Introduction
Unstable angina is a common disease in clinic, which
frequently occurs in the middle-aged and elderly people, and will
easily develop into myocardial infarction if not treated in time.
In recent years, with the increase of social pressure on
middle-aged people and the increase of aging population, the
incidence rate of unstable angina has also shown an increasing
trend year by year. Studies have also revealed that angina is
possibly related to obesity and familial inheritance (1,2).
Coronary atherosclerosis can lead to stenosis of vascular lumen,
and ischemic necrosis occurs easily in the myocardium with
underdeveloped collateral circulation, thus resulting in myocardial
infarction. Atheromatous plaques are mainly composed of cholesterol
and cholesteryl ester characterized by high brittleness, which,
under the influence of heart rate, blood pressure and myocardial
contractility, will rupture or fall off easily and flow with the
blood, blocking small blood vessels or capillaries, forming
thrombus and aggravating myocardial infarction (3–5).
Currently, conservative medical therapy is dominated in the
treatment of unstable angina, such as anti-platelet aggregation,
dilatation of coronary artery and lipid lowering. According to the
research on pathogenesis of unstable angina, the inflammatory
response-induced decline in the stability of atherosclerotic
plaque, platelet activation and aggregation are important
conditions causing the disease, so alleviating inflammatory
response, improving plaque stability and inhibiting platelet
activation are important measures to prevent the progression of
unstable angina and reduce the risk of myocardial infarction
(6,7).
Nicorandil is a nitrate drug with an effect of
opening potassium ion channel possessing anti-inflammatory,
anti-oxidation and endothelium protective functions (8). Therefore, it has been widely applied in
the treatment after interventional operation of coronary heart
disease, achieving positive curative effects (9). However, the value of nicorandil in the
treatment of unstable angina remains unclear. Thus, the effects of
nicorandil on inflammatory factors, platelet and myocardial
antioxidant function in patients with unstable angina were
studied.
Patients and methods
Basic data
A total of 157 patients diagnosed with unstable
angina in the First People's Hospital of FoShan (Affiliated FoShan
Hospital of Sun Yat-sen University; Foshan, China) from 2012 to
2017 were selected (10). The
patients were numbered as 1, 2, 3….157 and then divided into even
and odd number group, then further defined as experimental and
control group, respectively. Considering that several patients in
the control group were unstable angina pectoris accompanied with
myocardial infarction, these patients were included in the
experimental group. Finally, 73 patients in the control group and
84 patients in the experimental group were included. Basic data,
such as age, sex, familial genetic history, obesity index and
underlying complications, including diseases associated with
unstable angina, including myocardial infarction, coronary heart
disease, hypertension, liver diseases (fatty liver, high
cholesterol and gallstone) and diabetes, were comparable between
the two groups of patients (P>0.05).
The study was approved by the Ethics Committee of
the First People's Hospital of FoShan (Affiliated FoShan Hospital
of Sun Yat-sen University). Patients who participated in this
research had complete clinical data. The signed informed consents
were obtained from the patients or the guardians.
Treatment methods
At the beginning of treatment, patients in both
groups were orally administered conventional drugs for angina,
including aspirin tablets + metoprolol + atorvastatin + isosorbide
dinitrate. Patients were asked to take nitroglycerin under tongue
at the onset of angina. Hypertension patients were given
antihypertensive drugs, and hyperlipidemia patients took statins
for lipid-lowering treatment. Patients in the experimental group,
based on conventional drug treatment, were orally administered
nicorandil tablets (15 mg/day, 5 mg/tablet, H20080418, Asahi Kasei
Corporation), t.i.d., for 21 days as one course of treatment.
Observation indexes
Before and after treatment, venous blood was
collected and EDTA was added for anticoagulation. Then the blood
was centrifuged at 2,000 × g for 10 min at 4°C. Changes in levels
of matrix metalloproteinase-9 (MMP-9; ELISA kit), high-sensitivity
C-reactive protein (hs-CRP; C-SPOT kit), superoxide dismutase (SOD;
ELISA kit) and malondialdehyde (MDA; C-SPOT kit) in the supernatant
were detected via enzyme-linked immunosorbent assay (ELISA). The
platelet function was detected through labeling and screening
platelet fluorescence antibodies, such as CD63, CD42b and GP-VI.
Moreover, parameters in thromboelastogram, such as coagulation
response time (R), formation time of coagulation block (K),
thrombosis rate (Angle), comprehensive coagulation index (CI) and
maximum amplitude (MA), were measured using a coagulation analyzer
(TEG-5000, Haemonetics). Angle represents the rate angle of
hemocyte agglutination, which indicates the angle between tangent
line and horizontal line from the forming point to the maximum
curve Radian of the marker map. MA represents the maximum strength
or hardness of the clot and the stable form of the clot. All
experimental operations were carried out by specialized technicians
in strict accordance with the steps of the kit, and the
experimental data were repeated three times to take the average
value.
MMP-9 and hs-CRP as anti-inflammatory factor in the
blood can reflect the occurrence and level of inflammation in the
blood. SOD and MDA are reductive substances in cells representing
the strength of antioxidant capacity of cardiomyocytes. Coagulation
reaction time, clotting time, thrombus formation rate, synthetic
coagulation index and maximum amplitude were the parameters of
platelet coagulation function. These parameters were selected to
represent the levels of inflammation, myocardial antioxidant
capacity and platelet function in patients with unstable angina
pectoris. These parameters were easy to detect, and had little
damage to the patients.
Statistical analysis
SPSS17.0 (SPSS Inc., Chicago, IL, USA) was used for
statistical analysis. Chi-square test was used for counting data
and paired t-test was used for measuring data. P<0.05 was
considered as the difference with statistical significance.
Results
Comparison of basic data between the
two groups of patients
Basic data, including sex, age, body mass index,
familial genetic history, basic disease had no statistically
significant differences between the two groups of patients, and
they were comparable (P>0.05) (Table
I).
 | Table I.Comparison of basic data between the
two groups of patients. |
Table I.
Comparison of basic data between the
two groups of patients.
| Item | Control group
(n=73) | Experimental group
(n=84) |
t/F/χ2-value | P-value |
|---|
| Sex
(male/female) | 34/39 | 34/50 | 0.55 | 0.36 |
| Age (years) | 56.7±11.5 | 58.6±10.8 | 2.19 | 0.76 |
| Body mass index ≥25
kg/m2 | 27 | 33 | 0.02 | 0.76 |
| Familial genetic
history | 15 | 23 | 0.65 | 0.31 |
| Basic disease |
|
Myocardial infarction | 34 | 45 | 0.51 | 0.38 |
| Coronary
heart disease | 32 | 48 | 2.26 | 0.09 |
|
Hypertension | 26 | 31 | 1.12 | 0.86 |
| Liver
disease | 7 | 12 | 0.43 | 0.36 |
|
Diabetes | 4 | 6 | 0.009 | 0.67 |
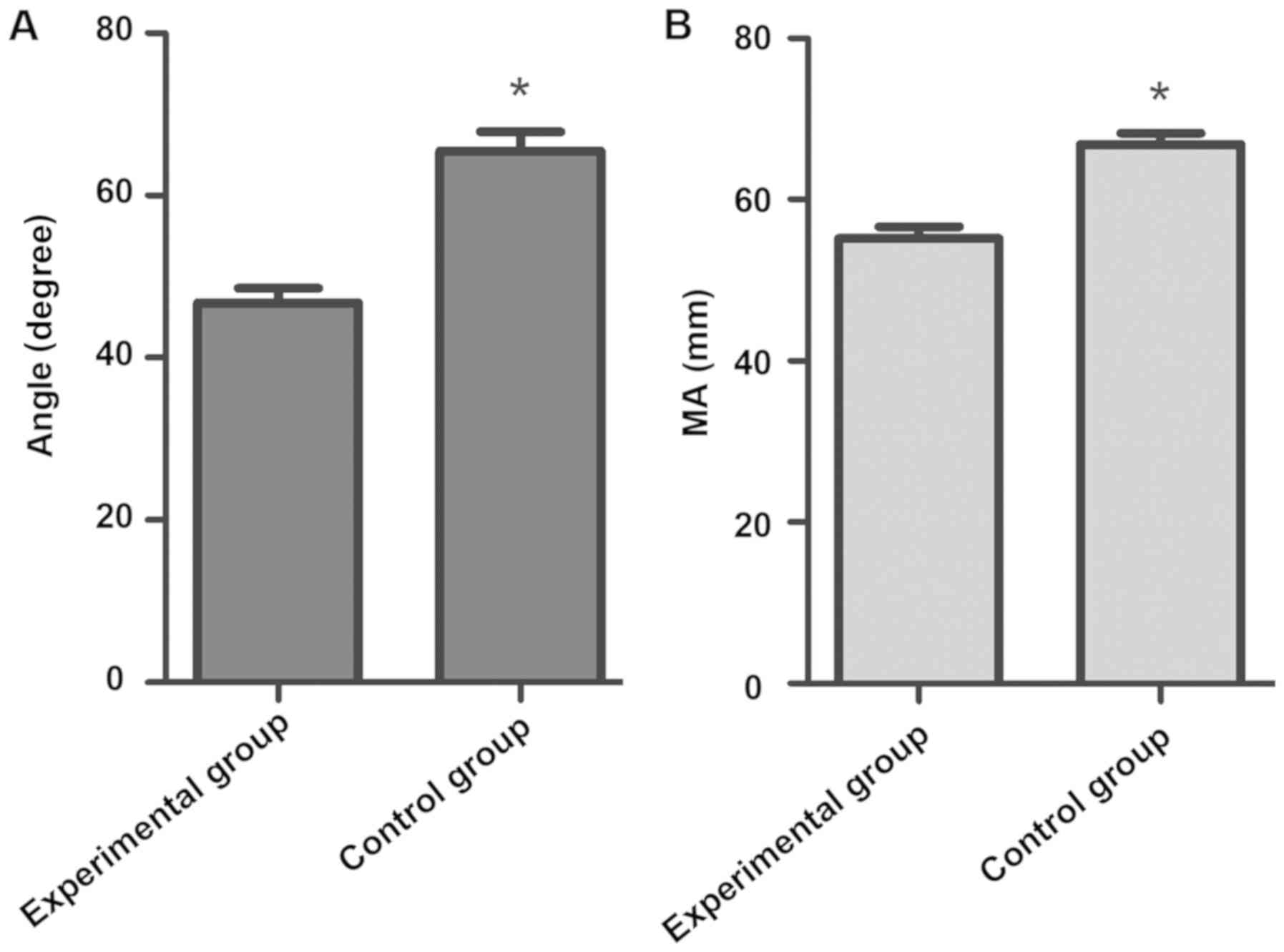
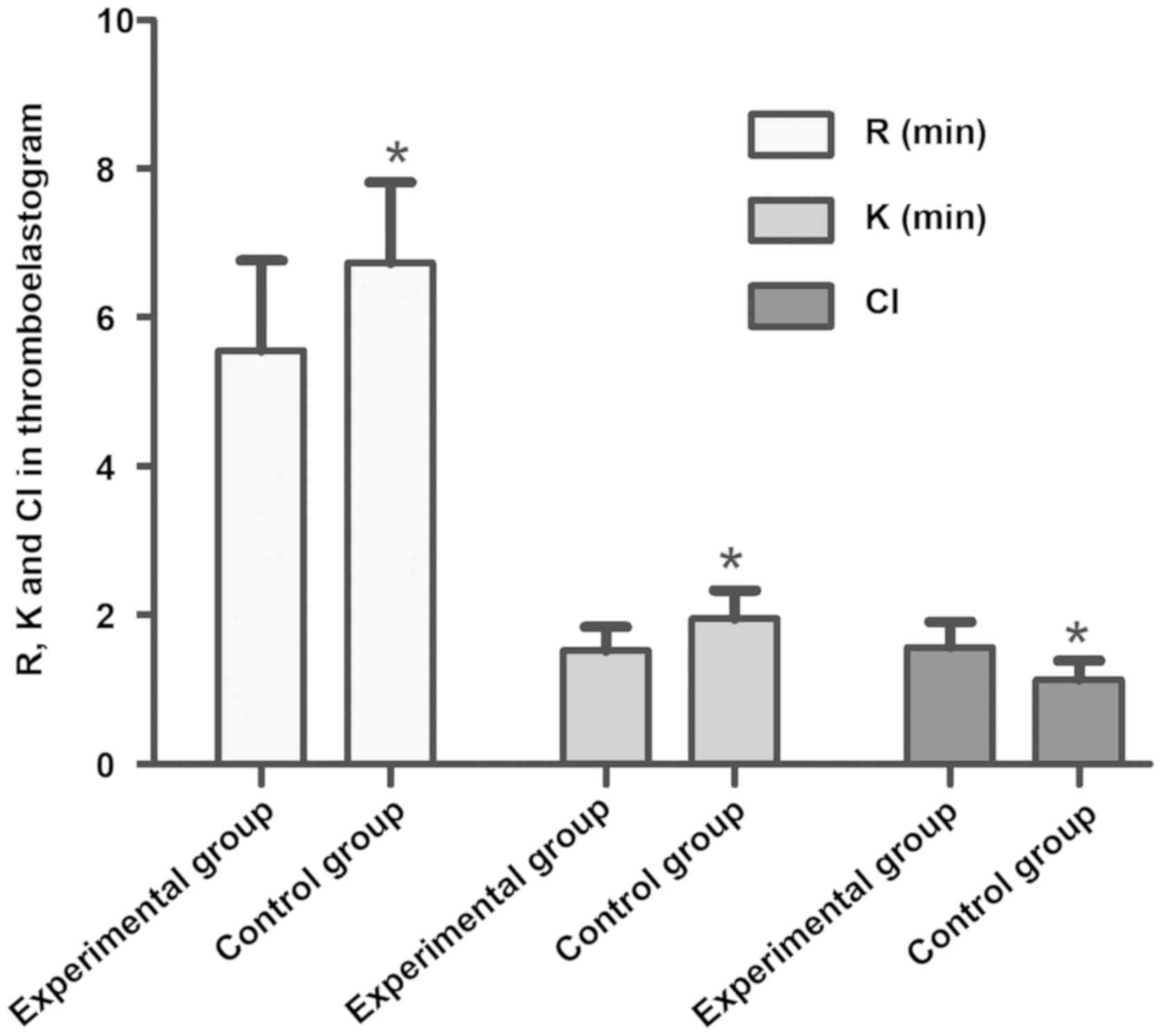
Comparison of platelet function
between the two groups of patients
After treatment, the platelet function was compared
between the two groups of patients. Results revealed that
expression of platelet membrane glycoproteins GP-VI, CD42b, PAC-1
and CD63 in the experimental group was 31.7±6.72, 27.8±5.33,
21.54±3.28 and 36.7±8.25, respectively, which is lower than those
in control group (P<0.05), while R and K in the experimental
group were longer than those in control group, showing
statistically significant differences (P<0.05). The above
indicates that the experimental group can inhibit better the
activation and the platelet function (Table II and Figs. 1 and 2).
 | Table II.Comparison of platelet parameters
between the two groups of patients. |
Table II.
Comparison of platelet parameters
between the two groups of patients.
| Groups | GP-VI | CD42b | PAC-1 | CD63 |
|---|
| Control (n=73) | 77.5±13.64 | 49.6±7.29 | 41.7±8.59 | 63.16±9.27 |
| Experimental
(n=84) |
31.7±6.72a |
27.8±5.33a |
21.54±3.28a |
36.7±8.25a |
Comparison of serum hs-CRP and MMP-9
levels between the two groups of patients
After treatment for 21 days, levels of serum hs-CRP
and MMP-9 in both groups of patients declined compared with those
before treatment. Levels of (6.07±0.94) and MMP-9 (49.2±6.22) in
the experimental group declined more significantly than those in
control group (t=12.93 and 8.95, P<0.05), and differences were
statistically significant, indicating that nicorandil can
significantly reduce levels of serum hs-CRP and MMP-9 in patients
with unstable angina and inhibited the activation of platelet by
serum inflammatory factors (Table
III).
 | Table III.Comparison of serum hs-CRP and MMP-9
levels between the two groups of patients. |
Table III.
Comparison of serum hs-CRP and MMP-9
levels between the two groups of patients.
|
| hs-CRP (ng/ml) | MMP-9 (pg/ml) |
|---|
|
|
|
|
|---|
| Groups | Before treatment | After treatment | Before treatment | After treatment |
|---|
| Control (n=73) | 16.36±1.33 | 9.14±1.23 | 227.63±36.81 | 82.9±9.48 |
| Experimental
(n=84) | 16.87±1.54 |
6.07±0.94a | 233.73±32.55 |
49.2±6.22a |
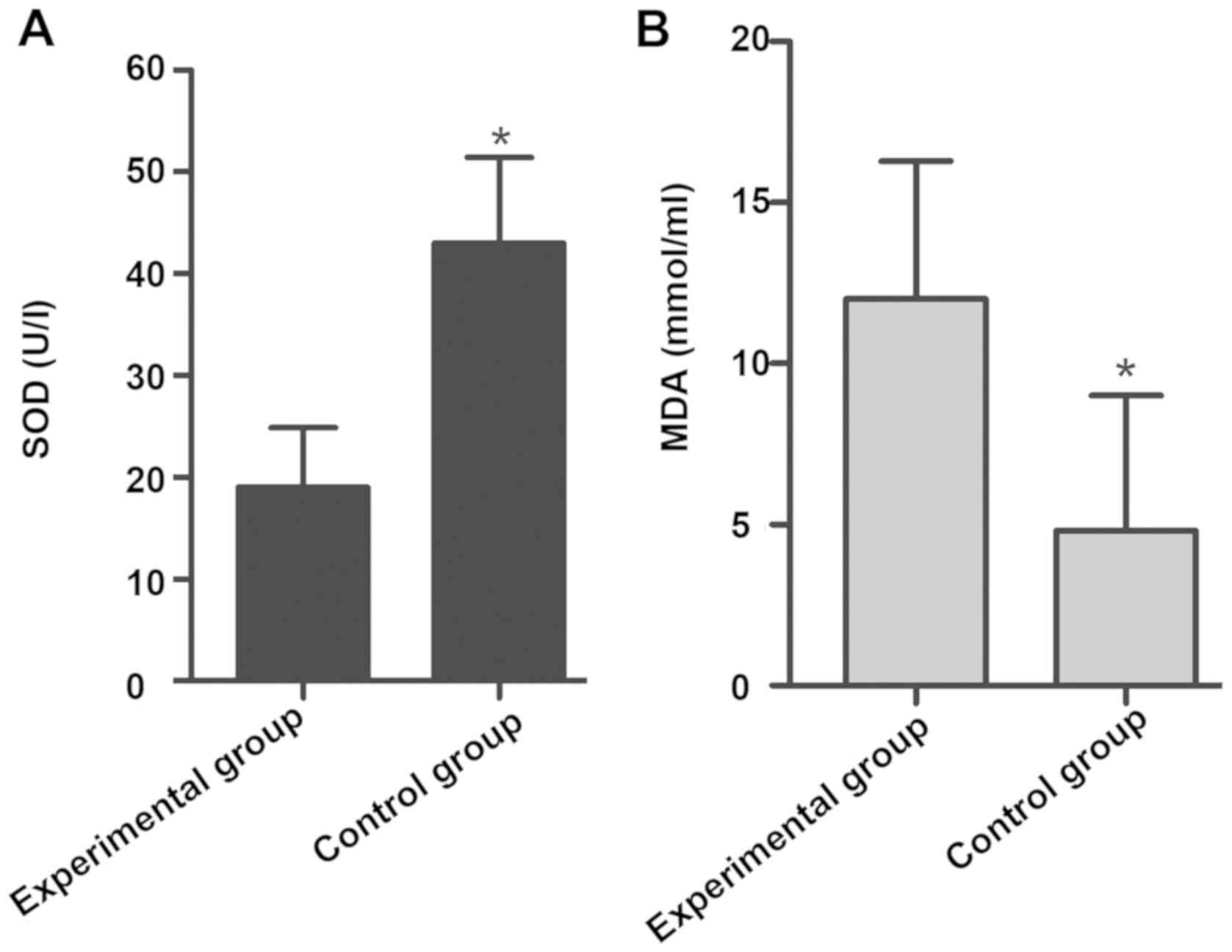
Comparison of myocardial antioxidant
function between the two groups of patients
Levels of serum anti-oxidation molecules MDA and SOD
were compared between the two groups of patients after treatment.
Results manifested that the serum SOD level was increased, while
the MDA level declined (results are not shown) in both groups
compared with those before treatment. Changes in levels of
anti-oxidation molecules were more significant in the experimental
group compared with those in control group (P<0.05) (Fig. 3).
Discussion
Stable angina will develop into unstable angina with
the increased frequency of pain, increase of precipitating factors
and progressive aggravation due to a variety of factors (11,12). Due
to the instability of local coronary artery lesions in patients and
other factors, the frequency, degree and precipitating factors of
angina are often changed, the pain will aggravate or return to
stability, and unstable angina may develop into myocardial
infarction in late stage (13),
affecting the normal life and work of patients. Currently,
conservative medical therapy dominates the treatment of unstable
angina, including anticoagulation therapy, inhibition of platelet
aggregation and activation, lipid-regulating drugs, blood pressure
lowering, thrombolytic therapy and dilation of blood vessels.
High-risk patients may also be treated with emergency
interventional therapy or emergency coronary artery bypass grafting
(14–16). In conservative medical therapy,
nicorandil is often applied as an adjuvant drug for unstable
angina, which, as a nitrate drug with an effect of opening
potassium ion channel, it can reduce the level of calcium ion
through activating guanylate-activating enzymein cells, thereby
relaxing the vascular smooth muscle and dilating the coronary
artery (17,18). In addition, nicorandil also possesses
anti-inflammatory, anti-oxidation and endothelium protective
functions. However, nicorandil has adverse reactions such as
inducing mucosal ulcer, and it easily leads to hemorrhage and
infection in patients (19,20), so there is still a certain risk in
the clinical application of nicorandil in the treatment of unstable
angina, and further in-depth research is needed.
The occurrence and development of unstable angina is
a complex process involving a variety of predisposing factors.
Atherosclerotic plaque, myocardial ischemia and viscous blood lipid
can induce unstable angina, in which platelet activation and
aggregation play key roles. After the rupture of atherosclerotic
plaque, the collagen under the vascular endothelium is exposed,
activating and aggregating platelets. Platelets aggregate around
the plaque and release a large number of inflammatory factors,
accelerating the formation of thrombus, leading to stenosis of
coronary arterial lumen and reducing the blood flow, thereby
resulting in insufficient myocardial blood supply. At the same
time, platelets will also release inflammatory factors into the
blood after activation, and then these inflammatory factors can
change the texture and stability of atherosclerotic plaque, induce
the rupture of atherosclerotic plaque, and promote the formation of
thrombus. In addition, oxygen free radicals can also induce the
expression of inflammatory cytokines in endothelial cells,
increasing the incidence of cardiovascular and cerebrovascular
diseases. SOD can scavenge the superoxide ion by disproportionation
and reduce the damage of the endothelial cells caused by oxygen
free radicals. Therefore, anti-inflammation, and inhibition of
platelet activation and reducing oxygen free radicals are the most
important links in the treatment process of patients with unstable
angina. This study investigated the effects of nicorandil on
platelet activation, inflammatory factors and myocardial
antioxidant function in patients with unstable angina, so as to
provide clinical data support for the treatment of patients with
unstable angina.
Collectively, it was found that expression of
platelet membrane glycoproteins CD63, PAC-1, CD42b and GP-VI
obviously declined in patients taking nicorandil, and R and K in
peripheral blood were longer than those in patients who did not
take nicorandil, while Angle, MA, and CI were lower than those in
patients who did not take nicorandil, indicating that nicorandil
can inhibit platelet activation and reduce thrombosis rate and
capacity in patients with unstable angina. Moreover, results of
blood biochemical study revealed that the decline in the content of
serum CRP and MMP-9 in experimental group was more significant than
that in control group, suggesting that nicorandil has a certain
effect of reducing the inflammatory response in patients with
unstable angina. In the analysis of myocardial antioxidant function
of patients, changes in levels of anti-oxidation factors MDA and
SOD were also compared between experimental group and control
group. Results manifested that after treatment, the level of SOD in
the experimental group was higher than that in the control group,
and the decreasing level of MDA was also higher than that in the
control group (P<0.05), indicating that nicorandil has a certain
effect of increasing myocardial anti-oxidation factors, improving
myocardial anti-oxidation level and protecting myocardium. At
present, nicorandil can be used not only in patients with
hypertension, but also in patients with angina pectoris, but the
therapeutic effect of nicorandil in patients with unstable colic
needs to be further studied. The side effect of nicorandil is
mainly headache, dizziness and other adverse reactions. The
comprehensive drug effect and metabolism in patients with unstable
angina pectoris are worthy of further study.
In conclusion, nicorandil can help reduce
inflammatory response, inhibit platelet function, increase
myocardial anti-oxidation level and improve therapeutic efficacy of
patients with unstable angina, which is worthy of further promotion
and application in clinic.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RP wrote the manuscript and collected the basic
information of patients. XY and XL recorded and analyzed
observation indexes. All the authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the First People's Hospital of FoShan (Affiliated FoShan Hospital
of Sun Yat-sen University; Foshan, China). Patients who
participated in this research had complete clinical data. The
signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
MacMahon S, Sharpe N, Gamble G, Hart H,
Scott J, Simes J and White H; LIPID Trial Research Group, : Effects
of lowering average of below-average cholesterol levels on the
progression of carotid atherosclerosis: Results of the LIPID
Atherosclerosis Substudy. Circulation. 97:1784–1790. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hauser ER, Mooser V, Crossman DC, Haines
JL, Jones CH, Winkelmann BR, Schmidt S, Scott WK, Roses AD,
Pericak-Vance MA, et al Design of the Genetics of Early Onset
Cardiovascular Disease study, : Design of the Genetics of Early
Onset Cardiovascular Disease (GENECARD) study. Am Heart J.
145:602–613. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vasilieva EJ, Shpector AV, Raskuragev AB,
Lekochmacher SS and Bespalko IA: Platelet function and plasma lipid
levels in patients with stable and unstable angina pectoris. Am J
Cardiol. 68:959–961. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ogawa H, Yasue H, Misumi I, Masuda T,
Okumura K, Bannai S, Takanashi N and Tsukada Y: Plasma
platelet-derived growth factor levels in coronary circulation in
unstable angina pectoris. Am J Cardiol. 69:453–456. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chakhtoura EY, Shamoon FE, Haft JI,
Obiedzinski GR, Cohen AJ and Watson RM: Comparison of platelet
activation in unstable and stable angina pectoris and correlation
with coronary angiographic findings. Am J Cardiol. 86:835–839.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fitzgerald DJ: Platelet activation in the
pathogenesis of unstable angina: Importance in determining the
response to plasminogen activators. Am J Cardiol. 68:51B–57B. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fitzgerald DJ, Roy L, Catella F and
FitzGerald GA: Platelet activation in unstable coronary disease. N
Engl J Med. 315:983–989. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Frampton J, Buckley MM and Fitton A:
Nicorandil. A review of its pharmacology and therapeutic efficacy
in angina pectoris. Drugs. 44:625–655. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim JH, Jeong MH, Yun KH, Kim KH, Kang DK,
Hong SN, Lim SY, Lee SH, Lee YS, Hong YJ, et al: Myocardial
protective effects of nicorandil during percutaneous coronary
intervention in patients with unstable angina. Circ J. 69:306–310.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Natarajan M: Unstable angina. Clin Evid.
8:225–235. 2002.
|
|
11
|
Xu FH and Wang JM: Clinical observation on
acupuncture combined with medication for intractable angina
pectoris Zhongguo Zhenjiu. 25:89–91. 2005.(In Chinese). PubMed/NCBI
|
|
12
|
Tada M: Unstable angina. Nippon Naika
Gakkai Zasshi. 72:721–726. 1983.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ibuki C: Unstable angina. Nihon Rinsho. 2
(Suppl 5):234–239. 2007.(In Japanese).
|
|
14
|
Waters DD, Walling A, Roy D and Théroux P:
Previous coronary artery bypass grafting as an adverse prognostic
factor in unstable angina pectoris. Am J Cardiol. 58:465–469. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Faxon DP, Detre KM, McCabe CH, Fisher L,
Holmes DR, Cowley MJ, Bourassa MG, Van Raden M and Ryan TJ: Role of
percutaneous transluminal coronary angioplasty in the treatment of
unstable angina. Report from the National Heart, Lung, and Blood
Institute Percutaneous Transluminal Coronary Angioplasty and
Coronary Artery Surgery Study Registries. Am J Cardiol.
53:131C–135C. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lubsen J: Medical management of unstable
angina. What have we learned from the randomized trials?
Circulation. 82 (Suppl):II82–II87. 1990.PubMed/NCBI
|
|
17
|
Walker A, McMurray J, Stewart S, Berger W,
McMahon AD, Dargie H, Fox K, Hillis S, Henderson NJ and Ford I:
Economic evaluation of the impact of nicorandil in angina (IONA)
trial. Heart. 92:619–624. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim SJ, Kim W, Woo JS, Ha SJ, Kang WY,
Hwang SH, Kang DG, Lee SU, Cho SK, Im JS, et al: Effect of
myocardial protection of intracoronary adenosine and nicorandil
injection in patients undergoing non-urgent percutaneous coronary
intervention: A randomized controlled trial. Int J Cardiol.
158:88–92. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Egred M: Nicorandil-associated
ulcerations. Eur J Gastroenterol Hepatol. 19:395–398. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gupta A and Morris G: Major aphthous
ulcers induced by nicorandil. Age Ageing. 29:372–373. 2000.
View Article : Google Scholar : PubMed/NCBI
|