Introduction
The number of cases of coronary heart disease (CHD)
is increasing worldwide. The Chinese cardiovascular disease report
of 2016 indicated that the current number of cases of CHD was ~11
million (1). In 2015, the mortality
rate from CHD in Chinese urban and rural residents was
significantly higher than in 2014.
In recent years, several biological factors have
been studied in association with CHD. Certain inflammatory factors,
including tumor necrosis factor (TNF), soluble intercellular
adhesion molecules (e.g. vascular cellular adhesion molecule-1 and
intercellular adhesion molecule-1), matrix metalloproteinases,
hypersensitive C-reactive protein (hs-CRP) and interleukin-6 (IL-6)
have all been extensively studied in different groups of patients
with CHD (2). It has been indicated
that Toll-like receptors (TLRs) are involved in the occurrence and
development of coronary atherosclerosis (3), implying that TLRs may be potential
novel targets for intervention of atherosclerosis. A previous study
suggested that the protein expression of TLR2 and TLR4 was involved
in the regulation of cardiovascular function in mice (4).
The Han and Zhuang ethnic groups make up the largest
proportion of the population of the Guangxi Zhuang Autonomous
Region of China (62 and 32%, respectively). Previously, a large
number of studies have focused on diseases in these two groups
within the population with several genetic differences, including
the prevalence of genes linked to hyperlipidemia and 3′APOB-VNTR
polymorphisms, and other differences, including the presence of
many pharmacogenetic variants and drug detoxification mechanisms,
having been identified (5–7). In this light, the present study was
performed to explore diagnostic biomarkers of coronary artery
stenosis in patients of the ethnic Zhuang group with CHD and to
validate potential correlations between the expression levels of
TLR2/4 in the circulatory system. The results indicated that the
measurement of TLR2/4 provides a tool for early clinical diagnosis
and a simple way of assessing the severity of CHD in such
patients.
Patients and methods
Patients
The present study complied with the Declaration of
Helsinki and was approved by the Ethics Committee Review Board of
the Affiliated Hospital of Youjiang Medical University for
Nationalities (Baise, China). Written informed consent was obtained
from each of the patients enrolled in the study. The present study
is a prospectively planned observational study on 568 subjects
admitted to The Affiliated Hospital of Youjiang Medical University
(Baise, China) between January 2016 and August 2016 who underwent
coronary angiography. They were divided into two groups according
to the results of coronary angiography, namely the CHD group (with
≥50% stenosis) and a control group (with no stenosis). They were
all from the Zhuang ethnic group. Patients with CHD (males, n=297;
females, n=169; age, 38–81 years; average age, 59.76±10.40 years).
In addition, 102 healthy individuals were recruited during the same
time period (males, n=57; females, n=45; age, 41–72 years; average
age, 62.15±10.32 years).
The exclusion criteria for the CHD group of patients
were as follows: Participants with rheumatic heart disease, dilated
cardiomyopathy, congenital heart disease, patients undergoing
intravenous thrombolysis, coronary stenting and coronary artery
bypass grafting, systemic or local severe infection,
auto-immunologic and blood system disease, severe kidney or liver
disease or malignant disease. The healthy control group of patients
were recruited from the Out-patients area within the hospital
including the renal and respiratory departments. None of the
patients included in the study had severe symptoms and they were
discharged within 12 h of admission. All patients who had severe
illnesses and were kept >12 h and those who had a history of
heart disease were also excluded from the study.
The CHD cases were further divided into the
following subgroups according to the number of diseased vessels: i)
Cases with single-vessel disease (n=127; 81 males and 46 females;
average age, 58.56±10.41 years), ii) cases with double-vessel
disease (n=243; 156 males and 87 females; average age, 60.97±10.26
years) and iii) cases with multi-vessel disease (n=96; 55 males and
41 females; average age, 58.25±10.46 years). The quantitative
analysis of the severity of coronary artery disease was performed
according to the Gensini integral (8), based on which the patients were
stratified into three groups: i) Mild stenosis group (n=126; 55
males and 71 females; average age, 58.88±10.84 years), ii) moderate
stenosis group (n=261; 175 males and 86 females; average age,
60.21±10.26 years) and iii) severe stenosis group (n=79; 49 males
and 30 females; average age, 59.65±10.70 years).
There were no significant differences in gender,
age, smoking habits, alcohol consumption, body mass index (BMI),
blood pressure and incidence of diabetes between the CHD and
control groups. None of the cases included in the present study had
any severe infections, immune system diseases, connective tissue
disease, blood system diseases, malignant tumors, liver and kidney
malfunctions, recent major surgeries or severe trauma.
Methods
All subjects were routinely fasted for at least 8 h
prior to obtainment of blood samples for analysis. These included
tests for glucose, lipid proteins, liver and renal function
parameters. The subjects were also subjected to the oral glucose
tolerance test. The protein concentrations of TLR2 and TLR4 in the
serum were detected using RT-6000 ELISA kits (Rayto Life and
Analytical Sciences Co., Ltd.). TLR2 and TLR4 kits were obtained
from Wuhan Huamei Biological Engineering Co., Ltd. The intra- and
inter-assay coefficient of variation for the ELISA kits were
determined to be <5% and <15%, respectively. The detection
limits of the ELISAs were 0.54 and 1.38 ng/ml for TLR2 and TLR4,
respectively.
Blood was collected aseptically from the caudal vein
by venipuncture into one of three vacutainer tubes containing
either sodium heparin, sodium citrate or EDTA. These tubes were
immediately centrifuged at 375 × g for 15 min in bench centrifuge
at 4°C and samples were prepared or analyzed within 45 min of
collection. Aliquots were frozen at −80°C for ELISA.
All patients underwent a routine coronary
angiography in strict accordance with the operating procedures. The
coronary intervention was an adaptation of the Judkins technique
(8). The right radial artery or
femoral artery paths were followed during the operation, which was
performed by at least two interventional cardiovascular physicians.
The coronary angiography results were recorded in detail together
with the degree of stenosis and blood flow of the coronary lesions.
When the degree of coronary artery stenosis of at least one vessel
in the left main stem, the left anterior descending branch, the
left circumflex branch, the right coronary artery or its major
branches was >50%, this was diagnosed as CHD. According to the
number of vascular lesions involved in the disease, the patients
were classified into i) the single-vessel disease group, ii) the
double-vessel disease group or iii) the multi-vessel disease group.
The Gensini score was determined according to the degree of each
lesion of vessel stenosis (9).
Statistical analysis
SPSS 17.0 software (SPSS, Inc.) was used for
statistical analysis. Measurement data are expressed as the mean ±
standard deviation. Comparisons between multiple groups were
performed using single-factor analysis of variance followed by
Tukey's post hoc test. Comparisons between two groups were
performed using the unpaired t-test, while the Shapiro-Wilk test
was used to check whether the data were normally distributed.
P<0.05 was considered to indicate statistical significance. The
correlation between the severity of coronary artery stenosis and
TLR2 or TLR4 was determined using Pearson's correlation analysis.
Comparison between the clinicopathological parameters of the
patients in the CHD and control groups were compared using the
paired Chi-square test.
Results
Characteristics of patients
The CHD and the control groups were not
significantly different in many of the general characteristics,
including gender, age, smoking and drinking habits, BMI and
incidence of hypertension and diabetes, indicating that the
baseline characteristics of the subjects were consistent and
comparable between the two groups (Table
I).
 | Table I.Characteristics of the control
subjects and CHD patients in the present study. |
Table I.
Characteristics of the control
subjects and CHD patients in the present study.
| Parameter | Control subjects
(n=102) | CHD patients
(n=466) |
χ2/t-value | P-value |
|---|
| Age (years) | 62.15±10.32 | 59.76±10.40 | 1.066 | 0.286 |
| BMI
(kg/m2) | 21.39±2.58 | 22.17±2.91 | 0.844 | 0.399 |
| Sex |
|
| 2.197 | 0.138 |
| Male | 57(55.9) | 297 (63.7) |
|
|
|
Female | 45(44.1) | 169 (36.3) |
|
|
| Smoking |
|
| 0.376 | 0.539 |
| Yes | 32 (31.4) | 161 (34.5) |
|
|
| No | 70 (68.6) | 305 (65.5) |
|
|
| Alcohol
consumption |
|
| 1.980 | 0.159 |
| Yes | 27 (26.5) | 94
(20.2) |
|
|
| No | 75 (73.5) | 372 (79.8) |
|
|
| Hypertension |
|
| 2.219 | 0.136 |
| Yes | 32 (31.4) | 183 (39.3) |
|
|
| No | 70 (68.6) | 283 (60.7) |
|
|
| Type 2 diabetes
mellitus |
|
| 0.122 | 0.727 |
| Yes | 11 (10.8) | 56
(12.0) |
|
|
| No | 91 (89.2) | 410 (88.0) |
|
|
TLR protein levels in patient
groups
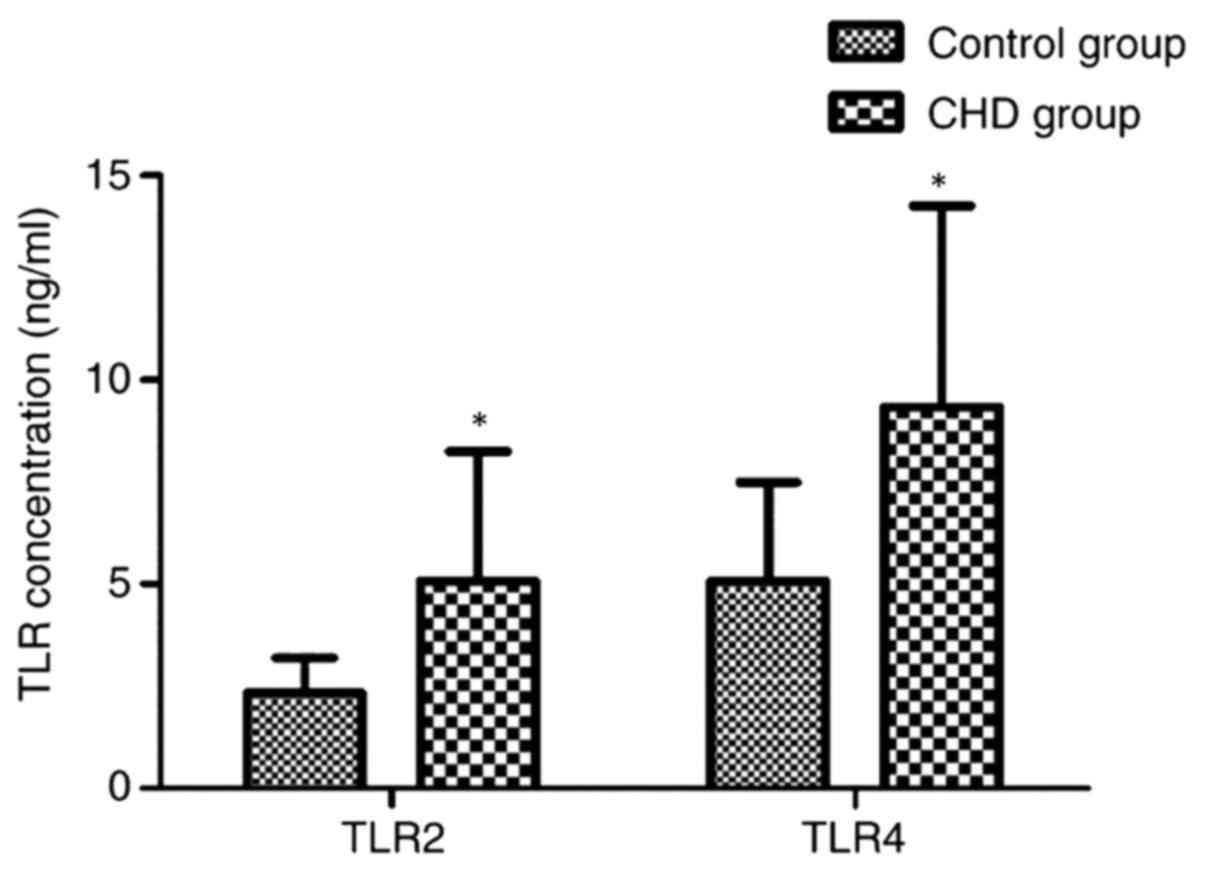
Comparison of the protein expression levels of TLR2
and TLR4 between the CHD and the control groups was performed by
ELISA measurements in the sera of all 568 patients. The results
indicated that the respective concentrations of TLR2 and TLR4 in
the serum were 5.22±3.16 and 9.33±4.92 ng/ml in CHD patients, and
the values obtained for control subjects were significantly lower
at 2.34±0.85 and 5.08±2.41 ng/ml, respectively (P<0.001;
Table II and Fig. 1). This suggests that the serum
concentrations of TLR2 and TLR4 are closely linked to the
occurrence and development of CHD in the ethnic Zhuang
population.
 | Table II.Concentrations of TLR2 and TLR4 in
control and CHD patients. |
Table II.
Concentrations of TLR2 and TLR4 in
control and CHD patients.
| Protein | Control subjects
(n=102) | CHD patients
(n=466) | t-value | P-value |
|---|
| TLR2 (ng/ml) | 2.34±0.85 | 5.22±3.16 | 17.039 | <0.001 |
| TLR4 (ng/ml) | 5.08±2.41 | 9.33±4.92 | 12.892 | <0.001 |
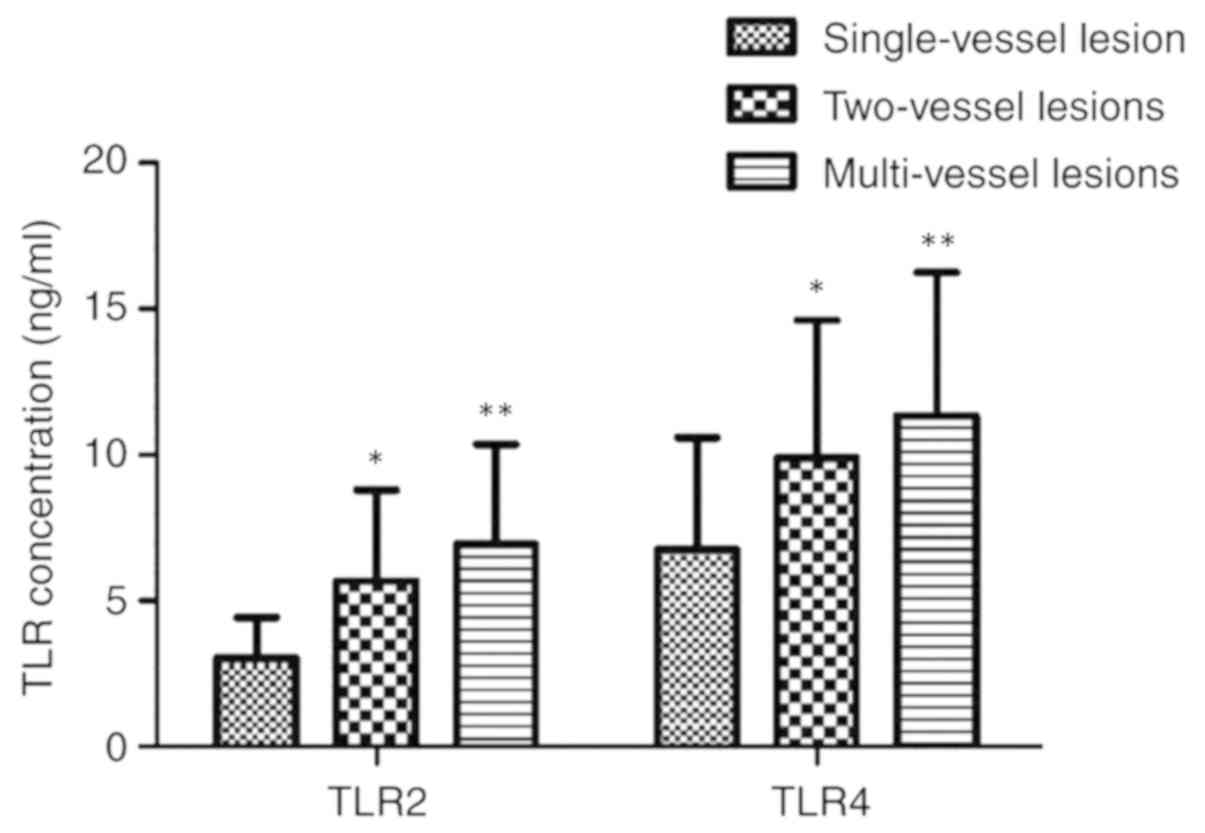
Comparisons of the expression levels of TLR2 or TLR4
between different groups according to the number of coronary
lesions were also performed. The concentration of TLR2 in the serum
was 3.05±1.38, 5.67±3.12 and 6.94±3.41 ng/ml, in the single-,
double- and multi-lesion group, respectively. The corresponding
values for TLR4 in the three groups were 6.75±3.84, 9.89±4.72 and
11.34±5.3 ng/ml, respectively (P<0.01; Table III and Fig. 2). The highest expression of TLR was
in the multi-vessel lesion group, followed by the two-vessel lesion
group and the lowest expression was in the single-vessel lesion
group.
 | Table III.Association between the levels of TLR2
or TLR4 in patients with coronary heart disease and the number of
coronary lesions. |
Table III.
Association between the levels of TLR2
or TLR4 in patients with coronary heart disease and the number of
coronary lesions.
| Protein | Single-vessel lesion
(n=127) | Two-vessel lesions
(n=243) | Multi-vessel
lesions (n=96) | F-value | P-value |
|---|
| TLR2 (ng/ml) | 3.05±1.38 |
5.67±3.12a |
6.94±3.41a,b | 108.436 | <0.01 |
| TLR4 (ng/ml) | 6.75±3.84 |
9.89±4.72a |
11.34±5.30a,b | 58.775 | <0.01 |
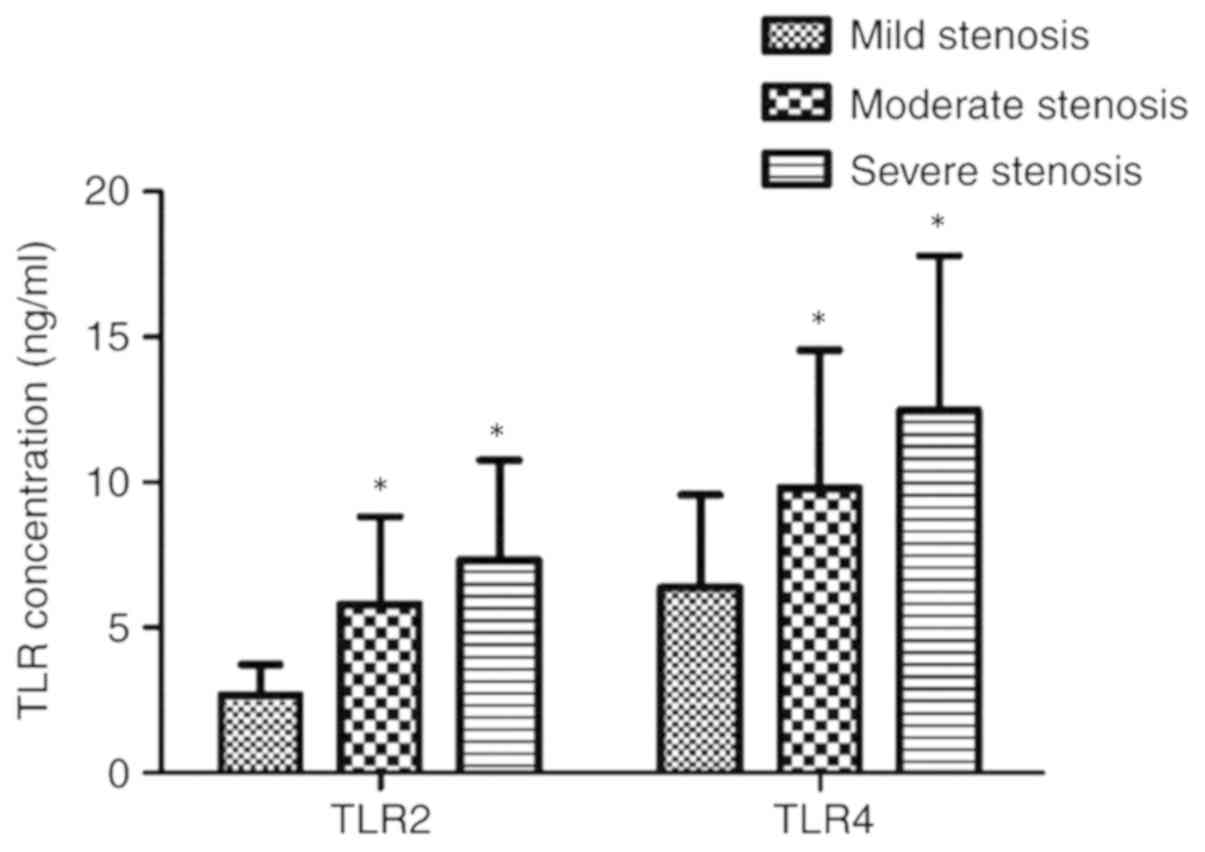
The expression levels of TLR2 and TLR4 protein
between the subgroups by severity of coronary artery stenosis were
2.67±1.06, 5.81±2.99 and 7.32±3.44 ng/ml, respectively, for the
mild, moderate and severe stenosis groups. The corresponding values
for TLR4 in the three groups were 6.38±3.17, 9.80±4.74 and
12.48±5.32 ng/ml, respectively. The levels of TLR2 and TLR4 in the
severe stenosis group were markedly higher than those in the mild
and moderate stenosis groups, and the TLR2 and TLR4 levels in the
moderate stenosis group were higher than those in the mild stenosis
group (P<0.01; Table IV and
Fig. 3). These results imply that in
the Zhuang ethnic group of patients, the degree of coronary artery
stenosis is associated with the circulatory levels of TLR2 and
TLR4, with higher levels observed in the more severe cases of
CHD.
 | Table IV.Association between the levels of
TLR2 or TLR4 in patients with coronary heart disease and the
severity of coronary artery stenosis. |
Table IV.
Association between the levels of
TLR2 or TLR4 in patients with coronary heart disease and the
severity of coronary artery stenosis.
| Protein | Mild stenosis
(n=126) | Moderate stenosis
(n=261) | Severe stenosis
(n=79) | F-value | P-value |
|---|
| TLR2 (ng/ml) | 2.67±1.06 |
5.81±2.99a |
7.32±3.44a,b | 162.697 | <0.01 |
| TLR4 (ng/ml) | 6.38±3.17 |
9.80±4.74a |
12.48±5.32a,ßb | 81.155 | <0.01 |
Correlation between TLR expression and
vessel stenosis
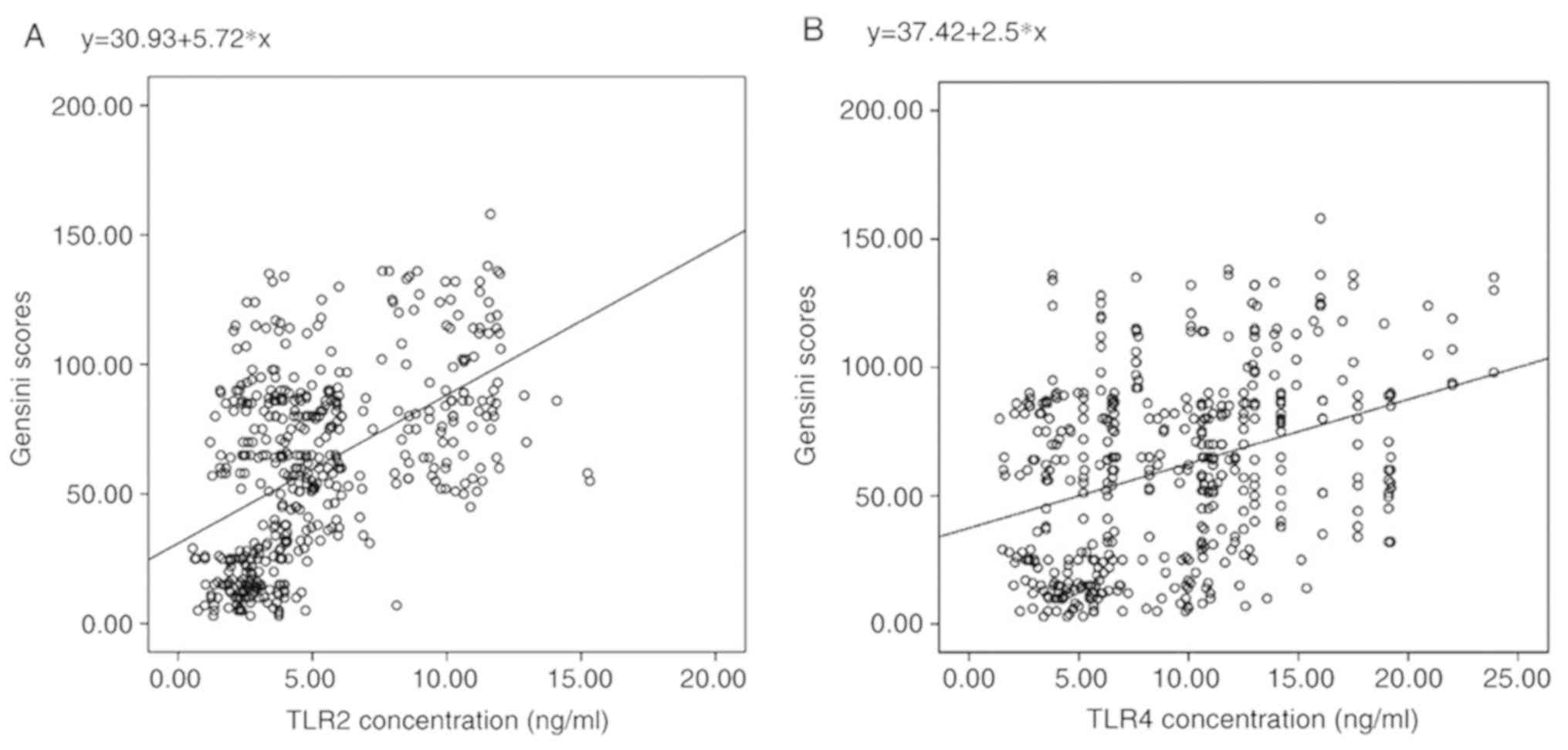
Positive correlations between the expression levels
of TLR2 or TLR4 and the coronary Gensini score were determined
using Pearson's correlation analysis. From this, the R-values were
calculated to be 0.508 and 0.346 for TLR2 and TLR4, respectively
(P<0.0001; Fig. 4A and B). It
appeared that in Zhuang patients with CHD, the severity of coronary
artery lesions is correlated with the plasma levels of TLR2 or TLR4
and that the patients with higher plasma concentrations of TLR2 and
TLR4 have a higher degree of severity of coronary artery
lesions.
Discussion
CHD that occurs due to coronary vascular
atherosclerosis proceeds to luminal stenosis and/or obstruction, or
coronary artery blood vessel function changes (spasms) and
myocardial tissue ischemia, hypoxia or necrosis. The associated
pathological changes result in atherosclerotic coronary blood
vessels, which in turn form stable or unstable plaques. These
events are the preclinical phase of coronary disease, frequently
leading to the rupture of plaques or lumen invasion, which in turn
leads to incomplete or complete vascular occlusion. During the
process of development and occurrence of CHD, a large number of
inflammatory factors are involved, including changes in the levels
of TLR2, TLR4, hs-CRP, IL-6, nitric oxide, myeloperoxidase, TNF,
CD40 and complement factors. These may be considered as important
inflammatory markers, which trigger and aggravate the inflammatory
response and participate in the occurrence and development of CHD
(10,11).
TLRs are members of the natural immune response and
are widely distributed in the total genome (12) TLR2 and TLR4 are also involved in the
occurrence and development of coronary atherosclerosis. TLR2 and
TLR4 are mainly distributed on the cell surface and are able to
recognize lipids. After its isomerization, TLR2 it is able to
recognize the peptides, lipoprotein and mycoplasma of gram-positive
bacteria. During atherosclerosis and subsequent hardening of the
arteries, TLR4 leads to the activation of inflammatory signaling
pathways, which in turn initiate the start induction of
intracellular signal transduction. This causes the activation of
NF-κB (13), which translocates into
the nucleus, promoting activation of the mitogen-activated protein
kinase pathway. Upregulation of hs-CRP, TNF-α and IL-6 follows
(14), leading to the induction of
macrophage infiltration and activation. This aggravates the
inflammatory response, promoting inflammatory activation of
atherosclerotic plaque, which may result in plaque rupture.
TLR4 may also identify lipopolysaccharides (LPS),
which occur in the outer membrane of Gram-negative bacteria, and
this promotes the development of atherosclerosis (15). Studies on TLR2 and TLR4 suggested
that these receptors are involved in signaling pathways mediating
inflammation that may lead to the occurrence and development of
coronary artery disease (16). It
was also indicated that in male patients with CHD, TLR4 mRNA levels
were positively correlated with the severity of coronary stenosis
(17). In addition, a study on CHD
patients of the Han ethnic group suggested differences in TLR2 and
TLR4 expression between genders and these differences were linked
to the levels of sex hormone (18).
A previous study indicated that the urinary albumin
creatinine ratio and cystatin C levels have a certain predictive
value for the degree of coronary artery stenosis (19). The aim of the present study was
mainly to investigate the correlation between the severity of
coronary artery stenosis and the expression levels of TLR2 and TLR4
in circulating blood in patients of the ethnic Zhuang group with
CHD. The results suggested that, compared with those in the healthy
control group, the levels of TLR2 and TLR4 were significantly
increased in patients with CHD, indicating that TLR2 and TLR4 may
be involved in the occurrence and development of coronary
atherosclerosis. Whether the patients were classified according to
the number of diseased vessels or to the coronary Gensini scores,
the severity of CHD was observed to correlate with these
parameters. The concentrations of TLR2 and TLR4 in circulating
blood appeared to have a certain predictive value for the degree of
coronary artery stenosis in patients with CHD. In patients with
>90% stenosis, an association between a high degree of stenosis
and reduced TLR4 responsiveness has been reported (20).
In addition, the present results indicated that the
concentrations of TLR2 and TLR4 were higher in patients with
two-vessel lesions, multi-vessel lesions, moderate stenosis and
severe stenosis, particularly in multi-vessel lesions and severe
stenosis. This means that higher concentrations of TLR2 and TLR4 in
circulating blood are associated with more severe coronary artery
stenosis, resulting in a larger number of diseased vessels.
Previous studies suggested that TLR4 mediated the release of TNF-α
and IL-6 and that the release of pro-inflammatory cytokines was
higher in patients with unstable angina or acute myocardial
infarction than in those with stable angina or healthy controls
(21–23). The expression of TLR4 on monocytes is
associated with TNF-α and IL-6 release after LPS stimulation, with
TLR4 participating in the occurrence and development of CHD via the
inflammatory response (22). In
addition, it was reported that the surface expression of TLR2 and
TLR4 on circulating monocytes increased markedly in acute
myocardial infarction and unstable patients with angina compared
with that in healthy control subjects (21,24).
However, these findings have yet to be fully explained and may be
linked to genetic factors.
In the present study, the expression levels of TLR2
and TLR4 in the circulating blood of CHD patients were
significantly higher than those in subjects without CHD. Higher
expression of TLR2 and TLR4 in the serum was associated with larger
and more numerous coronary artery lesions, resulting in a higher
severity of coronary artery stenosis. Thus, serum TLR2 and TLR4
levels in CHD patients may have predictive value regarding the
severity of coronary artery disease stenosis. In future studies, it
may be possible to measure the concentrations of TLR2 and TLR4 more
accurately and rapidly in order to increase their usefulness as
predictive markers.
Several subtypes of CHD (including myocardial
infarction, stable angina pectoris and unstable angina pectoris)
were included in the present study, but the numbers of patients in
these groups were relatively small and analysis of their serum TLR2
and TLR4 levels would not have been meaningful. In addition, the
size of the control group in the present study was relatively
small. In future studies, patients from several hospitals may be
recruited in order to overcome the limitations of the present
study.
Acknowledgements
Not applicable.
Funding
This study was supported by a grant from the Baise
Science and Technology Cooperation Project Foundation of Guangxi
Province, China (grant no. 20150819).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZH, WL, LLiang, YL and JM were involved in
acquisition, analysis or interpretation of the data. ZH, YL, JM,
KL, SRS, LLiu and ZL contributed to the design and the conception
of the study and interpretation of the data. ZH, YL, WL and JG
conceived of the study and participated in its design and
coordination. ZH, YL and JG drafted the manuscript. All authors
were involved in drafting/revising and approving the
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the Affiliated Hospital of Youjiang Medical University for
Nationalities (Baise, China), in accordance with the Declaration of
Helsinki. All participants provided written informed consent to
participate in this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang Z, Wang X, Chen Z, Zhang L and Zhu M:
Distribution of high-sensitivity C-reactive protein and its
relationship with other cardiovascular risk factors in the
middle-aged chinese population. Int J Environ Res Public Health.
13(pii): E8722016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sepehri ZS, Masoomi M, Ruzbehi F, Kiani Z,
Nasiri AA, Kohan F, Sheikh Fathollahi M, Kazemi Arababadi M,
Kennedy D and Asadikaram GA: Comparison of serum levels of IL-6,
IL-8, TGF-β and TNF-α in coronary artery diseases, stable angina
and participants with normal coronary artery. Cell Mol Biol
(Noisy-le-grand). 64:1–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kuwahata S, Fujita S, Orihara K, Hamasaki
S, Oba R, Hirai H, Nagata K, Ishida S, Kataoka T, Oketani N, et al:
High expression level of Toll-like receptor 2 on monocytes is an
important risk factor for arteriosclerotic disease.
Atherosclerosis. 209:248–254. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Okun E, Griffioen KJ, Rothman S, Wan R,
Cong WN, De Cabo R, Martin-Montalvo A, Levette A, Maudsley S,
Martin B, et al: Toll-like receptors 2 and 4 modulate autonomic
control of heart rate and energy metabolism. Brain Behav Immun.
36:90–100. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ruixing Y, Fengping H, Shangling P, Dezhai
Y, Weixiong L, Tangwei L, Yuming C, Jinzhen W, Limei Y and Jiandong
H: Prevalence of hyperlipidemia and its risk factors for the
middle-aged and elderly in the Guangxi Hei Yi Zhuang and Han
populations. J Investig Med. 54:191–200. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ruixing Y, Guangqin C, Yong W, Weixiong L,
Dezhai Y and Shangling P: Effect of the 3′APOB-VNTR polymorphism on
the lipid profiles in the Guangxi HeiYi Zhuang and Han populations.
BMC Med Genet. 8:452007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li J, Guo C, Yan M, Niu F, Chen P, Li B
and Jin T: Genetic polymorphisms in very important pharmacogenomic
variants in the Zhuang ethnic group of Southwestern China: A cohort
study in the Zhuang population. Medicine (Baltimore). 97:e05592018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Judkins MP: Percutaneous transfemoral
selective coronary arteriography. Radiol Clin North Am. 6:467–492.
1968.(In Portuguese). PubMed/NCBI
|
|
9
|
Gensini GG: A more meaningful scoring
system for determining the severity of coronary heart disease. Am J
Cardiol. 51:6061983. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Harrington RA: Targeting inflammation in
coronary artery disease. N Engl J Med. 377:1197–1198. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li H, Sun K, Zhao R, Hu J, Hao Z, Wang F,
Lu Y, Liu F and Zhang Y: Inflammatory biomarkers of coronary heart
disease. Front Biosci (Landmark Ed). 22:504–515. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McCoy KL: Interaction between cannabinoid
system and toll-like receptors controls inflammation. Mediators
Inflamm. 2016:58313152016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sugiyama K, Muroi M, Kinoshita M, Hamada
O, Minai Y, Sugita-Konishi Y, Kamata Y and Tanamoto K: NF-κB
activation via MyD88-dependent Toll-like receptor signaling is
inhibited by trichothecene mycotoxin deoxynivalenol. J Toxicol Sci.
41:273–279. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jia SJ, Niu PP, Cong JZ, Zhang BK and Zhao
M: TLR4 signaling: A potential therapeutic target in ischemic
coronary artery disease. Int Immunopharmacol. 23:54–59. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang Y, El-Far M, Dupuy FP, Abdel-Hakeem
MS, He Z, Procopio FA, Shi Y, Haddad EK, Ancuta P, Sekaly RP and
Said EA: HCV RNA activates APCs via TLR7/TLR8 while virus
selectively stimulates macrophages without inducing antiviral
responses. Sci Rep. 6:294472016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yu L and Feng Z: The role of toll-like
receptor signaling in the progression of heart failure. Mediators
Inflamm. 2018:98741092018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Guven M, Ismailoglu Z, Batar B, Unal S,
Onaran I, Karadag B and Ongen Z: The effect of genetic
polymorphisms of TLR2 and TLR4 in Turkish patients with coronary
artery disease. Gene. 558:99–102. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lashkari BS, Shahana S and Anumba DO:
Toll-like receptor 2 and 4 expression in the pregnant and
non-pregnant human uterine cervix. J Reprod Immunol. 107:43–51.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
de Boer RA, Nayor M, deFilippi CR, Enserro
D, Bhambhani V, Kizer JR, Blaha MJ, Brouwers FP, Cushman M, Lima
JAC, et al: Association of cardiovascular biomarkers with incident
heart failure with preserved and reduced ejection fraction. JAMA
Cardiol. 3:215–224. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Versteeg D, Hoefer IE, Schoneveld AH, de
Kleijn DP, Busser E, Strijder C, Emons M, Stella PR, Doevendans PA
and Pasterkamp G: Monocyte toll-like receptor 2 and 4 responses and
expression following percutaneous coronary intervention:
Association with lesion stenosis and fractional flow reserve.
Heart. 94:770–776. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Methe H, Kim JO, Kofler S, Weis M, Nabauer
M and Koglin J: Expansion of circulating Toll-like receptor
4-positive monocytes in patients with acute coronary syndrome.
Circulation. 111:2654–2661. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Satoh M, Shimoda Y, Maesawa C, Akatsu T,
Ishikawa Y, Minami Y, Hiramori K and Nakamura M: Activated
toll-like receptor 4 in monocytes is associated with heart failure
after acute myocardial infarction. Int J Cardiol. 109:226–234.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liuzzo G, Angiolillo DJ, Buffon A,
Rizzello V, Colizzi C, Ginnetti F, Biasucci LM and Maseri A:
Enhanced response of blood monocytes to in vitro
lipopolysaccharide-challenge in patients with recurrent unstable
angina. Circulation. 103:2236–2241. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ashida K, Miyazaki K, Takayama E,
Tsujimoto H, Ayaori M, Yakushiji T, Iwamoto N, Yonemura A, Isoda K,
Mochizuki H, et al: Characterization of the expression of TLR2
(toll-like receptor 2) and TLR4 on circulating monocytes in
coronary artery disease. J Atheroscler Thromb. 12:53–60. 2005.
View Article : Google Scholar : PubMed/NCBI
|