Introduction
The long head of the biceps (LHB) enters the
shoulder joint at a large angle and its lesion is a common cause of
shoulder pain (1). LHB lesions
include tendinitis, tendon wear, superior labral tear from anterior
to posterior (SLAP) lesion and partial or complete rupture
(2). Isolated LHB lesions are rare
and are frequently accompanied by rotator cuff tear or acromial
impingement (3). Tendon fixation is
a reliable and effective surgical procedure for the treatment of
LHB lesions (4). A number of
surgical methods have been used in the treatment of LHB, including
open, small incision or complete arthroscopy surgery, with a
variety of fixing methods, including high or low tenodesis, bone
tunnel fixation, soft tissue fixation, keyhole fixation, as well as
anchor or interference screw fixation (5). Siebenlist et al (6) demonstrated a novel fixation method to
treat LHB involving suspension from microplates on the inner
surface of the cortical bone, close to the humerus. This fixation
technique has resulted in good short-term biomechanical results;
however, this relies solely on the fixation on a single cortical
bone. The tendon is in contact with a small area of the cortical
bone surface, and this may be detrimental to tendon-bone healing.
This technique also requires pulling of the guide pin through the
contralateral side to pull out soft tissue, which may cause
axillary nerve injury. In this light, the present study provides
improvements to the technique and counteracts these problems
associated with the original treatment. Combined with keyhole
technology, the intramedullary microplate was transferred to the
surface of the ipsilateral cortical bone, and this treatment was
used in 9 patients with LHB ruptures, pop-eye sign and decreased
muscle strength. Application of this method resulted in beneficial
short-term effects.
Patients and methods
Patient information
Between April 2015 and July 2017, LH modified
keyhole suspension fixation was performed on 9 patients with LHB
rupture exhibiting pop-eye sign and decreased flexion strength. The
cohort included 8 males and 1 female aged between 43 and 65 years
of age, and all were physical laborers. In all patients, the
affected limb was that on the right side. A total of 6 patients
complained of shoulder pain after carrying heavy objects, which led
them to visit the hospital. A total of 3 patients had long-term
shoulder pain and discovered pop-eye sign at the right upper
extremity without any obvious cause. All patients were aware that
they exhibited a decline in elbow strength. The study inclusion
criterion was isolated LHB rupture without surgical
contraindications, while the exclusion criteria were surgical
contraindications. Each patient provided written informed consent.
All of the procedures performed in the present study complied with
the ethical requirements of the Affiliated Hospital of Nanjing
University of Chinese Medicine (Nanjing, China).
Surgical technique
Surgery was performed under general anesthesia. Each
patient was placed in the beach chair position and the affected
limb was placed at an abduction of 20° and elbow flexion of 90°,
with forearm supination. The surgical incision was made 2 cm
lateral to the coracoid, was 5 cm long and was inferior along the
edge of the deltoid muscle. The skin and subcutaneous tissue were
subsequently cut to expose the cephalic vein. The cephalic vein was
pulled to the medial, revealing the gap between the pectoralis
major and the deltoid muscle. The long head tendon sheath of the
biceps entered the cut to expose the broken LHB (sometimes, the
ends of the LHB were under the pectoralis major tendon after
rupture). After electrocoagulation of the anterior circumflex
artery branch, along the distal extension line of the
intertubercular sulcus and the upper edge of the pectoralis major
tendon, a hole was drilled in the proximal humerus cortical bone,
perpendicular to the medullary cavity, with a 4.0 mm drill, with
the direction slightly towards the cephalad. A second hole was
drilled with a 4.0 mm drill, 2 cm cranial to the first hole, with
the direction slightly towards the caudal side. The broken end of
the tendon was trimmed and the bicep tendon was tightened at the
elbow flexion of 90°. Subsequently, the junction of the tendon and
abdomen was at level with the lower edge of the pectoralis major
tendon. The stump of the long head was removed parallel to the
proximal bone hole. Two No. 5 Ethibond wires were used to knit the
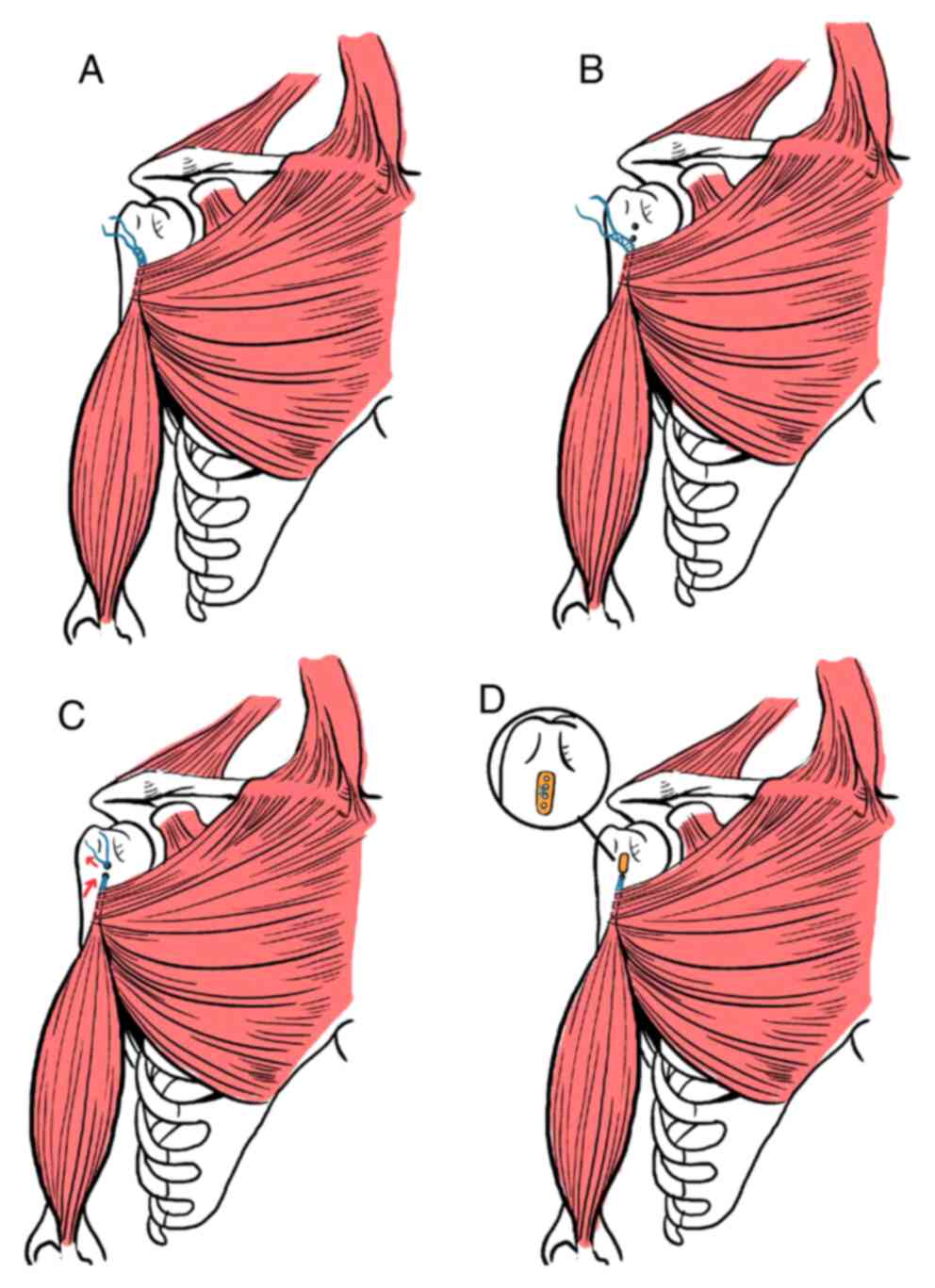
2.5-cm tendon ends (Fig. 1A and B).
The curved hollow guide pin was inserted from the lower hole to the
upper hole, and the wire loop in the guide pin was extended to
insert the folded No. 2 Ethibond wire. The curved hollow guide pin
was removed, the blind end of the No. 2 Ethibond wire was removed
from the hole of the distal cortical bone and the tendon-knitted
wire was inserted into the distal blind end of the No. 2 Ethibond
wire. The two free ends near the No. 2 Ethibond wire were pulled,
the knitted wire was pulled into the medullary cavity from the
lower bone hole and subsequently pulled out from the upper bone
hole. The long-headed tendon was pulled into the medullary cavity
from the distal bone hole by pulling the knitted wire and it was
removed from the proximal end of the bone hole (Fig. 1C). The loop of the endobutton was
subsequently cut off and the two ends of the two tendon-knitted
wires were passed through the two holes at the center of the
endobutton. The elbow was bent at 90° and the forearm was rotated.
The corresponding suture was knotted on the endobutton and the
elbow joint was slightly stretched. The endobutton was then
suspended from the surface near the bone hole and the LHB
suspension fixation was complete (Fig.
1D). Post-operative bleeding was prevented following incision
cleaning by suturing layer by layer. Antibiotics were routinely
used 30 min prior to and 24 h following surgery.
Post-operative treatment
The upper limbs were suspended at 90° for 6 weeks.
Passive activity training began on the second day following
surgery. Active elbow flexion was prohibited for 6 weeks and elbow
weight training was prohibited for 12 weeks. Although passive
activity training, including passive elbow flexion and extension,
began on the second day following surgery.
Observation indexes and evaluation of
therapeutic effect
Follow-up of patients was completed at 12 months
following surgery. The visual analogue scale (VAS) score (7), elbow flexion strength (8), elbow joint supination muscle strength
(9), the University of California
Los Angeles (UCLA) shoulder score (10) and Rating Scale of American Shoulder
Elbow Surgeons (ASES) score (11)
were determined to evaluate the outcome of the surgery. These
parameters were used to evaluate the discrepancies between
pre-operation and post-operation.
Statistical analysis
SPSS 19 software (IBM Corp.) was used for
statistical analysis. Values are expressed as the mean ± standard
deviation. Comparison between two groups (pre- and post-surgery)
was performed using a student's t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Surgery
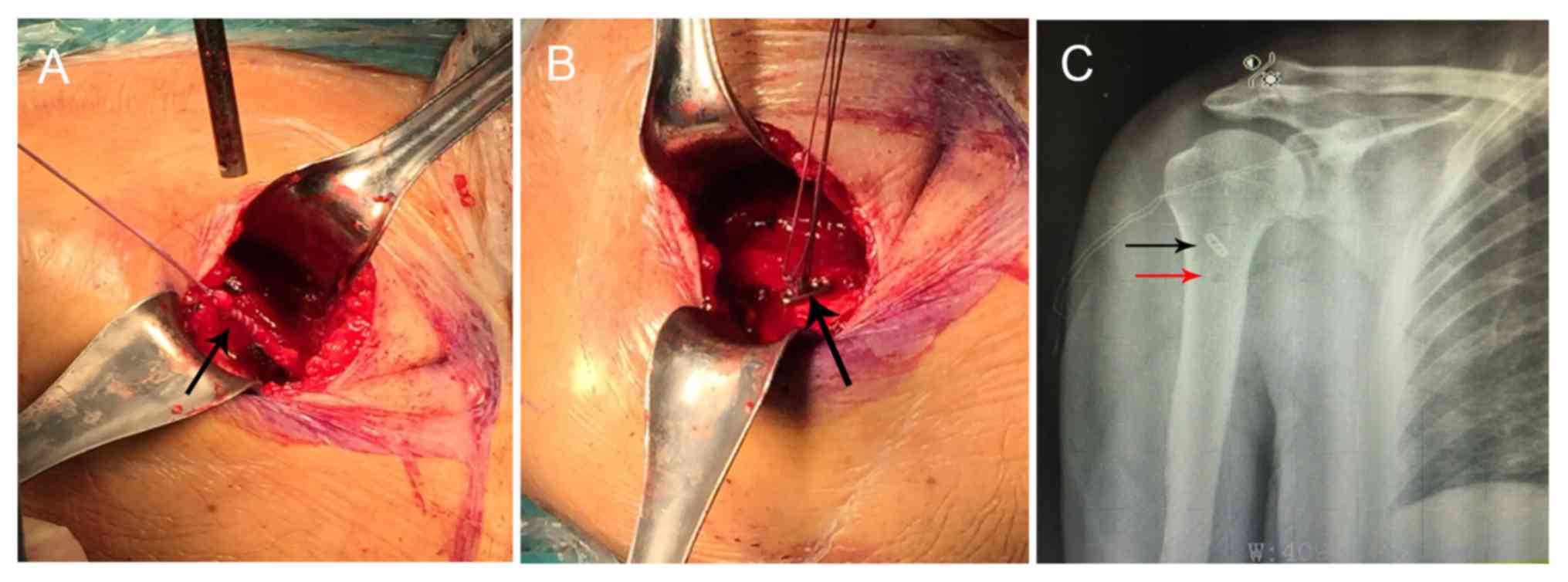
Representative intra-operative images and a
post-operative X-ray scanning image are presented in Fig. 2. Intraoperative bleeding was ~30–50
ml. Gentle tissue separation reduced bleeding, and accurate
incision positioning ensured moderate exposure of the LHB rupture
end (Fig. 2A and B). The operation
time was ~40–70 min.
Complications
After the surgery, the patients were followed up for
one year. None of the 9 patients included in the present study
exhibited any complications including nerve injury, infection and
shoulder rigidity during or following the surgery. No pop-eye signs
were observed during follow-up.
Surgical outcome at 1 year
At one year post-surgery, the VAS score, UCLA
shoulder scores and ASES scores were significantly increased
compared with the pre-operative values (Table I). All of the elbow flexion strength
and elbow joint supination muscle strength were restored to grade V
at the last follow-up. Active elbow flexion was allowed for 6 weeks
after operation and elbow weight training was allowed for 12 weeks
after operation. The upper limbs of all patients were fully
weight-bearing at 6 months after operation.
 | Table I.Functional scores of patients with LHB
rupture treated with the modified keyhole technique (n=9). |
Table I.
Functional scores of patients with LHB
rupture treated with the modified keyhole technique (n=9).
| Evaluation | Pain (VAS
scores) | Elbow flexion
strength (grade) | Strength of elbow
supination (grade) | UCLA scores | ASES scores |
|---|
| Pre-operation | 7.22±1.20 | 4 | 4 | 24.78±2.78 | 73.22±3.63 |
| Post-operation (1
year) | 1.00±0.71 | 5 | 5 | 31.89±2.26 | 90.02±6.12 |
| t-value | 4.46 |
|
| 2.215 | 2.356 |
| P-value | <0.01 | <0.01 | <0.01 | <0.05 | <0.05 |
Discussion
LHB lesions are a common cause of shoulder pain
(12). LHB lesions are caused by an
inflammatory reaction in or around the tendon or shoulder and may
be due to instability or trauma (13). With developments in orthopedic
science, the treatment for LHB lesions has been modified and
improved. In 1940, LHB was considered to be the major source of
shoulder pain, and due to this, tendon fixation was the first
choice of treatment (14,15). However, the current treatment options
for LHB, which is frequently associated with pain, remain
controversial. For refractory shoulder pain with secondary LHB
lesions, the optimal treatment is surgery (16). However, the biggest drawback of LHB
resection is that the tendon ends are free, exhibit a defective
appearance and elbow strength may be reduced (17). Osbahr et al (18) suggested that tendon resection may be
the cause of refractory and chronic biceps-derived pain.
LHB has recently been recognized as one of the
causes of rotator cuff lesions and treatment using surgical LHB
fixation has significantly expanded (19). Surgical indications of LHB fixation
are tendon tear (>50%), medial dislocation of the tendon and
tearing of the subscapularis muscle combined with dislocation of
LHB (20). Crenshaw and Kilgore
(21) suggested that bicep-derived
pain persisting for >5 months combined with limited activity
indicates the requirement for surgical treatment.
LHB fixation may be performed using arthroscopy, via
an open approach and via a combination of these methods. Numerous
techniques for fixation have been demonstrated and four common
types of surgical method exist for the treatment of LHB lesions:
Bone tunnel, soft tissue tendon fixation, keyhole technique and
anchor or interference screw fixation (5).
Soft tissue fixation and the keyhole technique are
performed in an open surgery, whereas anchor and interference screw
fixation are performed under arthroscopy. Amongst all surgical
goals, the fixed strength is most important. The ideal fixation
allows for active and passive activities of the shoulder joint in
its full range, which is important for elderly patients and
athletes due to the fact that a short shoulder joint fixation time
may lead to adhesion of the shoulder joint and a decrease in muscle
strength (22). The fixation
strength of the interference screw technique is greater compared
with that of the anchor, bone tunnel and keyhole techniques
(5,23,24). A
cadaveric study by Buchholz et al (25) indicated that the use of
intramedullary cortical bone plate to fix LHB exhibited no
significant difference in static loading compared with the
interference screw technique, but a decreased failure rate was
observed in cyclic loading. Therefore, the intramedullary cortical
plate has the best outcome in the treatment of LHB injuries.
Buchholz et al (25) also demonstrated that the
intramedullary plate fixation technique by Siebenlist et al
(6) uses a single-layer cortical
bone suspension fixation, places the plate into the medullary canal
and suspends the tendon in the extramedullary space. The
compressive stress between the plate and the intracavitary surface
of the cortical marrow leads to dissolving and absorption of
cancellous bone osteolysis between the plate and the cortical bone
surface of the medullary cavity, thereby resulting in fixation
failure. Therefore, this single-cortical suspension in the
medullary cavity is not reliable and the contralateral cortex
requires to be perforated to pull the tendon, which may result in
axillary nerve injury. Based on these effects, the keyhole
technology was used in the present study for the treatment of LHB
ruptures. Compared with the intramedullary fixation technique, two
holes were drilled on the same side of the LHB and the endobutton
was suspended outside the proximal cortical bone holes. In this
technique, the osteolysis phenomenon may be reduced compared with
the intramedullary suspension and the risk of axillary nerve injury
may be avoided. In addition, the tendon was in contact with ~2 cm
of the surface cortical bone in the medullary cavity, which
benefits tendon-bone healing. Compared with the traditional keyhole
technique, the fixed strength of this technology is more reliable.
However, in patients with LHB injury and rotator cuff tears,
arthroscopic LHB was used with anchor fixation or tenotomy
surgery.
Spatially, the LHB rupture surgery may be roughly
divided into the rotator cuff interval, as well as the
intra-articular and upper and lower edges of the pectoralis major
tendon according to the fixed position. Fixation of LHB at the
rotator cuff interval is frequently used when repairing the rotator
cuff under arthroscopy. Intra-articular fixation of LHB may be
performed using complete arthroscopy surgery and the fixation
position may be at the humeral head cartilage margin, around the
rotator cuff and at the apex of the intertubercular sulcus
(26). Intra-articular fixation of
LHB maximizes the original muscle tension of the biceps muscle and
eliminates spasmodic pain and pop-eye sign. However, post-operative
intractable pain has been previously reported following the
proximal fixation of LHB, which was caused by extra-articular LHB
tears and tenosynovitis in the intertubercular sulcus (27). A variety of scholars suggested that
the ‘hidden injury’ located in the intertubercular sulcus is
frequently missed under arthroscopy (28). Therefore, LHB is fixed at a low
position to prevent pain in the extra-articular and intertubercular
sulcus and to eliminate the cause of post-operative persistent
pain.
For simple SLAP injuries, intra-articular fixation
of LHB is a useful alternative surgical treatment (5). However, for other LHB tendon disorders,
including LHB ruptures in the intertubercular sulcus, which occurs
in the majority of cases due to the friction experienced by the
intertubercular sulcus, fixation in the intertubercular sulcus or
upper edge of the pectoralis major tendon is more effective
(28). For most patients with LHB
rupture, the tendon rupture occurs in the intertubercular sulcus,
and the preferred method of repair at our institution is fixation
under the intertubercular sulcus and upper the pectoralis major
tendon (5). The advantages of the
technique presented in the present study are that the tendon injury
derived from the intertubercular sulcus, which are often ignored by
surgeons, may be eliminated and adequate biceps muscular tension is
maintained.
Based on the strict selection criterion that the
patients had isolated LHB rupture, the present study examined a
limited number of cases with a relatively short follow-up period.
Therefore, it was not possible to include a control group. The
reasons for the lack of post-operative complications observed were
the limited number of patients and simple operation technique. For
the cases of isolated LHB rupture, a modified keyhole surgical
technique was used and combined with microplate suspension to treat
the LHB tendon. This treatment has the advantages of low difficulty
in operation, high safety and a resultant reliable fixation.
The results of the present study demonstrated that
with keyhole technology, the intramedullary microplate is a
reliable fixation treatment for LHB rupture.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YH wrote this manuscript. YH, LNS, HS and BH
collected and analyzed the data. YH and LNS performed the
experiments. FCZ, CSZ and CJP interpreted the results. LNS revised
and finalized the study. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Hospital of Nanjing University of
Chinese Medicine (Nanjing, China). The patients who participated in
this study had complete clinical data. Informed consent was
obtained from the patients or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Alpantaki K, McLaughlin D, Karagogeos D,
Hadjipavlou A and Kontakis G: Sympathetic and sensory neural
elements in the tendon of the long head of the biceps. J Bone Joint
Surg Am. 87:1580–1583. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Elser F, Braun S, Dewing CB, Giphart JE
and Millett PJ: Anatomy, function, injuries, and treatment of the
long head of the biceps brachii tendon. Arthroscopy. 27:581–592.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gaskill TR, Braun S and Millett PJ:
Multimedia article. The rotator interval: Pathology and management.
Arthroscopy. 27:556–567. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Frost A, Zafar MS and Maffulli N: Tenotomy
versus tenodesis in the management of pathologic lesions of the
tendon of the long head of the biceps brachii. Am J Sports Med.
37:828–833. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mazzocca AD, Bicos J, Santangelo S, Romeo
AA and Arciero RA: The biomechanical evaluation of four fixation
techniques for proximal biceps tenodesis. Arthroscopy.
21:1296–1306. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Siebenlist S, Lenich A, Buchholz A,
Martetschläger F, Eichhorn S, Heinrich P, Fingerle A, Doebele S,
Sandmann GH, Millett PJ, et al: Biomechanical in vitro validation
of intramedullary cortical button fixation for distal biceps tendon
repair: A new technique. Am J Sports Med. 39:1762–1768. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lopiz Y, Alcobía-Díaz B, Galán-Olleros M,
García-Fernández C, Picado AL and Marco F: Reverse shoulder
arthroplasty versus nonoperative treatment for 3- or 4-part
proximal humeral fractures in elderly patients: A prospective
randomized controlled trial. J Shoulder Elbow Surg. Sep 6–2019.doi:
10.1016/j.jse.2019.06.024 (Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Frank T, Seltser A, Grewal R, King GJW and
Athwal GS: Management of chronic distal biceps tendon ruptures:
Primary repair vs. semitendinosus autograft reconstruction. J
Shoulder Elbow Surg. 28:1104–1110. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sarda P, Qaddori A, Nauschutz F, Boulton
L, Nanda R and Bayliss N: Distal biceps tendon rupture: Current
concepts. Injury. 44:417–420. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rhee SM, Jeong HY, Ro K, Pancholi S and
Rhee YG: Double on-lay fixation using all suture-type anchor for
subpectoral biceps tenodesis has favorable functional outcomes and
leads to less cosmetic deformities than single on-lay fixation.
Knee Surg Sports Traumatol Arthrosc. Aug 13–2019.doi:
10.1007/s00167-019-05663-4 (Epub ahead of print). View Article : Google Scholar
|
|
11
|
Brochin RL, Zastrow R, Hussey-Andersen L,
Parsons BO and Cagle PJ: Revision rotator cuff repair: A systematic
review. J Shoulder Elbow Surg. Aug 28–2019.doi:
10.1016/j.jse.2019.06.023 (Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Urita A, Funakoshi T, Amano T, Matsui Y,
Kawamura D, Kameda Y and Iwasaki N: Predictive factors of long head
of the biceps tendon disorders-the bicipital groove morphology and
subscapularis tendon tear. J Shoulder Elbow Surg. 25:384–389. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zabrzynski J, Paczesny L, Lapaj L, Grzanka
D and Szukalski J: Process of neovascularization compared with pain
intensity in tendinopathy of the long head of the biceps brachii
tendon associated with concomitant shoulder disorders, after
arthroscopic treatment. Microscopic evaluation supported by
immunohistochemical. Folia Morphol (Warsz). 77:378–385. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Depalma AF and Callery GE: Bicipital
tenosynovitis. Clin Orthop. 3:69–85. 1954.PubMed/NCBI
|
|
15
|
Yedinak PR and Holbrook BG: Bicipital
tenosynovitis. Rocky Mt Med J. 51:185–191. 1954.PubMed/NCBI
|
|
16
|
Bhatia DN, van Rooyen KS and de Beer JF:
Direct arthroscopy of the bicipital groove: A new approach to
evaluation and treatment of bicipital groove and biceps tendon
pathology. Arthroscopy. 24:368.e1–e6. 2008. View Article : Google Scholar
|
|
17
|
Galasso O, Gasparini G, De Benedetto M,
Familiari F and Castricini R: Tenotomy versus tenodesis in the
treatment of the long head of biceps brachii tendon lesions. BMC
Musculoskelet Disord. 13:2052012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Osbahr DC, Diamond AB and Speer KP: The
cosmetic appearance of the biceps muscle after long-head tenotomy
versus tenodesis. Arthroscopy. 18:483–487. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kane P, Hsaio P, Tucker B and Freedman KB:
Open subpectoral biceps tenodesis: Reliable treatment for all
biceps tendon pathology. Orthopedics. 38:37–41. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lo IK and Burkhart SS: Arthroscopic biceps
tenodesis using a bioabsorbable interference screw. Arthroscopy.
20:85–95. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Crenshaw AH and Kilgore WE: Surgical
treatment of bicipital tenosynovitis. J Bone Joint Surg Am.
48:1496–1502. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Eakin CL, Faber KJ, Hawkins RJ and Hovis
WD: Biceps tendon disorders in athletes. J Am Acad Orthop Surg.
7:300–310. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Golish SR, Caldwell PE III, Miller MD,
Singanamala N, Ranawat AS, Treme G, Pearson SE, Costic R and Sekiya
JK: Interference screw versus suture anchor fixation for
subpectoral tenodesis of the proximal biceps tendon: A cadaveric
study. Arthroscopy. 24:1103–1108. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ozalay M, Akpinar S, Karaeminogullari O,
Balcik C, Tasci A, Tandogan RN and Gecit R: Mechanical strength of
four different biceps tenodesis techniques. Arthroscopy.
21:992–998. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Buchholz A, Martetschlager F, Siebenlist
S, Sandmann GH, Hapfelmeier A, Lenich A, Millett PJ, Stöckle U and
Elser F: Biomechanical comparison of intramedullary cortical button
fixation and interference screw technique for subpectoral biceps
tenodesis. Arthroscopy. 29:845–853. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Elkousy HA, Fluhme DJ, O'Connor DP and
Rodosky MW: Arthroscopic biceps tenodesis using the percutaneous,
intra-articular trans-tendon technique: Preliminary results.
Orthopedics. 28:1316–1319. 2005.PubMed/NCBI
|
|
27
|
Becker DA and Cofield RH: Tenodesis of the
long head of the biceps brachii for chronic bicipital tendinitis.
Long-term results. J Bone Joint Surg Am. 71:376–381. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Moon SC, Cho NS and Rhee YG: Analysis of
‘hidden lesions’ of the extra-articular biceps after subpectoral
biceps tenodesis: The subpectoral portion as the optimal tenodesis
site. Am J Sports Med. 43:63–68. 2015. View Article : Google Scholar : PubMed/NCBI
|