Hydatid cyst disease of the thyroid gland: Report of two cases. Int
Surg. 100:643–647. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Eken H, Isik A, Balci G, Firat D, Cimen O
and Soyturk M: A rare case of isolated cystic hydatid of thyroid
gland. Medicine (Baltimore). 95:e29292016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moghimi M, Kamrava SK, Asghari AM,
Heshmatzade Behzadi A, Jalessi M, Naraghi MM and Ehteshamia Afshar
E: Primary echisnococcal cyst in the thyroid gland: A case report
from Iran. J Infect Dev Ctries. 3:732–734. 2009.PubMed/NCBI
|
|
18
|
Oksuz S, Pektas E, Yavuz M, Aksungur N,
Cayir Y and Akcay MN: An unusual cause of hoarseness: Hydatid cyst
of the thyroid. Trop Biomed. 30:642–644. 2013.PubMed/NCBI
|
|
19
|
Capoğlu I, Unüvar N, Erdogan F, Yilmaz O
and Caydere M: A hydatid cyst of the thyroid gland. J Int Med Res.
30:206–209. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jain SK, Jamdade PT, Muneshwar SS,
Ambulgekar VK and Panzade SM: Hydatid cyst of thyroid: An unusual
cause of stridor. Indian J Otolaryngol Head Neck Surg. 57:80–81.
2005.PubMed/NCBI
|
|
21
|
Zulfikaroglu B, Ozalp N, Keskek M and Koc
M: Primary echinococcal cyst of the thyroid: Report of a case. Surg
Today. 38:833–835. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dey AK, Mandal PK, Dutta A, Pramanik S,
Maji S, Chakraborti and Dasgupta S: A case of hydatid cyst of
thyroid gland. Asian J Med Sci. 5:143–145. 2014. View Article : Google Scholar
|
|
23
|
Bartın MK, Yılmaz EM, Arslan H, Tekeli AE
and Karataş S: A case of primary hydatid cyst in the thyroid gland.
Ulus Cerrahi Derg. 31:94–95. 2014.PubMed/NCBI
|
|
24
|
Avcu S, Unal O, Kotan C, Oztürk M and Ozen
O: Submandibular and thyroid gland involvement of hydatid cysts: A
very rare association with percutaneous treatment. Diagn Interv
Radiol. 16:251–254. 2010.PubMed/NCBI
|
|
25
|
Azendour I, Boulaich M, Ayoubi A, Oujilal
A, Essakalli L and Kzadri M: Primary hydatid cyst of the thyroid
gland. Int J Otolaryngol. 2011:7130892011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Erkiliç S, Ozsaraç C, Koçer NE and Bayazit
YA: Hydaitd cyst of the thyroid gland in a child. Int J Pediatr
Otorhinolaryngol. 68:369–371. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gökçe C, Patiroğlu T, Akşehirli S, Durak
AC and Keleştimur F: Hydatic cyst in the thyroid gland diagnosed by
fine-needle aspiration biopsy. Thyroid. 13:987–989. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dissanayake PI, Chennuri R and Tarjan G:
Fine-needle aspiration diagnosis of primary hydatid disease of the
thyroid; first reported case in the USA. Diagn Cytopathol.
4:334–337. 2016. View
Article : Google Scholar
|
|
29
|
Kammerer WS and Schantz PM: Echinococcal
disease. Infect Dis Clin North Am. 7:605–618. 1993.PubMed/NCBI
|
|
30
|
Gharbi HA, Hassine W, Brauner MW and
Dupuch K: Ultrasound examination of the hydatic liver. Radiology.
139:459–463. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yaliniz H, Tokcan A, Salih OK and Ulus T:
Surgical treatment of cardiac hydatid disease: A report of 7 cases.
Tex Heart Inst J. 33:333–339. 2006.PubMed/NCBI
|
|
32
|
Versaci A, Macri A, Terranova M, Galipò S,
Barbera A, Speciale G and Famulari C: Primary echinococcosis of the
thyroid gland: Apropos of a case. G Chir. 18:427–431. 1997.(In
Italian). PubMed/NCBI
|
|
33
|
Song FL, Han SH, Fang J and Zhang L:
Diagnostic value of hepatic hydatid cyst with CT and MRI. J Pract
Radiol. 2006.
|
|
34
|
Zhang HX and H.N. F: Clinical diagnosis
and treatment of liver cystic echinococcosis. Chin J Endemiol.
34:309–312. 2015.
|
|
35
|
WHO Informal Working Group, :
International classification of ultrasound images in cystic
echinococcosis for application in clinical and field
epidemiological settings. Acta Trop. 85:253–261. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Engin G, Acunas B, Rozanes I and Acunas G:
Hydatid disease with unusual localization. Eur Radiol.
10:1904–1912. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhao YP, Liu WY, Wang J, Liu XL and Dang
J: The value of CT score in predicting surgical methods and
difficulty of hepatic cystic echinococcosis. Chin J Radiol.
45:55–59. 2011.(In Chinese).
|
|
38
|
Yoo WS and Chung HK: Recent advances in
autoimmune thyroid diseases. Endocrinol Metab (Seoul). 31:379–385.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kern P, Menezes da Silva A, Akhan O,
Mullhaupt B, Vizcaychipi KA, Budke C and Vuitton DA: The
echinococcoses: Diagnosis, clinical management and burden of
disease. Adv Parasitol. 96:259–369. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Grozavu C, Ilias M and Pantile D:
Multivisceral echinococcosis: Concept, diagnosis, management.
Chirurgia (Bucur). 109:758–768. 2014.PubMed/NCBI
|
|
41
|
Menezes da Silva A: Hydatid cyst of the
liver-criteria for the selection of appropriate treatment. Acta
Trop. 85:237–242. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Moghimi M, Kamrava SK, Asghari AM,
Heshmatzade Behzadi A, Jalessi M, Naraghi MM and Ehteshamia Afshar
E: Primary echinococcal cyst in the thyroid gland: A case report
from Iran. J Infect Dev Ctries. 3:732–734. 2009.PubMed/NCBI
|
|
43
|
Davis A, Dixon H and Pawlowski ZS:
Multicentre clinical trials of benzimidazole-carbamates in human
cystic echinococcosis (phase 2). Bull World Health Organ.
67:503–508. 1989.PubMed/NCBI
|
|
44
|
Vutova K, Mechkov G, Vachkov P, Petkov R,
Georgiev P, Handjiev S, Ivanov A and Todorov T: Effect of
mebendazole on human cystic echinococcosis: The role of dosage and
treatment duration. Ann Trop Med Parasitol. 93:357–365. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wen H: Advancement of diagnosis and
surgical treatment for hepatic echinococcosis. Zhong Hua Xiao Hua
Wai Ke Za Zhi. 10:290–292. 2011.(In chinese).
|