Introduction
The third International Consensus defines sepsis as
a life-threatening organ dysfunction caused by a dysregulated host
response to infection (1).
Sepsis-induced injury and dysfunction of multiple organs remain the
major cause of death in septic patients. One of the main organ
complications of sepsis is the acute lung injury (ALI), which is
characterized by alveolar edema, acute hypoxemic respiratory
failure and enhanced inflammatory response in the lungs (2).
Although sepsis is a systemic inflammation response
syndrome, overwhelming evidence implicates the underlying role of
oxidative stress in the pathogenesis of multiple organ failure in
septic patients (3). Oxidative
stress influences the molecular mechanisms that control
inflammation and directly cause tissue damage (4,5). The
lung is the primary organ that is affected initially and most
severely in sepsis (6). Under normal
physiological conditions, there is a balance between the levels of
antioxidants and oxidants in the lungs, and a disruption in this
balance is considered to be one of the primary events that causes
an inflammatory response in the lungs during septic infection
(6,7). Furthermore, oxidative stress further
activates cytokines and leukocytes, potentially leading to the
overexpression of nitric oxide (NO), an excess of which reacts with
O2− to produce ONOO−, which
mediates nitrative stress in sepsis (8). A clinical study detected a large
qaunitity of nitric oxide derived from inducible NO synthase (iNOS)
in septic patients, which indicated that nitrative stress is
involved in septic-mediated injury (9).
Dexmedetomidine (Dex), a selective agonist of the
α2-adrenergic receptor, is an effective sedative, anxiolytic and
analgesic agent for critically ill patients. Dex has been reported
to exert beneficial effects on respiration during sedation
(10). Recent studies on septic
animal models revealed that Dex attenuates lung injury (11). However, these studies primarily
focused on the effects of Dex on the inflammatory response. To the
best of our knowledge, the effects of Dex on oxidative stress and
nitrative stress in lung injury have not been reported. Other
studies demonstrated that Dex exerted antioxidant effects (12,13).
Thus, it was hypothesized that Dex may exert antioxidant and
anti-nitrative effects during septic-induced lung injury.
Heme oxygenase-1 (HO-1) is a stress-inducible enzyme
that can catalyze the conversion of heme to ferrous iron, carbon
monoxide and biliverdin. HO-1 is among the most critical protective
mechanisms activated during cellular stress and it is thought to
serve a key role in maintaining anti-oxidant/oxidant balance. A
previous study revealed that the stimulation of HO-1 was able to
exert protective effects against cellular oxidative stress
(14). Conversely, HO-1 deficient
mice presented with major pro-oxidant and pro-inflammatory
pathologies (15), and suffered
higher mortality rates compared with wild-type mice (16). Furthermore, lung protection by HO-1
was demonstrated in vitro and in vivo in several
models of experimental ALI and sepsis (17,18).
The present study was based on the hypothesis that
Dex attenuates lung injury and oxidative and nitrative stress in
septic mice by activating HO-1.
Materials and methods
Cecal ligation and puncture (CLP) to
induce sepsis in mice
A total of 56 male wild-type mice (20–25 g) were
obtained from the Experimental Centre of Wuhan University (Wuhan,
China). The mice were housed in the conditions of 18–22°C room
temperature and 50–60% humidity and given free access to standard
laboratory diet and drinking water on a 12-h light/dark cycle.
A CLP model was used for the induction of
polymicrobial sepsis in mice. As described in a previous study
(19), the mice were anesthetized by
administering intraperitoneal ketamine hydrochloride (120 mg/kg)
and xylazine hydrochloride (5 mg/kg). The abdominal area was shaved
and disinfected. A laparotomy was performed and the cecum was
ligated from the top and punctured twice by piercing the cecum with
an 18-gauge needle. A small amount of feces from the bowel was
expelled from the puncture hole and the cecum was returned into the
peritoneal cavity gently. Sham-operated mice underwent the same
procedure but with no ligation and perforation of the cecum.
Pre-warmed saline (0.5 ml/100 g body weight) was injected
subcutaneously following surgery. Postoperative pain control was
managed with one subcutaneous injection of bupivacaine (3 mg/kg).
All experimental procedures utilizing animals were approved by the
Experimental Animal Centre Review Board of Renmin Hospital of Wuhan
University (no. WDRM 2018).
Experimental protocol
Mice were randomly divided into four groups: Sham
group, CLP group, Dex group (CLP + Dex) and Dex + zinc
protoporphyrin (CLP + Dex + ZnPP). Following CLP or sham surgery,
intraperitoneal injections of 40 µg/kg Dex or saline were
immediately administered once. Znpp IX (40 mg/kg) was injected via
intraperitoneal administered 1 h before the CLP operation (20). Znpp IX (Sigma-Aldrich; Merck KGaA)
was dissolved in 0.2 M sodium hydroxide and adjusted to a pH of 7.4
(21).
Mortality rate
Mice (n=40) were randomly divided into four groups
(10 mice per group). The animals were CLP- or sham-operated and
administered Dex (40 µg/kg) (Jiangsu Hengrui Medicine Co., Ltd.) or
ZnPP IX (40 mg/kg) as stated above. Postoperative pain control was
managed with subcutaneous injection of bupivacaine (3 mg/kg,
Shandong Hualu Pharmaceutical Co., Ltd.) immediately post-operation
once per day. All animals were monitored after the operation and
administrations. The time when an animal died from septic infection
was recorded as 1 and the time when no death occurred was recorded
as 0. SPSS-15.0 software was used to analyze the mortality rate
within 96 h. Following 96-h, all experimental animals were
euthanized using 100% CO2 anesthesia using an air
displacement rate of 20% of the chamber volume/min. Preemptive
euthanasia was performed for humane reasons if mice showed any of
the following signs: Emaciated, gasping, no response to touch or
the anal temperature <25°C.
Histopathological assessment of
pulmonary tissue
Following 24 h post-CLP surgery, animals were
anesthetized by administering intraperitoneal ketamine
hydrochloride (120 mg/kg) and xylazine hydrochloride (5 mg/kg). The
lung tissues were perfused under controlled pressure with PBS at
room temperature. The right lung was fixed in 4% paraformaldehyde
at room temperature for 30 min and then embedded in paraffin, cut
into 4 µm sections and stained with hematoxylin and eosin
respectively for 5 min at room temperature. The slides were scored
under a light microscope (magnification, ×200) by two blinded
pathologists with expertise in lung pathology. The criteria for
scoring lung injury was as follows (22): 0–5, normal to minimal inflammation;
6–10, mild inflammatory change; 11–15, moderate inflammatory;
16–20, severe inflammatory injury.
Measurement of tissue myeloperoxidase
(MPO) activity
MPO is a marker of neutrophil accumulation and
activation. MPO activity in lung tissue was measured by using a MPO
detection assay kit according to the manufacturer's protocol
(Nanjing Jiancheng Bioengineering Institute). Following
homogenization and sonication (25 kHz; 4×30 sec) of lung tissue at
0°C, 100 µl of supernatant was added to 2.9 ml of o-Dianisidine
dihydrochloride and hydrogen peroxide solution for 5 min at room
temperature and then stopped by adding 0.1 ml of hydrochloric acid.
Absorbance was measured spectophotometrically at 400 nm and MPO
activity was expressed as U/mg tissue.
Measurement of superoxide dismutase
(SOD) activity, malondialdehyde (MDA) levels and total NO
production in lung tissue
Following 24 h post-operation, SOD activity in the
lung was measured using a SOD activity assay kit (Nanjing Jiancheng
Bioengineering Institute Co., Ltd.; cat. no. A001-3-2) as
previously described (14). SOD
activity was expressed as U/mg protein.
MDA serves as an index of membrane lipid
peroxidation. MDA levels in the tissue was determined using a MDA
assay kit (Nanjing Jiancheng Bioengineering Institute Co., Ltd.;
cat. no. A003-1-2) as previously described (14). The level of MDA was expressed as U/mg
protein. The content of lung NO was detected with a commercially
available NO assay kit (Nanjing Jiancheng Bioengineering Institute
Co., Ltd.; cat. no. A012-1-2) according to manufacturer's
protocol.
Quantitation of tissue nitrotyrosine
content
Lung tissues were homogenized in cold saline. The
nitrotyrosine content of lung tissues, a footprint of in
vivo ONOO− formation and an index of nitrative
stress, was evaluated using a nitrotyrosine ELISA kit (cat. no.
ab113848; Abcam) according to the manufacturer's protocol.
Measurement of serum cytokines
Following 24 h post-CLP surgery, 200 µl blood was
harvested from the heart for the serum interleukin (IL)-6 and tumor
necrosis factor (TNF)-α assays. Serum IL-6 and TNF-α were detected
using commercial ELISA kits (cat. nos. DY 506 and DY410-05; R&D
Systems, Inc.) according to manufacturer's protocol.
HO-1 activity
HO-1 activity was measured 24 h post-CLP surgery by
quantitatively determining biliverdin reductase using a commercial
assay kit (Genmed Scientifics, Inc.) as previously described
(14). HO-1 activity was expressed
as ng/mg protein.
Western blot analysis
Protein extraction and western blot analysis was
performed as described previously (14). Protein was extracted by
radioimmunoprecipitation assay lysis buffer (cat. no. C500005;
Sangon Biotech Co., Ltd.) then quantified by bicinchoninic acid
method. A total of 50 µg of protein was loaded per lane and
separated by 4–12% SDS-PAGE and then transferred to a PVDF
membrane. The membrane was blocked by 5% non-fat milk for 1 h at
room temperature and subsequently incubated with primary antibodies
for iNOS (1:1,000; Abcam, cat. nos. ab3523) and GAPDH (1:1,000;
Santa Cruz Biotechnology Inc.; cat. nos. sc-32233) overnight at
4°C. Immunoreactivity was detected by a secondary horseradish
peroxidase-conjugated IgG (1:5,000; Thermo Fisher Scientific, Inc.;
cat. no. A32731) for 1 h at room temperature. Proteins were
developed via enhanced ECL chemiluminescence reagent kit (cat. no.
32109; Thermo Fisher Scientific, Inc.) and visualized using Bio-rad
Imaging systems (Bio-Rad Laboratories, Inc.) and quantified with
Quantity One image software (v4.62, Bio-Rad Laboratories).
Statistical analysis
Data were expressed as the mean ± standard error.
Each experiment was repeated for three times. SPSS-15.0 software
(SPSS, Inc.) was used for data analysis. Statistical significance
was estimated via one-way analysis of variance followed by the
Student-Newman-Keul post hoc test. The mortality rates among groups
were compared using the Kaplan Meier method, followed by a post hoc
test (Bonferroni's method). P<0.05 was considered to indicate a
statistically significant difference.
Results
General characteristics of septic
mice
As presented in Table
I, at 24 h following surgery, CLP mice exhibited severe
hypotension with a 58% decrease in mean blood pressure and
hypothermia, which indicated that the CLP model was successfully
established.
 | Table I.General characteristics of septic
mice. |
Table I.
General characteristics of septic
mice.
| A, Sham group |
|---|
|
|---|
| Characteristics | Baseline | 24 h |
|---|
| Weight (g) | 23.2±2.1 | 20.3±1.8 |
| Mean blood pressure
(mmHg) | 82.0±1.0 | 83.0±6.0 |
| Temperature
(°C) | 37.0±0.5 | 37.1±0.2 |
|
| B, CLP
group |
|
|
Characteristics |
Baseline | 24 h |
|
| Weight (g) | 23.6±0.7 | 21.1±0.8 |
| Mean blood pressure
(mmHg) | 84.0±2.0 |
35.0±6.0a |
| Temperature
(°C) | 37.1±0.1 |
30.1±0.2a |
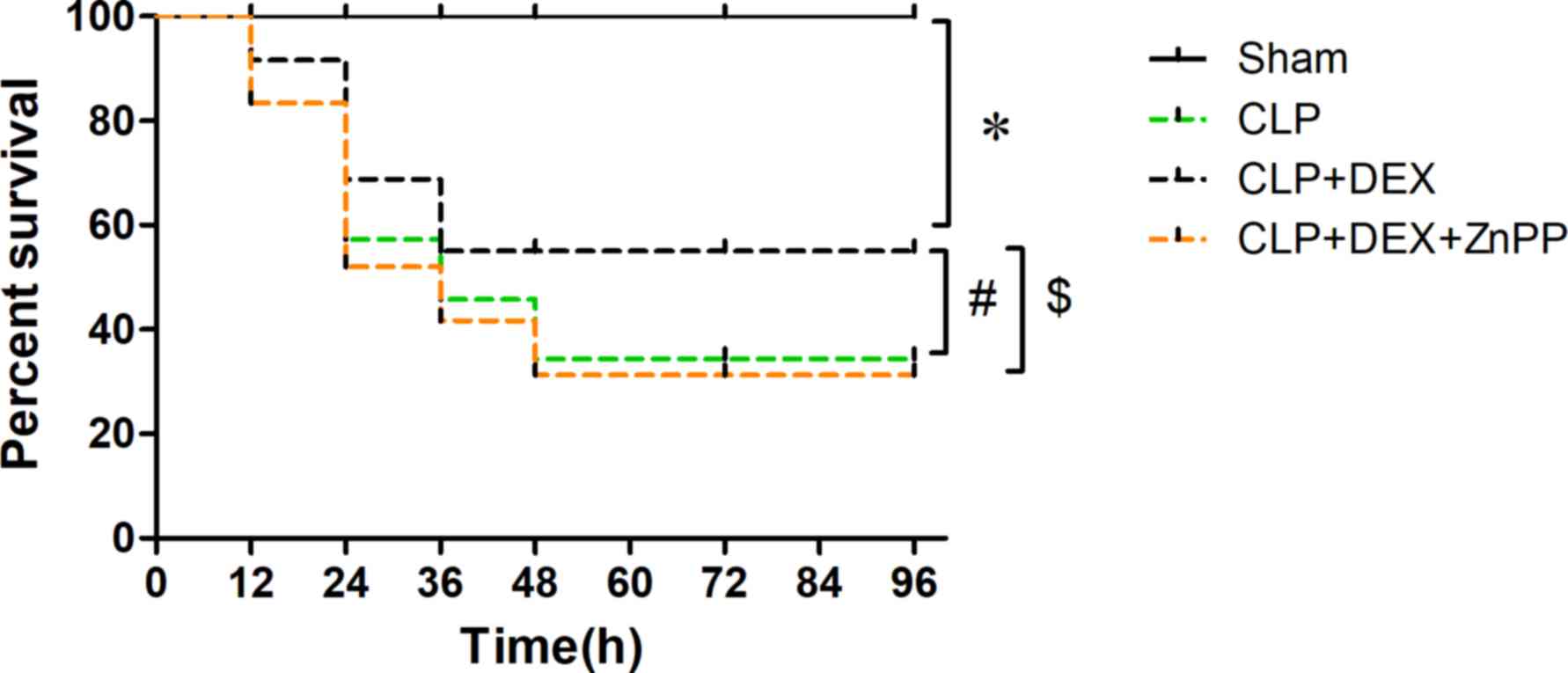
Pretreatment with Dex improves
survival in experimental sepsis
As presented in Fig.
1, the survival rates of mice at 96 h following surgery were
100, 34.4, 55 and 31.3% for the sham, CLP, CLP + Dex and CLP + Dex
+ ZnPP groups, respectively. Compared with the sham group, the
mortality rate in the CLP group significantly increased. Dex
pretreatment markedly decreased the elevated mortality rate induced
by CLP. However, ZnPP reverted the effects of Dex (Fig. 1).
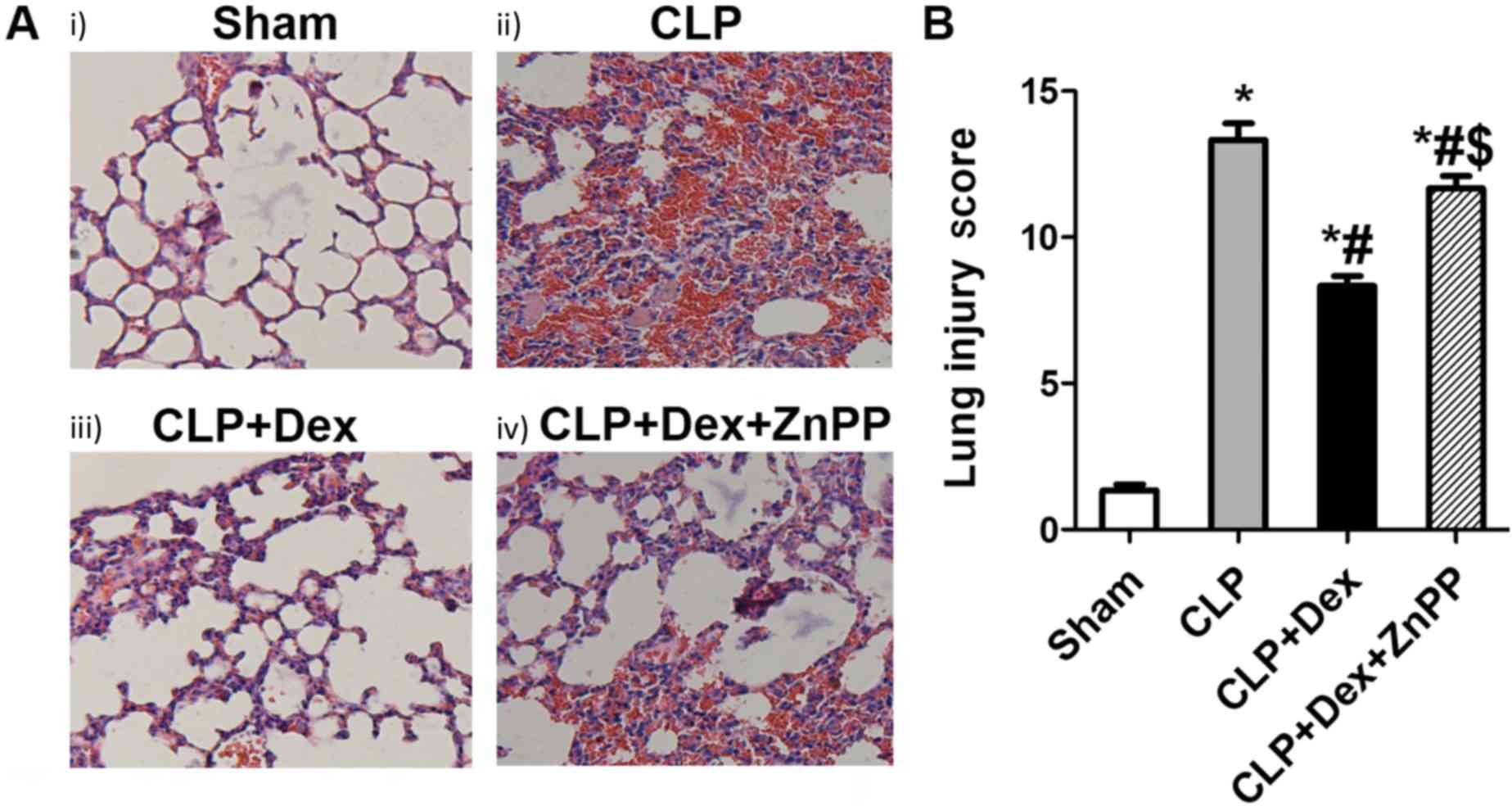
Dex treatment attenuates lung
histological injury in sepsis
Representative lung morphological changes are
presented in Fig. 2A. Lung tissue
sections in sham group showed normal alveolar architecture. In
contrast, septic mice exhibited severe lung damage in the CLP
group, evidenced by abundant inflammatory cells infiltration,
alveolar wall edema and congestion. However, compared with the CLP
group, only mild damage in lung tissue sections was observed in the
CLP + Dex group, while ZnPP partly revert the effects of Dex. The
inflammation scores of lung injury are presented in Fig. 2B. The lung injury score of the CLP +
Dex group was significantly lower than that in the CLP group.
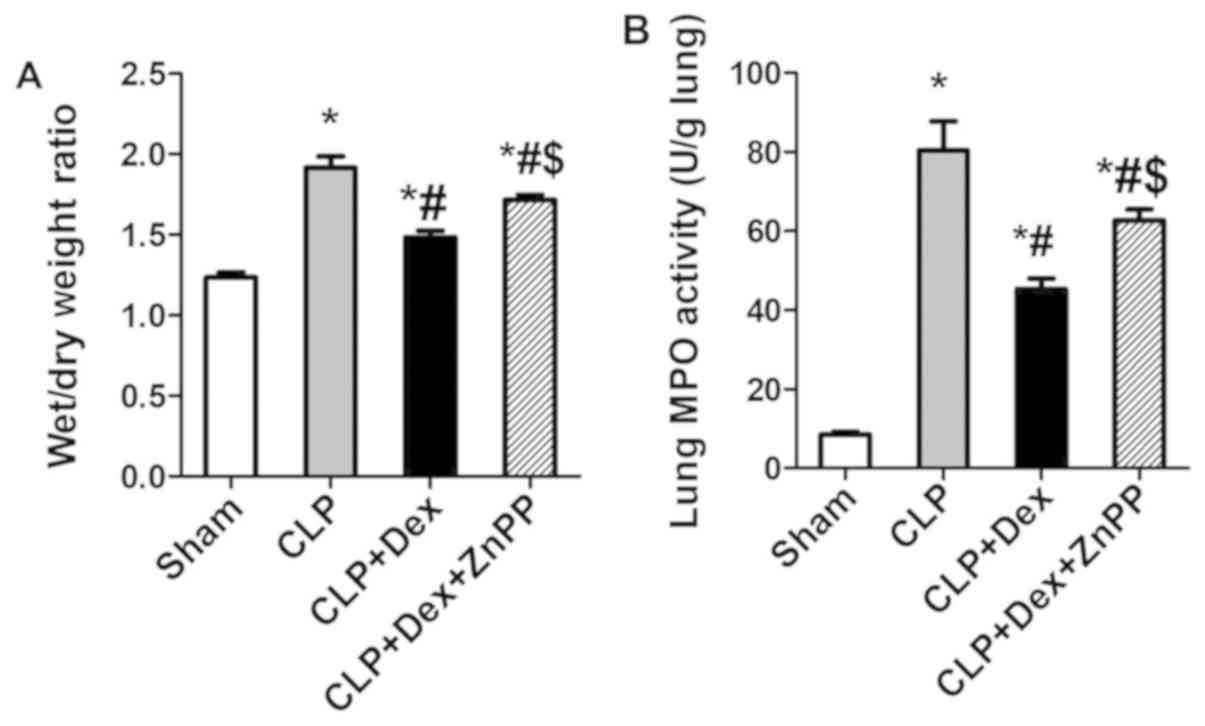
Wet/dry weight ratio and MPO
activity
The wet/dry weight ratio and MPO activity in the
lung tissues of the sham group was low. However, the wet/dry weight
ratio and MPO activity of CLP group was significantly higher than
those of the sham group (Fig. 3).
Pretreatment with Dex significantly inhibited the increase of
wet/dry weight ratio and MPO activity in septic mice. However, ZnPP
partially reverted the effects of Dex.
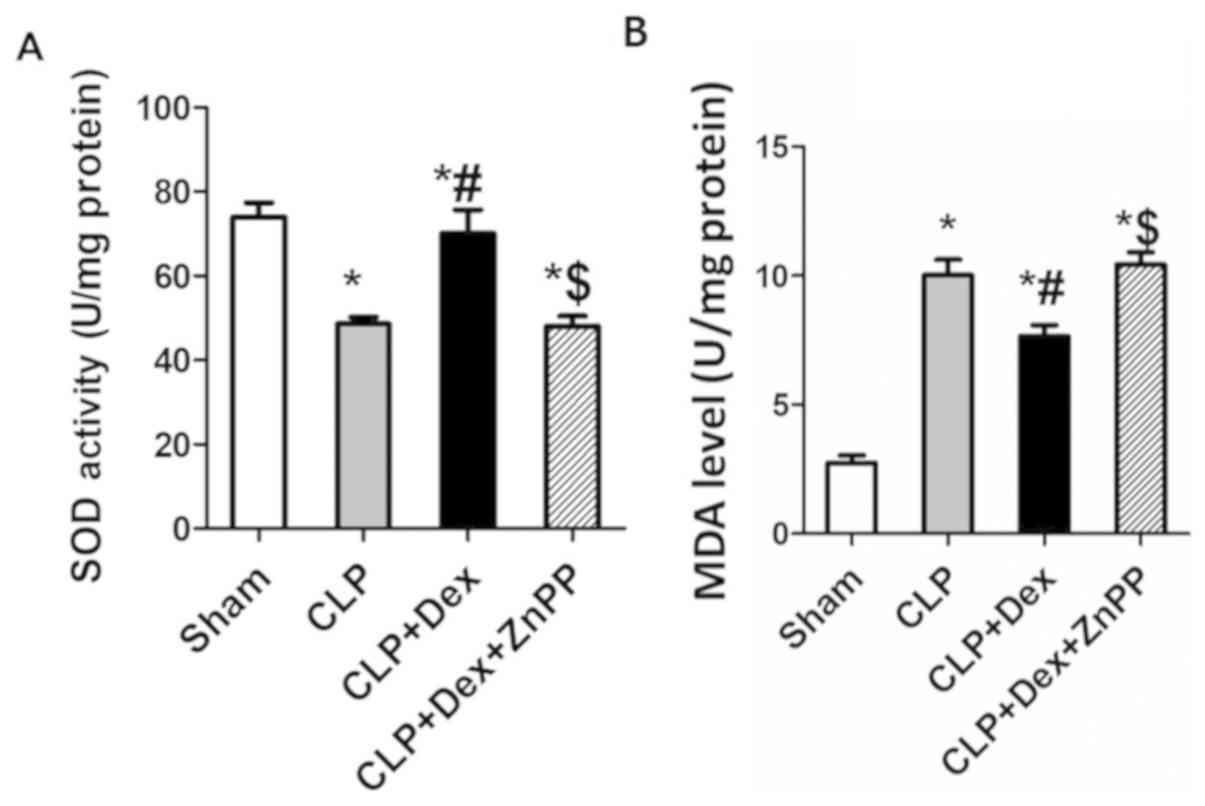
Dex reduces CLP-induced pulmonary
oxidative injury
A reduction in SOD activity was also observed in
septic mice at 24 h following CLP surgery compared with
sham-operated mice (Fig. 4A). MDA
content in murine pulmonary tissue was also significantly increased
in septic mice compared with sham-operated mice (Fig. 4B). Additionally, Dex treatment
significantly decreased pulmonary MDA content and increased
pulmonary SOD activity in septic mice. However, ZnPP reverted the
effects of Dex (Fig. 4).
Dex decreases serum levels of
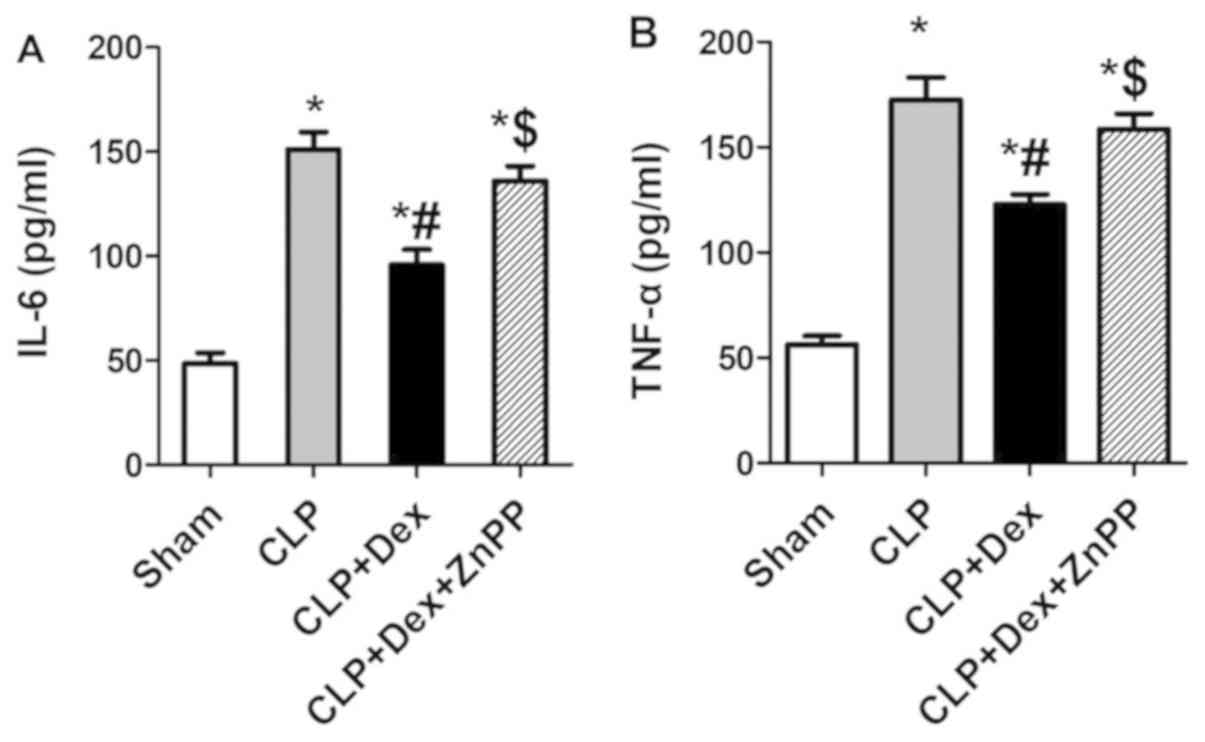
proinflammatory cytokines in septic mice
ELISA assays were performed to evaluate the serum
levels of IL-6 and TNF-α. Serum levels of TNF-α and IL-6 in septic
mice, induced by CLP surgery, were significantly increased compared
with those in the sham group. Dex markedly inhibited the
sepsis-induced upregulation of TNF-α and IL-6 production, whilst
ZnPP reversed the effects of Dex (Fig.
5).
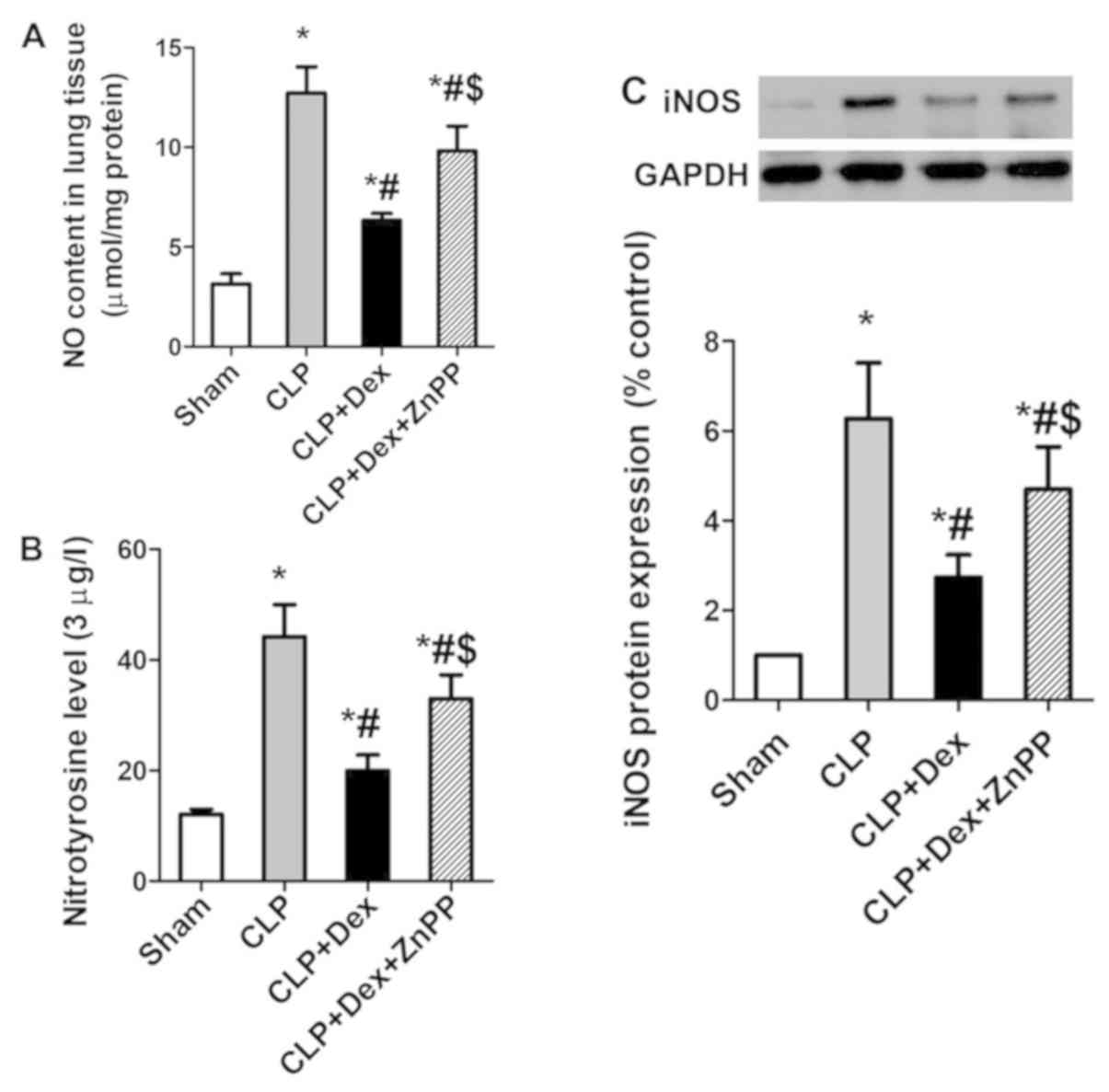
Dex decreases CLP-induced pulmonary
nitrative injury
Lung tissue nitrotyrosine content was significantly
increased in CLP mice compared with the sham-operated group
(Fig. 6B). This augmentation was
significantly decreased in Dex-treated mice when compared with the
CLP group (Fig. 6B). However, ZnPP
partially reversed the effects of Dex (Fig. 6B).
NO production was implicated during inflammation,
mainly due to the inducible NO synthase (iNOS). NO production and
iNOS expression were significantly increased in lung tissues of
septic mice (Fig. 6A and C).
Dex-treatment significantly decreased NO production and attenuated
the elevated iNOS expression in CLP mice (Fig. 6A and C).
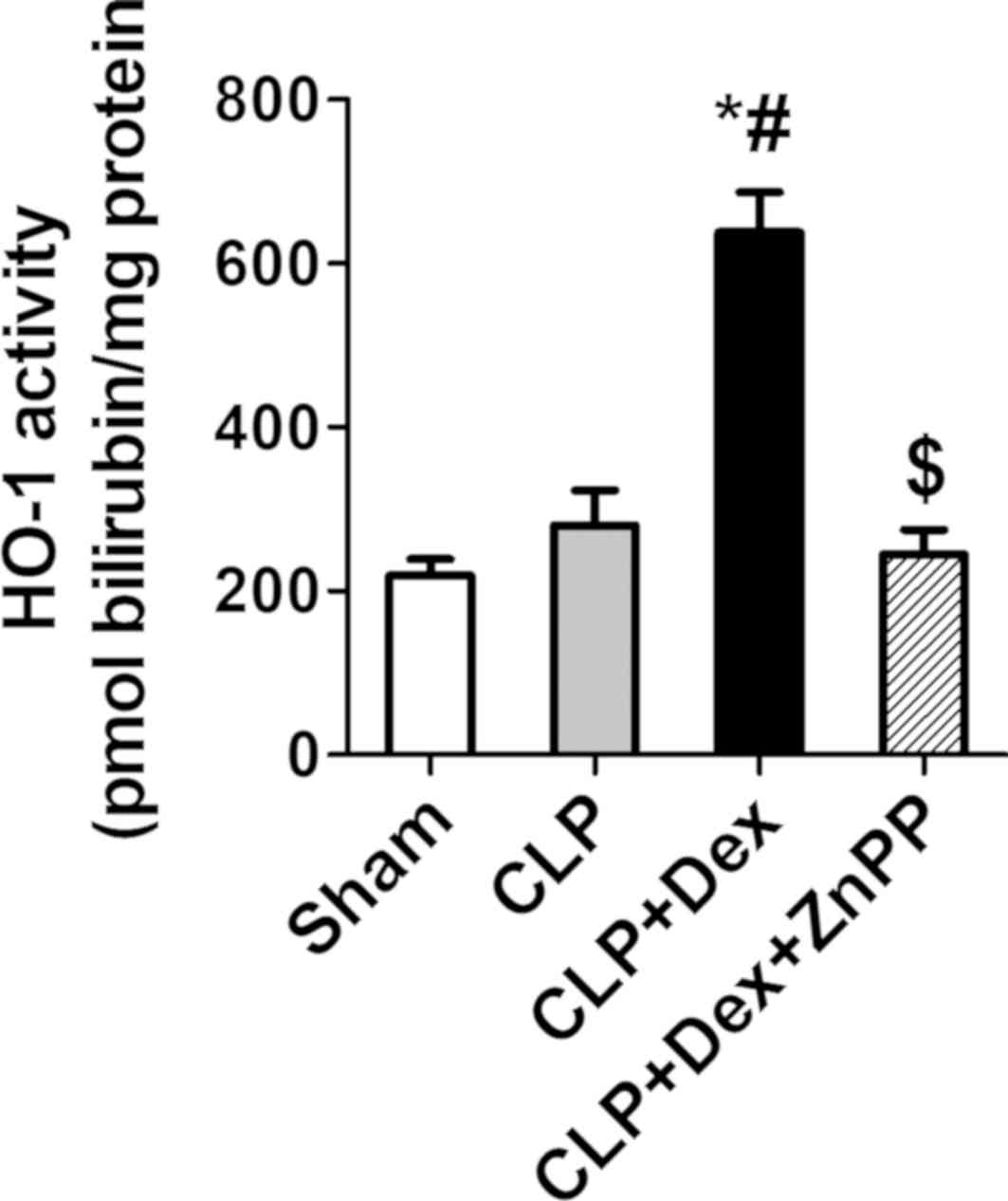
HO-1 activity in lung
HO-1 activity in the lung was low in the
sham-operated group. CLP slightly increased the lung HO-1 activity
and Dex significantly enhanced HO-1 activity following CLP
operation, while ZnPP reversed the effect of Dex (Fig. 7).
Discussion
The present study revealed that sepsis-induced lung
injury was associated with increased oxidative stress and nitrative
stress, as indicated by a significant increase in lung tissue
levels of MDA and nitrotyrosine content. Enhanced levels of
oxidative stress were accompanied by compromised plasma SOD
activity. Furthermore, Dex prevented septic-induced
oxidative/nitrative stress and increased HO-1 activity with
concomitant decreased lung levels of MDA, nitrotyrosine and NO
content as well as iNOS expression. However, HO-1 inhibitor ZnPP
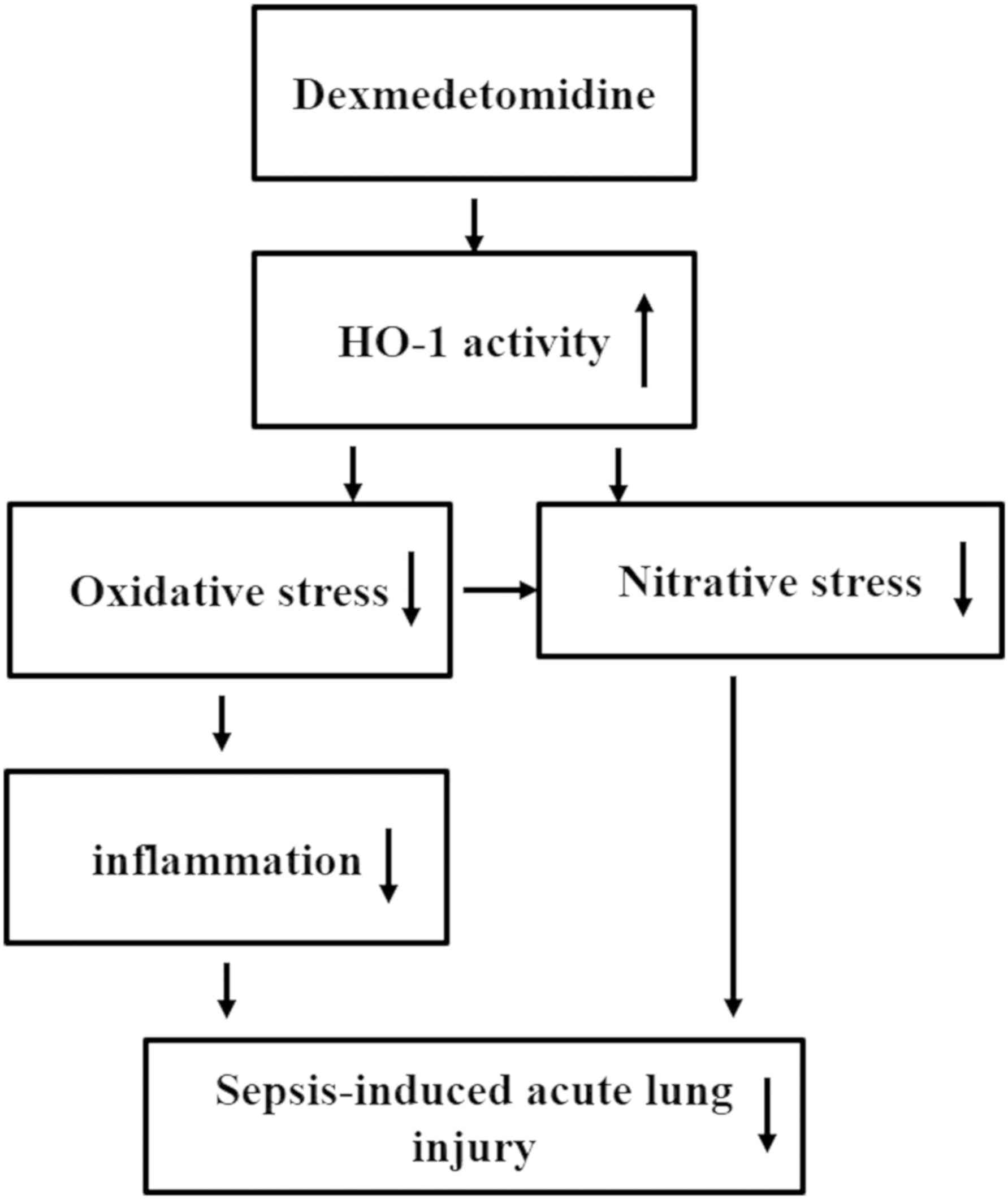
reversed the effects of Dex. The results support the hypothesis
that Dex exerts antioxidant and antinitrative effects on
septic-induced lung injury partially by increasing HO-1 activity. A
hypothetical diagram of this mechanism is presented in Fig. 8.
In sepsis, decreased endogenous antioxidant capacity
may lead to the excess production of reactive oxygen species (ROS)
(4,5), which have been assumed to serve an
important role in the induction of many pro-inflammatory cytokines
and mediators to trigger acute inflammatory responses in lung
tissue. The antioxidant, N-acetylcysteine, decreases
pro-inflammatory cytokine levels and ameliorates sepsis-associated
lung injury by suppressing intracellular ROS production (23). Consistent with other reports
(5,6)
the present study demonstrated that sepsis induced an
oxidant-anti-oxidant imbalance, evidenced by significantly
increased lung MDA levels and the decreased activity of the
antioxidant enzyme, SOD, in septic mice. An increased serum IL-6
and TNF-α expression and an enhanced lung MPO activity were also
observed, which indicated that a large number of inflammatory cells
were infiltrating lung tissues. Dex treatment decreased MDA levels,
inhibited the expression of IL-6 and TNF-α, and decreased
inflammatory cell infiltration, which implied that Dex exerted
protective effects on sepsis-induced lung injury by inhibiting
oxidative stress. However, the HO-1 ZnPP inhibitor partially
reverted the anti-oxidant effects of Dex. The protective effects of
Dex against sepsis-induced lung injury was associated with its
anti-oxidant property, by directly inhibiting superoxides, but also
by indirectly enhancing the activity of anti-oxidant enzyme
HO-1.
Sepsis induces lung vascular injury by increasing
nitrative stress, which is mediated by an increased NO production,
and the formation of strong oxidizing ROS, such as nitrotyrosine
(8,9). In the normal lung, NO is mainly
produced by endothelial NO synthase, while during inflammation, NO
is mainly induced by iNOS (24).
Zhang et al (25) reported
that resveratrol, which has anti-nitrative property, decreased
endotoxemia-induced acute lung injury by decreasing iNOS
expression, NO and nitrotyrosine production. In the present study,
the data revealed that septic lungs exhibited a marked increase in
nitrative stress, evidenced by the significantly increased NO
content and nitrotyrosine production, paralleled with an increased
protein expression of iNOS. Dex caused a decreased expression of
nitrotyrosine, indicating that Dex attenuates sepsis-induced
nitrative stress in lung tissue. However, these effects of Dex were
partially reverted by the HO-1 inhibitor ZnPP, suggesting that Dex
may exert its anti-nitrative effects by activating the HO-1
pathway.
Enhancing HO-1 activity, leading to the inhibition
of oxidative stress/nitrative stress, may be the underlying
mechanism whereby Dex attenuates sepsis-induced acute lung injury.
HO-1 is a rate-limiting enzyme involved in heme catabolism
possessing potent anti-oxidant effects. A number of studies
suggested that enhancing HO-1 expression in lung tissue alleviates
lung injury induced by sepsis (26–28). Gao
et al (29) reported that Dex
increased HO-1 expression in lung tissue and decreased oxidative
stress during one-lung ventilation. Consistent with this report,
the present study determined that Dex significantly increased HO-1
activity, accompanied with decreased MDA levels in the lung tissues
of septic mice. However, a previous report has indicated that
treatment with an adenoviral vector overexpressing HO-1 inhibits
the protein expression of iNOS in the cerebrum and blocks the toxic
formation of ONOO−during cerebral ischemia, implying
that HO-1 attenuates nitrative stress (8). In the present study, it was
demonstrated that Dex markedly activated HO-1 and decreased
superoxide anion production and nitrotyrosine content as well as
iNOS expression in the lung tissue of septic mice. The HO-1
activity inhibitor partially reverted the effects of Dex,
indicating that Dex inhibits sepsis-induced oxidative/nitrative
stress to attenuate sepsis-induced lung injury partly by activating
HO-1.
In conclusion, Dex was demonstrated to attenuate
sepsis-induced acute lung injury by attenuating oxidative/nitrative
stress, partially by increasing HO-1 activity. The present results
provide further basis for the use of dexmedetomidine to decrease
sepsis mortality.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Nature Science Foundation of China (grant no. 81301621) and the
National Nature Science Foundation of Hubei, China (grant no.
WJ2015MB193).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
GY made substantial contributions to conception and
design. SL contributed to acquisition of data, analysis and
interpretation of data. JX built the model and analyzed data, and
was a major contributor in writing the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
All experimental procedures utilizing animals were
approved by the Experimental Animal Centre Review Board of Renmin
Hospital of Wuhan University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Singer M, Deutschman CS, Seymour CW,
Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche
JD, Coopersmith CM, et al: The third international consensus
definitions for sepsis and septic shock (sepsis-3). JAMA.
315:801–810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choudhury S, Kandasamy K, Maruti BS,
Addison MP, Kasa JK, Darzi SA, Singh TU, Parida S, Dash JR, Singh V
and Mishra SK: Atorvastatin along with imipenem attenuates acute
lung injury in sepsis through decrease in inflammatory mediators
and bacterial load. Eur J Pharmacol. 765:447–456. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Boueiz A and Hassoun PM: Regulation of
endothelial barrier function by reactive oxygen and nitrogen
species. Microvasc Res. 77:26–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kvietys PR and Granger DN: Role of
reactive oxygen and nitrogen species in the vascular responses to
inflammation. Free Radic Biol Med. 52:556–592. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bedreag OH, Rogobete AF, Sarandan M,
Cradigati AC, Papurica M, Dumbuleu MC, Chira AM, Rosu OM and
Sandesc D: Oxidative stress in severe pulmonary trauma in critical
ill patients. Antioxidant therapy in patients with multiple
trauma-a review. Anaesthesiol Intensive Ther. 47:351–359. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lang JD, McArdle PJ, O'Reilly PJ and
Matalon S: Oxidant-antioxidant balance in acute lung injury. Chest
122 (6 Suppl). 314S–320S. 2002. View Article : Google Scholar
|
|
7
|
Zheng Y and Zhu D: Molecular hydrogen
therapy ameliorates organ damage induced by sepsis. Oxid Med Cell
Longev. 2016:58060572016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chao XD, Ma YH, Luo P, Cao L, Lau WB, Zhao
BC, Han F, Liu W, Ning WD, Su N, et al: Up-regulation of heme
oxygenase-1 attenuates brain damage after cerebral ischemia via
simultaneous inhibition of superoxide production and preservation
of NO bioavailability. Exp Neurol. 239:163–169. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang Z, Feng K, Yue M, Lu X, Zheng Q,
Zhang H, Zhai Y, Li P, Yu L, Cai M, et al: A non-synonymous SNP in
the NOS2 associated with septic shock in patients with sepsis in
Chinese populations. Hum Genet. 132:337–346. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Becker SE: A pilot study implementing a
protocol using dexmedetomidine as a safe alternative to traditional
sedation to decrease ventilator days for patients difficult to
extubate. Dimens Crit Care Nurs. 35:291–297. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu Z, Wang Y, Wang Y, Ning Q, Zhang Y,
Gong C, Zhao W, Jing G and Wang Q: Dexmedetomidine attenuates
inflammatory reaction in the lung tissues of septic mice by
activating cholinergic anti-inflammatory pathway. Int
Immunopharmacol. 35:210–216. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xia R, Xu J, Yin H, Wu H, Xia Z, Zhou D,
Xia ZY, Zhang L, Li H and Xiao X: Intravenous infusion of
dexmedetomidine combined isoflurane inhalation reduces oxidative
stress and potentiates hypoxia pulmonary vasoconstriction during
One-lung ventilation in patients. Mediators Inflamm.
2015:2380412015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ning Q, Liu Z, Wang X, Zhang R, Zhang J,
Yang M, Sun H, Han F, Zhao W and Zhang X: Neurodegenerative changes
and neuroapoptosis induced by systemic lipopolysaccharide
administration are reversed by dexmedetomidine treatment in mice.
Neurol Res. 39:357–366. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xu J, Li H, Irwin MG, Xia ZY, Mao X, Lei
S, Wong GT, Hung V, Cheung CW, Fang X, et al: Propofol ameliorates
hyperglycemia-induced cardiac hypertrophy and dysfunction via heme
oxygenase-1/signal transducer and activator of transcription 3
signaling pathway in rats. Crit Care Med. 42:e583–e594. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Immenschuh S, Vijayan V, Janciauskiene S
and Gueler F: Heme as a target for therapeutic interventions. Front
Pharmacol. 8:1462017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wiesel P, Patel AP, DiFonzo N, Marria PB,
Sim CU, Pellacani A, Maemura K, LeBlanc BW, Marino K, Doerschuk CM,
et al: Endotoxin-induced mortality is related to increased
oxidative stress and end-organ dysfunction, not refractory
hypotension, in heme oxygenase-1-deficient mice. Circulation.
102:3015–3022. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yu J, Shi J, Wang D, Dong S, Zhang Y, Wang
M, Gong L, Fu Q and Liu D: Heme Oxygenase-1/Carbon
Monoxide-regulated mitochondrial dynamic equilibrium contributes to
the attenuation of endotoxin-induced acute lung injury in rats and
in lipopolysaccharide-activated macrophages. Anesthesiology.
125:1190–1201. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee JW, Chun W, Kwon OK, Park HA, Lim Y,
Lee JH, Kim DY, Kim JH, Lee HK, Ryu HW, et al:
3,4,5-Trihydroxycinnamic acid attenuates lipopolysaccharide
(LPS)-induced acute lung injury via downregulating inflammatory
molecules and upregulating HO-1/AMPK activation. Int
Immunopharmacol. 64:123–130. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xu J, Feng Y, Jeyaram A, Jay SM, Zou L and
Chao W: Circulating plasma extracellular vesicles from septic mice
induce inflammation via MicroRNA- and TLR7-dependent mechanisms. J
Immunol. 201:3392–3400. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen H, Xie K, Han H, Li Y, Liu L, Yang T
and Yu Y: Molecular hydrogen protects mice against polymicrobial
sepsis by ameliorating endothelial dysfunction via an Nrf2/HO-1
signaling pathway. Int Immunopharmacol. 28:643–654. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xiong J, Wang K, Yuan C, Xing R, Ni J, Hu
G, Chen F and Wang X: Luteolin protects mice from severe acute
pancreatitis by exerting HO-1-mediated anti-inflammatory and
antioxidant effects. Int J Mol Med. 39:113–125. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu Y, Liu Y, Huang H, Zhu Y, Zhang Y, Lu F
and Zhou C, Huang L, Li X and Zhou C: Dexmedetomidine inhibits
inflammatory reaction in lung tissues of septic rats by
suppressingTLR4/NF-κB pathway. Mediators Inflamm. 2013:5621542013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Campos R, Shimizu MH, Volpini RA, de
Bragança AC, Andrade L, Lopes FD, Olivo C, Canale D and Seguro AC:
N-acetylcysteine prevents pulmonary edema and acute kidney injury
in rats with sepsis submitted to mechanical ventilation. Am J
Physiol Lung Cell Mol Physiol. 302:L640–L650. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
van der Vliet A and Cross CE: Oxidants,
nitrosants, and the lung. Am J Med. 109:398–421. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang HX, Duan GL, Wang CN, Zhang YQ, Zhu
XY and Liu YJ: Protective effect of resveratrol against
endotoxemia-induced lung injury involves the reduction of
oxidative/nitrative stress. Pulm Pharmacol Ther. 27:150–155. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cao TH, Jin SG, Fei DS, Kang K, Jiang L,
Lian ZY, Pan SH, Zhao MR and Zhao MY: Artesunate protects against
sepsis-induced lung injury via heme oxygenase-1 modulation.
Inflammation. 39:651–662. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yu Y, Yang Y, Yang M, Wang C, Xie K and Yu
Y: Hydrogen gas reduces HMGB1 release in lung tissues of septic
mice in an Nrf2/HO-1-dependent pathway. Int Immunopharmacol.
69:11–18. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen X, Wang Y, Xie X, Chen H, Zhu Q, Ge
Z, Wei H, Deng J, Xia Z and Lian Q: Heme oxygenase-1 reduces
sepsis-induced endoplasmic reticulum stress and acute lung injury.
Mediators Inflamm. 2018:94138762018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gao S, Wang Y, Zhao J and Su A: Effects of
dexmedetomidine pretreatment on heme oxygenase-1 expression and
oxidative stress during one-lung ventilation. Int J Clin Exp
Pathol. 8:3144–3149. 2015.PubMed/NCBI
|