Introduction
Silicosis is the most serious occupational disease
and is caused by long-term inhalation of large amount of free
silica dust and deposition in the lung to cause pulmonary fibrosis
as the main pathological change. Silicosis is the most common type
of pneumoconiosis with rapid progression and poor prognosis
(1–3). As its specific pathogenesis has not
been fully studied, there are no specific drugs that can alleviate
or reverse silica-induced lung injury. The purpose of clinical
treatment is to control the progressive development of lung injury,
improve the quality of life and prolong the life span of the
patients (4,5).
Tetrandrine is a calcium channel blocker, and can
reduce the level of type I and III collagen mRNA in lung tissue and
collagen deposition in the lung. It can effectively alleviate
pulmonary fibrosis and inflammatory reaction of the body, and is an
effective drug for the treatment of silicosis (6,7).
N-acetylcysteine decreased the content of reactive oxygen species
(ROS) in the lung tissue of rats exposed to silica, thus inhibiting
apoptosis of mitochondria and alleviating the severity of pulmonary
fibrosis (8). In recent years, a
small number of studies have reported the therapeutic effect of
tetrandrine combined with N-acetylcysteine in silicosis. The
combination of the two can effectively alleviate the clinical
symptoms such as cough, chest tightness and improve respiratory
function in patients with silicosis (9). However, this method has not been widely
used in clinical treatment, and its therapeutic effect has not been
widely confirmed. In a rat model of silicosis, the therapeutic
effect of tetrandrine combined with N-acetylcysteine was again
verified. The results showed that the combined therapy could
effectively reduce the levels of malondialdehyde (MDA), TNF-α and
IL-6 in lung tissue and alleviate the silica-induced pulmonary
fibrosis in rats (10). These
studies have reported better therapeutic effects of tetrandrine
combined with N-acetylcysteine in silicosis.
In order to confirm the therapeutic effect of
tetrandrine combined with N-acetylcysteine in silicosis, this study
used clinical experiments to verify and analyze the relationship
between TNF-α, IL-6 and the clinical therapeutic effect, so as to
provide guidance for clinical judgement of the prognosis of
silicosis patients.
Patients and methods
General materials
In this study, 196 patients with silicosis admitted
to Qingdao Central Hospital (Qingdao, China), aged 40 to 70 years,
were collected by prospective analysis. The patients were divided
into two groups according to the different methods of treatment.
One hundred and eight patients in the control group received
routine treatment, including anti-inflammatory, cough and asthma
relief. Eighty-eight patients in the observation group were treated
with tetrandrine combined with N-acetylcysteine on the basis of
routine treatment.
Inclusion and exclusion criteria
Inclusion criteria
All patients met the 2015 GBZ70-2015 Diagnostic
Criteria for Pneumoconiosis (11);
the patient was treated for the first time in this hospital; the
patients were not exposed to silicon dioxide during treatment; this
study followed the principles of the Helsinki Declaration.
Exclusion criteria
Patients with history of tuberculosis or period of
tuberculosis activity; patients with other causes of pulmonary
fibrosis; patients with lung tumor; patients with other severe
organ dysfunction; patients with autoimmune diseases and history of
it; patients with systemic inflammatory response syndrome; pregnant
or lactating women.
The study was approved by the Ethics Committee of
Qingdao Central Hospital, and patients were consulted by telephone
or letter. Each patient and/or their family signed an informed
consent form.
Therapeutic method
Control group
Included anti-inflammatory, cough and asthma relief;
the main drugs were ambroxol hydrochloride oral liquid (Harbin
Renhuang Pharmaceutical Co., Ltd.; SFDA Approval no. H20067008) 10
ml/time, twice a day, tiobutramine bromide powder inhaler (Jiangsu
Zhengda Tianqing Pharmaceutical Co., Ltd.; SFDA Approval no.
H20060454), one each time, once a day, with nutritional support and
lung rehabilitation training.
Observation group
On the basis of the control group, tetrandrine
combined with N-acetylcysteine was given. Tetrandrine (Zhejiang
China Resources Sanjiu Zhongyi Pharmaceutical; SFDA Approval no.
2236H1330) 60 mg-100 mg/time, 3 times a day, taken for 6 days and
then stopped for 1 day, with a course of treatment of 3 months.
Acetylcysteine effervescent tablets (Zambon S.p.A.; SFDA Approval
no. H20140449) 1 tablet/time, 1–2 times/day. The treatment lasted 8
months in both groups.
Evaluation criteria
The curative effect of the two groups was analyzed
by X-ray, and the incidence of adverse reactions was compared
between the two groups. The changes of pulmonary function indexes
and the distance of 6-min walking test were analyzed in the groups.
The changes of IL-6 and TNF-α in the peripheral blood of the two
groups were measured before and after treatment, and the
relationship between IL-6, TNF-α and the therapeutic effect was
analyzed.
Test method
Efficacy assessment methods: TOSHIBA multi-function
remote-control digital X-ray machine was purchased from Toshiba
Medical Systems Co., Ltd.; all the patients were examined by X-ray
before and after treatment, and the films were read by 3 attending
doctors with 10-year working experience in this hospital. Grading:
the lung texture is obviously reduced to be markedly effective, the
lung shadow is reduced to be effective, the lung texture is not
changed or even increased and aggravated in ineffective result.
Total effective rate = markedly effective rate + effective
rate.
Lung function
MSPFT- B pulmonary function instrument was purchased
from Shanghai Hanfei Medical Devices Co., Ltd.; main observation
indexes were respiratory rate (RR), forced vital capacity (FVC),
and first second forced expiratory volume (FEV1).
6-min walk experiment
A 20 m-long straight line was plotted on the flat to
record the patient's 6-min walking distance and assess the
patient's exercise tolerance.
ELISA
Levels of IL-6, TNF-α were detected by ELISA; the
test kits were purchased from Wuhan Ellette Biotechnology Co., Ltd.
(SFDA Approval no. E-EL-H0102c, E-EL-H0109c), and the specific test
steps referred to the kit instructions.
Statistical analysis
SPSS 19.0 (Asia Analytics Formerly SPSS China) was
used. Enumeration data were expressed in rates. χ2 test
was used to compare the rate. Measurement data were expressed in
mean ± SD. Independent sample t-test was used for comparison
between the two groups. Paired t-test was used for intra-group
comparison. The relationship between IL-6, TNF-α and the
therapeutic effect was analyzed by ROC curve. P<0.05 was
considered a statistically significant difference.
Results
General materials
There were 108 patients in the control group,
including 70 males (64.81%) and 38 females (35.19%) aged
48.67±12.59 years. There were 88 patients in the observation group,
including 61 males (69.32%) and 27 females (30.68%) aged
52.44±14.72 years. There was no significant difference in sex ratio
and age between the two groups (P>0.05). There was no
significant difference in BMI, stage, dust exposure time and type
of work between the two groups (P>0.05) (Table I).
 | Table I.General information. |
Table I.
General information.
| Features | Control group
(n=108) | Observation group
(n=88) | χ2/t | P-value |
|---|
| Sex [n (%)] |
|
| 0.444 | 0.505 |
| Male | 70 (64.81) | 61 (69.32) |
|
|
|
Female | 38 (35.19) | 27 (30.68) |
|
|
| Age (years) | 48.67±12.59 | 52.44±14.72 | 1.932 | 0.055 |
| BMI
(kg/m2) | 18.25±0.83 | 18.37±0.62 | 1.124 | 0.262 |
| Stage [n(%)] |
|
| 0.345 | 0.833 |
| I | 55 (50.92) | 41 (46.59) |
|
|
| II | 35 (32.41) | 31 (35.23) |
|
|
| III | 18 (16.67) | 16 (18.18) |
|
|
| Dust exposure time
(years) | 7.43±3.25 | 7.83±3.47 |
|
|
| Type of work [n
(%)] |
|
| 4.361 | 0.499 |
|
Roadheader | 32 (29.63) | 23 (26.14) |
|
|
|
Stonecutter | 39 (36.11) | 26 (29.55) |
|
|
| Raw
material worker | 11 (10.18) | 12 (13.64) |
|
|
| Rock
driller | 13 (12.04) | 12 (13.64) |
|
|
|
Stoker | 11 (10.18) | 9
(10.23) |
|
|
| Comminution
worker | 2 (1.85) | 6 (6.82) |
|
|
| Smoking history [n
(%)] |
|
| 0.034 | 0.854 |
| Yes | 22 (20.37) | 17 (19.32) |
|
|
| No | 86 (79.63) | 71 (80.68) |
|
|
Analysis of clinical efficacy
The markedly effective rate and total effective rate
of treatment in the observation group were significantly higher
than those in the control group (P<0.05), and the ineffective
rate was lower than that in the control group (P<0.05). There
was no significant difference in the effective rate between the two
groups (P>0.05) (Table II).
 | Table II.Analysis of clinical efficacy [n
(%)]. |
Table II.
Analysis of clinical efficacy [n
(%)].
| Clinical
efficacy | Control group
(n=108) | Observation group
(n=88) | χ2 | P-value |
|---|
| Markedly
effective | 49 (45.37) | 58 (65.91) | 8.252 | 0.004 |
| Effective | 36 (33.33) | 28 (31.82) | 0.051 | 0.822 |
| Ineffective | 23 (21.30) | 2 (2.27) | 57.843 | <0.001 |
| Total effective
rate | 85 (78.70) | 86 (97.73) | 57.843 | <0.001 |
Incidence of complications
In the control group, complications (abdominal
distension, nausea, itching of the skin) occurred in 7 cases. In
the observation group, complications (abdominal distension, nausea,
skin rashes, itching of the skin and transaminase elevation)
occurred in 11 cases, and disappeared after withdrawal. There was
no significant difference in the incidence of complications between
the two groups (P>0.05) (Table
III).
 | Table III.Analysis of the incidence of the
complications [n (%)]. |
Table III.
Analysis of the incidence of the
complications [n (%)].
| Complications | Control group
(n=108) | Observation group
(n=88) | χ2 | P-value |
|---|
| Abdominal
distension | 3 (2.78) | 2 (2.27) | 0.050 | 0.824 |
| Nausea | 2 (1.85) | 3 (3.41) | 0.473 | 0.492 |
| Chromatosis | 0 (0.00) | 2 (2.27) | Fisher | 0.200 |
| Itching of the
skin | 2 (1.85) | 1 (1.14) | 0.165 | 0.685 |
| Transaminase
elevation | 0 (0.00) | 3 (3.41) | Fisher | 0.088 |
| Total incidence
rate of adverse reactions | 7 (6.48) | 11 (12.50) | 2.106 | 0.147 |
Lung function
There was no significant difference in RR, FVC and
FEV1 between the two groups before treatment (P>0.05). After
treatment, RR decreased, whereas, FVC and FEV1 increased in both
groups (P<0.05), and RR in the observation group was lower than
that in the control group (P<0.05), FVC and FEV1 were higher
than those in control group (P<0.05) (Table IV).
 | Table IV.Detection of lung function. |
Table IV.
Detection of lung function.
| Lung function
index | Control group
(n=108) | Observation group
(n=88) | t | P-value |
|---|
| RR (time/min) |
| Before
treatment | 42.31±7.15 | 43.26±7.64 | 0.897 | 0.371 |
| After
treatment |
37.72±5.42a |
30.15±5.13a | 9.961 | <0.001 |
| FVC (%) |
| Before
treatment | 75.16±7.57 | 76.21±7.42 | 0.975 | 0.331 |
| After
treatment |
80.63±7.28a |
89.06±7.17a | 8.118 | <0.001 |
| FEV1 (%) |
| Before
treatment | 71.42±8.04 | 70.58±8.26 | 0.719 | 0.473 |
| After
treatment |
74.33±7.53a |
85.67±7.85a | 10.288 | <0.001 |
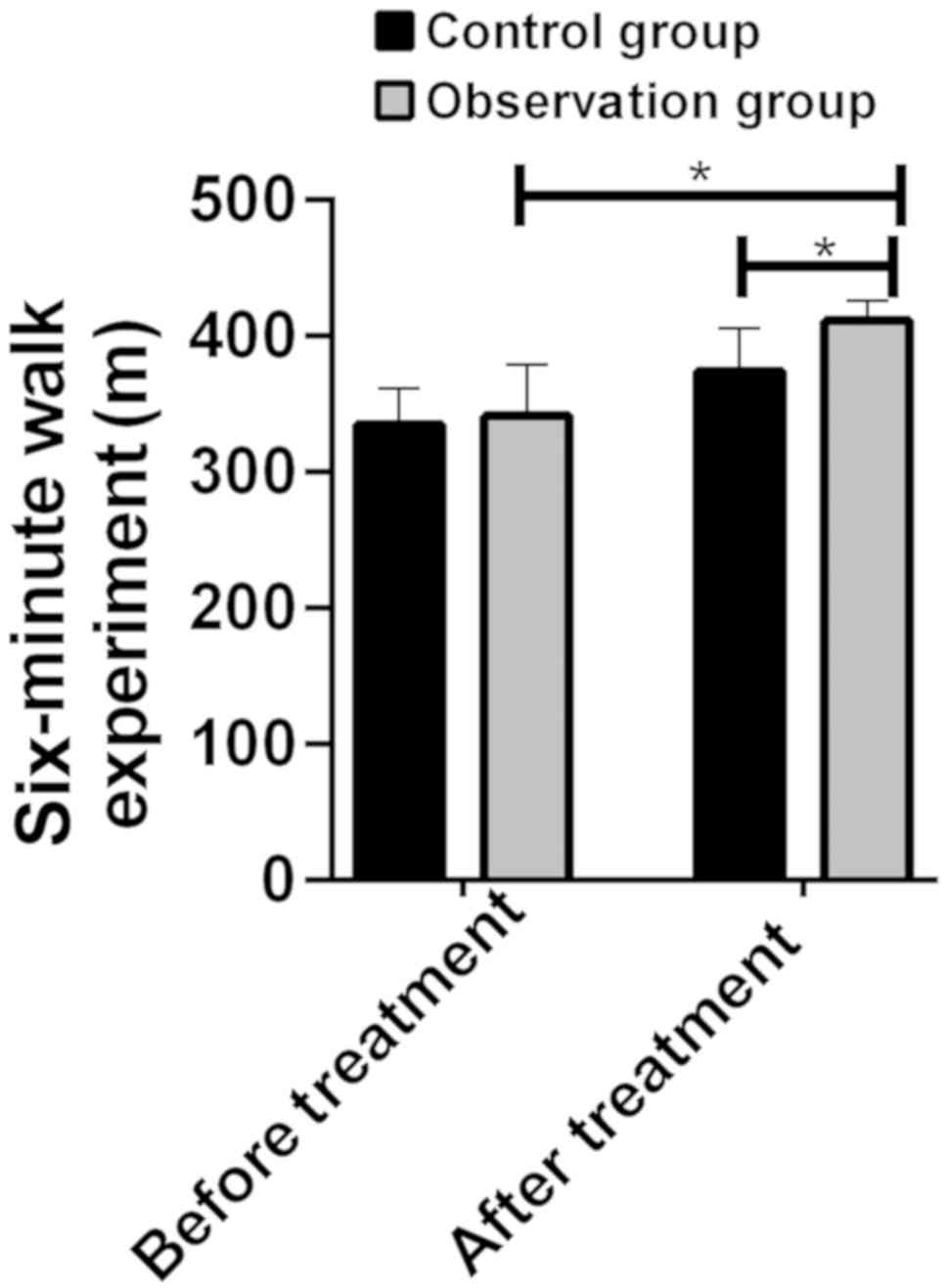
6-min walk experiment
There was no significant difference in the results
of 6-min walking test between the two groups before treatment
(P>0.05), but the 6-min walking distance of the two groups
increased after treatment (P<0.05), and the 6-min walking
distance in the observation group was longer than that in the
control group (P<0.05) (Fig.
1).
Changes of IL-6 and TNF-α expression
levels
There was no significant difference in serum IL-6
and TNF-α levels between the two groups before treatment
(P>0.05). After treatment, the levels of IL-6 and TNF-α in the
two groups decreased (P<0.05), and the IL-6 and TNF-α levels in
the observation group after treatment were significantly lower than
those in the control group (P<0.05) (Table V).
 | Table V.Changes of IL-6 and TNF-α expression
levels. |
Table V.
Changes of IL-6 and TNF-α expression
levels.
| Expression
levels | Control group
(n=108) | Observation group
(n=88) | t | P-value |
|---|
| IL-6 (ng/ml) |
| Before
treatment | 15.39±6.83 | 15.97±8.14 | 0.542 | 0.588 |
| After
treatment |
13.32±5.35a |
10.01±5.13a | 4.388 | <0.001 |
| TNF-α (ng/ml) |
| Before
treatment | 21.59±5.59 | 20.22±9.13 | 1.291 | 0.198 |
| After
treatment |
19.75±6.34a |
17.11±5.02a | 3.178 | 0.002 |
Relationship between IL-6, TNF-α and
the clinical therapeutic effect
According to the effect of clinical treatment, the
patients were re-divided into two groups. The patients who had
significant therapeutic effect and the effective treatment were
treated as the effective group, and those who had no effect were
treated as the ineffective group. The results of ROC curve analysis
showed that IL-6 evaluation of effective and ineffective AUC,
critical value, sensitivity and specificity were 0.743, 13.72
ng/ml, 52.42 and 65.38%, respectively. The AUC, critical value,
sensitivity and specificity of TNF-α were 0.723, 17.74 ng/ml, 92.00
and 49.71%, respectively (Table VI
and Fig. 2).
 | Figure 2.Clinical value of IL-6 and TNF-α in
the treatment of silicosis. IL-6 evaluation of effective and
ineffective AUC, critical value, sensitivity and specificity were
0.743, 13.72 ng/ml, 52.42 and 65.38%, respectively. The AUC,
critical value, sensitivity and specificity of TNF-α were 0.723,
17.74 ng/ml, 92.00 and 49.71%, respectively. |
 | Table VI.Relationship between IL-6, TNF-α and
the clinical therapeutic effect. |
Table VI.
Relationship between IL-6, TNF-α and
the clinical therapeutic effect.
| ROC curve
index | IL-6 | TNF-α |
|---|
| AUC | 0.743 | 0.723 |
| 95% Cl | 0.635–0.850 | 0.637–0.809 |
| Cut-off | 13.72 ng/ml | 17.74 ng/ml |
| Sensitivity
(%) | 52.42 | 92.00 |
| Specificity
(%) | 65.38 | 49.71 |
Discussion
Silicosis still has a high incidence in many
countries in the world, including China, and South Africa. The main
pathogenesis of silicosis is the humoral immune excess caused by
macrophages, lymphocytes and their cytokines, as well as cellular
immunosuppression, which leads to immune dysfunction or imbalance.
Inflammatory reaction and pulmonary fibrosis are important
pathological changes and cause respiratory impairment (12). At present, there is no cure method
for silicosis. It is of great significance for clinical treatment
of silicosis to find new drugs or therapeutic regimens.
The anti-inflammatory effect of tetrandrine has been
proven. Seow et al (13)
reported that tetrandrine can inhibit the uptake of deoxyglucose by
neutrophils and monocytes and inhibit the adhesion of inflammatory
cells. Mazurek et al (14)
demonstrated that tetrandrine could inhibit the random movement,
chemotaxis and phagocytosis of human neutrophils in vitro.
It can inhibit the shunt activity of hexose-monophosphate and the
production of hydrogen peroxide and superoxide anion, so as to
exert anti-inflammatory effects such as anti-phagocytosis, and
anti-oxidation. Tetrandrine also plays an anti-fibrotic role
through calcium channel block. In the past few decades, tetrandrine
has been widely used in the clinical treatment of silicosis, and
the combination of drugs has a more obvious inhibitory effect on
the formation of fibrosis (15). But
there is no single drug or treatment that can completely cure
silicosis so far. Acetylcysteine is the precursor of glutathione,
which can supplement the content of glutathione in the body and
enhance the antioxidant effect of the organism. Acetylcysteine also
has an antioxidant effect that protects biological macromolecules
by reducing oxidized disulfide bonds to eliminate hydroxyl radicals
and hydrogen peroxide, and inhibits the proliferation of
fibroblasts and the formation of extracellular matrix to play an
anti-fibrotic role (16,17). Acetylcysteine has been used in the
treatment of pulmonary fibrosis in the past, such as the treatment
of idiopathic pulmonary fibrosis with pirfenidone, and has achieved
a good clinical therapeutic effect (18). However, few studies have been
reported on the application of acetylcysteine in silicosis,
especially in clinical studies.
The clinical efficacy of acetylcysteine combined
with tetrandrine tablets in the treatment of silicosis was studied
prospectively. There was no statistical difference in sex, age and
other general data between the two groups, suggesting that the two
groups of patients included in this study were comparable. We first
analyzed the therapeutic effects of the two groups of patients.
Compared with the conventional treatment, the total effective rate
and markedly effective rate of treatment for silicosis patients
were significantly increased with the addition of acetylcysteine
and tetrandrine. These results suggest that acetylcysteine combined
with tetrandrine can effectively improve the therapeutic effect of
silicosis. Some indexes of pulmonary function and the results of
6-min walking test also suggested the positive effect of
acetylcysteine and tetrandrine. But we calculated the incidence of
adverse reactions in the two groups of patients to avoid more
adverse reactions caused by increased use of drugs. The results
showed that there was no significant difference in the incidence of
total adverse reactions and single adverse reaction between the two
groups, which suggested that increasing the use of tetrandrine and
acetylcysteine was still safe. But the patients in the observation
group had two new adverse reactions, rash and elevation of
transaminase. Due to the long period of clinical treatment of
silicosis, it is necessary to remind patients to pay close
attention to the changes in the course of treatment, and to go to
the hospital for regularly review. At present, there are few
studies on the combination of acetylcysteine and tetrandrine in the
treatment of silicosis. Some studies reported that, compared to
routine treatment, tetrandrine combined with acetylcysteine can
effectively alleviate clinical symptoms such as cough and dyspnea,
improve pulmonary function, reduce oxidative stress levels and
limit the progression of fibrosis in silicosis patients, which also
confirms the accuracy of our results.
This study did not analyze the changes of oxidative
stress levels in the two groups of patients, but analyzed the
changes of IL-6 and TNF-α and its relationship with therapeutic
effect. IL-6 and TNF-α are two factors closely related to
inflammatory reaction, and their elevated levels may indicate an
increase in the degree of inflammatory response in the body
(19,20). The results of this study showed that
the degree of improvement of inflammatory reaction in the
observation group was significantly better than that in the control
group. The results of ROC analysis suggest that the levels of IL-6
and TNF-α have a good diagnostic value in the clinical treatment of
silicosis. The AUC of effective and ineffective differential
therapy were 0.743 and 0.723, respectively. These results suggest
that the detection of IL-6 and TNF-α may reduce the use of X-ray
and other imaging methods to a certain extent, and reduce the cost
of treatment.
This study also has some shortcomings. The
prospective study inevitably has Hawthorne effect. In addition,
this study did not carry out a long follow-up, so the final outcome
of the patient cannot be judged. We will continue to track patients
and evaluate their long-term outcomes.
In conclusion, tetrandrine combined with
acetylcysteine can effectively improve the clinical therapeutic
effect of silicosis, alleviate the degree of inflammation and
improve the levels of IL-6 and TNF-α in peripheral blood, which is
valuable in judging the clinical therapeutic effect of
silicosis.
Acknowledgements
Not applicable.
Funding
This study was supported by Qingdao Medical
Scientific Research Guidance Plan for 2014 (no. 2014-WJZD076).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JS and PS analyzed and interpreted the patient
general data. YW performed ELISA. YC was responsible for analysis
of observation indicators. JS wrote the manuscript. All the authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Qingdao Central Hospital (Qingdao, China). Patients who
participated in this study, had complete clinical data. Patients
and/or their families signed an informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee S, Hayashi H, Mastuzaki H,
Kumagai-Takei N and Otsuki T: Silicosis and autoimmunity. Curr Opin
Allergy Clin Immunol. 17:78–84. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yew WW, Leung CC, Chang KC, Zhang Y and
Chan DP: Can treatment outcomes of latent TB infection and TB in
silicosis be improved? J Thorac Dis. 11:E8–E10. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bang KM, Mazurek JM, Wood JM, White GE,
Hendricks SA and Weston A; Centers for Disease Control and
Prevention (CDC), : Silicosis mortality trends and new exposures to
respirable crystalline silica - United States, 2001–2010. MMWR Morb
Mortal Wkly Rep. 64:117–120. 2015.PubMed/NCBI
|
|
4
|
Brown T, Darnton A, Fortunato L and
Rushton L; British Occupational Cancer Burden Study Group, :
Therapeutic effects of adipose-tissue-derived mesenchymal stromal
cells and their extracellular vesicles in experimental silicosis.
Br J Cancer. 107:S56–S70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Field RW and Withers BL: Occupational and
environmental causes of lung cancer. Clin Chest Med. 33:681–703.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bhagya N and Chandrashekar KR: Tetrandrine
- a molecule of wide bioactivity. Phytochemistry. 125:5–13. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhao YZ, Kim JY, Park EJ, Lee SH, Woo SW,
Ko G and Sohn DH: Tetrandrine induces apoptosis in hepatic stellate
cells. Phytother Res. 18:306–309. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang L, He YL, Li QZ, Hao XH, Zhang ZF,
Yuan JX, Bai YP, Jin YL, Liu N, et al: N-acetylcysteine alleviated
silica-induced lung fibrosis in rats by down-regulation of ROS and
mitochondrial apoptosis signaling. Toxicol Mech Methods.
24:212–219. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen Z, Zhao L, Zhao F, Yang G and Wang
JJ: Tetrandrine suppresses lung cancer growth and induces
apoptosis, potentially via the VEGF/HIF-1α/ICAM-1 signaling
pathway. Oncol Lett. 15:7433–7437. 2018.PubMed/NCBI
|
|
10
|
Xiao Y, Xia H, Zhu L, Li X, Chen R, Yin X,
Jiang Z, Feng L, Chen J, et al: Study on the therapeutic effects of
tetrandrine combined with N-acetylcysteine on experimental
silicosis of rats. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi.
33:519–522. 2015.PubMed/NCBI
|
|
11
|
Zhou Z: Understanding the administrative
regulation on occupational health and trend in China. J Occup
Health. 60:126–131. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Maeda M, Nishimura Y, Kumagai N, Hayashi
H, Hatayama T, Katoh M, Miyahara N, Yamamoto S, Hirastuka J, et al:
Dysregulation of the immune system caused by silica and asbestos. J
Immunotoxicol. 7:268–278. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Seow WK, Si-Ying L and Thong YH:
Inhibitory effects of tetrandrine on human neutrophil and monocyte
adherence. Immunol Lett. 13:83–88. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mazurek JM, Wood JM, Schleiff PL and
Weissman DN: Surveillance for silicosis deaths among persons aged
15–44 years - United States, 1999–2015. MMWR Morb Mortal Wkly Rep.
66:747–752. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xie QM, Tang HF, Chen JQ and Bian RL:
Pharmacological actions of tetrandrine in inflammatory pulmonary
diseases. Acta Pharmacol Sin. 23:1107–1113. 2002.PubMed/NCBI
|
|
16
|
Monti D, Sotgia F, Whitaker-Menezes D,
Tuluc M, Birbe R, Berger A, Lazar M, Cotzia P, Draganova-Tacheva R,
et al: Pilot study demonstrating metabolic and anti-proliferative
effects of in vivo anti-oxidant supplementation with
N-acetylcysteine in Breast Cancer. Semin Oncol. 44:226–232. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mazurek JM, Schleiff PL, Wood JM,
Hendricks SA and Weston A; Centers for Disease Control and
Prevention (CDC), : Notes from the Field: Update: Silicosis
Mortality - United States, 1999–2013. MMWR Morb Mortal Wkly Rep.
64:653–654. 2015.PubMed/NCBI
|
|
18
|
Sakamoto S, Muramatsu Y, Satoh K, Ishida
F, Kikuchi N, Sano G, Sugino K, Isobe K, Takai Y, et al:
Effectiveness of combined therapy with pirfenidone and inhaled
N-acetylcysteine for advanced idiopathic pulmonary fibrosis: A
case-control study. Respirology. 20:445–452. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Del Giudice M and Gangestad S W:
Rethinking IL-6 and CRP: Why they are more than inflammatory
biomarkers, and why it matters. Brain Behav Immun. 70:61–75. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Charrad R, Berraïes A, Hamdi B, Ammar J,
Hamzaoui K and Hamzaoui A: Anti-inflammatory activity of IL-37 in
asthmatic children: Correlation with inflammatory cytokines TNF-α,
IL-β, IL-6 and IL-17A. Immunobiology. 221:182–187. 2015. View Article : Google Scholar : PubMed/NCBI
|