Introduction
Lumbar spinal stenosis is one of the most common
causes of lumbar disease and frequently leads to back and waist
pain (1). As the elderly population
increases, the incidence of lumbar spinal stenosis is increasing
worldwide (2). Conventional open
surgery (COS) has previously been regarded as the gold standard for
the treatment of patients with lumbar spinal stenosis (3). Currently, various minimally invasive
spine surgery (MISS) techniques are being explored as alternative
methods for the treatment of lumbar spinal stenosis (4). MISS has been widely used for the
treatment of lumbar spinal stenosis as it is considered to be
superior to the COS approach (5,6). The
major advantages of MISS are the reduction of infection,
unnecessary exposure and tissue trauma (7). The current study compared clinical
outcomes in patients with lumbar spinal stenosis who received MISS
or COS during a 12-month period.
Postoperative pain is one of the most common
characteristics for patients with lumbar spinal stenosis following
surgery (8). Postoperative
inflammation is still regarded as a crucial criterion for
evaluating the efficacy of surgery for patients with lumbar spinal
stenosis (9). Retrospective,
demographic and clinical investigations have indicated the
bacterial causes of postoperative infection in lumbar spinal
stenosis patients following surgery (10). Reports have indicated that MISS leads
to a decrease in the incidence of infections compared with COS for
patients with lumbar spinal stenosis due to the smaller incision
and reduced vertebral muscle damage (11,12).
However, systemic investigations comparing the outcomes of MISS and
COS have not been performed for patients with lumbar spinal
stenosis.
In the current study, the efficacy of MISS surgery
was investigated for patients with lumbar spinal stenosis.
Significant differences between the MISS and COS groups were
identified for inflammation score, wound length, hospital stay,
Oswestry Disability Index (ODI) and visual analog scale (VAS) score
for back and leg pain in a 12-month period following surgery. The
current findings suggest that MISS management provides a better
therapeutic strategy for patients with lumbar spinal stenosis.
Materials and methods
Study design, subjects and
sampling
A total of 82 patients with L2/3 lumbar spinal
stenosis (mean age, 62 years; range, 49.2–68.4 years) were
recruited from the Department of Orthopedics at Affiliated National
Hospital of Guangxi Medical University (Nanning, China) in this
retrospective study. The study included 40 male and 42 female
patients. Institutional Review Board approval (Affiliated National
Hospital of Guangxi Medical University) was obtained for the
current study. The study protocol was performed from May 2013 to
June 2014 and was approved by the Central Ethics Committee (Ethics
Committee of Wuhan No. 1 Hospital, Wuhan, China; approval no.
WHHOP20130214). All patients were required to provide written
informed consent. The subsequent inclusion criteria included
pathological characteristics of lumbar spinal stenosis,
non-irritability for ampicillin, surgery history of lumbar
stenosis, leg and/or back pain. All patients underwent imaging
examination that exhibited lumbar lateral recess stenosis
consistent with the symptoms and signs of degenerative lumbar
scoliosis.
Drug administration
In total, 82 patients were administered with an
antibiotics regimen (ampicillin; Tianjin Tianshili Medicine Co.,
Ltd., Tianjin, China) in a 14-day continuation phase after surgery.
The indicated dosage of resveratrol and/or antibiotic regimen
(ampicillin) (both from Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) was 4.0 g/day daily.
Preoperative assessment
All patients received neurological and clinical
evaluation prior to surgery (13).
The back and leg pain in patients with lumbar spinal stenosis was
measured for the lower back and legs using a self-assessment
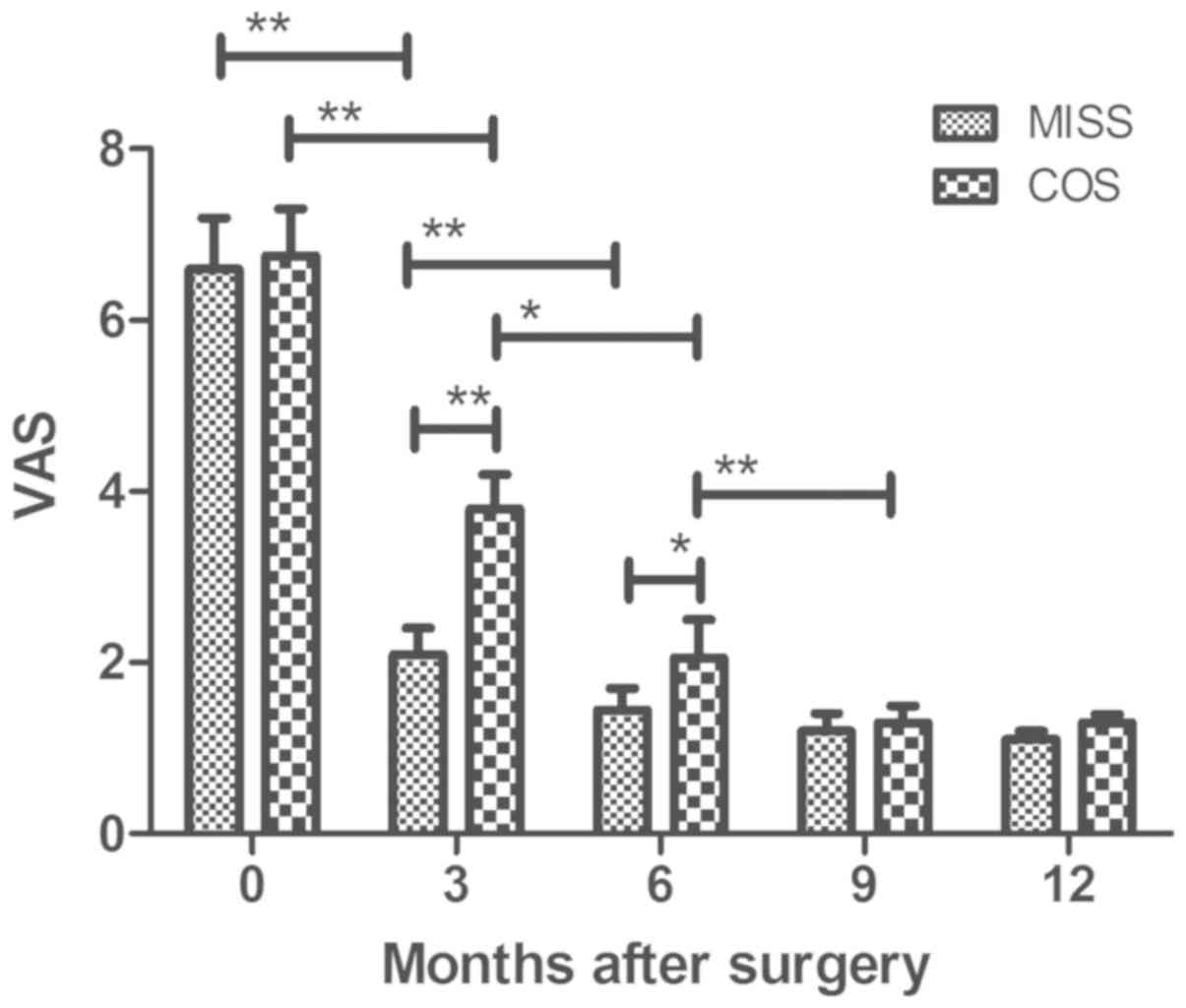
10-point VAS method (14). Intensity
of pain was measured using VAS scores from 0 to 10 (0 is no pain
and 10 is worst pain). VAS score was measured at 0, 3, 6, 9 and 12
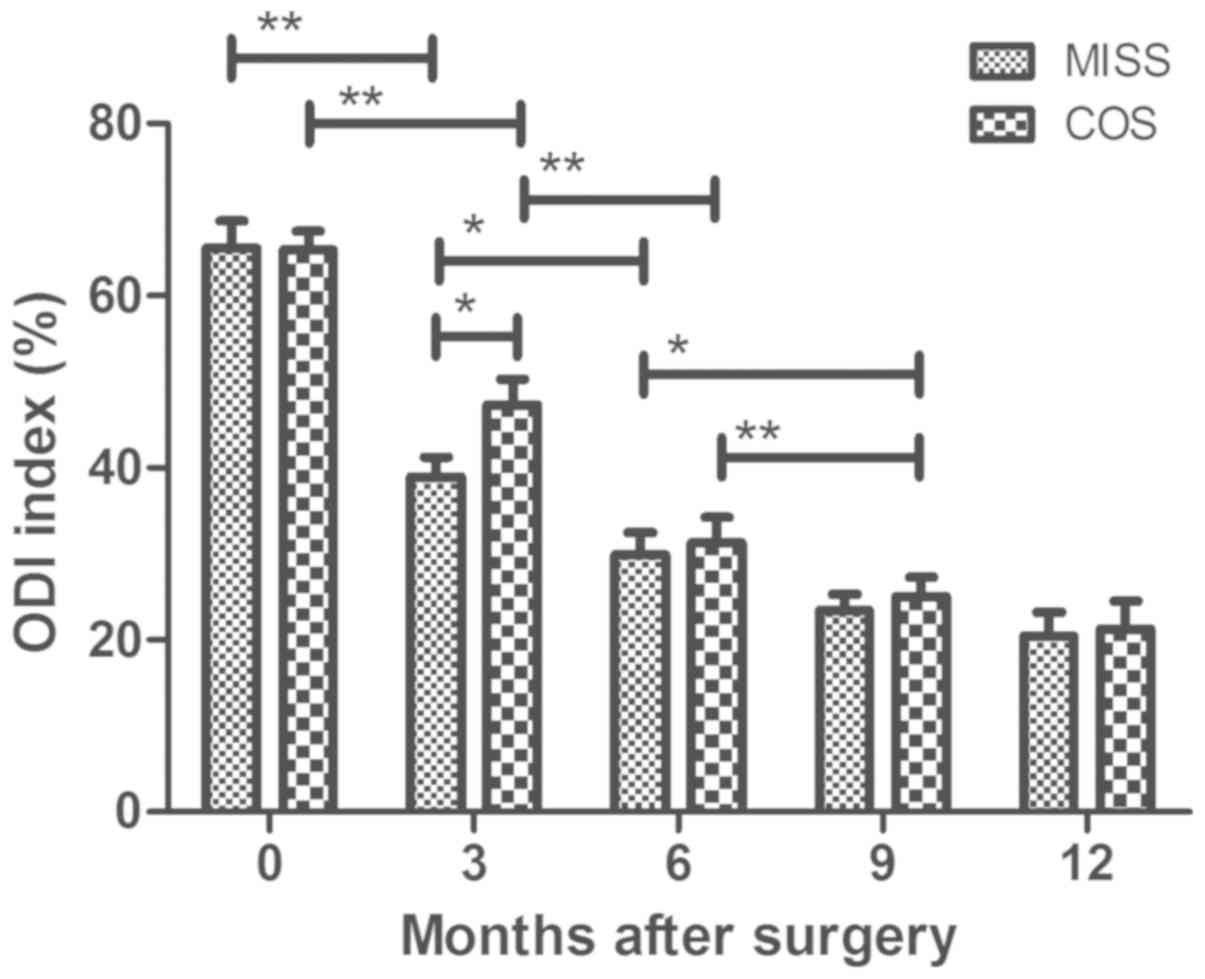
months following surgery. Disability was assessed using the ODI as
described previously (15).
Inflammation severity score
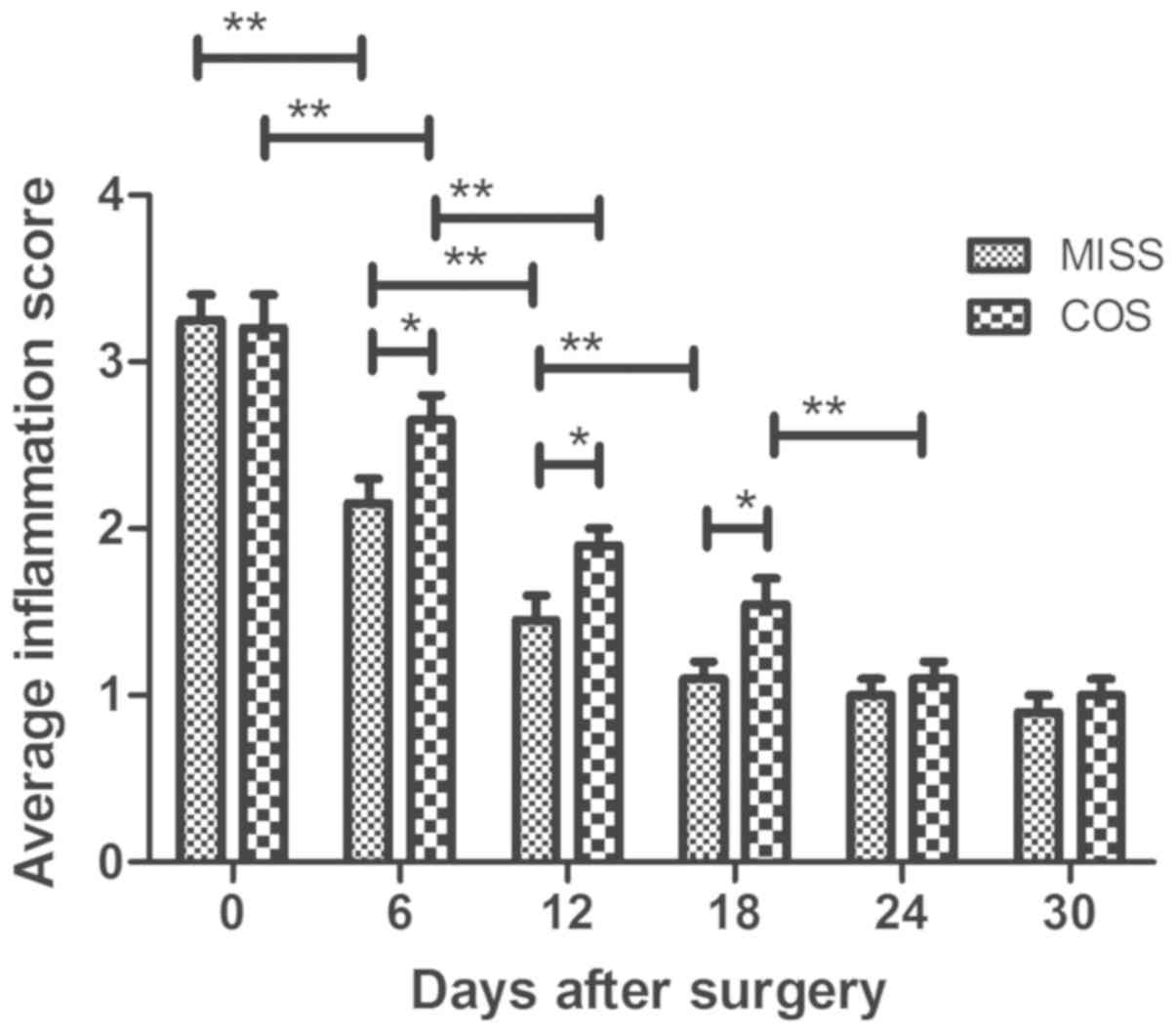
The primary efficacy criterion was the reduction in
inflammation severity score in patients with lumbar spinal stenosis
following MISS or COS. Inflammation severity score was assessed on
day 0, 6, 12, 18, 24 and 30 following MISS or COS. Mean
inflammation severity score was evaluated as described previously
(16).
Surgical procedures
All patients with lumbar spinal stenosis received
MISS (n=41) and COS (n=41; allocated at random) following
administration of general anesthesia in the prone position. The
MISS and COS surgery was performed in a consistent way and an
operative microscope was used in all cases (17).
In the MISS group, a C-arm X-ray machine (Biplanar
500e; Swemac Medical Appliances AB, Täby, Sweden), METRx Quadrant
System and percutaneous pedicle screw (both from Medtronic,
Minneapolis, MN, USA) were prepared. An incision was planned by
connecting a line between the outer portions of both end pedicles
(~3.0 cm off midline). Then, a skin incision of 3–4 cm was made on
the more symptomatic side or more severe pathology side according
to imaging. Decompression was conducted by cutting the inferior
portion of the lamina, hypertrophied superior and inferior
articular processes, and ligamenta flava. Then, the intervertebral
space was enlarged with a distractor followed by a PEEK cage
(Capstone; Medtronic). Then, percutaneous pedicle screw fixation
was conducted.
For the COS group, following routine disinfection
and draping, a G-arm machine was used to confirm the affected
segment. Then, a longitudinal incision was made in the middle of
the spine, and muscular fasciae were cut apart. Musculus
sacrospinalis were then bluntly dissected until the lumbar
transverse process was exposed. Pedicle screws were placed into the
upper and subjacent vertebral pedicle of the segmental lesions.
Spinous process, lamina, hyperplasia of yellow ligament and
interior zygapophysis were removed according to the scope of the
lesions, and lateral recess as well as nerve root canal was
enlarged with the protection of dural sac and nerve tissue. Then,
fibrous rings were cut and nucleus pulposus was removed, and the
intervertebral space was opened. The removed laminar and
zygapophysis were crushed into smaller pieces for incorporation as
autograft, then the cage with crushed bones was also inserted.
Next, titanium rods were used to connect the screws and fixed.
Finally, negative pressure drainage was placed and the incision was
sewn up.
Outcome assessment
ODI score and VAS score in lumbar spinal stenosis
patients was logged at 0, 3, 6, 9 and 12 months following MISS or
COS (18). Patient satisfaction
following MISS surgery was analyzed using the patient satisfaction
index (PSI, a modified sub-item of the North American Spine Society
outcome questionnaire) method, as reported previously (19).
Statistical analysis
Continuous variables are reported as the mean ±
standard deviation. All data were analyzed using SPSS Statistics
19.0 (IBM Corp., Armonk, NY, USA) and GraphPad Prism 5.0 (GraphPad
Software, Inc., La Jolla, CA, USA) with the help of Microsoft Excel
2010 (Microsoft Corporation, Redmond, WA, USA). Unpaired data were
compared by Student's t-test and comparisons between multiple
groups were performed using one-way analysis of variance (ANOVA)
followed by Tukey's post hoc test. VAS scores exhibited normal
distribution prior to surgery and were analyzed by the Wilcoxon
test prior to and following surgery. The t-test was used to analyze
ODI index and inflammation score prior to and following surgery.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Characteristics of lumbar spinal
stenosis patients
A total of 82 patients with lumbar spinal stenosis
were enrolled in the current study. It was demonstrated that the
mean body mass index was 26.4 and 25.2 kg/m2 in the MISS
and COS groups, respectively. There was no notable difference in
the incidence of leg and back pain between the MISS and COS groups.
The characteristics and symptoms of lumbar spinal stenosis patients
are summarized in Table I. It was
observed that there were no significant differences between
patients in the MISS and COS groups prior to surgery.
 | Table I.Characteristics of patients with
lumbar spinal stenosis. |
Table I.
Characteristics of patients with
lumbar spinal stenosis.
| Parameter | MISS | COS |
|---|
| Total number | 41 | 41 |
| Male | 19 | 21 |
| Female | 22 | 20 |
| Age (years) | 50.4–65.6 | 49.2–68.4 |
| Mean BMI
(kg/m2) | 26.4 | 25.2 |
| Neurogenic
claudication | 17 | 14 |
| Numbness | 26 | 29 |
| Leg pain | 24 | 20 |
| Back pain | 17 | 21 |
| Follow-up duration
(months) | 12 | 12 |
Efficacy of MISS on postoperative pain
for patients with lumbar spinal stenosis
As indicated in Fig.
1, patients in the MISS group exhibited lower VAS scores
compared with the COS group at 3 and 6 months post-surgery. There
was no significant difference in VAS between the two groups at 9 or
12 months post-surgery. As indicated in Fig. 2, MISS exhibited greater efficacy
compared with COS at relieving back and leg pain at 3 months
post-surgery for patients with lumbar spinal stenosis. None of the
patients demonstrated postoperative deterioration in neurological
status.
Efficacy of MISS for postoperative
inflammation and infection in patients with lumbar spinal
stenosis
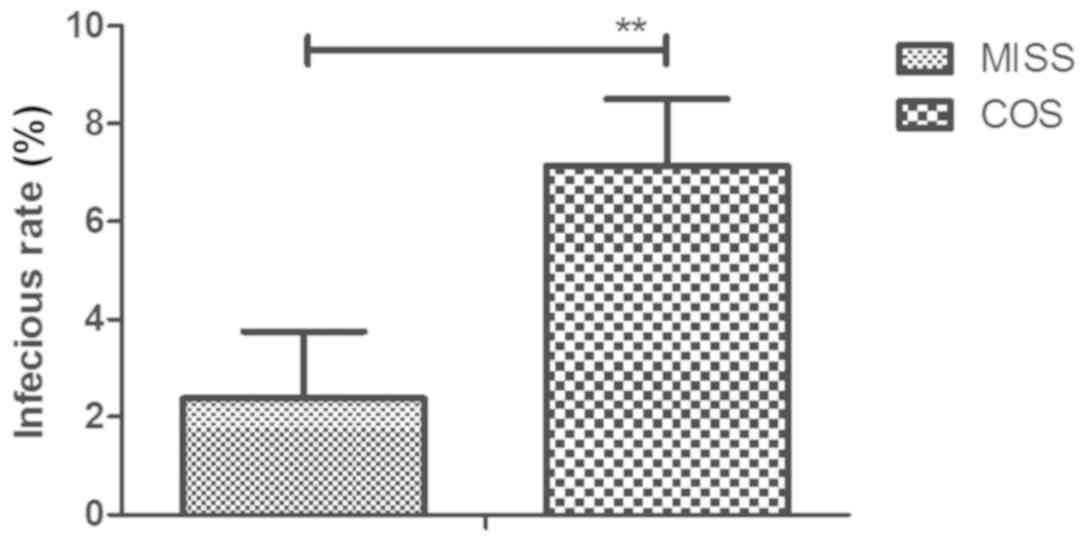
Inflammation and infection was analyzed in patients
with lumbar spinal stenosis following MISS or COS. All patients
received ampicillin antibiotic regimen for a total of 14 days. The
inflammatory score was significantly decreased in patients who
received MISS compared with those who received COS on days 6, 12
and 18 post-surgery (Fig. 3). As
indicated in Fig. 4, patients who
received MISS exhibited significantly lower infection rates
compared with COS (2.38 vs. 7.17%). None of the patients exhibited
postoperative incurable infection.
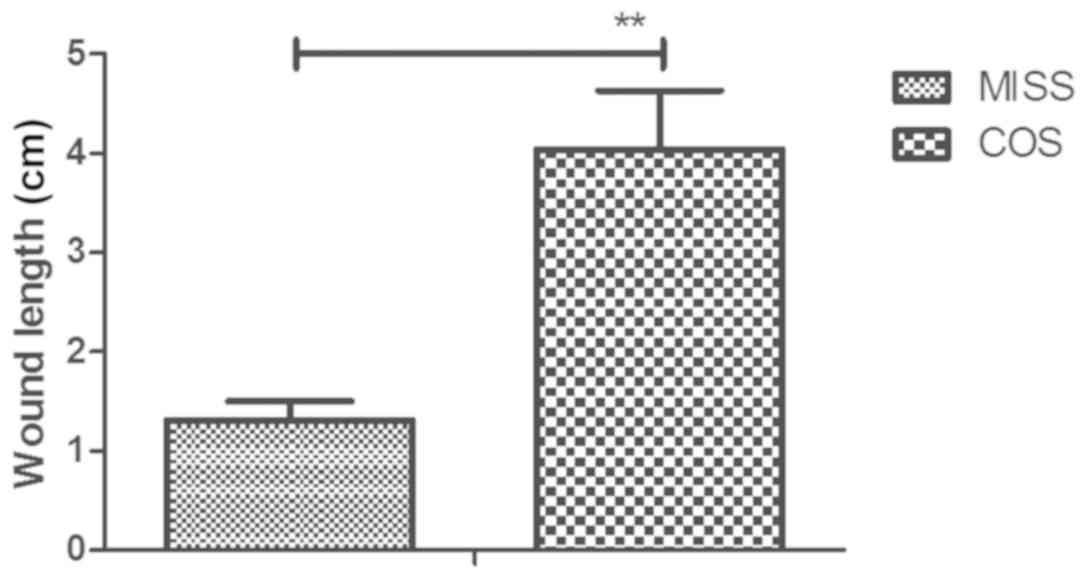
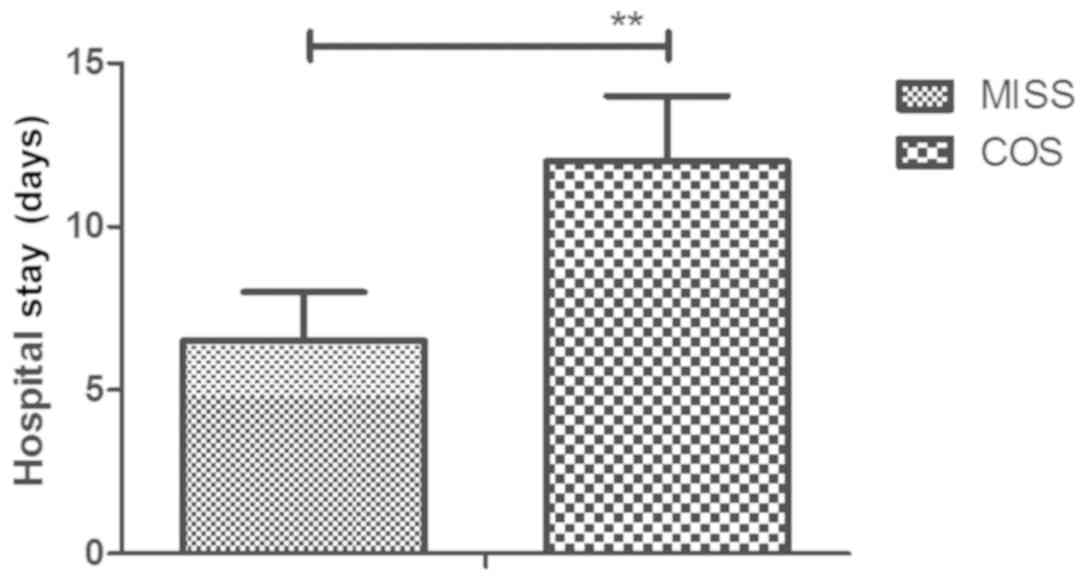
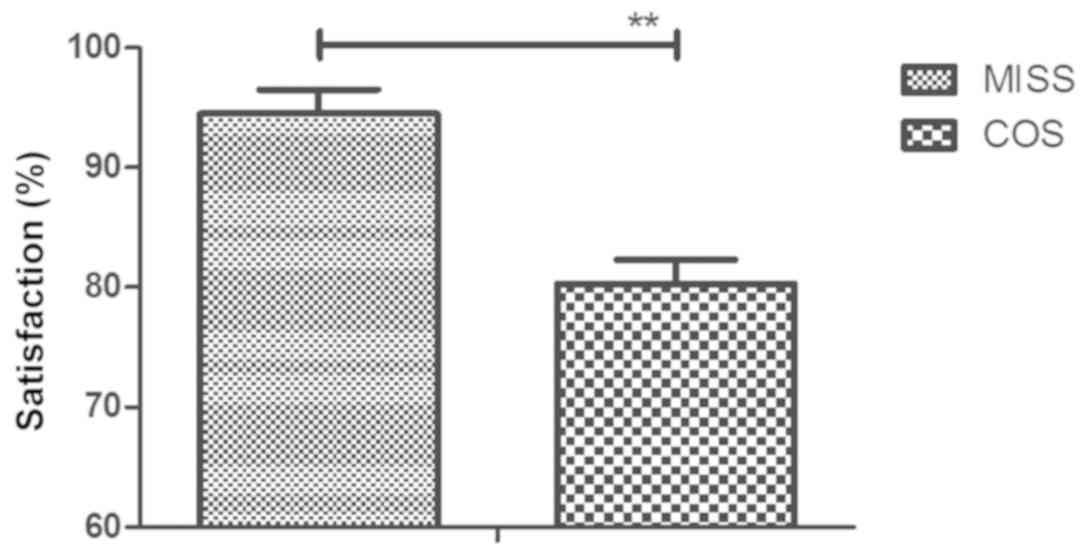
Efficacy of MISS for recovery in
patients with lumbar spinal stenosis
As indicated in Fig.
5, preoperative wound length was significantly increased in the
COS group compared with the MISS group (4.04 vs. 1.32 cm). Length
of hospital stay was significantly shorter in the MISS group
compared with the COS group (Fig. 6;
6.5 vs. 12 days). Patient satisfaction was significantly higher in
the MISS group (94.8%) compared with the COS group (80.3%), as
determined by PSI (overall satisfaction) during the 12-month
follow-up period (Fig. 7). None of
the patients succumbed during the 12-month follow-up period.
Discussion
Lumbar spinal stenosis is one of the most common
orthopedic diseases and the incidence rate is more than 5% in the
elderly population worldwide (20).
COS is the most common method used for the treatment of lumbar
spinal stenosis (18). However, in
recent years, MISS has been widely used for patients with lumbar
spinal stenosis (21). In the
current study, the efficacy of MISS and COS was compared in
patients with lumbar spinal stenosis. It was identified that MISS
presented advantages over COS for patients with lumbar spinal
stenosis, including improvements of back and leg pain,
postoperative inflammation and infection rate in the clinic. The
current findings indicated that patients with lumbar spinal
stenosis who received MISS reported higher satisfaction compared
with those who received COS during a 12-month follow-up period.
None of the patients demonstrated postoperative incurable
infection, postoperative deterioration in neurological status or
mortality.
Complications occur frequently for patients with
lumbar spinal stenosis following surgery, including surgical site
infection, bone graft migration, intraoperative neurological injury
and dural tear (22). A previous
study indicated that microendoscopic discectomy MISS techniques
could decrease postoperative complications for lumbar spinal
stenosis patients (23). In the
current study, no cases of intraoperative neurological injury, bone
graft migration or dural tear were observed. However, 4 patients in
the COS group presented with surgical site infection, while 1
patient presented with surgical site infection in the MISS group.
Notably, MISS exhibited better therapeutic effects compared with
COS in relieving back and leg pain at 0 and 3 months post-surgery
as determined by ODI and VAS.
For patients with lumbar spinal stenosis,
inflammation may affect the length of hospital stays (24). A previous study reviewed the role of
muscular markers, inflammatory parameters and cytokines and
concluded that MISS efficiently decreased post-surgery inflammation
compared with COS (24). In the
current study, it was observed that patients with lumbar spinal
stenosis that underwent MISS exhibited a lower inflammation score
and shorter hospital stays compared with those that underwent COS.
A previous study indicated that decreasing postoperative surgical
infection using MISS may decrease mortality rates (10). In the current study, it was reported
that MISS efficiently decreased postoperative surgical infections
in patients with lumbar spinal stenosis compared with COS.
In conclusion, the current findings indicate that
are significant differences between the outcomes of MISS and COS
for patients with lumbar spinal stenosis in terms of inflammation
score, infection rate, VAS and ODI. The study identified that MISS
resulted in improved symptoms in patients with lumbar stenosis,
including reduced postoperative pain and shorter hospital stays.
Therefore, it could be regarded as a standard treatment for
patients with lumbar spinal stenosis. However, prospective
randomized studies should be performed in a larger lumbar spinal
stenosis population in order to verify the conclusions of the
current study.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HP performed the experiments. GT, XZ, SL and YB
prepared and analyzed experimental data. LX designed the
experiments.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Affiliated National Hospital of Guangxi Medical
University (Nanning, China). Written informed consent was obtained
from all patients.
Patient consent for publication
Written informed consent was obtained from all
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Houten JK and Nasser R: Symptomatic
progression of degenerative scoliosis after decompression and
limited fusion surgery for lumbar spinal stenosis. J Clin Neurosci.
20:613–615. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kuang MJ, Ma JX and Ma XL: Decompression
and coflex interlaminar stabilization compared with conventional
surgical procedures for lumbar spinal stenosis: A systematic review
and meta-analysis. Int J Surg. 45:164–165. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ulrich NH, Kleinstück F, Woernle CM,
Antoniadis A, Winklhofer S, Burgstaller JM, Farshad M, Oberle J,
Porchet F and Min K; LumbSten Research Collaboration, : Clinical
outcome in lumbar decompression surgery for spinal canal stenosis
in the aged population: A prospective Swiss multicenter cohort
study. Spine (Phila Pa 1976). 40:415–422. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Minamide A, Yoshida M, Iwahashi H, Simpson
AK, Yamada H, Hashizume H, Nakagawa Y, Iwasaki H, Tsutsui S,
Kagotani R, et al: Minimally invasive decompression surgery for
lumbar spinal stenosis with degenerative scoliosis: Predictive
factors of radiographic and clinical outcomes. J Orthop Sci.
22:377–383. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moojen WA and Peul WC: Minimally invasive
surgery for lumbar spinal stenosis. BMJ. 350:h16642015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim HJ, Lee JI, Kang KT, Chang BS, Lee CK,
Ruscheweyh R, Kang SS and Yeom JS: Influence of pain sensitivity on
surgical outcomes after lumbar spine surgery in patients with
lumbar spinal stenosis. Spine (Phila Pa 1976). 40:193–200. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vasudeva VS and Chi JH: Fusion surgery for
lumbar spinal stenosis. N Engl J Med. 375:5982016.PubMed/NCBI
|
|
8
|
Park CK, Kim SB, Kim MK, Park BJ, Choi SG,
Lim YJ and Kim TS: Comparison of treatment methods in lumbar spinal
stenosis for geriatric patient: Nerve block versus radiofrequency
neurotomy versus spinal surgery. Korean J Spine. 11:97–102. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang ZH, Wu DH, Ma C and Dai WX: Surgical
treatment of postoperative deep wound infection after posterior
lumbar interlumbar fusion of the lumbar stenosis. Zhongguo Gu
Shang. 25:928–930. 2012.(In Chinese). PubMed/NCBI
|
|
10
|
Yaldiz C, Yaldiz M, Ceylan N, Kacira OK,
Ceylan D, Kacira T, Kizilcay G and Tanriverdi T: Retrospective,
demographic, and clinical investigation of the causes of
postoperative infection in patients with lumbar spinal stenosis who
underwent posterior stabilization. Medicine (Baltimore).
94:e11772015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Polikandriotis JA, Hudak EM and Perry MW:
Minimally invasive surgery through endoscopic laminotomy and
foraminotomy for the treatment of lumbar spinal stenosis. J Orthop.
10:13–16. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lauryssen C: Technical advances in
minimally invasive surgery: Direct decompression for lumbar spinal
stenosis. Spine (Phila Pa 1976). 35 (Suppl 26):S287–S293. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sakalauskienė G, Obelienius V, Pilvinienė
R and Jauniškienė D: Evaluation of daily outpatient
multidisciplinary rehabilitative treatment of patients with
musculoskeletal, neurological and traumatic disorders in a
municipality outpatient setting. Medicina (Kaunas). 52:61–68. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Scott J and Huskisson EC: Graphic
representation of pain. Pain. 2:175–184. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Copay AG, Glassman SD, Subach BR, Berven
S, Schuler TC and Carreon LY: Minimum clinically important
difference in lumbar spine surgery patients: A choice of methods
using the Oswestry disability index, Medical outcomes study
questionnaire Short Form 36, and pain scales. Spine J. 8:968–974.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lane SS and Holland EJ: Loteprednol
etabonate 0.5% versus prednisolone acetate 1.0% for the treatment
of inflammation after cataract surgery. J Cataract Refract Surg.
39:168–173. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hudak EM and Perry MW: Outpatient
minimally invasive spine surgery using endoscopy for the treatment
of lumbar spinal stenosis among obese patients. J Orthop.
12:156–159. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Haddadi K and Ganjeh Qazvini HR: Outcome
after surgery of lumbar spinal stenosis: A randomized comparison of
bilateral laminotomy, trumpet laminectomy, and conventional
laminectomy. Front Surg. 3:192016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Aghayev E, Elfering A, Schizas C and
Mannion AF; SWISSSpine Registry Group, : Factor analysis of the
North American Spine Society outcome assessment instrument: A study
based on a spine registry of patients treated with lumbar and
cervical disc arthroplasty. Spine J. 14:916–924. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Coronado-Zarco R, Cruz-Medina E,
Arellano-Hernández A, Chavez-Arias D and León-Hernández SR:
Effectiveness of calcitonin in intermittent claudication treatment
of patients with lumbar spinal stenosis: A systematic review. Spine
(Phila Pa 1976). 34:E818–E822. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rubino F, Deutsch H, Pamoukian V, Zhu JF,
King WA and Gagner M: Minimally invasive spine surgery: An animal
model for endoscopic approach to the anterior cervical and upper
thoracic spine. J Laparoendosc Adv Surg Tech A. 10:309–313. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Podichetty VK, Spears J, Isaacs RE, Booher
J and Biscup RS: Complications associated with minimally invasive
decompression for lumbar spinal stenosis. J Spinal Disord Tech.
19:161–166. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ikuta K, Tono O, Tanaka T, Arima J, Nakano
S, Sasaki K and Oga M: Surgical complications of microendoscopic
procedures for lumbar spinal stenosis. Minim Invasive Neurosurg.
50:145–149. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Imajo Y, Taguchi T, Neo M, Otani K, Ogata
T, Ozawa H, Miyakoshi N, Murakami H and Iguchi T: Complications of
spinal surgery for elderly patients with lumbar spinal stenosis in
a super-aging country: An analysis of 8,033 patients. J Orthop Sci.
22:10–15. 2017. View Article : Google Scholar : PubMed/NCBI
|