Introduction
Diabetes mellitus is a group of common metabolic
disorders that has become a major public health worldwide (1). Diabetes currently affects 6.4% of
adults (285 million) globally and its incidence is expected to
increase to 7.7% by 2030, affecting 439 million adults (2). In developing countries, the incidence
of diabetes is predicted to increase by 60% in the next 20 years
(2). Although the incidence of
diabetes in China is relatively low, this may change in the future
due to changes in lifestyle and increased psychological and
physiological stress (3). In 2016,
the World Health Organization revealed that diabetes causes ~1.5
million (2.7%) deaths every year, while the major cause of death in
diabetic patients is glucotoxicity-induced complications in major
organs (4). Although the lung is one
of the least studied organs in diabetes, a number of studies have
revealed that the lung is a common target of glucotoxicity-induced
diabetic injury (5).
The pathogenesis of diabetic lung disease is complex
and remains largely unknown (6).
Excessive nitric oxide (NO) in lung tissue can cause platelet
activation and induce chronic inflammation, which in turn leads to
damaged lung capillary endothelium and microangiopathy (7). Nitric oxide synthases (NOSs) are a
family of enzymes, which catalyze the production of NO from
L-arginine (8). The inhibition of
NOSs production under high-glucose conditions may prevent the
occurrence of diabetic lung disease by protecting lung cells via
reducing the inflammatory response.
Smoke and cancer-associated lncRNA 1 (SCAL1), also
known as lung cancer associated transcript 1 (LUCAT1), is a long
non-coding RNA (lncRNA) that was initially identified to play a
role in lung cancer (9). In lung
cancer, SCAL1 interact with downstream NRF2 in airway epithelial
cells to mediate oxidative stress protection and regulate gene
expression. In view of the roles of NOSs in the oxidative
metabolism (8), the present study
hypothesized that SCAL1 may also interact with NOSs. The current
study aimed to investigate the role of SCAL1 in diabetic lung
disease and its possible interactions with nitric oxide synthase
(iNOS) to provide potential novel treatment targets.
Materials and methods
Patients and specimens
A total of 56 patients with type 2 diabetes without
lung disease (diabetic group) and 44 patients with type 2 diabetes
with pneumonia (diabetic lung group) were included in the current
study. All patients with type 2 diabetes were diagnosed according
to the criteria established by Chinese Medical Association (2014)
and enrolled at Hebei General Hospital between March 2015 and
January 2017. Inclusion criteria were as follows: i) patients
received treatment for the first time; ii) patients with normal
major organ function; and iii) patients willing to participate in
the study. Exclusion criteria were as follows: i) detection of
other severe diseases or other respiratory diseases; ii) patients
aged ≥70 years (chronic disease prevalence rates are increased in
patients aged ≥70 years); and iii) patients with lung inflammation
caused by other factors. In addition, 40 healthy controls who
received physical examinations were included in the current study
as the control group. No significant differences in age and gender
were observed among the three groups (Table I). Blood samples were collected from
all participants on the first day of admission. Lung biopsies were
obtained from 25/44 (57%) patients in the diabetic lung group. This
study was approved by the Ethics Committee of Hebei General
Hospital (Shijiazhuang, China). All participants and/or their
families provided written informed consent.
 | Table I.Basic information of participants. |
Table I.
Basic information of participants.
| Group | n | Male (n) | Female (n) | Age range, years | Mean age, years |
|---|
| Control | 40 | 26 | 14 | 24–69 | 46.0±6.4 |
| Diabetes | 56 | 30 | 26 | 26–69 | 44.8±5.2 |
| Diabetic lung | 44 | 24 | 20 | 23–67 | 45.1±5.1 |
Cell culture and transfection
Normal human lung cell line BEAS-2B
(ATCC® CRL-9609™) was purchased from the American Type
Culture Collection (ATCC). Cells were cultured in ATCC-formulated
Eagle's Minimum Essential Medium (cat. no. 30-2003; ATCC)
supplemented with 10% FBS (Sangon Biotech Co., Ltd.) and maintained
at 37°C in a 5% CO2-humidified incubator. The
full-length SACL1 cDNA fragment was obtained by PCR amplification
and cloned into the linearised pIRSE2 vector (Clontech
Laboratories, Inc.) to generate the SACL1 expression vector.
Lipofectamine® 2000 reagent (Thermo Fisher Scientific,
lnc.) was initially mixed with expression vectors (10 nm) to form
transfection reagent-vector complexes, prior to transfection. Cells
were transfected with transfection reagent-vector complexes at 37°C
for 5 h at 37°C. Cells were subsequently washed with fresh
ATCC-formulated Eagle's Minimum Essential Medium to avoid
cytotoxicity. Cells transfected with empty pIRSE2 vector were used
as the negative control (NC), while untransfected cells were used
as the control (C). SACL1 overexpression was confirmed by RT-qPCR
at 24 h post-transfection and cells were collected at this time
pointfor subsequent experimentation.
NO assay
Total NO in the cell culture supernatant was
examined using the Nitric Oxide Detection kit (cat. no.
ADI-917-010; Enzo Life Sciences, Inc.), according to the
manufacturer's protocol.
Reverse transcription-quantitative PCR
(RT-qPCR)
Total RNA was extracted from blood, tissue and cells
using TRIzol® reagent (Invitrogen; Thermo Fisher
Scientific, Inc.), according to the manufacturer's protocol. For
in vitro experiments, BEAS-2B cells were treated with
D-glucose (5, 10, 20, 30 and 40 mM) for 5, 10 and 15 h at 37°C.
Total RNA was reverse transcribed into cDNA using SuperScript III
Reverse Transcriptase (Thermo Fisher Scientific, Inc.). The
following conditions were used for RT: 50°C for 15 min and 80°C for
10 min. qPCR was subsequently performed using SYBR®
Green Real-Time PCR Master mix (Thermo Fisher Scientific, Inc.).
The following primer pairs were used for qPCR: lncRNA SACL1
forward, 5′-GTGTCAAGCTCGGATTGCCT-3′ and reverse,
5′-GAGCCCACACACTCAGGTTC-3′; iNOS forward,
5′-CCCTTCCGAAGTTTCTGGCAGCAG-3′ and reverse,
5′-GGCTGTCAGAGCCTCGTGGCTTTGG-3′; and β-actin forward,
5′-GACCTCTATGCCAACACAGT-3′ and reverse, 5′-AGTACTTGCGCTCAGGAGGA-3′.
The following thermocycling conditions were used for qPCR: Initial
denaturation at 95°C for 40 sec, 40 cycles of 95°C for 20 sec and
57°C for 30 sec. All data were quantified using the
2−ΔΔCq method (10) and
normalized to the internal control β-actin.
Western blot analysis
Total protein was extracted from cells using RIPA
buffer (Thermo Fisher Scientific, Inc.), according to the
manufacturer's protocol. For in vitro experiments, cells
were treated with D-glucose (30 mM) for 15 h at 37°C. Total protein
was quantified using a bicinchoninic acid assay and 20 µg
protein/lane was separated via SDS-PAGE on a 10% gel. The separated
proteins were transferred onto PVDF membranes, and then blocked for
1 h at room temperature with 5% skimmed milk. Membranes were washed
and incubated with primary antibodies against iNOS (1:1,200;
ab3523) and GAPDH (1:1,000; ab9485; both Abcam) overnight at 4°C.
Membranes were washed and then incubated with horseradish
peroxidase-labeled anti-rabbit IgG secondary antibody (1:1,000;
MBS435036; MyBioSource) for 1 h at room temperature. Protein bands
were visualized using Pierce™ ECL Western Blotting Substrate
(Pierce; Thermo Fisher Scientific, Inc.). Protein expression was
quantified using ImageJ v1.48 software (National Institutes of
Health) and normalized to the loading control GAPDH.
Statistical analysis
Data were presented as the mean ± standard
deviation. All statistical analyses were performed using GraphPad
Prism software (version 6.0; GraphPad Software). One-way analysis
of variance followed by the least significant difference test was
used to analyze differences among multiple groups. Correlation
analyses were performed using Pearson's correlation analysis.
Receiver operating characteristic (ROC) curve analysis was
performed to evaluate the diagnostic value of serum lncRNA SCAL1 in
diabetic patients with diabetic lung disease compared with healthy
controls. P<0.05 was considered to indicate a statistically
significant difference.
Results
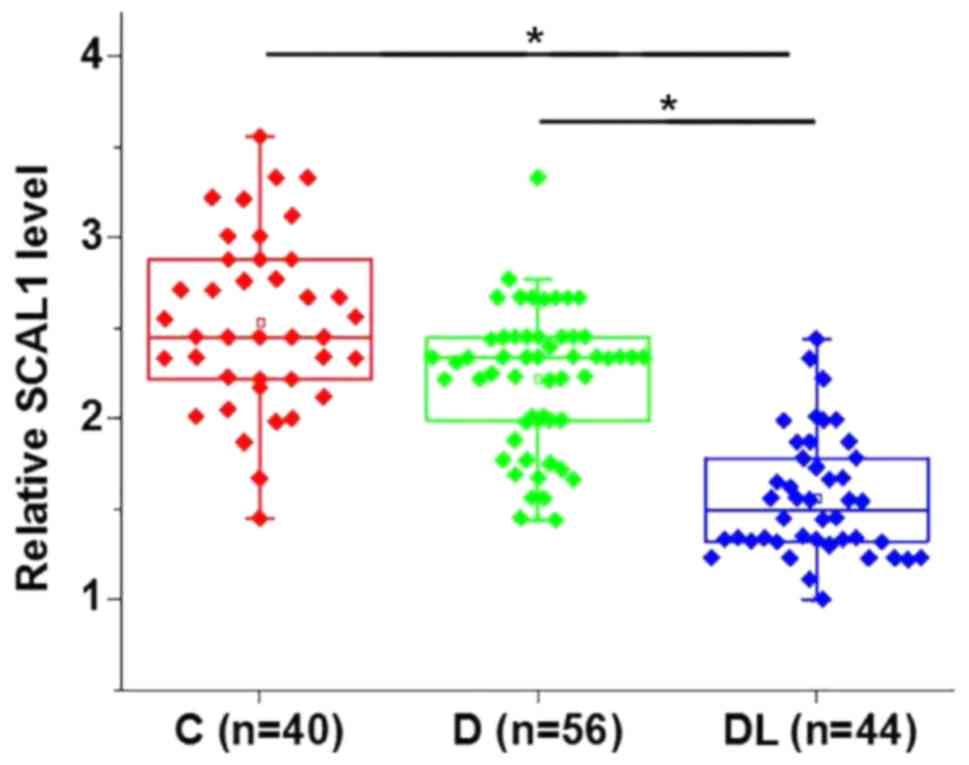
Serum levels of lncRNA SCAL1 were
significantly downregulated in diabetic patients with diabetic lung
disease
Differentially expressed genes between healthy
controls and patients with a disease can often indicate the
involvement of certain genes in a disease. The relative expression
level of lncRNA SACL1 was determined by RT-qPCR in serum samples
from healthy controls, diabetic patients without lung disease and
diabetic patients with diabetic lung disease. The serum expression
level of lncRNA SACL1 was significantly decreased in diabetic
patients with diabetic lung disease compared with diabetic patients
without lung disease and healthy controls (P<0.05; Fig. 1). Serum levels of SACL1 were
decreased in diabetic patients without lung disease compared with
healthy controls; however, the difference was not statistically
significant.
Low serum lncRNA SCAL1 distinguishes
diabetic patients with diabetic lung disease from diabetic patients
without diabetic lung disease and healthy controls
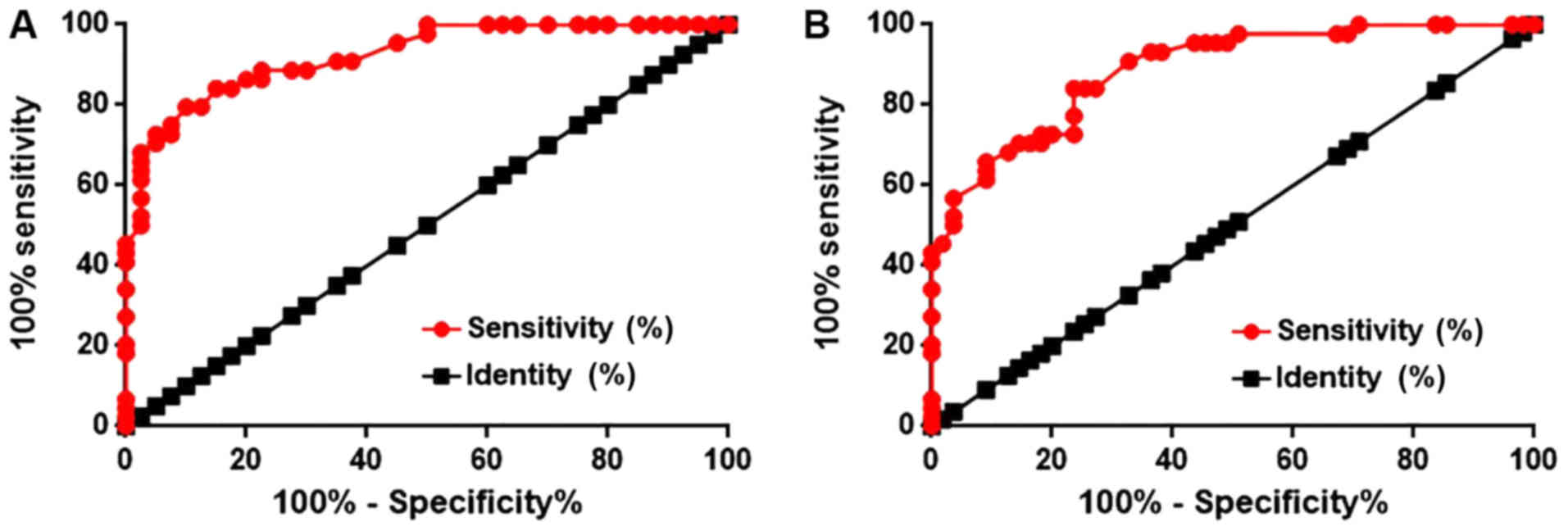
ROC curve analysis determined that the area under
the curve (AUC) was 0.9233 (95% confidence interval: 0.8679–0.9769)
with a standard error of 0.02735 (Fig.
2A). In addition, ROC analysis was used to evaluate the
diagnostic value of serum lncRNA SCAL1 in discriminating diabetic
patients with diabetic lung disease from diabetic patients without
diabetic lung disease. The AUC was 0.8876 (95% confidence interval:
0.8254–0.9498) with a standard error of 0.03174 (Fig. 2B). An AUC>0.65 indicates the
potential diagnostic value of a certain indicator for a disease
(11). Therefore, serum levels of
lncRNA SCAL1 can be used to effectively distinguish diabetic lung
patients from healthy controls and diabetic patients without lung
disease.
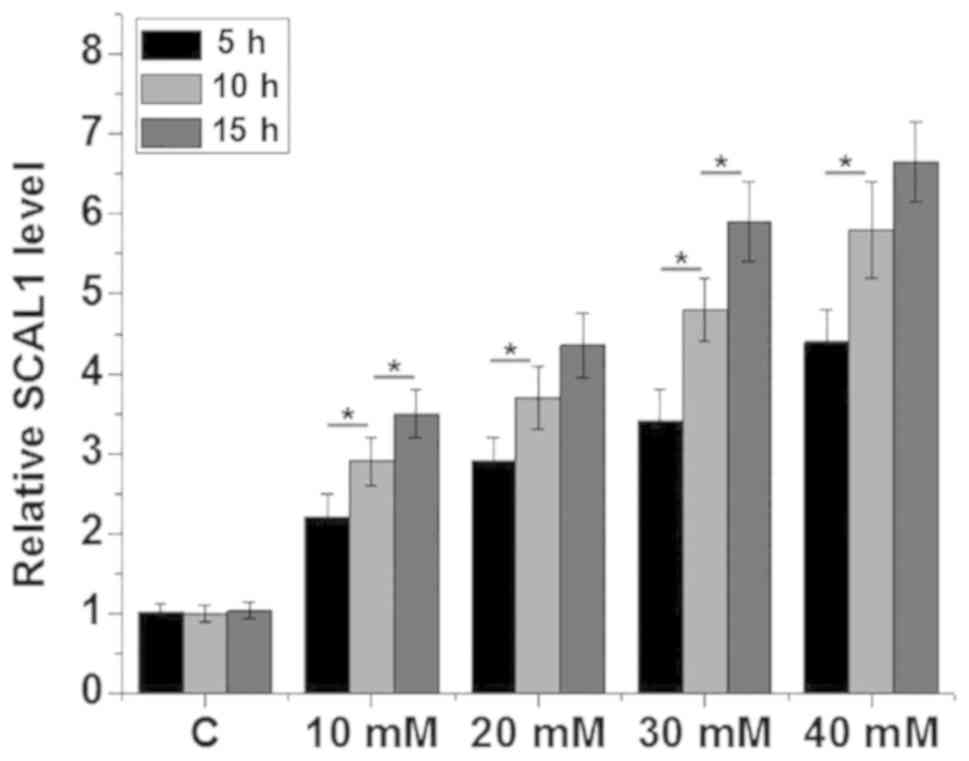
Expression levels of lncRNA SCAL1 are
significantly upregulated in normal human lung cells following
treatment with high glucose
D-glucose (5, 10, 20, 30 and 40 mM) was used to
treat the BEAS-2B normal human lung cell line for 5, 10 and 15 h,
respectively. The relative SCAL1 expression levels were
significantly increased in lung cells treated with high glucose
(10, 20, 30 and 40 mM) concentrations in a time- and dose-dependent
manner compared with the control group (P<0.05; Fig. 3).
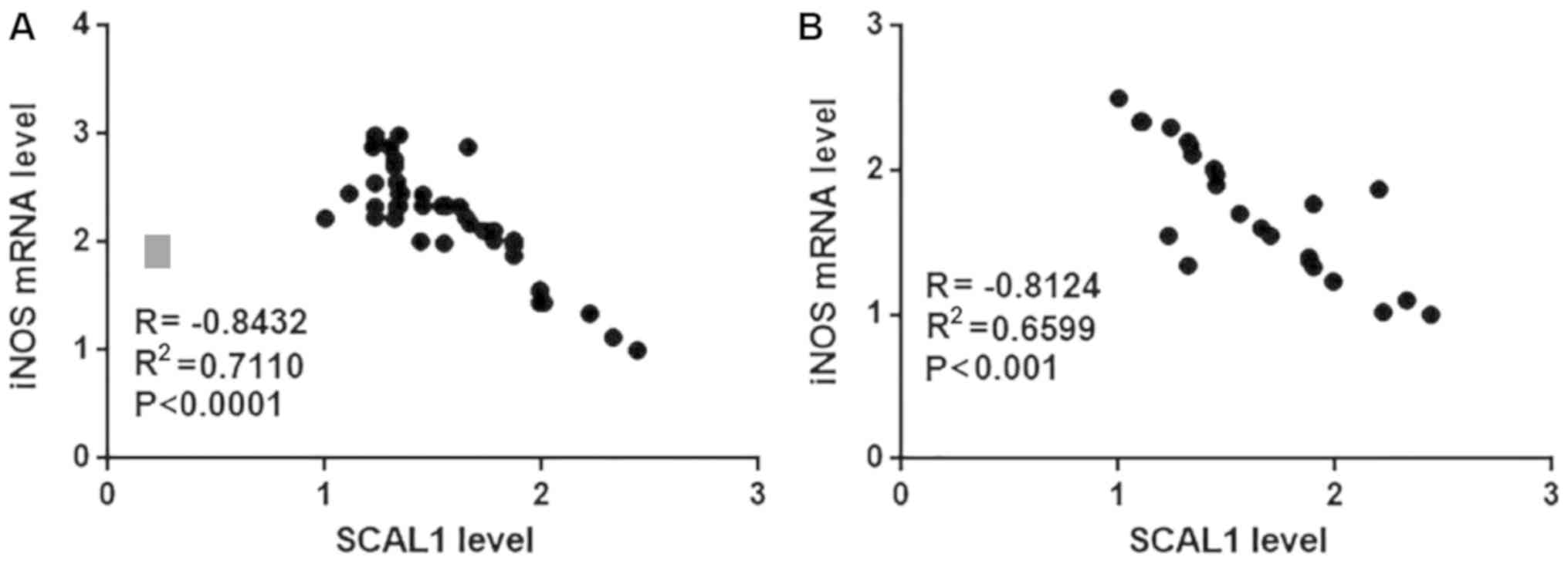
SCAL1 and iNOS mRNA expression in
blood and lung tissue samples are negatively correlated in diabetic
patients with diabetic lung disease
Pearson correlation analysis was used to examine the
correlation between SCAL1 and iNOS mRNA expression in blood and
lung tissue samples from diabetic patients with diabetic lung
disease. Pearson's correlation analysis indicated a significant
negative correlation between SCAL1 and iNOS mRNA expression levels
in blood (R=−0.8432, P<0.0001; Fig.
4A) and lung tissue samples (R2=−0.8124, P<0.001;
Fig. 4B) from diabetic patients with
diabetic lung disease. No significant correlation was observed
between SCAL1 and iNOS expression levels in blood and lung tissue
samples from diabetic patients without diabetic lung disease or
healthy controls (data not shown).
SCAL1 overexpression inhibits iNOS
expression and reduces NO production in normal human lung
cells
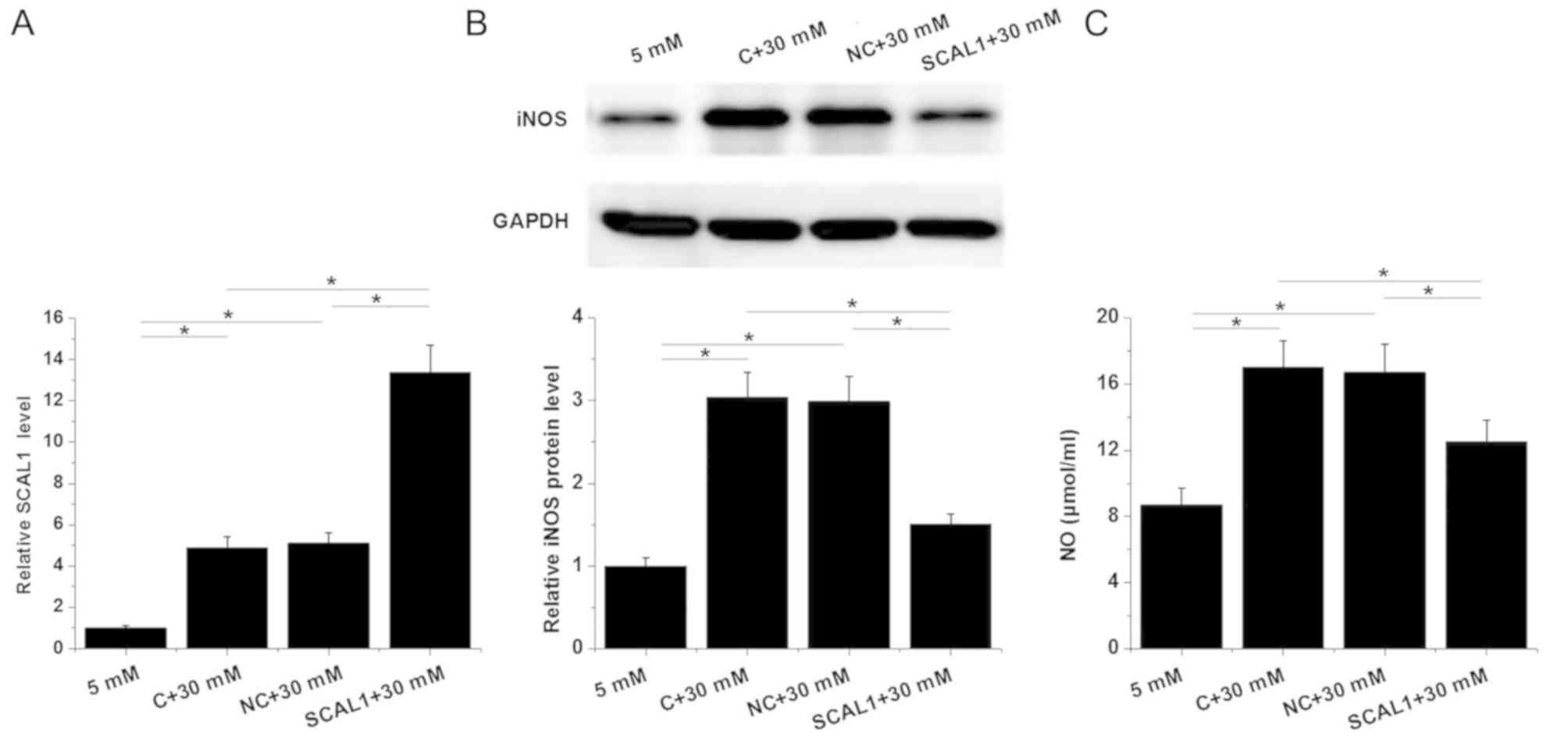
The expression of lncRNA SACL1 was determined by
RT-qPCR in normal human lung cells following transfection with
SCAL1 expression vector and treatment with D-glucose (30 mM).
Untransfected cells and cells transfected with empty circular
pIRSE2 vector were used as control and negative control groups,
respectively (Fig. 5). The relative
expression level of lncRNA SACL1 was significantly increased in the
control group following treatment with high (30 mM D-glucose)
glucose compared with the group treated with low (5 mM D-glucose)
glucose (Fig. 5A). In addition, the
relative expression level of lncRNA SACL1 was significantly
increased in cells following transfection with SCAL1 expression
vector compared with the negative control, indicating that the
transfection was successful (P<0.05; Fig. 5A).
The relative protein expression level of iNOS, and
secretion of NO into the cell supernatant were significantly
upregulated in cells treated with high glucose compared with those
treated with low glucose (P<0.05; Fig. 5B and C). The overexpression of SCAL1
inhibited iNOS protein expression and reduced NO production
following treatment with high glucose compared with the high
glucose-treated controls (P<0.05; Fig. 5B and C). Furthermore, no significant
differences were observed in the protein expression level of iNOS
and NO production in cells following the overexpression of SCAL1
and treatment with low glucose compared with control cells
following treatment with low glucose (data not shown).
Discussion
Excessive NO production plays a pivotal role in the
development of diabetic lung disease (7). The current study demonstrated that
SCAL1, a lncRNA with a role in lung cancer, may be involved in the
pathogenesis of diabetic lung disease. It also indicated that
underlying mechanism of SCAL1 in diabetic lung may be via the
downregulation of iNOS expression and reduced NO production.
Glucotoxicity, which is caused by a high-glucose
environment in patients with diabetes, affects the expression
levels of several genes as well as lncRNAs (12,13).
Altered expression of lncRNAs may participate in the pathogenesis
of diabetes-associated complications by controlling blood glucose
concentrations (14,15). SCAL1 is upregulated in human lung
cancer cell lines in response to cigarette smoke (9). In the current study, serum expression
levels of SCAL1 were decreased in diabetic patients without lung
disease compared with healthy controls, although the difference was
not observed to be significant. However, in vitro
experiments performed in the present study suggest that the
expression level of lncRNA SCAL1 was upregulated under high-glucose
conditions. Therefore, it is suggested that the downregulation of
SCAL1 expression in patients with diabetic lung disease may be
induced by the formation of lung lesions.
Diabetic lung disease is one of the least studied
diabetes-associated complications and its pathogenesis is largely
unknown, leading to difficulties in disease diagnosis. A previous
study reported that caveolin-1 overexpression is associated with
structural modifications of endothelial cells in patients with
diabetic lung disease, indicating the potential application of
caveolin-1 as a diagnostic biomarker for diabetic lung disease
(16). The development of human
disease is usually associated with changes in certain substances in
the blood, and the detection of those substances may provide
guidance for disease diagnosis (17). In the current study, the relative
expression levels of SCAL1 were significantly downregulated in
patients with diabetic lung disease, and downregulated serum
expression levels of SCAL1 effectively distinguished diabetic
patients with diabetic lung disease from diabetic patients without
lung disease and healthy controls. Therefore, serum SCAL1 may serve
as a potential diagnostic biomarker for diabetic lung disease in
diabetic patients.
Excessive production of NO is thought to be involved
in the pathogenesis of different human diseases, including diabetic
lung disease (7,18,19) and,
therefore, inhibition of NO production may suppress the development
of those diseases. In the current study, the lncRNA SCAL1
expression level was inversely correlated with the iNOS mRNA
expression level in blood and lung tissue samples from patients
with diabetic lung disease. Furthermore, SCAL1 overexpression
inhibited iNOS protein expression and NO production in normal lung
cells. Therefore, SCAL1 may be used as a therapeutic target for the
prevention and treatment of diabetic lung disease. The current
study demonstrated a potential interaction between SCAL1 and iNOS
in lung tissue under high-glucose conditions; however, whether this
interaction is direct or indirect remains unknown and further
experimentation is required to further examine this
interaction.
The current study is limited by the small sample
size; therefore, future studies with a larger sample size are
required to further confirm the conclusions made. In addition, the
underlying molecular mechanism by which SCAL1 regulates iNOS
remains unclear and requires further investigation.
In conclusion, the relative expression levels of
SCAL1 were significantly downregulated in diabetic patients with
diabetic lung disease. SCAL1 expression may suppress diabetic lung
disease by inhibiting iNOS protein expression, and thereby reducing
the production of NO in lung tissues.
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
PL designed experiments. PL and NZ performed
experiments. PL, FP, YG and LC assisted experiments and analyzed
data. PL drafted the manuscript and all authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Hebei General Hospital (Shijiazhuang, China). All
participants and/or their families provided written informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Piero MN, Nzaro GM and Njagi JM: Diabetes
mellitus-a devastating metabolic disorder. Asian J Biomed Pharm.
5:1–7. 2015. View Article : Google Scholar
|
|
2
|
Shaw JE, Sicree RA and Zimmet PZ: Global
estimates of the prevalence of diabetes for 2010 and 2030. Diabetes
Res Clin Pract. 87:4–14. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li MZ, Su L, Liang BY, Tan JJ, Chen Q,
Long JX, Xie JJ, Wu GL, Yan Y, Guo XJ and Gu L: Trends in
prevalence, awareness, treatment, and control of diabetes mellitus
in mainland China from 1979 to 2012. Int J Endocrinol. 753150,
2013. 2013. View Article : Google Scholar
|
|
4
|
Roglic G: WHO Global report on diabetes: A
summary. Int J Noncommun Dis. 1:3–8. 2016. View Article : Google Scholar
|
|
5
|
Pitocco D, Fuso L, Conte EG, Zaccardi F,
Condoluci C, Scavone G, Incalzi RA and Ghirlanda G: The diabetic
lung-a new target organ. Rev Diabet Stud. 9:23–25. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hsia CC and Raskin P: The diabetic lung:
Relevance of alveolar microangiopathy for the use of inhaled
insulin. Am J Med. 118:205–211. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Agrawal A: Diabetic Lung: A Sweet Kiss of
Impending Death. EC Pulmonology and Respiratory Medicine.
7:341–342. 2018.
|
|
8
|
Leferink NG, Hay S, Rigby SE and Scrutton
NS: Towards the free energy landscape for catalysis in mammalian
nitric oxide synthases. FEBS J. 282:3016–3029. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Thai P, Statt S, Chen CH, Liang E,
Campbell C and Wu R: Characterization of a novel long noncoding
RNA, SCAL1, induced by cigarette smoke and elevated in lung cancer
cell lines. Am J Respir Cell Mol Biol. 49:204–211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hanley JA and McNeil BJ: The meaning and
use of the area under a receiver operating characteristic (ROC)
curve. Radiology. 143:29–36. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kaizer EC, Glaser CL, Chaussabel D,
Banchereau J, Pascual V and White PC: Gene expression in peripheral
blood mononuclear cells from children with diabetes. J Clin
Endocrinol Metab. 92:3705–3711. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Reynier F, Pachot A, Paye M, Xu Q,
Turrel-Davin F, Petit F, Hot A, Auffray C, Bendelac N, Nicolino M,
et al: Specific gene expression signature associated with
development of autoimmune type-I diabetes using whole-blood
microarray analysis. Genes Immun. 11:269–278. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Alvarez ML and DiStefano JK: The role of
non-coding RNAs in diabetic nephropathy: potential applications as
biomarkers for disease development and progression. Diabetes Res
Clin Pract. 99:1–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
He X, Ou C, Xiao Y, Han Q, Li H and Zhou
S: LncRNAs: Key players and novel insights into diabetes mellitus.
Oncotarget. 8:71325–71341. 2017.PubMed/NCBI
|
|
16
|
Uyy E, Antohe F, Ivan L, Haraba R, Radu DL
and Simionescu M: Upregulation of caveolin-1 expression is
associated with structural modifications of endothelial cells in
diabetic lung. Microvasc Res. 79:154–159. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tobolowsky FA, Wada N, Martinez-Maza O,
Magpantay L, Koletar SL, Palella FJ Jr, Brown TT and Lake JE: Brief
report: Circulating markers of fibrosis are associated with immune
reconstitution status in HIV-infected men. PLoS One.
13:e01916062018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yuste JE, Tarragon E, Campuzano CM and
Ros-Bernal F: Implications of glial nitric oxide in
neurodegenerative diseases. Front Cell Neurosci. 9:3222015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakamura T and Lipton SA: Protein
S-nitrosylation as a therapeutic target for neurodegenerative
diseases. Trends Pharmacol Sci. 37:73–84. 2016. View Article : Google Scholar : PubMed/NCBI
|