Introduction
Septic shock is the most common acute critical
disease encountered at the Intensive Care Unit (ICU). Septic shock
is also the major cause of death at the ICU (1). The annual incidence of reported cases
of septic shock is increasing year by year. Determination of the
prognosis of patients with septic shock remains a difficult problem
for clinicians. Disturbance of hemodynamics is the most prominent
manifestation of septic shock (2).
To maintain the stability of the cycle in the early stage of shock,
resuscitation of a large amount of fluid is frequently required.
After sufficient fluid resuscitation, certain patients exhibit
obvious responses, including an increased amount of urine or blood
pressure, while other patients exhibit a lesser reaction, leading
to infusion of more fluids and gradually more tissue edema, but
those patients remain in a state of hypotension with no increase in
urine.
Once a patient's condition improves, a large amount
of liquid returns to the blood vessels. If the function of the
patient's heart, lung, liver and kidney are intact at this time,
the excess liquid is eliminated by increasing the amount of urine,
which is referred to as a negative balance of liquid in the clinic
and the edema of the whole body fades away. Once this negative
balance of fluid is present, fluid resuscitation may cause
excessive load and aggravate the burden of the heart and lung.
Indirect evaluation of prognosis through evaluating the success of
fluid resuscitation has become the focus of clinical research
(3). As a low-perfusion index for
patients with septic shock, lactic acid has been used for numerous
years (4). However, multiple
non-perfusion factors may also cause an increase in lactic acid and
consequently, the reliability of this index is limited. Therefore,
the discovery of novel and more accurate indicators has become a
hot spot of clinical research.
The Acute Physiology and Chronic Health Evaluation
(APACHE II) score is used to evaluate the severity of septic shock,
with a higher score indicating more serious septic shock, more
extensive physiological dysfunction of the body and greater
difficulty for patients to reach a negative fluid balance (5). The Sequential Organ Failure Assessment
(SOFA) score numerically quantifies the number of organs with
failure and the severity thereof (6). The two indexes are commonly used to
evaluate the severity of septic shock in the clinic. Ospina-Tascón
et al (7) indicated that the
combination of arterial lactate levels and ratio of venous-arterial
CO2 to arterial-venous O2
(Cv-aCO2/Da-vO2) exhibited an improved
ability to identify high-risk.
The aim of the present study was to investigate
whether Cv-aCO2/Da-vO2 may serve as an
independent predictor of the success rate of resuscitation and the
prognosis of patients with septic shock. Also the present study
aimed to further clarify the specific value of
Cv-aCO2/Da-vO2 as a high-risk indicator.
Patients and methods
Patients
The clinical data of patients (n=108; male, 74;
female, 34) with septic shock treated at the ICU, The First
Hospital of Shijiazhuang (Shijiazhuang, China), from March 2012 to
December 2017, were retrospectively reviewed. The patient
characteristics are listed in Table
I. The inclusion criteria were as follows: i) Patients with
septic shock who received resuscitation at the ICU; ii) the septic
shock was diagnosed in accordance with the diagnostic criteria of
septic shock of International Sepsis Definitions Conference in 2001
(8): Systolic blood pressure <90
mmHg, or <40 mmHg than the base value, patient is not able to
recover or requires maintenance by vasoactive drugs after 1 h of
fluid resuscitation, patients with low perfusion of organ tissue
and patients with lactic acid poisoning, oliguria or changes in
state of acute consciousness. Patients were excluded if the
following applied: Age of <18 years, pregnancy, chronic renal
failure, acute cerebrovascular disease, severe arrhythmia, valvular
heart disease, untreated tumors, expected death within 48 h and
excessive volume load as judged by the clinicians, or patients with
heart function intolerance of dilatant. The present study was
approved by the Ethics Committee of First Hospital of Shijiazhuang
and written informed consent was obtained from each subject or
their immediate family members.
 | Table I.Baseline data of the 2 groups. |
Table I.
Baseline data of the 2 groups.
| Variable | Group A | Group B | P-value |
|---|
| Case (N) | 52 | 56 | – |
| Sex (male, N) | 36 | 38 | 0.878 |
| Age (yrs.) | 59 (51–71) | 60 (47–69) |
|
| APACHE II
Score | 17.9±2.0 | 18.5±2.2 | 0.123 |
| SOFA score at day
1 | 8.86±1.7 | 8.72±1.8 | 0.679 |
Resuscitation
A dual-lumen vein catheter was inserted through the
internal jugular vein or subclavian vein after patients were
admitted to the ICU. Standardized treatment was performed following
the China guidelines for sepsis from 2014, as early as possible
(9). This included fluid
resuscitation as soon as possible, vasoactive drug application,
complete recording of etiological information within 1 h,
antibiotic application and oxygen therapy. The resuscitation target
in the first 6 h was as follows: Central venous pressure (CVP) 8–12
mmHg, mean arterial pressure (MAP) ≥65 mmHg, urine volume ≥0.5
ml/kg/h, central venous oxygen saturation (SCVO2) ≥70%
or SvO2 ≥65% and a superior vena cava oxygen saturation
of >70%.
Demographic data and parameters
Demographic data, including the patients' gender and
age, as well as basic vital signs, including body temperature,
heart rate, blood pressure were obtained. Routine examination
indexes, including arterial blood gas analysis, upper vena cava
blood gas analysis, routine hematuria, liver and kidney function,
electrolytes, myocardial enzymes and myocardial markers were
determined, and chest, thoracic and abdominal computed tomography
was performed. The following parameters were evaluated with a GEM
Premier 4000 blood gas analyzer (GE Healthcare) and recorded:
Cv-aCO2/Da-vO2 ratio at 6-h of resuscitation,
resuscitation rate at 6 h, incidence of multiple organ dysfunction
and mortality rate at day 7 and 35. The
Cv-aCO2/Da-vO2 was calculated according to
Ospina-Tascón et al (7) with
assistance by Werfen.
Statistical analysis
Statistical analysis was performed with SPSS 19
software (IBM Corp.). The measured data were expressed as the mean
± standard deviation. Continuous variables between the 2 groups
were compared using the t-test and count data were compared with a
Chi-squared test. Kaplan-Meier analysis with the log-rank
(Mantel-Cox) test was performed to compare survival in the 2 groups
with follow up to 35 days. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline data
After screening, 108 cases treated between January
2012 and December 2017 were selected. Of these, 59 cases were male
and 49 were female, and their average age was 55.4±13.4 (range
34–71) years. The patients were divided into 2 groups according to
the calculated Cv-aCO2/Da-vO2 ratio at 6 h
after fluid resuscitation: Group A,
Cv-aCO2/Da-vO2 >1 (n=52); group B,
Cv-aCO2/Da-vO2 <1 (n=56). The average age
was 63.2±5.2 years in group A and 61.9±3.2 years in group B. The
baseline data of the 2 groups are listed in Table I. Comparison indicated that the age
and gender distribution were not significantly different between
the 2 groups, while group A had a lower APACHE II score and higher
SOFA score at day 1; however, the differences were not
significant.
Resuscitation within 24 h
Table II provides a
comparison of resuscitation data between the two groups. The ratio
of subjects who reached the target of resuscitation at 6 h was not
significantly different between groups A and B (40/52 vs. 43/56;
P=0.987), while the ratio of subjects who reached the target of
resuscitation was significantly decreased in group A compared with
that in group B at 24 h (42/52 vs. 53/56; P=0.027). In addition,
the 24-h lactate clearance rate in group A was significantly lower
than that in group B (0.21±0.14 vs. 0.47±0.15; P<0.0001). The
number of cases with SCVO2 >70% in group A was also
lower than that group B (30 vs. 44; P=0.038) and the 24-h cardiac
output (CO) in group A was significantly decreased compared with in
group B (4.47±0.34 vs. 5.03±0.41; P<0.0001).
 | Table II.Comparison of 2 groups with 24-h of
resuscitation. |
Table II.
Comparison of 2 groups with 24-h of
resuscitation.
| Variable | Group A | Group B | P-value |
|---|
| Case (N) | 52 | 56 | – |
| Mechanical
ventilation (case, N) | 49 | 54 | 0.587 |
| Adrenaline user
(case, N) | 52 | 56 | – |
| Resuscitation
volume at 6-h (ml) | 3,029±320 | 2,992±288 | 0.529 |
| Reached targeted
resuscitation case at 6-h (N) | 40 | 43 | 0.987 |
| Lactate clearance
rate at 6-h (%) | 16.5±10.2 | 23.5±15.2 | 0.0063 |
| CO at 6-h
(l/min) | 4.45±0.38 | 4.85±0.49 | <0.0001 |
| Reached targeted
resuscitation case at 24-h (N) | 42 | 53 | 0.0268 |
| Lactate clearance
rate at 24-h (%) | 21.1±13.9 | 47.4±15.6 | <0.0001 |
| Case of
SCVO2 at 24-h >70% (N) | 30 | 44 | 0.038 |
| CO at 24-h
(l/min) | 4.47±0.34 | 5.03±0.41 | <0.0001 |
| Mortality at day 7
(N, dead/survival) | 29/23 | 6/50 | <0.001 |
| Mortality at day 35
(N, dead/survival) | 37/15 | 21/35 | <0.001 |
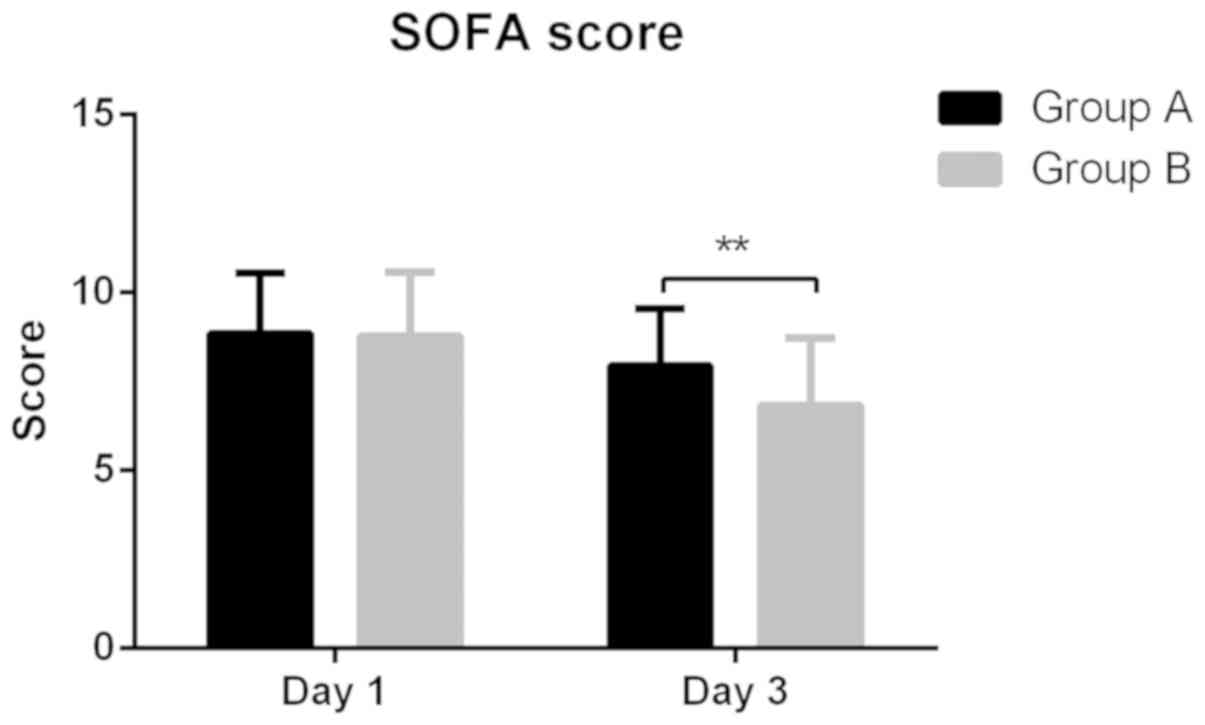
SOFA score and mortality
At day 1, the SOFA score in group A was similar to
that in group B and the SOFA score had decreased in the two groups
after resuscitation. At day 3, the SOFA score was significantly
decreased in group B compared with in group A (6.82±1.92 vs.
7.94±1.62; P=0.0013; Fig. 1). In
addition, the mortality rate at day 7 and 35 was significantly
higher in group A when compared with that group B (29/52 vs. 6/56;
P<0.001; 37/52 vs. 21/56; P<0.001), which was shown in
Table II.
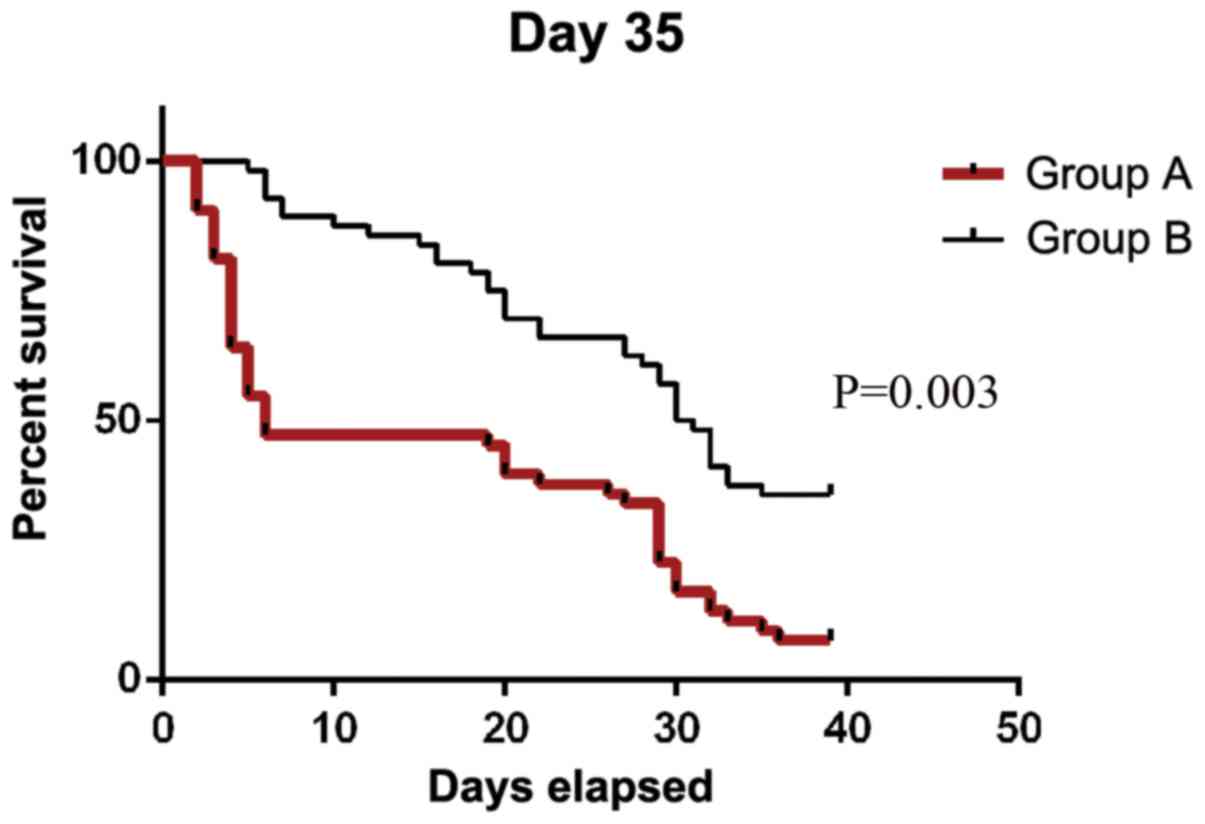
Survival analysis
Kaplan-Meier analysis with the log-rank (Mantel-Cox)
test was performed to compare survival in the 2 groups with follow
up to 35 days. The results suggested that survival in group A was
significantly lower than that in group B (P=0.003; Fig. 2). The median survival time in group A
during 35-day period was 6 days, while the median survival time in
group B was 17 days.
Discussion
The treatment of sepsis represents a severe
healthcare challenge worldwide. The reported incidence of sepsis in
the past 10 years in developed countries is 4.37/100,000 per year,
with a mortality rate of 17.1%. The incidence of severe sepsis is
2.72/100,000 per year, with a mortality rate of 26.4% (10). A Chinese study determined that the
number of hospitalized sepsis patients accounts for >50% of the
total number of ICU patients (11).
For developing countries, no relevant data are available, but the
rate is expected to be even higher.
Since Rivers et al (1) proposed the concept of early
goal-directed therapy in 2001, early fluid resuscitation therapy
for septic shock has received widespread clinical attention. A
series of guidelines published in recent years have affirmed that
early fluid resuscitation, early diagnosis and early hemodynamic
support are important means of septic shock treatment (12–14).
Rivers et al (1) also
proposed to achieve the goal of resuscitation within 6 h after the
onset of septic shock and strive to correct early hemodynamic
abnormalities and systemic tissue hypoxia in the early stage of
shock in order to prevent the occurrence of more serious
inflammation and multiple organ failure. Fitch and Gossage
(15) determined that if the MAP was
raised to 65–75 mmHg within 1 h after fluid resuscitation, the
hemodynamic status of septic shock patients was significantly
improved in the early stage. Early fluid resuscitation in septic
shock can improve hemodynamic stability, improve tissue and organ
perfusion, reduce the incidence of multiple organ failure and
reduce mortality.
These benefits stem from the increased emphasis on
monitorable and assessable goal-directed therapy in early fluid
resuscitation. Fluid resuscitation remains a challenge in daily
practice due to the potential hazards of insufficient vascular
content and overload. Various methods have been developed to set
targets for fluid resuscitation. Simple evaluation of the vital
signs, CVP and urine volume as indicators has certain limitations.
SCVO2 may reflect the balance of oxygen supply and
demand in the entire body. When SCVO2 is >70%, oxygen
supply and demand reach a balance. SCVO2 may be used as
an evaluation index of fluid resuscitation in the early stage of
septic shock (16).
A recent study confirmed that the SCVO2
value is frequently reported to be normal or near normal on
admission to the ICU (17). In
addition, normal hemodynamic and oxygen metabolism indices do not
ensure adequate tissue perfusion and do not prevent progression and
organ dysfunction leading to death or complete organ failure
(18). Lactic acid has also been
proposed as a target for resuscitation (19). In fact, not only the basic level of
lactate, but the direction of lactate level changes after treatment
intervention is also associated with clinical prognosis (20). However, the effects that have been
reported when using the lactate-oriented resuscitation cluster
strategy are not consistent among studies (21). Therefore, more indicators reflecting
tissue hypoperfusion should be explored, particularly when
SCVO2 is close to normal.
Recently, the partial pressure of carbon dioxide
(Pv-aCO2) has been recommended as an alternative
indicator of hypoperfusion (22).
Derived from oxygen parameters, persistently elevated
Pv-aCO2 is an independent predictor of poor prognosis
and may predict changes of lactate levels (22). However, high cardiac conduction to
high flow prevents the accumulation of intravenous carbon dioxide
in septic shock (23).
Pv-aCO2 may be normal even in the presence of severe
tissue hypoperfusion; similarly, due to the Haldane effect,
Pv-aCO2 increases in certain patients even without
tissue hypoperfusion (22).
Therefore, the change of CO2 must be evaluated through
the change in O2. Under aerobic metabolism conditions,
the production of CO2 should not exceed the utilization
of O2. Thus, the ratio of
Pv-aCO2/Da-vO2 may replace the ratio of
VCO2/VO2 (i.e. respiratory quotient) and
identify patients at risk of anaerobic metabolism.
Using this principle, Mekontso-Dessap et al
(24) demonstrated that
Pv-aCO2/Da-vO2 >1.4 was significantly
superior to Pv-aCO2, SvO2 and
Da-vO2 in predicting hyperlactatemia in critically ill
patients. Importantly, changes in
Pv-aCO2/Da-vO2 are more sensitive than lactic
acid, making it an attractive monitoring indicator. Therefore, when
SCVO2 or SvO2 is relatively low, the change
of Cv-aCO2/Da-vO2 may better reflect the
change of oxygen consumption than that of
Pv-aCO2/Da-vO2. This is due to
Cv-aCO2/Da-vO2 reflecting persistent
anaerobic metabolism.
Ospina-Tascón et al (7) suggested that
Cv-aCO2/Da-vO2 is a reliable indicator for
resuscitation, while the present clearly indicated that 1 is a
suitable threshold. In the present study, it was demonstrated that
the CO at 6 and 24 h, ratio of patients who reached the target of
resuscitation at 24 h, lactic acid clearance rate at 24 h and
number of cases with SCVO2 >70% were decreased in
patients with Cv-aCO2/Da-vO2 >1. In
addition, the mortality rate at day 7 and 35 was increased in
patients with Cv-aCO2/Da-vO2 >1 and the
survival rate was different at day 35, which demonstrated that
Cv-aCO2/Da-vO2 may be used to effectively
evaluate the success rate of resuscitation and identify patients at
high risk of adverse outcomes. It may be suggested that if the
Cv-aCO2/Da-vO2 ratio is >1, early
intervention may improve the prognosis of such patients.
If patients present with a
Cv-aCO2/Da-vO2 ratio of <1, it provides a
measure of the extent of anaerobic metabolism. In this case, the
present study recommends the following actions: Increase the dose
of fluid resuscitation, increase CO, improve total hypoxia levels
and improve the respiratory function of patients. If the
Cv-aCO2/Da-vO2 ratio increases, indicating
improved prognosis, intensive fluid resuscitation can then be
reduced.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science and
Technology Support Plan of Shijiazhuang Science and Technology
Bureau (grant no. 151460623).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ was in charge of manuscript writing and data
analysis. XS and SW were in charge of clinical data recording. ZH
and HC were in charge of design of the experiments, analysis and
interpretation of the data, and also provided funding support. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of First Hospital of Shijiazhuang and written informed
consent was obtained from each subject or their immediate family
members.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rivers E, Nguyen B, Havstad S, Ressler J,
Muzzin A, Knoblich B, Peterson E and Tomlanovich M; Early
Goal-Directed Therapy Collaborative Group, : Early goal-directed
therapy in the treatment of severe sepsis and septic shock. N Engl
J Med. 345:1368–1377. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Feihl F, Waeber B and Liaudet L: The
hemodynamics of septic shock: A historical perspective. Curr Vasc
Pharmacol. 11:133–138. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Long B, Koyfman A, Modisett KL and Woods
CJ: Practical considerations in sepsis resuscitation. J Emerg Med.
52:472–483. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhou X, Liu D, Su L, Yao B, Long Y, Wang
X, Chai W, Cui N, Wang H and Rui X: Use of stepwise lactate
kinetics-oriented hemodynamic therapy could improve the clinical
outcomes of patients with sepsis-associated hyperlactatemia. Crit
Care. 21:332017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hwang SY, Lee JH, Lee YH, Hong CK, Sung AJ
and Choi YC: Comparison of the sequential organ failure assessment,
acute physiology and chronic health evaluation II scoring system,
and trauma and injury severity score method for predicting the
outcomes of intensive care unit trauma patients. Am J Emerg Med.
30:749–753. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Granholm A, Moller MH, Krag M, Perner A
and Hjortrup PB: Predictive performance of the simplified acute
physiology score (SAPS) II and the initial sequential organ failure
assessment (SOFA) score in acutely Ill intensive care patients:
Post-hoc analyses of the SUP-ICU inception cohort study. PLoS One.
11:e01689482016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ospina-Tascón GA, Umaña M, Bermúdez W,
Bautista-Rincón DF, Hernandez G, Bruhn A, Granados M, Salazar B,
Arango-Dávila C and De Backer D: Combination of arterial lactate
levels and venous-arterial CO2 to arterial-venous
O2 content difference ratio as markers of resuscitation
in patients with septic shock. Intensive Care Med. 41:796–805.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Levy MM, Fink MP, Marshall JC, Abraham E,
Angus D, Cook D, Cohen J, Opal SM, Vincent JL and Ramsay G:
SCCM/ESICM/ACCP/ATS/SIS: 2001 SCCM/ESICM/ACCP/ATS/SIS international
sepsis definitions conference. Crit Care Med. 31:1250–1256. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lang J, Li J, Li L and Hu D: China's
guidelines for the treatment of severe sepsis/septic shock. Chin
Med Assoc Severe med. 27:401–426. 2015.
|
|
10
|
De Freitas ER: Profile and severity of the
patients of intensive care units: Prospective application of the
APACHE II index. Rev Lat Am Enfermagem. 18:317–323. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fang W: A correlation analysis of the
change rate of APACHE II scores and the prognosis in severe ill ICU
patients. Chin J Crit Care Med. 33:919–921. 2013.
|
|
12
|
Larsen GY, Mecham N and Greenberg R: An
emergency department septic shock protocol and care guideline for
children initiated at triage. Pediatrics. 127:e1585–e1592. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhou X, Liu D, Long Y, Mei D, Chai W, Rui
X, Wang X, Wang H, Zhang Q, Guo H, et al: Prognostic outcomes of
adherence to guideline of bundle therapy by key points of control
strategies in septic shock patients. Zhonghua Yi Xue Za Zhi.
94:994–998. 2014.(In Chinese). PubMed/NCBI
|
|
14
|
Pruinelli L, Westra BL, Yadav P, Hoff A,
Steinbach M, Kumar V, Delaney CW and Simon G: Delay within the
3-hour surviving sepsis campaign guideline on mortality for
patients with severe sepsis and septic shock. Crit Care Med.
46:500–505. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fitch SJ and Gossage JR: Optimal
management of septic shock. Rapid recognition and institution of
therapy are crucial. Postgrad Med. 111:53–64. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Marx G and Reinhart K: Venous oximetry.
Curr Opin Crit Care. 12:263–268. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee YK, Hwang SY, Shin TG, Jo IJ, Suh GY
and Jeon K: Prognostic value of lactate and central venous oxygen
saturation after early resuscitation in sepsis patients. PLoS One.
11:e01533052016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Guo Z, Yin M, Kong J, Wang B, Dai K, Zuo
T, Yu G and Bao Y: Relationship analysis of central
venous-to-arterial carbon dioxide difference and cardiac index for
septic shock. Sci Rep. 9:88222019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rady MY, Rivers EP and Nowak RM:
Resuscitation of the critically ill in the ED: Responses of blood
pressure, heart rate, shock index, central venous oxygen
saturation, and lactate. Am J Emerg Med. 14:218–225. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shin TG, Jo IJ, Hwang SY, Jeon K, Suh GY,
Choe E, Lee YK, Lee TR, Cha WC and Sim MS: Comprehensive
interpretation of central venous oxygen saturation and blood
lactate levels during resuscitation of patients with severe sepsis
and septic shock in the emergency department. Shock. 45:4–9. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tobias AZ, Guyette FX, Seymour CW,
Suffoletto BP, Martin-Gill C, Quintero J, Kristan J, Callaway CW
and Yealy DM: Pre-resuscitation lactate and hospital mortality in
prehospital patients. Prehosp Emerg Care. 18:321–327. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mallat J, Lemyze M, Tronchon L, Vallet B
and Thevenin D: Use of venous-to-arterial carbon dioxide tension
difference to guide resuscitation therapy in septic shock. World J
Crit Care Med. 5:47–56. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wan XY, Wei LL, Jiang Y, Li P and Yao B:
Effects of time delay and body temperature on measurements of
central venous oxygen saturation, venous-arterial blood carbon
dioxide partial pressures difference, venous-arterial blood carbon
dioxide partial pressures difference/arterial-venous oxygen
difference ratio and lactate. BMC Anesthesiol. 18:1872018.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mekontso-Dessap A, Castelain V, Anguel N,
Bahloul M, Schauvliege F, Richard C and Teboul JL: Combination of
venoarterial PCO2 difference with arteriovenous
O2 content difference to detect anaerobic metabolism in
patients. Intensive Care Med. 28:272–277. 2002. View Article : Google Scholar : PubMed/NCBI
|