Introduction
Lumbar disc herniation (LDH) is a common clinical
degenerative discogenic disease, with an incidence rate of 10–20%
(1). The condition is
age-associated, which is closely associated with life and work
habits, including bad posture (1).
Of the patients with LDH, ~70–85% suffer from lower back pain and
unilateral leg neurological symptoms (2,3).
Clinically, minimally invasive techniques and open surgery are
performed for patients with LDH following failure of conservative
treatments. Patients diagnosed with LDH with no severe neurologic
symptoms, including cauda equina syndrome, pareses or other
syndromes that require acute surgical intervention, are suitable
candidates for minimally invasive techniques (4). Targeted percutaneous laser disc
decompression (T-PLDD) is one such minimally invasive technique
that has been used to treat patients with LDH and is cheaper than
surgery (4,5). In T-PLDD, energy produced by a laser
fired through an optical fiber vaporizes nucleus pulposus tissue to
decrease intradisc pressure, thus causing the extruded nucleus
pulposus to retract (4,5).
By 2002, ~35,000 PLDDs were performed worldwide and
were gradually replaced subsequently due to its high complication
rates (4,6). For the conventional optical fiber
(Con), the refractive index of the outer core is smaller than that
of the fiber core, so the energy released radially is similar to
that released from a flashlight. This type of radial energy can
lead to the vaporization of the nucleus pulposus in one direction,
but the surrounding nucleus pulposus is less affected. Therefore,
to sufficiently vaporize the nucleus pulposus and to reduce the
intradisc pressure, the laser energy required is too high, which
may seriously destroy the structure of the nucleus pulposus and
accelerate the degeneration of the intervertebral disc (5). A large amount of energy may easily
damage the nerve and lead to a number of complications, including
aggravated lumbago, endplate inflammation, spinal canal stenosis
and even disability (4,6–8).
Therefore, in 2010, the Con was improved so that the
energy could gather around the tip of the optical fiber when
working (unpublished data). This was applied in clinical practice
for the treatment of LDH. The present study, to the best of our
knowledge, was the first to report the differences between Con and
the modified optical fiber (Mod), and verify its use via animal
studies. Additionally, a retrospective study was performed to
analyze the effects of using Mod in T-PLDD in patients with lumbar
disc herniation.
Materials and methods
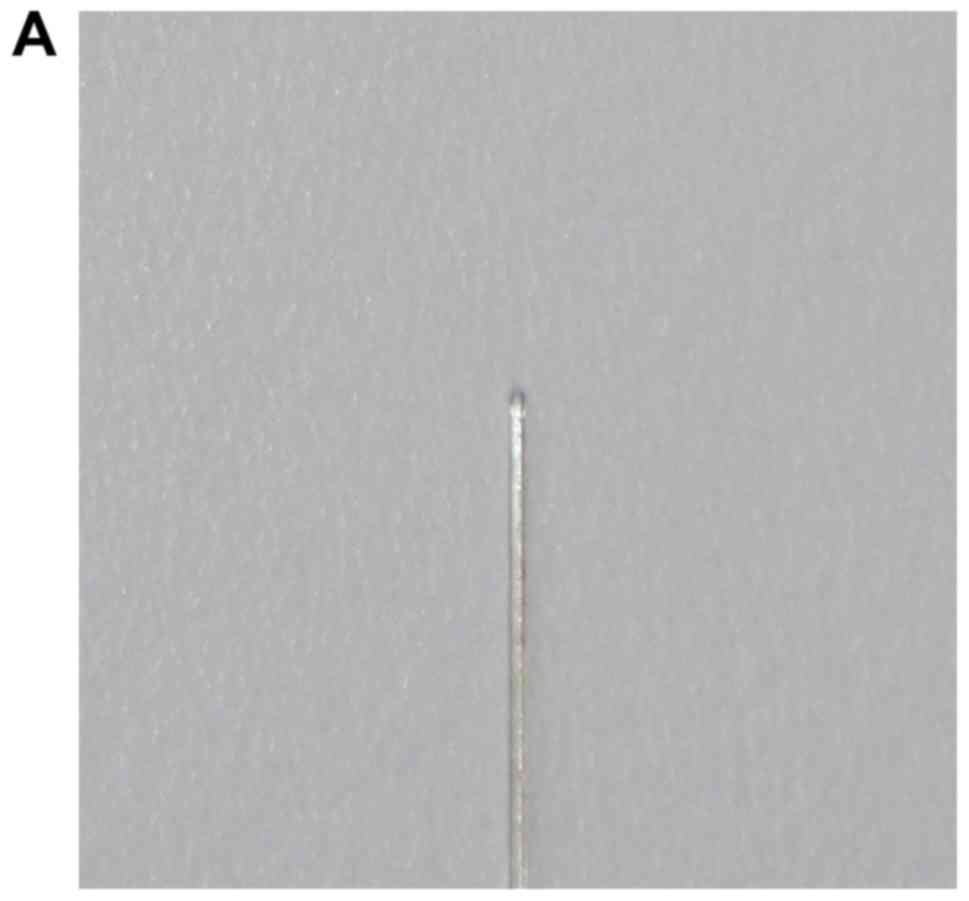
Con
The Con used in the present study was a transparent
glass fiber that consisted of a fiber core, silicone resin and
nylon bushing (from inside to outside; Fig. 1A and C).
Mod
The composition of the Mod was consistent with that
of the Con. However, wells in the Mod optical fiber were created
irregularly at 2.5 mm from the tip of the optical fiber (Fig. 1B and D).
Animal study
A total of 60 spinal motor units supplied by the
Affiliated Hospital of Qingdao University, consisting of
intervertebral discs, two adjacent vertebral bodies, facet joints
and intervertebral ligaments, were obtained from 8 mature male
domestic pigs (age, 18 months; weight, 150–170 kg). The pigs were
kept at a 12 h light/dark cycle and received water and food ad
libitum at room temperature in a 21% O2 + 78%
N2 atmosphere. The 60 units were randomly divided into
two groups: The Con and Mod groups. Each group included three
subgroups according to the different energies (200, 400 and 600 J;
n=10). All protocols were approved by the Institutional Ethics
Committee of the Affiliated Hospital of Qingdao University
(Qingdao, China).
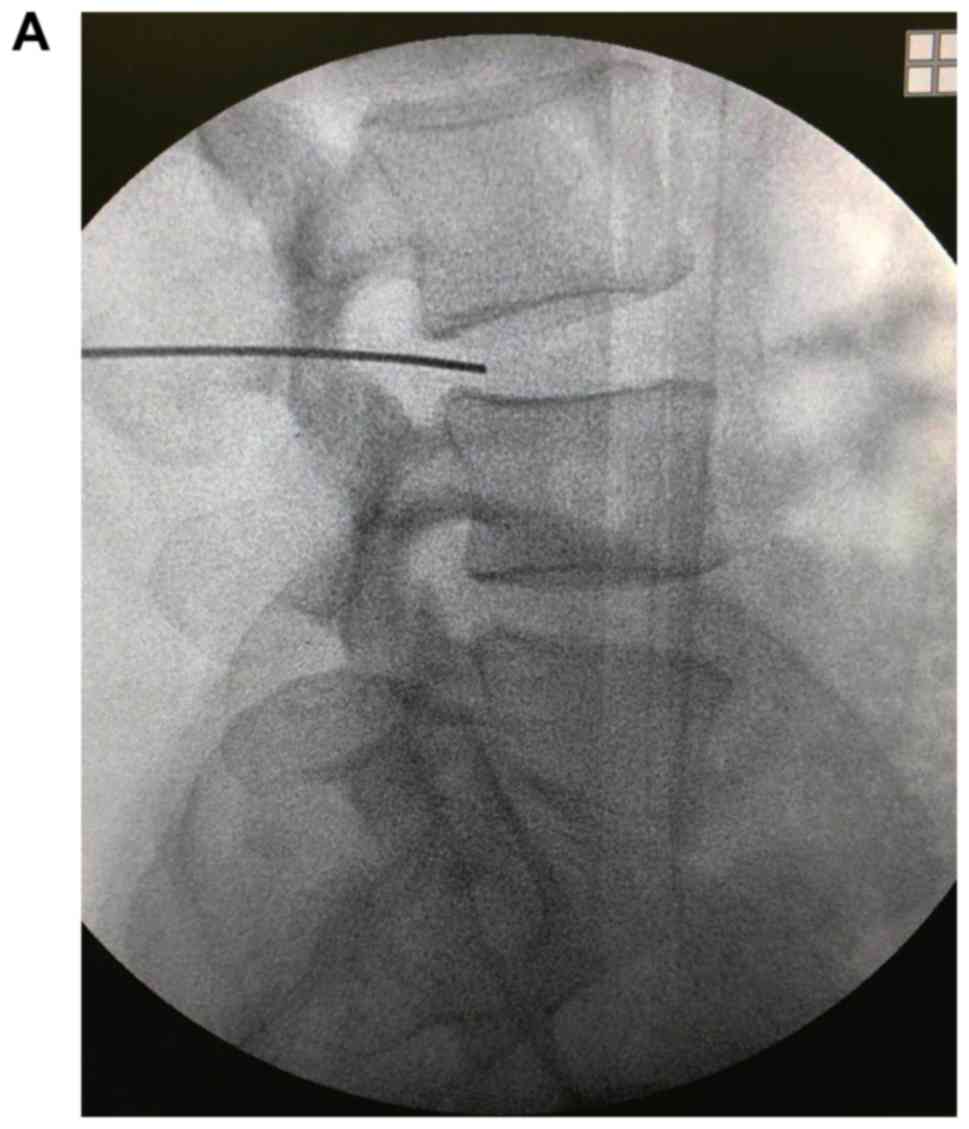
Under the guidance of the C-arm X-ray device
(Posvet-100HF; Poskom Co., Ltd.), the needle paralleling the two
adjacent vertebral bodies was inserted from the posterolateral disc
and passed through the fibrous ring to the center of the nucleus
pulposus. After confirmation of the needle position, the needle
core was removed and the optical fiber was inserted (Con in the Con
group and Mod in the Mod group). Subsequently, the parameters of
the laser apparatus (1064 nm Nd:YAG pulsed laser therapeutic
apparatus; Beijing Dongtai Jiguang Technology Co., Ltd) were set
(laser pulse width, 0.4 msec; duration of the laser each use, 1
sec; interval time, 1 sec; laser power, 13.5 W; laser pulse
repetition frequency, 15 Hz). The total energy was set in different
groups. After a total energy of laser ablation (200, 400 or 600 J)
was delivered, the procedure was finished. The length and width of
the vaporization cavity were measured using a ruler.
Patients
The database of The Affiliated Hospital of Qingdao
University (Qingdao, China) was searched to identify the patients
who were hospitalized in the Department of Pain Management between
June 2011 and May 2012 and received T-PLDD using the Mod. Patients
without complete follow-up who lacked any information were excluded
from the present study. All 58 patients, the American Society of
Anesthesiologists Grade (5) I–III,
underwent T-PLDD successfully. There were 26 males and 32 females
with an average age of 52.1±12.9 years (age range, 21–75
years).
The patients were diagnosed with
LDH
The following exclusion criteria was applied:
Serious heart, lung or kidney diseases, coagulation abnormalities,
communication disorders, local or systemic infections, allergies to
anesthetics or steroids, previous surgery for LDH, percutaneous
endoscopic lumbar discectomy, open lumbar surgery, spinal fracture
or tumor, serious disc calcification or pregnancy. The patients
provided written informed consent (including consent for
publication) to receive T-PLDD. Additionally, patients with free
herniated disc fragments were not suitable for PLDD.
The present study was retrospective in
nature
The information in the database included the
following: General characteristics, modified MacNab grade (9), 10-point numeric rating score (NRS, 0
for no pain and 10 for unbearable pain) for pain (4), oswestry disability index (ODI)
(10), pain rating index (PRI) of
short-form McGill pain questionnaire (11), 12-item Short Form Health Survey
(SF-12) (6), surgery duration, laser
energy, disc height and T2 values according to MRI scans (General
Electric Company), hospital days, complications and analgesics
intake.
Statistical analysis
In the animal study (three experimental repetitions
independently), the T2 values of the nucleus pulposus and the
length and width of the vaporization cavity were presented as the
mean ± standard deviation. These quantitative data were compared
using one-way ANOVA followed by a Least Significant Difference
t-test was used.
In the clinical study, the quantitative data,
including the NRS, ODI, PRI, SF-12, disc height and T2 values were
compared using one-way ANOVA. The count data, including the
modified MacNab grade, complications and analgesic intake, were
presented as numbers and percentages and were compared using the
χ2 test, Fisher's exact test or R*C χ2 test.
Subsequently, to observe the effect of age on prognosis following
surgery, the data were grouped by age and a Student's t-test,
repeated data of ANOVA, χ2 test, Fisher's exact test or
R*C χ2 test were used. P<0.05 was considered to
indicate a statistically significant difference. SPSS (v20.0; IBM
Corp.) was used to perform statistical analysis.
Results
Vaporization cavity of nucleus
pulposus in the animal study
Postoperatively, the length and width of the
vaporization cavity in the Con 400 group (0.73±0.09 cm; 0.32±0.08
cm) were greater than those of the Con 200 group (0.36±0.07 cm;
0.17±0.07 cm). Additionally, the length and width of the
vaporization cavity in the Con 600 group (1.08±0.14 cm; 0.69±0.14
cm) were higher than those in the Con 400 group (P<0.05;
Fig. 2A-C). The length and width of
the vaporization cavity in the Mod 400 group (0.62±0.06 cm;
0.51±0.07 cm) and Mod 600 group (0.69±0.10 cm; 0.56±0.07 cm) were
increased compared with those in the Mod 200 group (0.39±0.07 cm;
0.30±0.07 cm; P<0.05); however, there were no significant
differences identified between the Mod 400 and Mod 600 groups
(Fig. 2D-F). Additionally, the
length of the vaporization cavity in the Mod 400 and Mod 600 groups
were lower than those in the Con 400 and Con 600 groups
(P<0.05); however, there was no significant difference
identified between the Mod 200 and Con 200 groups. The width of the
vaporization cavity in the Mod 200 and Mod 400 groups was higher
than that in the Con 200 and Con 400 groups (P<0.05), whereas
that in the Mod 600 group was lower than that in the Con 600 group
(P<0.05; Fig. 2G).
Patient characteristics
All patients received drugs and/or physiotherapy,
including but not limited to polarized light and ultrasonic drug
penetration therapy or epidural block therapy without any previous
spinal surgery at the same disc level. Among the patients, 28 and
30 had L4/5 and L5/S1 levels of disc herniation, respectively, and
31 patients had left leg pain, whereas 27 patients had right leg
pain. The American Society of Anesthesiologists Grade (5) grades of I, II and III were attributed
to 17, 31 and 10 patients, respectively. The average duration of
pain was 12.1±5.0 months (range, 2.7–21.8). Preoperatively, the
NRS, ODI, SF-12 and PRI of the patients were 7.86±1.15 (range,
6–10), 62.57±7.50% (range, 44.44–73.33%), 29.31±6.86 (range,
20.45–43.18) and 15.28±2.30 (range, 11–19), respectively (Table I).
 | Table I.Demographic data and clinical
characteristics. |
Table I.
Demographic data and clinical
characteristics.
| No. | Age, years | Sex | Weight, kg | Height, m | BMI,
kg/m2 | ASA | Disc herniation
level | Dominant leg
pain | Duration, months | NRS | ODI, % (score) | SF-12 (score) | PRI |
|---|
| 1 | 66 | M | 77 | 1.72 | 26.03 | II | L4-L5 | Left | 6.4 | 6 | 44.44 (20) | 43.18 (31) | 12 |
| 2 | 27 | F | 80 | 1.55 | 33.30 | I | L5-S1 | Right | 9.1 | 8 | 66.67 (30) | 38.64 (29) | 16 |
| 3 | 32 | M | 71 | 1.69 | 24.86 | I | L4-L5 | Left | 11.3 | 7 | 62.22 (28) | 34.09 (27) | 12 |
| 4 | 75 | M | 62 | 1.71 | 21.20 | III | L4-L5 | Left | 10.2 | 7 | 51.11 (23) | 31.82 (26) | 14 |
| 5 | 58 | F | 72 | 1.54 | 30.36 | II | L5-S1 | Right | 17.2 | 8 | 62.22 (28) | 27.27 (24) | 15 |
| 6 | 44 | M | 66 | 1.64 | 24.54 | II | L5-S1 | Right | 4.7 | 9 | 62.22 (28) | 25.00 (23) | 18 |
| 7 | 62 | F | 74 | 1.62 | 28.20 | II | L4-L5 | Right | 6.5 | 9 | 68.89 (31) | 22.73 (22) | 17 |
| 8 | 55 | F | 79 | 1.59 | 31.25 | III | L4-L5 | Right | 7.3 | 8 | 66.67 (30) | 27.27 (24) | 18 |
| 9 | 49 | F | 80 | 1.56 | 32.87 | II | L5-S1 | Left | 14.1 | 6 | 53.33 (24) | 40.91 (30) | 11 |
| 10 | 52 | M | 75 | 1.72 | 25.35 | I | L5-S1 | Right | 15.2 | 6 | 48.89 (22) | 38.64 (29) | 12 |
| 11 | 73 | F | 71 | 1.61 | 27.39 | III | L4-L5 | Left | 8.7 | 8 | 62.22 (28) | 25.00 (23) | 15 |
| 12 | 69 | F | 69 | 1.70 | 23.88 | II | L4-L5 | Left | 6.9 | 9 | 68.89 (31) | 22.73 (22) | 17 |
| 13 | 47 | F | 55 | 1.62 | 20.96 | III | L4-L5 | Left | 5.1 | 9 | 71.11 (32) | 22.73 (22) | 18 |
| 14 | 51 | M | 72 | 1.61 | 27.78 | I | L5-S1 | Left | 19.7 | 6 | 53.33 (24) | 43.18 (31) | 11 |
| 15 | 29 | M | 78 | 1.77 | 24.90 | I | L4-L5 | Right | 8.4 | 9 | 68.89 (31) | 27.27 (24) | 17 |
| 16 | 33 | M | 51 | 1.74 | 16.85 | I | L5-S1 | Right | 18.2 | 10 | 73.33 (33) | 22.73 (22) | 18 |
| 17 | 47 | F | 63 | 1.61 | 24.30 | II | L4-L5 | Left | 14.2 | 7 | 55.56 (25) | 38.64 (29) | 15 |
| 18 | 50 | F | 83 | 1.59 | 32.83 | III | L5-S1 | Right | 9.7 | 9 | 66.67 (30) | 27.27 (24) | 16 |
| 19 | 52 | F | 72 | 1.55 | 29.97 | II | L5-S1 | Left | 20.1 | 6 | 51.11 (23) | 40.91 (30) | 11 |
| 20 | 66 | F | 59 | 1.50 | 26.22 | III | L5-S1 | Left | 13.7 | 7 | 55.56 (25) | 36.36 (28) | 14 |
| 21 | 62 | F | 67 | 1.63 | 25.22 | II | L4-L5 | Right | 21.3 | 6 | 46.67 (21) | 43.18 (31) | 14 |
| 22 | 53 | M | 71 | 1.63 | 26.72 | I | L4-L5 | Right | 17.5 | 8 | 64.44 (29) | 27.27 (24) | 15 |
| 23 | 58 | F | 59 | 1.62 | 22.48 | II | L5-S1 | Right | 14.1 | 7 | 62.22 (28) | 29.55 (25) | 13 |
| 24 | 67 | F | 78 | 1.52 | 33.76 | II | L5-S1 | Left | 7.9 | 8 | 66.67 (30) | 25.00 (23) | 16 |
| 25 | 31 | F | 74 | 1.55 | 30.80 | I | L5-S1 | Left | 7.3 | 8 | 64.44 (29) | 22.73 (22) | 19 |
| 26 | 59 | F | 58 | 1.61 | 22.38 | II | L5-S1 | Left | 5.7 | 8 | 68.89 (31) | 25.00 (23) | 18 |
| 27 | 44 | M | 90 | 1.69 | 31.51 | II | L5-S1 | Left | 13.3 | 7 | 62.22 (28) | 25.00 (23) | 18 |
| 28 | 48 | M | 82 | 1.82 | 24.76 | II | L5-S1 | Right | 8.9 | 8 | 64.44 (29) | 20.45 (21) | 17 |
| 29 | 50 | F | 69 | 1.65 | 25.34 | II | L5-S1 | Right | 16.1 | 8 | 66.67 (30) | 25.00 (23) | 14 |
| 30 | 46 | F | 62 | 1.66 | 22.50 | II | L5-S1 | Left | 14.2 | 9 | 71.11 (32) | 22.73 (22) | 15 |
| 31 | 43 | F | 61 | 1.59 | 24.13 | I | L4-L5 | Left | 17.2 | 8 | 64.44 (29) | 27.27 (24) | 16 |
| 32 | 51 | M | 81 | 1.63 | 30.49 | II | L4-L5 | Left | 20.3 | 6 | 51.11 (23) | 38.64 (29) | 11 |
| 33 | 55 | M | 62 | 1.59 | 24.52 | I | L5-S1 | Right | 18.7 | 7 | 46.67 (21) | 40.91 (30) | 11 |
| 34 | 39 | M | 54 | 1.72 | 18.25 | I | L5-S1 | Left | 12.7 | 9 | 66.67 (30) | 22.73 (22) | 15 |
| 35 | 49 | F | 74 | 1.61 | 28.55 | III | L4-L5 | Right | 15.1 | 6 | 48.89 (22) | 43.18 (31) | 13 |
| 36 | 52 | M | 76 | 1.77 | 24.26 | I | L4-L5 | Left | 11.9 | 9 | 71.11 (32) | 22.73 (22) | 18 |
| 37 | 71 | M | 69 | 1.63 | 25.97 | II | L4-L5 | Right | 17.1 | 8 | 64.44 (29) | 25.00 (23) | 18 |
| 38 | 58 | M | 51 | 1.69 | 17.86 | II | L5-S1 | Left | 15.6 | 8 | 66.67 (30) | 25.00 (23) | 16 |
| 39 | 48 | F | 79 | 1.59 | 31.25 | II | L4-L5 | Left | 13.9 | 9 | 66.67 (30) | 20.45 (21) | 17 |
| 40 | 61 | F | 61 | 1.62 | 23.24 | III | L4-L5 | Right | 9.6 | 9 | 71.11 (32) | 22.73 (22) | 17 |
| 41 | 66 | M | 77 | 1.53 | 32.89 | II | L5-S1 | Right | 8.5 | 8 | 64.44 (29) | 22.73 (22) | 17 |
| 42 | 53 | M | 68 | 1.67 | 24.38 | II | L4-L5 | Right | 8.1 | 9 | 68.89 (31) | 25.00 (23) | 18 |
| 43 | 40 | F | 51 | 1.60 | 19.92 | II | L5-S1 | Left | 16.5 | 7 | 60.00 (27) | 34.09 (27) | 14 |
| 44 | 45 | F | 63 | 1.58 | 25.24 | II | L4-L5 | Left | 16.1 | 7 | 62.22 (28) | 31.82 (26) | 15 |
| 45 | 27 | F | 59 | 1.70 | 20.42 | I | L5-S1 | Left | 14.1 | 8 | 64.44 (29) | 31.82 (26) | 16 |
| 46 | 21 | F | 53 | 1.66 | 19.23 | I | L4-L5 | Right | 13.7 | 6 | 46.67 (21) | 38.64 (29) | 12 |
| 47 | 39 | F | 78 | 1.62 | 29.72 | I | L4-L5 | Left | 7.2 | 9 | 68.89 (31) | 27.27 (24) | 16 |
| 48 | 57 | M | 83 | 1.75 | 27.10 | II | L4-L5 | Right | 11.1 | 7 | 64.44 (29) | 34.09 (27) | 13 |
| 49 | 59 | M | 73 | 1.82 | 22.04 | II | L4-L5 | Right | 3.8 | 10 | 73.33 (33) | 25.00 (23) | 17 |
| 50 | 63 | M | 82 | 1.69 | 28.71 | II | L5-S1 | Left | 6.7 | 8 | 66.67 (30) | 22.73 (22) | 18 |
| 51 | 75 | M | 71 | 1.55 | 29.55 | III | L5-S1 | Left | 14.9 | 9 | 64.44 (29) | 29.55 (25) | 18 |
| 52 | 46 | F | 66 | 1.60 | 25.78 | II | L5-S1 | Right | 13.9 | 8 | 68.89 (31) | 27.27 (24) | 13 |
| 53 | 72 | F | 61 | 1.57 | 24.75 | II | L4-L5 | Left | 2.7 | 10 | 68.89 (31) | 22.73 (22) | 16 |
| 54 | 69 | M | 50 | 1.78 | 15.78 | II | L4-L5 | Right | 5.6 | 9 | 64.44 (29) | 27.27 (24) | 15 |
| 55 | 66 | M | 79 | 1.69 | 27.66 | II | L5-S1 | Right | 7.9 | 9 | 68.89 (31) | 25.00 (23) | 18 |
| 56 | 52 | F | 72 | 1.62 | 27.44 | III | L5-S1 | Right | 19.1 | 7 | 60.00 (27) | 29.55 (25) | 14 |
| 57 | 41 | M | 65 | 1.73 | 21.72 | I | L4-L5 | Left | 21.8 | 7 | 62.22 (28) | 29.55 (25) | 13 |
| 58 | 52 | F | 70 | 1.60 | 27.34 | I | L5-S1 | Left | 7.6 | 8 | 62.22 (28) | 25.00 (23) | 15 |
Surgery-associated results and
hospital stay
Under the guidance of radiation, the needle reached
one-fifth of the distance into the intervertebral space at the
lateral position (Fig. 3A) and at
the lateral border of the vertebral body in the anteroposterior
position (Fig. 3B). The surgery time
was 58.9±6.6 min and the average length of hospital stay was
3.34±0.66 days. There were 12 patients who received 150 J, 19
patients who received 200 J, nine patients who received 250 J and
18 patients who received 300 J. No serious complications, including
nerve injury and infection, occurred in any of the patients;
however, there was one case of hematoma, which resolved within 7
days. There were 19 patients with pain who received Celebrex (200
mg/day) for 2 days (Table II).
 | Table II.Surgery-associated results and
hospital stay. |
Table II.
Surgery-associated results and
hospital stay.
| Surgery time
(min) |
| Laser energy |
| Hospital stay,
days | Complications | Analgesic |
|---|
| 58.9±6.6 | 150 J (n) | 200 J (n) | 250 J (n) | 300 J (n) | 3.34±0.66 | Yes (n) | No (n) | Yes (n) | No (n) |
|
| 12 | 19 | 9 | 18 |
| 1 | 57 | 19 | 39 |
NRS, ODI, PRI and SF-12 in
patients
The NRS in the patients preoperatively was 7.86±1.15
and decreased significantly to 5.12±1.37 at 1 week postoperatively,
3.26±1.41 at 1 month, 1.64±0.97 at 3 months, 1.53±0.88 at 6 months,
1.50±0.86 at 12 months, 1.48±0.86 at 24 months and 1.48±0.86 at 36
months (P<0.05). Compared with the NRS at 1 week, the 1-month
score was decreased significantly and the 3-month score was lower
than the 1-month score (P<0.05). However, the NRS of patients at
3, 6, 12, 24 and 36 months postoperatively exhibited no significant
difference. A similar trend was revealed for the ODI, SF-12 and
PRI; however, those of patients at 6, 12, 24 and 36 months
post-surgery exhibited no significant difference (Table III).
 | Table III.Clinical outcomes of the patients in
terms of NRS, ODI, SF-12 and PRI. |
Table III.
Clinical outcomes of the patients in
terms of NRS, ODI, SF-12 and PRI.
| Variable | Baseline | 1 week | 1 month | 3 months | 6 months | 12 months | 24 months | 36 months |
|---|
| NRS | 7.86±1.15 |
5.12±1.37a |
3.26±1.41a,b |
1.64±0.97a–c |
1.53±0.88a–c |
1.50±0.86a–c |
1.48±0.86a–c |
1.48±0.86a–c |
| ODI (%) | 62.57±7.50 |
44.94±6.97a |
33.03±7.23a,b |
27.70±7.71a–c |
24.56±6.78a–d |
23.49±6.50a–d |
23.10±6.20a–d |
23.10±6.20a–d |
| SF-12 | 29.31±6.86 |
39.34±5.27a |
54.90±4.83a,b |
64.26±4.92a–c |
69.40±5.08a–d |
70.57±5.41a–d |
70.89±5.39a–d |
70.89±5.39a–d |
| PRI | 15.28±2.30 |
11.52±1.85a |
7.83±1.31a,b |
5.79±1.57a–c |
5.10±1.51a–d |
4.93±1.46a–d |
4.91±1.43a–d |
4.91±1.43a–d |
Modified MacNab
The clinical good-to-excellent rating at 1 week
post-surgery was 74.2%, which increased significantly to 82.8% at 1
month and to 94.8% at 3 months (P<0.05). The good-to-excellent
rating at 6 months reached 96.5% and was maintained until 36
months. However, no significant differences were identified among
the good-to-excellent ratings at 3, 6, 12, 24 and 36 months
(Table IV).
 | Table IV.Clinical outcomes in terms of
modified MacNab. |
Table IV.
Clinical outcomes in terms of
modified MacNab.
| MacNab | 1 week, n (%) | 1 month, n (%) | 3 months, n
(%) | 6 months, n
(%) | 12 months, n
(%) | 24 months, n
(%) | 36 months, n
(%) |
|---|
| Excellent | 27 (46.6) | 35 (60.4) | 48 (82.8) | 50 (86.2) | 51 (87.9) | 51 (87.9) | 51 (87.9) |
| Good | 16 (27.6) | 13 (22.4) | 7 (12.0) | 6 (10.3) | 5 (8.6) | 5 (8.6) | 5 (8.6) |
| Fair | 10 (17.2) | 7 (12.0) | 3 (5.2) | 2 (3.5) | 2 (3.5) | 2 (3.5) | 2 (3.5) |
| Poor | 5 (8.6) | 3 (5.2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Good to excellent
rate | 74.2% | 82.8%a | 94.8%a,b | 96.5%a,b | 96.5%a,b | 96.5%a,b | 96.5%a,b |
Alterations of intervertebral disc
height and T2 values after surgery
The intervertebral disc height postoperatively was
not identified to exhibit a significant difference compared with
the preoperative value (Table V).
The T2 value at 1-week postoperatively was 76±8, which was lower
than the preoperative value (156±11; P<0.05). However, the T2
value increased to 152±11 at 3 months and was maintained until 36
months, when it exhibited no significant difference compared with
the preoperative value (Table
V).
 | Table V.Disc height and T2 value according to
MRI. |
Table V.
Disc height and T2 value according to
MRI.
| Variable | Baseline | 1 week | 1 month | 3 months | 6 months | 12 months | 24 months | 36 months |
|---|
| Disc height,
mm | 12.3±1.0 | 12.2±1.0 | 12.2±0.9 | 12.4±1.1 | 12.2±0.9 | 12.2±1.0 | 12.1±1.0 | 12.2±1.1 |
| T2 value | 156±11 | 76±8a | 110±10a,b | 152±11b,c | 156±11b,c | 155±11b,c | 156±11b,c | 156±17b,c |
Age-associated results
To observe the effect of age on prognosis following
surgery, the patients were divided into two groups: The elderly
group (≥50 years of age) and the young group (<50 years of age).
There were 33 patients in the Elderly group (18 males and 15
females) and 25 patients in the Young group (eight males and 17
females). The characteristics of the two groups exhibited no
significant differences (Table
VI).
 | Table VI.Characteristics of patients in the
Elderly and Yong groups. |
Table VI.
Characteristics of patients in the
Elderly and Yong groups.
| Characteristic | Elderly group | Young group | P-value |
|---|
| Sex, n
(male/female) | 18/15 | 8/17 | 0.113 |
| ASA |
|
| 0.094 |
| I | 6 | 11 |
|
| II | 20 | 11 |
|
|
III | 7 | 3 |
|
| BMI,
kg/m2 | 26.13±3.89 | 25.38±4.86 | 0.519 |
| Disc herniation
level, n (L4-L5/L5-S1) | 17/16 | 11/14 | 0.606 |
| Dominant leg pain,
n (left/right) | 16/17 | 15/10 | 0.434 |
| Duration,
months | 11.7±5.5 | 12.7±4.2 | 0.471 |
| NRS | 7.82±1.19 | 7.92±1.12 | 0.741 |
| ODI, % | 61.82±8.15 | 63.56±6.57 | 0.387 |
| SF-12 | 29.48±7.04 | 63.56±6.57 | 0.834 |
| PRI | 15.21±2.42 | 15.36±2.18 | 0.811 |
| Operation time,
min | 58.15±6.20 | 59.84±7.15 | 0.340 |
| Hospital stay,
days | 3.48±0.91 | 3.32±0.69 | 0.452 |
There was no significant difference in the NRS at
different time points between the Young and Elderly groups. In the
Elderly group, the NRS at 6 months was lower than that at baseline,
1 week, 1 month and 3 months (P<0.05), whereas it was similar to
that at 12, 24 and 36 months. In the Young group, the NRS at 3
months was lower than that at baseline, 1 week and 1 month
(P<0.05), while it was similar to that at 6, 12, 24 and 36
months. The ODI at 12 months in the Elderly group was lower than
that at baseline, 1 week, and 1, 3 and 6 months (P<0.05), while
it was similar to that at 24 and 36 months. The ODI at 6 months in
the Young group was lower than that at baseline, 1 week, 1 month
and 3 months (P<0.05), while it was similar to that at 12, 24
and 36 months. The SF-12 results exhibited a similar trend compared
with ODI and the PRI results exhibited a similar trend compared
with the NRS (Table VII).
 | Table VII.NRS, ODI, SF-12 and PRI in the
Elderly and Young groups. |
Table VII.
NRS, ODI, SF-12 and PRI in the
Elderly and Young groups.
| Variable | Group | Baseline | 1 week | 1 month | 3 months | 6 months | 12 months | 24 months | 36 months |
|---|
| NRS | Elderly | 7.82±1.18 |
5.03±1.40a |
3.12±1.41a,b |
1.67±1.02a–c |
1.48±0.87a–d |
1.48±0.87a–d |
1.45±0.87a–d |
1.45±0.87a–d |
|
| Young | 7.92±1.12 |
5.24±1.33a |
3.44±1.42a,b |
1.60±0.91a–c |
1.60±0.91a–c |
1.52±0.87a–c |
1.52±0.87a–c |
1.52±0.87a–c |
| ODI, % | Elderly | 61.82±8.15 |
45.45±7.31a |
34.48±6.48a,b |
28.96±7.42a–c |
24.98±7.64a–d |
23.30±7.18a–e |
23.10±6.87a–e |
23.10±6.87a–e |
|
| Young | 63.56±6.57 |
44.27±6.57a |
31.11±7.83a,b |
26.84±8.70a–c |
24.00±5.56a–d |
23.73±5.62a–d |
23.11±5.33a–d |
23.11±5.33a–d |
| SF-12 | Elderly | 29.48±7.04 |
39.33±5.55a |
55.03±5.17a,b |
64.33±5.00a–c |
68.80±4.99a–d |
70.66±5.55a–e |
71.01±5.36a–e |
71.01±5.36a–e |
|
| Young | 29.09±6.75 |
39.36±4.98a |
54.73±4.45a,b |
64.18±4.92a–c |
70.18±5.18a–d |
70.45±5.33a–d |
70.73±5.54a–d |
70.73±5.54a–d |
| PRI | Elderly | 15.21±2.42 |
11.48±2.06a |
8.00±1.44a,b |
6.27±1.40a–c |
5.12±1.43a–d |
4.94±1.39a–d |
4.91±1.40a–d |
4.91±1.40a–d |
|
| Young | 15.36±2.18 |
11.56±1.58a |
7.60±1.12a,b |
5.16±1.57a–c |
5.08±1.63a–c |
4.92±1.58a–c |
4.92±1.50a–c |
4.92±1.50a–c |
Discussion
At present, T-PLDD has been replaced by other
minimally invasive techniques due to the increased rate of
complications (12). However, the
Con was modified by create wells irregularly at the tip to decrease
the complication rate. It was used in the clinical setting for the
treatment of LDH to determine the curative effects, which were
evaluated in a retrospective study.
The Mod was based on the radiofrequency electric
knife. Following modification, energy is released so as to be
turned into emission around the tip, and the laser energy is
concentrated at the local area. When the radiofrequency is
operational, the energy gathers in the tip of the radiofrequency
electric knife and only acts on the tissues located around the tip,
as indicated in the current study. Therefore, the traditional
optical fiber was improved to make its energy gather at the top of
the fiber. First, an animal study was performed to observe the
effects of the Mod on the vaporization cavity. The length of the
vaporization cavity created by the Mod was similar to the width,
which increased the volume of the vaporization cavity significantly
and further demonstrated that the energy was being evenly released
around the tip, not just in a forward direction. Additionally, the
Mod exhibited a ceiling effect; the vaporization cavity was altered
inconspicuously when the energy exceeded 400 J. This may be due to
several reasons. First, the energy spread from the tip of the
fiber, whereas the range was not altered for a high energy
attenuation rate when the energy exceeded 400 J. Second, the
nucleus pulposus was optimally vaporized when the energy reached
400 J. In addition, the water content of the target nucleus
pulposus was finite, so no more water was vaporized as the energy
increased. Therefore, the 400 J energy of the Mod provided the
greatest effectiveness and the energy did not exceed 400 J in one
position when the Mod was used in a clinical application for
T-PLDD.
During surgery, the Mod achieved a more accurate
targeted localization without destroying additional tissue.
Although 400 J of the Mod provided the greatest effectiveness in
animal studies, 150, 200, 250 or 300 J was also used in the
clinical setting. The animal study could not be entirely replicated
in the clinical setting, as energies had to be selected based on
the tolerance of patients and the degree of extrusion of the
nucleus pulposus.
In the clinical study, the Mod used in T-PLDD for
patients increased the good-to-excellent rating and decreased the
NRS, ODI, PRI and SF-12 in the short- and long-term with no marked
alterations observed in intervertebral disc height and T2 values.
The total length of the hospital stay was only 3.34±0.66 days.
The present study used T2 relaxation on a
quantitative T2-mapping MRI technique (T2 value) to assess the
water content of the nucleus pulposus. The water content of the
nucleus pulposus was abundant and the T2 relaxation on quantitative
T2-mapping MR technique of the MRI tended to be a high signal that
was reduced when the nucleus pulposus degenerated. Zhu et al
(13) revealed that the T2 value
exhibits a high sensitivity for detecting water alterations in the
nucleus pulposus. Additionally, several studies have demonstrated a
good association between the T2 value and water content in the disc
(14,15). Therefore, the relevance of the T2
value and water content in the present study were not further
validated. As the results demonstrated, the T2 value increased to
normal at 3 months post-surgery, which demonstrated that the water
content of the nucleus pulposus could be restored after 3 months in
patients treated using T-PLDD.
Compared with open surgery, PLDD provides improved
long-term outcomes and is safer and less invasive (16). However, the energy required for PLDD
is large, and short-term clinical outcomes are not significant
(17). Luo et al (6) reported that T-PLDD improves short-term
clinical outcomes. The present study also revealed that T-PLDD
improved short-term outcomes, as demonstrated by the increased
good-to-excellent rating and SF-12 and the decreased NRS, ODI and
PRI. In the present study, pain-associated scores including NRS and
PRI, were decreased at 1 week and reached their best state at 3
months post-surgery. The functional scores, including ODI and SF-12
were restored to their best state at 6 months post-surgery.
In the study by Luo et al (6), the total laser energy was 600–1500 J
for T-PLDD, which is similar to the non-T-PLDD (17). The rate of reoperation in T-PLDD was
~38% (18). Although no serious
complications have been observed within 1 year after T-PLDD with
600–1500 J (6), it is difficult to
evaluate the long-term prognosis. In the present study, a lower
energy of 150–300 J was used and there were differences in outcomes
compared with the study by Luo et al (6). Luo et al (6) revealed that the Visual Analogue Scale
at 3 days, 1 month and 12 months was 2.94±1.10, 2.24±0.66 and
1.31±0.85, respectively, and the good-to-excellent rating at 12
months was 82.5%, which was similar to the present study. However,
the good-to-excellent rating at 1 month (57.5%) was markedly lower
than that in the present study (82.8%). This suggests that the Mod
achieved the same therapeutic effects at low energy and provided
improved pain relief and a good-to-excellent rating during short-
and long-term follow-up.
Zhao et al (4)
adopted 300–500 J in the T-PLDD and the good-to-excellent ratings
at 1 and 12 months were 80.0 and 92.0%, respectively, which was
also indicated in the present study. However, only one index (the
modified MacNab) was used in the study by Zhao et al
(4), which did not fully evaluate
the feasibility and safety of this treatment scheme. The present
study first demonstrated the ceiling effect of Mod in animal
experiments; the energy could not exceed 400 J. Furthermore, the
present study reported improved clinical long-term outcomes. Pain
relief was maintained for 3 years, as demonstrated by the NRS and
PRI, the functional outcomes also indicated an improvement in the
3-year follow-up. No pain recurrence or hypofunction occurred
during the 3-year follow-up. Additionally, the intervertebral disc
height following surgery was not altered, which maintained the
normal tissue structure and assisted the quick postoperative
recovery. Therefore, the Mod used for patients with T-PLDD provided
a great long-term effect. This provided a theoretical basis and
clinical data for the clinical promotion of Mod.
Following surgery, 19 patients received nonsteroidal
anti-inflammatory drugs for pain at the puncture site for 2 days,
which diminished after the puncture site healed. Hematoma occurred
in only 1 patient. Surgery was minimally invasive and the puncture
needle was very thin. However, a hematoma could result from the
rupture of a vessel during puncture or from a prolonged coagulation
time secondary to old age. The hematoma resolved within 7 days and
the therapeutic outcome was not affected.
To observe the effects of age on the outcomes of Mod
used for T-PLDD, patients were divided into Elderly and Young
groups. It was identified that the pain in patients <50 years
old was most alleviated at 3 months after surgery and perfect
recovery of function occurred at 6 months after surgery. For the
patients >50 years old, the perfect recovery state following
surgery was delayed; however, the long-term outcomes were not
affected.
The present study had several limitations. First, no
record of NRS within 24–48 h after PLDD was found in the database,
which was important missing data. However, the patients were
prescribed oral antibiotics for 1 day and painkillers were
prescribed according to the degree of pain experienced by patients.
In the present study, 19 patients received analgesics, which meant
that 32.8% of patients experienced pain within 2 days, which may
have been caused by intradiscal, annular inflammation or edema.
Second, in the clinical part assessment of the present study, there
were no comparison groups, such as a Con group or other treatment
groups. Due to this lack of comparison, it was difficult to
conclude that the efficacy of Mod was improved compared with that
of Con. However, following PLDD with Mod, patients exhibited a
satisfactory treatment effect, which meant the PLDD with the Mod
was efficacious. Additionally, an advantage of the Mod was that the
energy required was lower and the potential complications caused by
high energy were avoided. Finally, Ignatieva et al (19) proposed that lasers could induce the
damage of degenerative annulus fibrosus of lumbar intervertebral
disc. However, their samples were obtained from rabbits and the
annulus fibrosus closed to the fiber tip in their study (19). In the present study, only the fiber
tip could release energy and the tip was inserted in the nucleus
pulposus, which was away from the annulus fibrosus. Therefore, the
annulus fibrosus was rarely affected. The observation that the
patients were not identified to have significant annulus fibrosus
damage during the short- or long-term follow-up also supported this
conclusion.
In conclusion, application of the Mod in T-PLDD
decreased the pain experienced by patients following LDH and
improved the quality of life and curative effects in the short- and
long-term. There was no alteration in the intervertebral disc
height observed at a relatively low energy during a 3-year
follow-up. The Mod should replace the Con in T-PLDD in a clinical
setting due to its low energy and good curative effects.
Additionally, patients with LDH who are <50 years old should be
recommended for T-PLDD surgery.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science and
Technology Plan of Qingdao (grant no. 3067).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CM made substantial contributions to conception and
design, drafted the manuscript, and approved the version to be
published. YL made substantial contributions to acquisition of
data, drafted the manuscript and approved the version to be
published. SW made substantial contributions to analysis and
interpretation of data, completed all animal experiments, drafted
the manuscript and approved the final version to be published. JY
made substantial contributions to the acquisition of data, drafted
the manuscript and approved the version to be published. DK made
substantial contributions to analysis and interpretation of data,
revised the manuscript critically for important intellectual
content and approved the version to be published. CL made
substantial contributions to conception and design, provide the
grant, drafted the manuscript, revised the manuscript critically
for important intellectual content and approved the version to be
published.
Ethics approval and consent to
participate
All protocols were approved by the Institutional
Ethics Committee of the Affiliated Hospital of Qingdao University
(Qingdao, China). The present study was retrospective in
nature. The patients provided written informed consent
(including consent for publication) to receive T-PLDD.
Patient consent for publication
The patients provided written informed consent
(including consent for publication) to receive T-PLDD.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ramakrishnan A, Webb KM and Cowperthwaite
MC: One-year outcomes of early-crossover patients in a cohort
receiving nonoperative care for lumbar disc herniation. J Neurosurg
Spine. 7:391–396. 2017. View Article : Google Scholar
|
|
2
|
Ren C, Li Y, Qin R, Sun P and Wang P:
Transforaminal endoscopic lumbar discectomy for lumbar disc
herniation causing bilateral symptoms. World Neurosurg.
106:413–421. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Andersson GB: Epidemiological features of
chronic low-back pain. Lancet. 354:581–585. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhao XL, Fu ZJ, Xu YG, Zhao XJ, Song WG
and Zheng H: Treatment of lumbar intervertebral disc herniation
using C-arm fluoroscopy guided target percutaneous laser disc
decompression. Photomed Laser Surg. 30:92–95. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
van den Akker-van Marle ME, Brouwer PA,
Brand R, Koes B, van den Hout WB, van Buchem MA and Peul WC:
Percutaneous laser disc decompression versus microdiscectomy for
sciatica: Cost utility analysis alongside a randomized controlled
trial. Interv Neuroradiol. 23:538–545. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luo DX, Jin XJ, Li GT, Sun HT, Li YY and
Qi Y: The use of targeted percutaneous laser disc decompression
under the guidance of puncture-radiating pain leads to better
short-term responses in lumbar disc herniation. Eur Rev Med
Pharmacol Sci. 18:3048–3055. 2014.PubMed/NCBI
|
|
7
|
Schenk B, Brouwer PA, Peul WC and van
Buchem MA: Percutaneous laser disk decompression: A review of the
literature. Am J Neuroradiol. 27:232–235. 2006.PubMed/NCBI
|
|
8
|
Choy DS: Percutaneous laser disc
decompression (PLDD): Twelve years' experience with 752 procedures
in 518 patients. J Clin Laser Med Surg. 16:325–331. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oertel JM and Burkhardt BW: Endoscopic
intralaminar approach for the treatment of lumbar disc herniation.
World Neurosurg. 103:410–418. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fairbank JC and Pynsent PB: The oswestry
disability index. Spine (Phila Pa 1976). 25:2940–2952. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Melzack R: The short form McGill pain
questionnaire. Pain. 30:191–197. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Klessinger S: The frequency of resurgery
after percutaneous lumbar surgery using dekompressor in a ten-year
period. Minim Invasive Surg. 2018:52867602018.PubMed/NCBI
|
|
13
|
Zhu T, Ai T, Zhang W, Li T and Li X:
Segmental quantitative MR imaging analysis of diurnal variation of
water content in the lumbar intervertebral discs. Korean J Radiol.
16:139–145. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Perry J, Haughton V, Anderson PA, Wu Y,
Fine J and Mistretta C: The value of T2 relaxation times to
characterize lumbar intervertebral disks: Preliminary results. AJNR
Am J Neuroradiol. 27:337–342. 2006.PubMed/NCBI
|
|
15
|
Zou J, Yang H, Miyazaki M, Morishita Y,
Wei F, McGovern S and Wang JC: Dynamic bulging of intervertebral
discs in the degenerative lumbar spine. Spine (Phila Pa 1976).
34:2545–2550. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Choy DS, Hellinger J, Hellinger S, Tassi
GP and Lee SH: 23rd Anniversary of percutaneous laser disc
decompression (PLDD). Photomed Laser Surg. 27:535–538. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Choy DS: Percutaneous laser disc
decompression: A 17-year experience. Photomed Laser Surg.
22:407–410. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brouwer PA, Brand R, van den Akker-van
Marle ME, Jacobs WC, Schenk B, van den Berg-Huijsmans AA, Koes BW,
van Buchem MA, Arts MP and Peul WC: Percutaneous laser disc
decompression versus conventional microdiscectomy in sciatica: A
randomized controlled trial. Spine J. 15:857–865. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ignatieva N, Zakharkina O, Andreeva I,
Sobol E, Kamensky V and Lunin V: Effects of laser irradiation on
collagen organization in chemically induced degenerative annulus
fibrosus of lumbar intervertebral disc. Lasers Surg Med.
40:422–432. 2008. View Article : Google Scholar : PubMed/NCBI
|