Introduction
Pre-operative anxiety is a commonly encountered
unpleasant and stressful state prior to surgery, which may
negatively affect treatment outcomes, lead to an increased demand
for anesthetics during surgery and enhance vulnerability to
infection (1). Previous studies have
proved that high pre-operative anxiety predicts increased
intra-operative sedative requirements (2). Effective intra-operative sedation is
required to relieve anxiety, as well as for patient cooperation and
satisfaction with the surgery.
Butorphanol is a synthetic opioid with partial
agonist action at the µ-opioid and κ-opioid receptors (3); it has analgesic and sedative effects
and only few side effects, low addiction potential and low toxicity
(4). The World Health Organization
guidelines also recommend the use of butorphanol as an adjunctive
anesthetic for intra-operative sedation and post-operative pain
relief (5).
Several studies have reported on sedative drugs
commonly used during surgery (2,6,7). However, few studies have been performed
on sedation with butorphanol in patients with pre-operative
anxiety. Furthermore, a formula to predict the precise butorphanol
requirement to maintain patients with a high pre-operative anxiety
score in an adequate sedative state has remained to be
determined.
In the present study, patients who were scheduled
for orthopedic procedures under regional anesthesia were selected
and prior to the surgery, their pre-operative anxiety score was
evaluated by using the Amsterdam pre-operative anxiety and
information scale (APAIS). It was hypothesized that there is an
association between the APAIS score and the duration of reaching
adequate sedation, which can potentially be used to predict the
requirement of butorphanol.
Patients and methods
Subjects
The inclusion criteria were as follows: i) Chinese
male or female patients aged 18–75 years; ii) American Society of
Anaesthesiologists physical status I or II (8); iii) scheduled for elective lower limb
orthopedic procedures under regional anesthesia at Shengjing
Hospital of China Medical University (Shenyang, China) between
March 2018 and March 2019. The exclusion criteria were as follows:
i) Central nervous system disease; ii) cardiovascular disease; iii)
autonomic nervous system disease; iv) long-term use of analgesic,
sedative or anti-anxiety drugs; vi) psychosis or a language
communication disorder; vii) patient did not provide informed
consent.
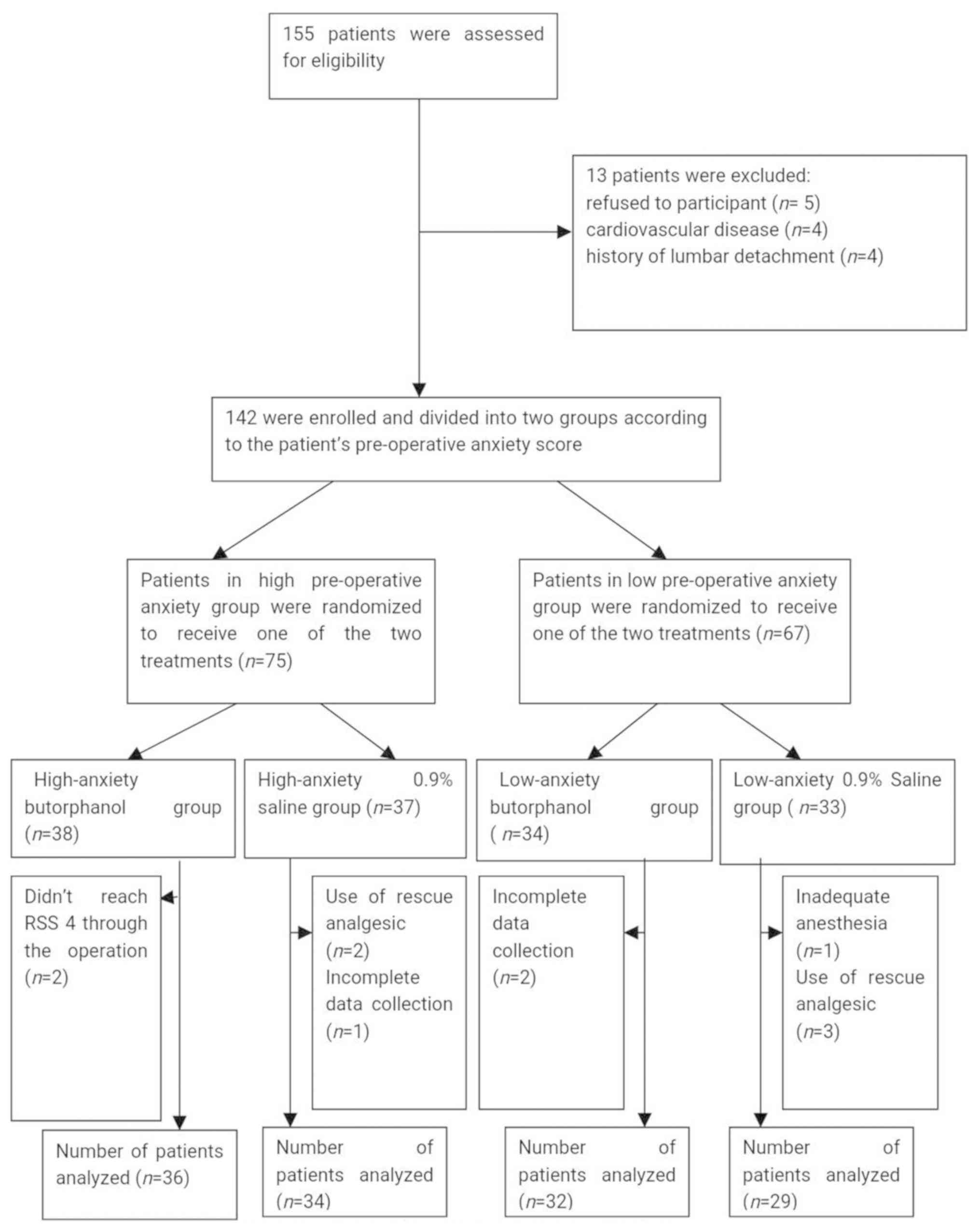
Following assessment of 155 patients for
eligibility, 13 patients were excluded based on the above-mentioned
criteria. Finally, 142 patients were enrolled as eligible subjects.
After evaluating the patients' pre-operative anxiety score by using
the APAIS scale (9–12), as well as a computer-generated
sequence of random numbers and a sealed-envelope technique, 75
patients in the high pre-operative anxiety group (pre-operative
anxiety score >10) were randomized to receive one of the two
treatments (high-anxiety butorphanol group, n=38; high-anxiety 0.9%
saline group, n=37) and 67 patients in the low pre-operative
anxiety group (pre-operative anxiety score ≤10) were also
randomized to receive one of the two treatments (low-anxiety
butorphanol group, n=34; low-anxiety 0.9% saline group, n=33).
Following completion of the study, 5 patients in the high
pre-operative anxiety group were excluded from the study,
comprising 2 patients who did not reach a Ramsay Sedation Score
(RSS) of 4 during the operation (13), 2 patients who received rescue
analgesic and 1 patient with incomplete data. Furthermore, 6
patients in the low pre-operative anxiety group were excluded from
the study, comprising 2 patients with incomplete data, 1 patient
with inadequate anesthesia and 3 patients who received rescue
analgesic. Therefore, the data from 36 patients in the high-anxiety
butorphanol group and 34 patients in the high-anxiety 0.9% saline
group were analyzed in the present study. Furthermore, the data
from 32 patients in the low-anxiety butorphanol group and 29
patients in the low-anxiety 0.9% saline group were analyzed in the
present study (Fig. 1).
Study design
This study was approved by the Human Research
Ethical Committee of Shengjing Hospital (Shenyang, China; IRB
registration no. 2018PS254K) and written informed consent was
obtained from all subjects participating in the trial. The trial
was registered prior to patient enrollment at clinicaltrials.gov (no. NCT03429179; principal
investigator, Bijia Song; date of registration, 20.01.2018).
In the present study, the APAIS was used by an
experimental assistant to evaluate the degree of pre-operative
anxiety of patients enrolled in the study prior to administration
of pre-medication. According to the total anxiety score on the
APAIS, patients were divided into a high pre-operative anxiety
group (pre-operative anxiety score >10) and a low pre-operative
anxiety group (pre-operative anxiety score ≤10). Although a
previous study have stated that it was acceptable to not provide
sedation for this type of lower-limb surgery under local anesthesia
(14), patients enrolled into the
present study were exhibiting pre-operative anxiety and it was
considered ethical to provide sedation. Preliminary experiments
performed by our group indicated no statistically significant
differences in RSS after pre-operative intramuscular injection of
low-dose midazolam for patients with different anxiety levels,
which was confirmed by statisticians (15). Thus, intramuscular midazolam (0.05
mg/kg) as a pre-medication was administered to patients 60 min
prior to transfer to the operating room. All patients were
routinely prepared according to the requirements of regional
anesthesia. Upon arrival in the operating room, standard
monitoring, including an electrocardiogram, non-invasive blood
pressure (NIBP) and peripheral oxygen saturation (SpO2),
were applied. Regional anesthesia was then implemented through the
L2-3 or L3-4 intervertebral space and 0.5% bupivacaine was injected
into the subarachnoid cavity according to the age and weight of the
patients until the block plane reached T8-T10. In the high-anxiety
butorphanol group and low-anxiety butorphanol group, patients
received an intravenous (i.v.) loading dose of 15 µg/kg butorphanol
5 min prior to the beginning of the surgery, followed by infusion
of 7.5 µg/kg/h butorphanol and the infusion was stopped when the
RSS reached 4. The high-anxiety 0.9% saline group and the
low-anxiety 0.9% saline group received an infusion of the same
volume of 0.9% saline. Ramosetron (0.3 mg) was administered
prophylactically at the end of the surgery. The anesthesiologist
connected the i.v. microcomputer-controlled drug-infusion devices
to the patients (Kelijianyuan Med. Co.). The study was
double-blinded for all of the researchers, physicians who collected
the data, the nurses and the staff who prepared the medications.
Each device syringe was filled with butorphanol or 0.9% saline from
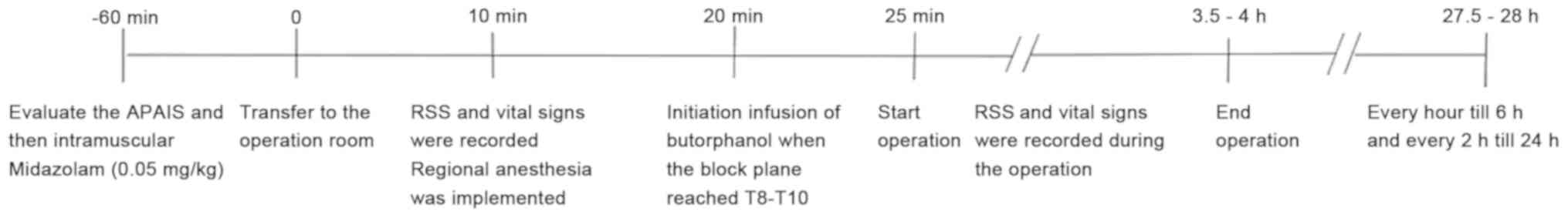
similar ampoules to the same volume. The timeline of the
experimental procedure is provided in Fig. 2.
Experimental data collection
NIBP, mean arterial pressure (MAP) and heart rate
(HR) were recorded 10 min after entering the operating room
(baseline, T0), and at 5 min (T1), 10 min
(T2), 15 min (T3) and 30 min (T4)
after the commencment of i.v. butorphanol infusion of. Hypotension
(MAP <70 mmHg) was treated with fluid boluses and 6 mg i.v.
boluses of ephedrine, while bradycardia (HR<50 bpm) was treated
with 0.6 mg i.v. atropine. Respiratory depression was defined as a
respiratory rate of <8 breaths/min or an SpO2 of
<90% on room air. Patients were given supplemental O2
via face mask at 6 l/min if the SpO2 decreased <90%.
The RSS in the four groups was recorded at 10 min after entering
the operation room and at 5, 10, 15 and 30 min after infusion of
butorphanol or 0.9% saline, and the duration for the RSS to reach 4
in the high-anxiety butorphanol group and the low-anxiety
butorphanol group was also recorded. In the post-operative period,
pain scores were assessed on the visual analogue scale (VAS)
(16) every hour up to 6 h and then
every 2 h up to 24 h. Patients were given flurbiprofen axetil 50 mg
as a rescue analgesic and then excluded from the analysis. Adverse
events, including nausea/vomiting, dizziness, bradycardia and
respiratory depression were recorded at the same time-points as the
VAS scores and treated accordingly.
Evaluation of pre-operative
anxiety
The APAIS is a questionnaire to assess patients'
pre-operative anxiety score, which was developed in 1996 by the
Dutch clinician Moerman (9). The
APAIS comprises 6 items rated on a five-point Likert scale, which
includes two scales: Anxiety (items 1, 2, 4 and 5) and requirement
for information (items 3 and 6) (10,11). The
maximal total APAIS score is 30; this is comprised of a maximum
score expressing the patient's requirement for information of 10
and a maximal score of the two items concerning anxiety regarding
anesthesia and surgery of 10 each, resulting in a maximal score of
20 for total anxiety (APAIS-A-T). In the present study, APAIS-A-T
>10 was used as a cut-off to define patients with high anxiety,
with a higher score indicating a higher level of anxiety (12).
Evaluation of sedation
The depth of sedation was determined based on the
RSS scale (13), as follows: 1,
Anxious and agitated or restless or both; 2, cooperative,
orientated and tranquil; 3, responds to commands only; 4, brisk
response to a light glabellar tap or auditory stimulus; 5, sluggish
response to a light glabellar tap or auditory stimulus; and 6, no
response to a light glabellar tap or auditory stimulus. Patients
with a sedation score equal to 4 were considered to have adequate
sedation.
Evaluation of patient
satisfaction
Patient satisfaction was recorded on 5 levels: a)
Agreeable experience; b) neither pleasant nor unpleasant; c)
slightly uncomfortable; d) disagreeable experience; e) traumatic
experience.
Statistical analysis
SPSS 20.0 statistical software (IBM Corp.) was used
for data analysis. Continuous variables are expressed as the mean ±
standard deviation and the Chi-squared test was used to analyse
differences in demographic data, post-operative side effects and
patient satisfaction between groups. Comparisons between two groups
were performed by using an independent-samples Student's t-test.
One-way analysis of variance (ANOVA) followed by Bonferroni
correction was used for multiple comparisons and Welch's ANOVA
followed by Tamhane's T2 post-hoc pairwise comparison was used for
multiple groups which did not meet the Levene's test criteria.
Linear association analysis was performed between the APAIS score
and duration of RSS reaching 4 to calculate an r2 value.
P<0.05 was considered to indicate statistical significance.
Results
Patient characteristics
The patient characteristics are provided in Table I. There were no significant
differences among the study groups regarding demographic
characteristics, type of surgery or duration of surgery.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
|
| High pre-operative
anxiety group | Low pre-operative
anxiety group |
|
|---|
|
|
|
|
|
|---|
| Item | Butorphanol group
(n=36) | 0.9% saline group
(n=34) | Butorphanol group
(n=32) | 0.9% saline group
(n=29) | P-value |
|---|
| Sex |
|
|
|
| 0.888 |
| Male | 17 (47.2) | 14 (41.2) | 13 (40.6) | 11 (37.9) |
|
|
Female | 19 (52.8) | 20 (58.8) | 19 (59.4) | 18 (62.1) |
|
| Age (years) | 47.1±16.8 | 47.3±16.0 | 41.5±14.2 | 41.0±12.3 | 0.172 |
| Weight (kg) | 65.8±3.0 | 68.6±10.6 | 69.8±8.3 | 66.0±4.1 | 0.069 |
| Duration of surgery
(min) | 83.3±15.8 | 84.0±16.5 | 85.2±18.4 | 86.5±16.4 | 0.877 |
| Type of surgery |
|
|
|
| 0.283 |
| Repair of
ligament injury | 15 (41.7) | 17 (50) | 11 (34.4) | 9 (31.1) |
|
| Repair of
meniscus injury | 11 (30.6) | 8 (23.5) | 10 (31.3) | 15 (51.7) |
|
|
Other | 10 (27.8) | 9 (26.5) | 11 (34.4) | 5 (17.2) |
|
Comparison of the RSS among the
different groups
The RSS score of the different groups at various
time-points is provided in Table
II. Of note, there was no significant difference in RSS at 10
min after entering the operating room among the four groups
(P>0.05). The sedation scores of the high-anxiety 0.9% saline
group were lower than those of the high-anxiety butorphanol group
at each time-point after infusion (P<0.05). There were also
significant differences between the high-anxiety butorphanol group
and the low-anxiety butorphanol group at each time-point after
infusion (P<0.05).
 | Table II.Ramsay Sedation Score. |
Table II.
Ramsay Sedation Score.
| Group | T0 | T1 | T2 | T3 | T4 |
|---|
| High pre-operative
anxiety |
|
|
|
|
|
| butorphanol
group | 1.42±0.5 |
1.92±0.6a |
2.22±0.5a |
2.42±0.5a |
3.31±1.0a |
| 0.9% saline
group | 1.41±0.5 |
1.47±0.5a,b |
1.53±0.5a,b |
1.65±0.6a,b |
1.82±0.6a,b |
| Low pre-operative
anxiety group |
|
|
|
|
|
| butorphanol
group | 1.53±0.5 |
2.34±0.5b |
2.91±0.8b |
3.47±0.8b |
4.0±0.0b |
| 0.9% saline
group | 1.52±0.4 |
1.55±0.5a,b |
1.66±0.7a,b |
1.83±0.7a,b |
1.97±0.5a,b |
| P-value | 0.665 | <0.001 | <0.001 | <0.001 | <0.001 |
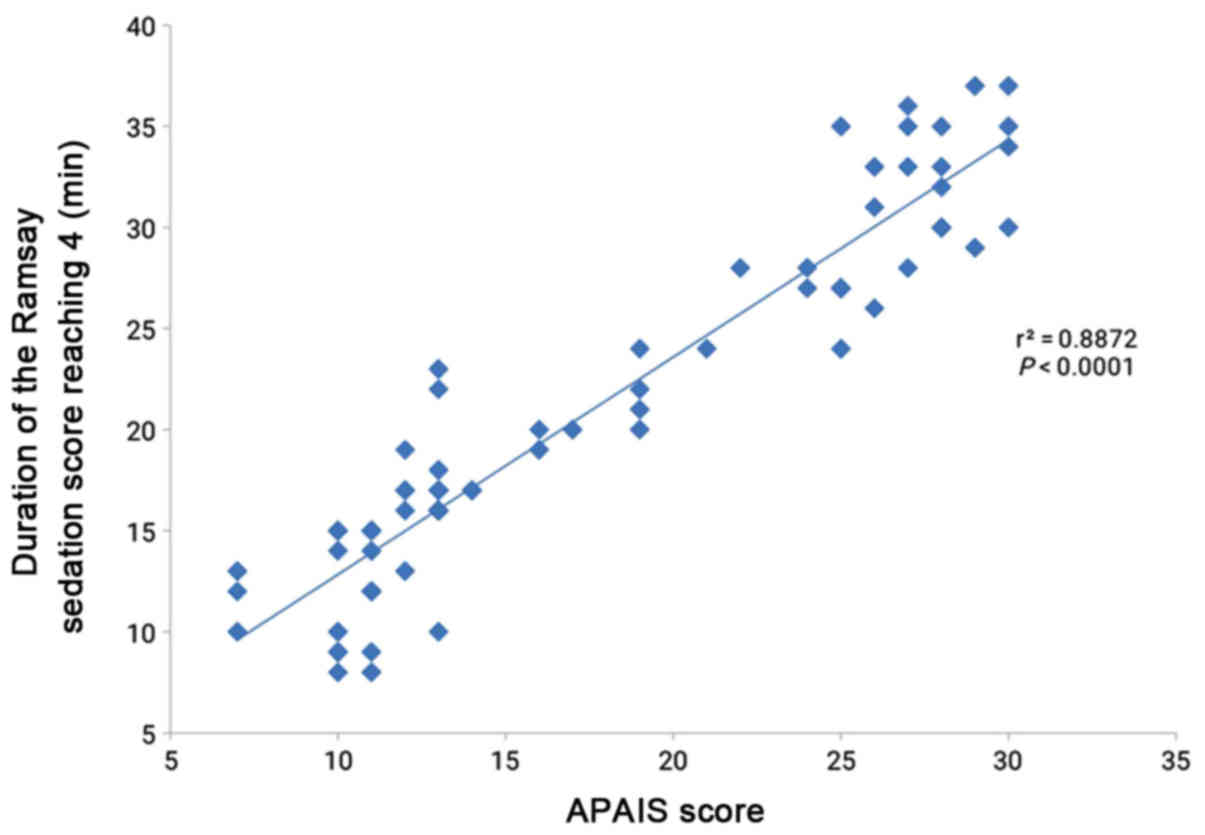
Association between the APAIS score
and duration of RSS reaching 4
As presented in Fig.
3, an approximately linear correlation between the APAIS score
and duration of RSS reaching 4 was observed. Linear regression
analysis revealed an r2-value of 0.887, suggesting that
88.7% of the variation in the time taken for the RSS to reach 4 may
be accounted for by the APAIS score (P<0.0001). The regression
equation was determined as follows: Duration of reaching adequate
sedation (min)=(1.075 × APAIS score) + 2.081. According to the
butorphanol infusion method applied in the present study, the
formula to determine the required dose was as follows: Precise dose
of butorphanol (µg/kg)=15.26 + (0.14 × APAIS score).
Comparison of HR and MAP among the
different groups
The HR and MAP in the different groups at each
time-point are provided in Table
III. In the high-anxiety butorphanol group and low-anxiety
butorphanol group, the MAP at each time-point was significantly
lower than that at the respective previous time-point in the same
group (P<0.05). However, no significant differences were
obtained in the high-anxiety 0.9% saline group and low-anxiety 0.9%
saline group with this regard (P>0.05). The MAP at each time
point in the high-anxiety 0.9% saline group was higher compared
with that in the other three groups. Furthermore, the HR at T0 in
the high-anxiety butorphanol group and high-anxiety 0.9% saline
group were higher compared with that in the low-anxiety butorphanol
group, though there was no significant difference between the
low-anxiety 0.9% saline and the low-anxiety butorphanol groups. The
HR value in the high-anxiety 0.9% saline group remained at a high
level during the operation. There was no difference in
SpO2 among the four groups during the course of the
study (data not shown).
 | Table III.Comparison of HR and MAP among
different groups. |
Table III.
Comparison of HR and MAP among
different groups.
| A, HR |
|---|
|
|---|
| Group | Cases (n) | T0 | T1 | T2 | T3 | T4 |
|---|
| High pre-operative
anxiety group | 70 |
|
|
|
|
|
|
Butorphanol group | 36 |
88.1±9.3a |
73.4±8.2b |
70.4±9.2b |
68.1±7.9b |
66.3±7.7b |
| 0.9%
saline group | 34 |
89.8±8.4a |
88.4±5.1a |
88.1±5.6a |
87.0±7.9a |
86.2±6.7a |
| Low pre-operative
anxiety group | 61 |
|
|
|
|
|
|
Butorphanol group | 32 | 74.0±7.7 |
71.7±6.6b |
69.8±7.3b | 68.3±6.2 | 66.1±5.8 |
| 0.9%
saline group | 29 | 73.1±6.4 | 72.1±6.4 | 71.1±7.5 | 70.7±5.8 | 70.0±5.0 |
|
| B, MAP |
|
| Group | Cases
(n) | T0 | T1 | T2 | T3 | T4 |
|
| High pre-operative
anxiety group | 70 |
|
|
|
|
|
|
Butorphanol group | 36 |
96.1±3.9a |
88.3±3.2b |
84.8±4.0b |
82.7±3.6b |
80.9±3.6b |
| 0.9%
saline group | 34 |
97.9±5.7a |
97.1±4.2a |
96.4±3.4a |
95.7±3.3a |
95.0±3.6a |
| Low pre-operative
anxiety group | 61 |
|
|
|
|
|
|
Butorphanol group | 32 | 89.3±4.8 |
86.9±3.9b |
83.9±5.2b |
81.9±2.8b |
80.5±2.9b |
| 0.9%
saline group | 29 | 88.5±5.2 | 88.2±4.8 |
87.3±3.6a |
86.8±2.8a |
86.1±2.8a |
Post-operative recovery
The VAS scores were significantly lower in the
butorphanol groups (high-anxiety butorphanol group and low-anxiety
butorphanol group) as compared with those in the 0.9% saline groups
(high-anxiety 0.9% saline group and low-anxiety 0.9% saline group)
throughout the the first 24 h post operation (P<0.05; Table IV). The differences in adverse
events (nausea/vomiting, dizziness, bradycardia and respiratory
depression) were statistically insignificant among the four groups
(Table IV). However, regarding
post-operative patient satisfaction, the rating ‘agreeable
experience’ was significantly more frequently given by the group
receiving intra-operative sedation (P=0.032), while the saline
group more frequently provided the rating ‘disagreeable experience’
(P=0.005) compared with the respective other group (Table V).
 | Table IV.Post-operative parameters in the
first 24 h after operation. |
Table IV.
Post-operative parameters in the
first 24 h after operation.
| A, Adverse
events |
|---|
|
|---|
|
| High pre-operative
anxiety group | Low pre-operative
anxiety group |
|
|---|
|
|
|
|
|
| Item | Butorphanol group
(n=36) | 0.9% saline group
(n=34) | Butorphanol group
(n=32) | 0.9% saline group
(n=29) | P-value |
|---|
| Nausea and
vomiting | 7 (19.4) | 6 (17.6) | 3 (9.4) | 1 (3.4) | 0.196 |
| Dizziness | 7 (19.4) | 3 (8.8) | 5 (15.6) | 2 (6.9) | 0.391 |
| Respiratory
depression | 0 (0) | 0 (0) | 0 (0) | 0 (0) | – |
| Bradycardia | 0 (0) | 0 (0) | 0 (0) | 0 (0) | – |
|
| B,
Post-operative VAS score |
|
| Time-point
(h) | Butorphanol
groups | 0.9% Saline
groups | P-value |
|
| 1 | 0.90±0.7 |
2.79±0.8 |
<0.001 |
| 2 | 1.16±0.6 |
3.22±0.7 |
<0.001 |
| 4 | 1.44±0.5 |
3.62±0.5 |
<0.001 |
| 6 | 1.79±0.4 |
3.76±0.4 |
<0.001 |
| 12 | 2.62±0.6 |
4.29±0.8 |
<0.001 |
| 24 | 3.28±0.6 |
5.13±0.6 |
<0.001 |
 | Table V.Post-operative patient
satisfaction. |
Table V.
Post-operative patient
satisfaction.
| Rating | Butorphanol
groups | 0.9% Saline
groups | P-value |
|---|
| Agreeable
experience | 44 (64.7) | 29 (46) | 0.032 |
| Neither pleasant
nor unpleasant | 19 (27.9) | 18 (28.6) | 0.936 |
| Slightly
uncomfortable | 5 (7.4) | 9 (14.3) | 0.199 |
| Disagreeable
experience | 0 (0) | 7 (11.1) | 0.005 |
| Traumatic
experience | 0 (0) | 0 (0) | – |
Discussion
The results of the present study indicated that the
requirement of butorphanol for conscious sedation was correlated
with the level of pre-operative anxiety in patients receiving
lower-limb orthopedic surgery under regional anesthesia. The
duration of reaching an adequate sedative state increased
approximately linearly with the increase of the APAIS score, which
may suggest that for a higher anxiety score, more butorphanol
should be used. Previous studies have also reported a correlation
between different levels of anxiety and sedative or anesthetic
requirement when conscious sedation or anesthesia is used (2,17,18),
which was consistent with the results of the present study.
In the present study, APAIS, as a well-established
measuring scale, was used to evaluate the level of the patients'
pre-operative anxiety, which was also used in previous studies
(19,20), and the clinical scoring method used
to measure the level of patient sedation was the commonly used RSS
scale (21). A sedative state with
an RSS of 3 or 4 was considered as an adequate level of sedation
(22). Therefore, in the present
study, the time taken for the RSS to reach 4 was defined as the
endpoints of i.v. butorphanol infusion (i.e. the time infusion was
terminated).
Lower-limb orthopedic surgery is frequently
performed with regional anesthesia (23). Despite several advantages, those
surgeries are associated with discomfort and worry for the
patients. Furthermore, lower-limb orthopedic surgery usually
requires to be performed under the tourniquet to achieve a clear
operation field. However, application of a tourniquet is a
non-physiological process, resulting in an irritable state, local
sense of pressure and higher blood pressure after a certain time.
Becher et al (24) reported
that patients were prone to depression and anxiety after orthopedic
injuries, which was also in accordance with our experience at our
institution. Stress factors in the operating room and ineffective
or patchy blocks may aggravate nervosity and anxiety in patients
under regional anesthesia. Thus, sufficient sedation and
cooperation of the patient are of great importance.
Procedural sedation, known as monitored anesthesia
care, includes methods including a single-dose, intermittent or
continuous infusion. However, the different responses of patients
with different levels of pre-operative anxiety to sedative drugs
may result in ineffective or deep sedation (2). In the present study, to better explore
the sedative requirements of patients with different pre-operative
anxiety scores, butorphanol was administered with a loading dose
followed by a maintenance dose. A previous study also reported that
continuous i.v. infusion of butorphanol was able to maintain plasma
butorphanol concentrations within a stable range, resulting in
effective analgesia, and the side effects were reduced during the
infusion compared with a single injection of butorphanol (25). The total safe dose of butorphanol
that may be given i.v. is 20–40 µg/kg (26). According to the administration method
in the present study, the total dose of butorphanol may be
guaranteed to be in the safe range when the duration of the
operation is ≤3.5 h. In the present study, the longest duration of
surgery did not exceed 3.5 h and the total dose of butorphanol was
still in the safe range.
Sinha et al (7) reported that butorphanol provided
satisfactory sedation, and in the present study, the RSS in
patients with high pre-operative anxiety in the butorphanol group
was higher than that in patients with high pre-operative anxiety in
the 0.9% saline group at each time-point after infusion.
Furthermore, a linear correlation between the duration for the RSS
to reach 4 and the APAIS score of patients in the butorphanol
groups was determined, and the butorphanol infusion method applied
in the present study was as follows: The total dose of butorphanol
was administered as a loading dose of 15 µg/kg butorphanol,
followed by infusion of 7.5 µg/kg/h. After substituting the linear
regression equation derived from the correlation graph into that
for the butorphanol infusion method, the following formula was
obtained: Precise dose of butorphanol (µg/kg)=15.26 + (0.14 × APAIS
score).
Pre-operative anxiety was also reported to cause
fluctuation of hemodynamics and damage to sleep quality, which may
be potentially harmful to patients; however, an adequate sedative
state in patients may reduce hemodynamic changes and raise the
level of patients' satisfaction (27). In the present study, the hemodynamics
were kept lower during the operation in MAP and HR in patients with
high pre-operative anxiety in the butorphanol group than in
patients with high pre-operative anxiety in the 0.9% saline group.
The level of patient satisfaction with conscious i.v. sedation was
between agreeable and neither pleasant nor unpleasant for 92.6% of
patients and slightly uncomfortable for 7.4%, which was better than
in the patients in the 0.9% saline groups. The side effects were
similar among patients, regardless of the level of pre-operative
anxiety. Although the incidence of nausea/vomiting and dizziness in
patients with high pre-operative anxiety in the butorphanol group
was higher than that in the other three groups, there were still no
significant differences among the four groups. None of the patients
had respiratory depression or bradycardia in the first 24 h
post-operation.
Sinha et al (7) also demonstrated that butorphanol
decreased the post-operative analgesic requirement. Similar to
their results, the present study indicated that the VAS scores were
significantly lower in the butorphanol groups as compared with
those in the 0.9% saline groups throughout the first 24 h
post-operation.
The present study has certain limitations that are
worth mentioning. First, the RSS scale and APAIS used in the
present study are authoritative scales, while the method used to
measure the level of patient sedation and pre-operative anxiety
were based on the subjective observation of the investigator,
leading to a lack of objectivity of data to a certain extent.
Furthermore, the proposed formula requires further improvement to
determine which way of infusion should be used to rapidly achieve
an adequate sedative state. Finally, after application of sedative
drugs, there were still two patients with a high pre-operative
anxiety score in the butorphanol group who did not reach RSS 4
throughout the operation, which may suggest that the infusion
method applied in the present study does not apply to all types of
patient.
In conclusion, butorphanol did not only provide an
effective sedative and analgesic effect without a significant
increase in adverse effects, including nausea, vomiting,
bradycardia or respiratory depression, but also provided stable
hemodynamic changes during the surgery and higher post-operative
satisfaction for patients with pre-operative anxiety. The formula
proposed was as follows: Precise dose of butorphanol (µg/kg)=15.26
+ (0.14 × APAIS score; adherence to this formula may provide an
improvement for patients who exhibit a high level of pre-operative
anxiety. If patients with a higher pre-operative anxiety score do
not achieve adequate sedation within the calculated total dose,
combined use of other sedative drugs should be considered.
Acknowledgements
The authors would like to thank Dr Liqiang Zheng
from the Department of Statistics, Shengjing Hospital of China
Medical University at Shenyang (Shenyang, China) for discussion and
advice regarding the statistical analysis of this study.
Funding
The present study was funded by the Support Plan for
Innovative Talents in Liaoning Higher Education Institutions (grant
no. 201834).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
BS, YY and JZ designed the study. BS, YY, WB, XT and
YL performed the study. BS, WB and JZ analyzed the data. BS, YY, WB
and JZ prepared the manuscript. All authors contributed to the
conception of the study and read and approved the final
manuscript.
Ethics approval and consent to
participate
Ethical approval of this study was granted by the
Human Research Ethical Committee of Shengjing Hospital (Shenyang,
China; IRB registration no. 2018PS254K). Informed consent was
obtained from all of the participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
APAIS
|
Amsterdam pre-operative anxiety and
information scale
|
|
RSS
|
Ramsay sedation score
|
|
NIBP
|
non-invasive blood pressure
|
|
SpO2
|
peripheral oxygen saturation
|
|
MAP
|
mean arterial pressure
|
|
HR
|
heart rate
|
|
VAS
|
visual analogue scale
|
References
|
1
|
Seifi Z, Beikmoradi A, Oshvandi K,
Poorolajal J, Araghchian M and Safiaryan R: The effect of lavender
essential oil on anxiety level in patients undergoing coronary
artery bypass graft surgery: A double-blinded randomized clinical
trial. Iran J Nurs Midwifery Res. 19:574–570. 2014.PubMed/NCBI
|
|
2
|
Osborn TM and Sandler NA: The effects of
pre-operative anxiety on intravenous sedation. Anesth Prog.
51:46–51. 2004.PubMed/NCBI
|
|
3
|
Jaw SP, Hoskins B and Ho IK: Opioid
antagonists and butorphanol dependence. Pharmacol Biochem Behav.
44:497–500. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nelson KE and Eisenach JC: Intravenous
butorphanol, meperidine, and their combination relieve pain and
distress in women in labor. Anesthesiology. 102:1008–1013. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
WHO Expert Committee on Drug Dependence, .
WHO expert committee on drug dependence. World Health Organ Tech
Rep Ser i. 1-21:23–24. 2006.
|
|
6
|
Elcicek K, Tekin M and Kati I: The effects
of intravenous dexmedetomidine on regional hyperbaric ropivacaine
anesthesia. J Anesth. 24:544–548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sinha C, Kaur M, Kumar A, Kulkarni A,
Ambareesha M and Upadya M: Comparative evaluation of midazolam and
butorphanol as oral premedication in pediatric patients. J
Anaesthesiol Clin Pharmacol. 28:32–35. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mohamed D: American society of
anaesthesiologists physical status classification. Indian J
Anaesth. 55:111–114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moerman N: Psychological aspects of
anesthesia. Nederlands Tijdschrift Voor Anesthesiol. 2:61–63.
1996.
|
|
10
|
Goebel S, Kaup L and Mehdorn HM: Measuring
pre-operative anxiety in patients with intracranial tumors: The
Amsterdam pre-operative anxiety and information scale. J Neurosurg
Anesthesiol. 23:297–293. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wattier JM, Barreau O, Devos P, Prevost S,
Vallet B and Lebuffe G: Measure of pre-operative anxiety and need
for information with six issues. Ann Fr Anesth Reanim. 30:533–537.
2011.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Moerman N, van Dam FS, Muller MJ and
Oosting H: The Amsterdam preoperative anxiety and information scale
(APAIS). Anesth Analg. 82:445–451. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ramsay MA, Savege TM, Simpson BR and
Goodwin R: Controlled sedation with alphaxalone-alphadolone. Br Med
J. 2:656–659. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gurajala I, Nikhar SA, Jayaram K and
Gopinath R: Regional anesthesia is safe and effective for lower
limb orthopedic surgery in patient with renal tubular acidosis and
hypokalemia. J Anaesthesiol Clin Pharmacol. 34:117–119.
2018.PubMed/NCBI
|
|
15
|
Tago N, Kanaya N, Nakayama M, Seki S,
Kawana S and Nakiki A: Evaluation of midazolam premedication for
preoperative anxiolysis. Masui. 43:1520–1523. 1994.(In Japanese).
PubMed/NCBI
|
|
16
|
Behrend CJ, Schönbach EM, Vaccaro AR,
Coyne E, Prasarn ML and Rechtine GR: Maximum pain on visual analog
scales in spinal disorders. Spine J. 17:1061–1065. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Maranets I and Kain ZN: Preoperative
anxiety and intraoperative anesthetic requirements. Anesth Analg.
89:1346–1351. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hong JY, Jee YS and Luthardt FW:
Comparison of conscious sedation for oocyte retrieval between
low-anxiety and high-anxiety patients. J Clin Anesth. 17:549–553.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Celik F and Ipek S: Evaluation of
preoperative anxiety and fear of anesthesia using APAIS score. Eur
J Med Res. 23:412018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Aust H, Eberhart L, Sturm T, Schuster M,
Nestoriuc Y, Brehm F and Rüsch D: A cross-sectional study on
pre-operative anxiety in adults. J Psychosom Res. 111:133–139.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Deol H, Dimtri F, Minaie A, Surani S and
Udeani G: Role of Ramsay sedation scale in sedative dosage
modulation for Critically-Ill intubated patients. Chest.
152:A3302017. View Article : Google Scholar
|
|
22
|
Strøm T: Sedation in the ICU. Dan Med J.
59:B44582012.PubMed/NCBI
|
|
23
|
Ekin A, Donmez F, Taspinar V and Dikmen B:
Patient-controlled sedation in orthopedic surgery under regional
anesthesia: A new approach in procedural sedation. Braz J
Anesthesiol. 63:410–414. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Becher S, Smith M and Ziran B: Orthopaedic
trauma patients and depression: A prospective cohort. J Orthop
Trauma. 28:e242–e246. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sellon DC, Monroe VL, Roberts MC and
Papich MG: Pharmacokinetics and adverse effects of butorphanol
administered by single intravenous injection or continuous
intravenous infusion in horses. Am J Vet Res. 62:183–189. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
WHO: 34th ECDD 2006/4.1: Critical review
of BUTORPHANOL, . http://www.who.int/medicines/areas/quality_safety/4.1ButhorphanolCritReview.pdfFebruary
12–2012
|
|
27
|
Tripathi M, Nath SS, Chaudhary A, Singh PK
and Pandey CM: Patient controlled sedation during center neuraxial
anesthesia. J Postgrad Med. 55:108–112. 2009. View Article : Google Scholar : PubMed/NCBI
|